Introduction
Schwannomas are rare and benign tumors of the nerve
sheath originating from well-differentiated Schwann cells in the
peripheral nervous system (1). The
incidence of schwannoma has been reported to be 0.3-0.4 per 100,000
individuals per year (2). The
condition is characterized by the slow growth of a solitary lesion
encapsulated within a tumor envelope. For schwannomas with painful
symptoms, surgical intervention is recommended if surgery is
possible without causing neurological deficits (3). Therefore, surgical resection is the
main treatment for patients with schwannoma and a good prognosis
can be achieved (4-6).
Although the sciatic nerve is the largest nerve of
the human body, schwannomas localized in the sciatic nerve are very
rare, <1% (7,8). During surgery, the sciatic nerve is
usually exposed through a posterior median approach outside the
pelvis. The resection of tumors with the posterior sciatic nerve
approach usually requires a large incision with open exposure
(9). However, in cases of
intrapelvic lesions, a transabdominal approach might be required
(10). To the best of our
knowledge, there are few studies reporting the laparoscopic
resection of intrapelvic sciatic schwannoma. The current report
presents a case of intrapelvic sciatic schwannoma that was recently
successfully resected with laparoscopic excision.
Case report
A 58-year-old woman presented with pain in the right
hip and leg that had persisted for 2 years and had progressively
worsened over time. The patient visited Peking Union Medical
College Hospital (Beijing, China) in June 2022 for treatment. The
pain was associated with numbness of the right lower limb. The
patient had been treated with physiotherapy and acupuncture at
other hospitals, but no benefit was observed. The patient presented
without a previous history of trauma and no subcutaneous nodules
had been noted. There was no family history of schwannomatosis or
neurofibromatosis type 2.
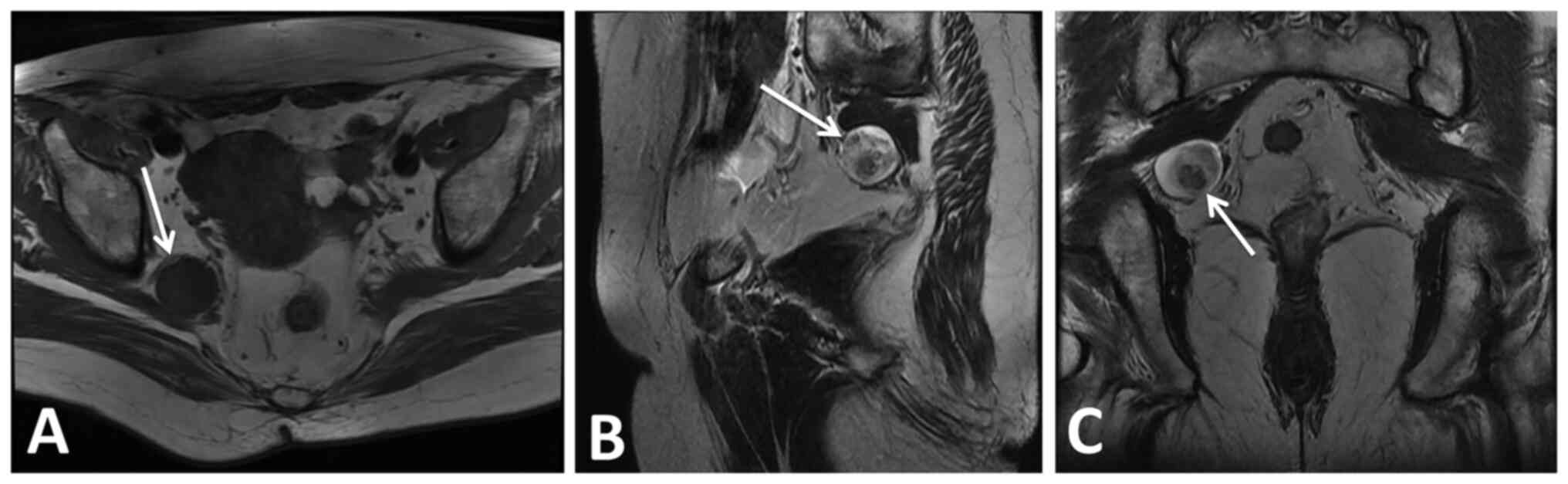
On magnetic resonance imaging (MRI) scans of the
abdomen and pelvis, there was a soft-tissue mass (2.6x2.9x2.3 cm)
in the right pelvic cavity (Fig.
1A). MRI showed a rounded and nonhomogeneous high signal
intensity on T2-weighted images (Fig.
1B and C). On neurological
examination, there was no significant motor loss in the affected
extremity. Before the operation, the patient was informed of the
possibility of conversion to open surgery, as, due to degeneration,
bleeding or cystic changes, it may be hard to divide the tumor from
the normal nerve. In this case, it may be necessary to convert to
open surgery to preserve neurological function. However, if the
tumor was considered to be malignant and nerve invasion had
occurred, radical surgery would be performed.
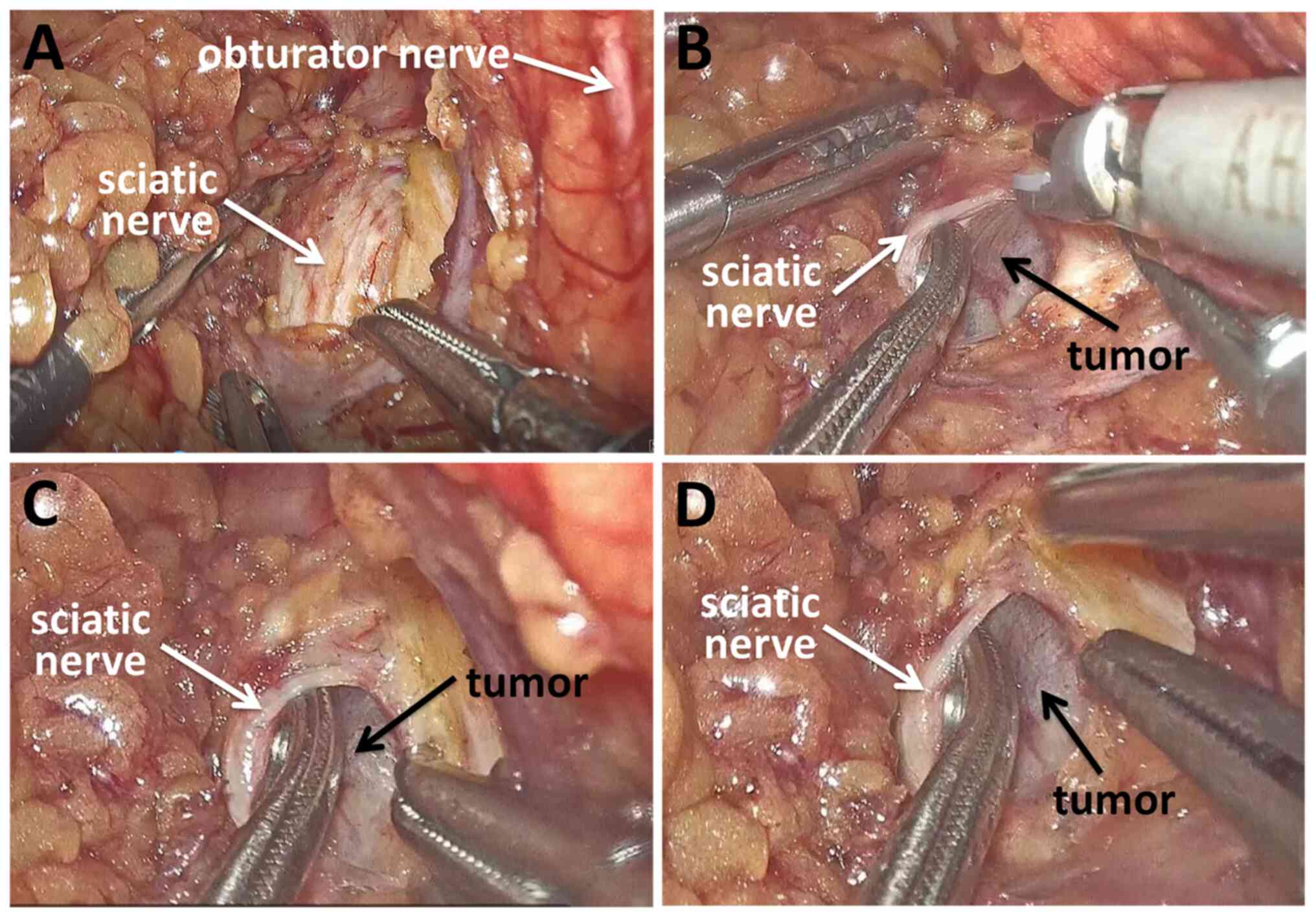
Based on the experience of the surgeons with regard
to laparoscopic surgery for benign presacral tumors and rectal
tumors, this operation was performed with a total laparoscopy. The
patient was placed in the lithotomy position under general
anesthesia. The space created by the induced pneumoperitoneum
facilitated good vision in the confined pre-sacral space. The
pelvic peritoneum was incised along the right ovarian vessel, and
the ovary and ureter were pulled inwards. The right round ligament
of the uterus was severed. The sciatic nerve was exposed by
separating tissue along the internal iliac vascular space to the
vicinity of the piriformis muscle, revealing a tumor 2.5 cm in
diameter. The mass was suspected to be a neurogenic tumor
originating from the right sciatic nerve. After the capsule was
incised, the right sciatic nerve was pulled inwards to detach it
from the surrounding tissue, the mass was removed from the capsule
and the surgical specimen was removed in a specimen bag (Fig. 2). Finally, a drain was inserted
into the space of the right pelvis and the pelvic peritoneum was
sutured closed. The operation time was 70 min and the
intraoperative blood loss was 15 ml.
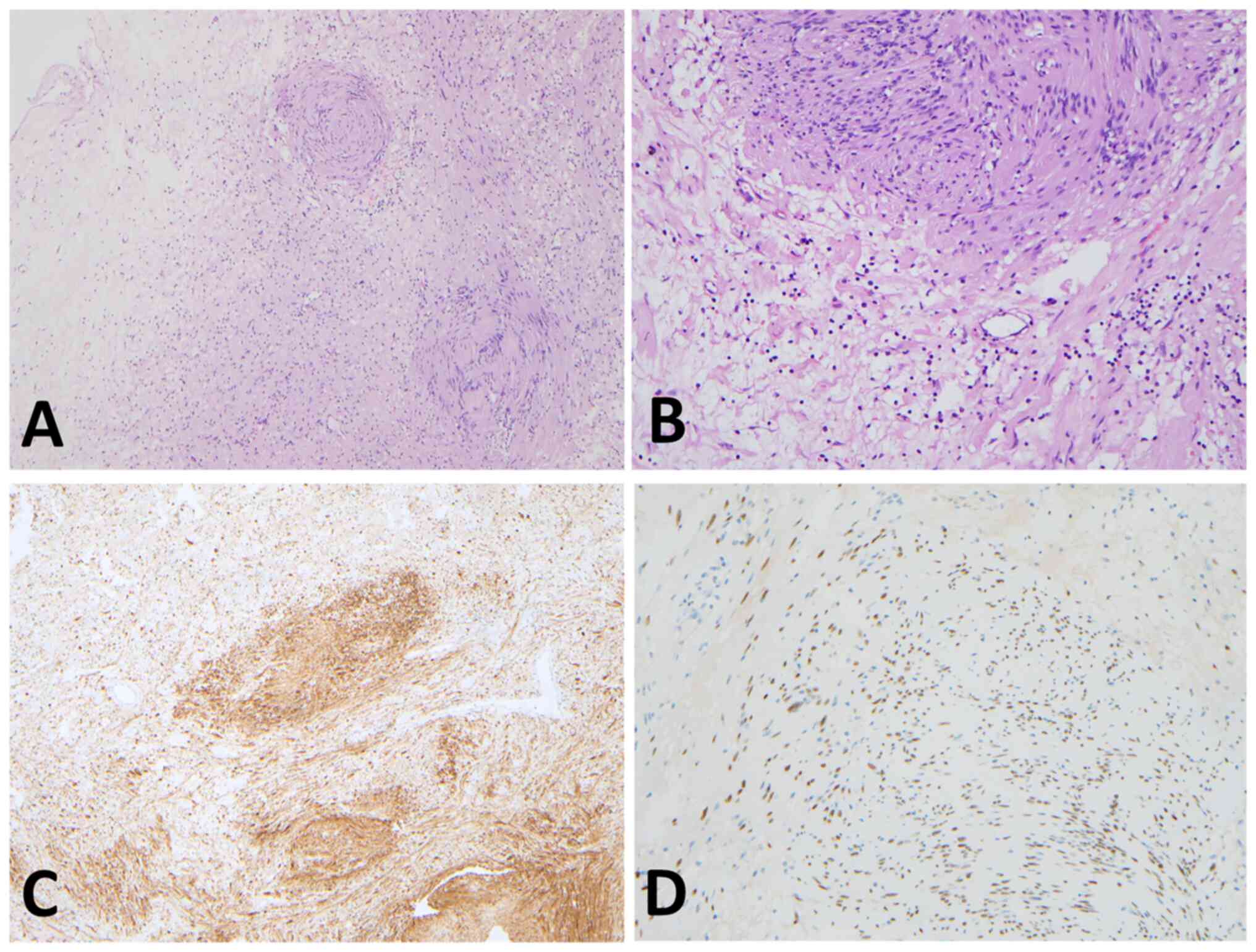
Pathological examination showed a schwannoma, and
immunohistochemistry was positive for S-100 and transcription
factor SOX-10 (Fig. 3). Tumor
tissues were immersed in 4% paraformaldehyde for 24 h and hydrated
through a serial alcohol gradient before being embedded in paraffin
wax blocks. Tissue sections (4 µm) were dewaxed in xylene,
rehydrated through decreasing concentrations of ethanol, and washed
in phosphate buffered saline (PBS). Then, the tissues stained with
hematoxylin and eosin for 5 min at room temperature. Antigens were
unmasked in citrate buffer with pH 6.0. S-100 (Ready to use; cat.
no. GA504; Dako; Agilent Technologies, Inc.) and SOX-10 (Dilution
1:50; cat. no. sc-374170; Santa Cruz; Biotechnology, Inc.) were
immunohistochemically detected. Primary antibodies were incubated
at 37˚C for 2 h. Endogenous peroxidase was blocked by 3% hydrogen
peroxide for 10 min at room temperature. The process of secondary
antibody staining was based on the BOND-MAX Fully Automated IHC
Stainer (Leica Biosystems). The tumor sections were observed by
using an Olympus light microscopy (Olympus Corporation). The
pathological diagnosis was a benign schwannoma. The postoperative
course was uneventful. There were no neurological deficits except
for transient numbness in the right heel. The patient recovered
well and was discharged on postoperative day 4. The patient was
satisfied with the recovery and is still being followed-up.
Discussion
Peripheral nerve tumors are rare, especially those
originating from the sciatic nerve. Most of these tumors are
exposed through a posterior median approach outside the pelvis
(7). For extremely rare schwannoma
cases originating from the intrapelvic sciatic nerve, a surgical
approach to the lateral pelvic space is needed. However, surgical
access to these tumors is difficult due to the narrow lateral
pelvic spaces. In traditional open surgery, a large skin incision
is required to remove the tumor from a lateral pelvic space.
Since the advent of the laparoscopic approach for
benign retrorectal tumors, laparoscopic surgery has gradually
entered the field of pelvic surgery (10). The advantage of the magnified
vision of laparoscopy, as well as the convenience of the long
instruments, enables access of the scope from the pelvis to the
subcutaneous layer of the coccygeal region, facilitating the
exposure and surgical removal of the tumor, which is rarely
achieved by laparotomy and posterior approaches (11). However, extensive experience in
laparoscopic rectal surgery is necessary for surgeons who decide to
approach intrapelvic tumors by laparoscopy.
It has been reported that the laparoscopic approach
for presacral tumors has the advantages of less intraoperative
blood loss, less trauma, quicker recovery and a smaller skin
incision (12). The laparoscopic
approach could provide a feasible and safe alternative to the
conventional approach for presacral tumors. To date, few cases of
laparoscopic resection of sciatic schwannomas in the lateral pelvic
space have been reported (10,13).
Hidaka et al (10) reported
that the laparoscopic resection of schwannoma in the lateral pelvic
space was safe and feasible due to the magnified views on
laparoscopy. This approach also avoids large skin incisions and can
be useful in separating the schwannoma from the right sciatic
nerve.
There are no published guidelines describing
indications for laparoscopic surgery for pelvic schwannomas. Based
on the literature and the surgical experience of the present
medical center, laparoscopic surgery could be safely performed for
benign intrapelvic schwannoma (10). Recurrence seems to be rare for
benign schwannomas, so some surgeons consider a partial resection
to be feasible (14). Therefore,
there is no strict limit on the tumor size. For a large pelvic
schwannoma that affects the exposure to the surgical field,
preoperative embolization could be performed (15). However, if the tumor is >10 cm
with no significant change after embolization, open surgery is
recommended by the present study. If imaging is accompanied by
malignant signs or the biopsy pathology suggests a malignancy, a
complete resection should be performed. Laparoscopic resection of
malignant pelvic schwannoma may have a risk of recurrence and
metastasis (16,17).
Robotic systems have been gradually applied to the
removal of benign presacral tumors, as they can provide improved
three-dimensional visualization and more flexible and stable
manipulation. It has also been suggested that robotic laparoscopic
resection of pelvic schwannomas may have advantages in preserving
the function of the nerves (18,19).
Due to the learning curve, robotic laparoscopic resection should be
limited to experienced surgeons in high-volume centers, which
somewhat limits the progress of these systems. To the best of our
knowledge, no evidence of superiority between laparoscopic
resection and robotic laparoscopic resection of pelvic schwannoma
exists. It is believed that with the increasing popularity of
robotic surgery, its advantages will gradually become
prominent.
Surgical resection of schwannomas aims to preserve
the associated nerves. On the premise of tumor resection, damage to
the nerve should be minimized. During the operation, the tumor
capsule should be dissected layer by layer and carefully explored
to avoid nerve injury. We recommended that this procedure should be
performed with assistance from laparoscopic surgeons who are also
able to perform the same surgery. Good cooperation of surgeons is
beneficial to expose the surgical field and reduce the possibility
of nerve injury. Adjunctive electrophysiological monitoring can
also be applied to prevent nerve damage during robotic-assisted or
laparoscopic surgery (11,20).
The present study demonstrated the safety and
feasibility of laparoscopic excision for intrapelvic schwannomas of
the sciatic nerve. The detailed surgical approach should be based
on patient factors such as previous surgery, tumor characteristics
and the expertise of the surgeon. Although the prognosis for most
of these tumors is good, long-term follow-up is still necessary. In
the future, more delicate and minimally invasive surgical
techniques will be used to reduce the damage to patients and
accelerate recovery.
Acknowledgements
Not applicable.
Funding
Funding: This study was funded by the Chinese Academy of Medical
Sciences Innovation Fund for Medical Sciences (grant no.
2021-I2M-1-015).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
RW was responsible for the writing of the
manuscript. BW conceived the original idea, supervised the study
and was the primary physician of the patient. RW and SL collected
pathological and immunohistochemical data. SL performed the
literature search and performed the revisions. RW and BW confirm
the authenticity of all the raw data. CL and FG acquired data from
the patient, and investigated the patient history and clinical
data. XX and BN participated in the surgery. XX, BN and BW reviewed
the literature and revised the manuscript. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained for the
publication of the patient's data and images in this case
report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Huang J, Mobbs R and Teo C: Multiple
schwannomas of the sciatic nerve. J Clin Neurosci. 10:391–393.
2003.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Godkin O, Ellanti P and O'Toole G: Large
schwannoma of the sciatic nerve. BMJ Case Rep.
2016(bcr2016217717)2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Evans DG, Mostaccioli S, Pang D, Fadzil
OCM, Pittara M, Champollion N, Wolkenstein P, Thomas N, Ferner RE,
Kalamarides M, et al: ERN GENTURIS clinical practice guidelines for
the diagnosis, treatment, management and surveillance of people
with schwannomatosis. Eur J Hum Genet. 30:812–817. 2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Oberle J, Kahamba J and Richter HP:
Peripheral nerve schwannomas-an analysis of 16 patients. Acta
Neurochir (Wien). 139:949–953. 1997.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Hooper J, O'Connor IT, Golub IJ, Decilveo
AP and Wittig JC: Retrospective analysis of 20 patients with
schwannomas: Magnetic resonance imaging characteristics, pain, and
outcomes following excision. Orthopedics. 40:e1036–e1043.
2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Gosk J, Gutkowska O, Urban M, Wnukiewicz
W, Reichert P and Ziolkowski P: Results of surgical treatment of
schwannomas arising from extremities. Biomed Res Int.
2015(547926)2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Telera S, Raus L, Vietti V, Pace A,
Villani V, Galie E, Freda N, Carosi M and Costantini M: Schwannomas
of the sciatic nerve: A rare and neglected diagnosis. A review of
the literature with two illustrative cases. Clin Neurol Neurosurg.
195(105889)2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Erdoğan F, Say F and Barış YS:
Schwannomatosis of the sciatic nerve: A case report. Br J
Neurosurg: Jul 18, 2021 (Epub ahead of print).
|
|
9
|
Russell SM: Preserve the nerve:
Microsurgical resection of peripheral nerve sheath tumors.
Neurosurgery. 61 (Suppl 3):S113–S117. 2007.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Hidaka E, Ishiyama Y, Maeda C, Nakahara K,
Shimada S, Mukai S, Sawada N, Ishida F and Kudo SE: Laparoscopic
extirpation of a schwannoma in the lateral pelvic space. Case Rep
Surg. 2016(1351282)2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Mazzola CR, Power N, Bilsky MH, Robert R
and Guillonneau B: Pudendal schwannoma: A case report and
literature review. Can Urol Assoc J. 8:E199–E203. 2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Zhou J, Zhao B, Qiu H, Xiao Y, Lin G, Xue
H, Xiao Y, Niu B, Sun X, Lu J, et al: Laparoscopic resection of
large retrorectal developmental cysts in adults: Single-centre
experiences of 20 cases. J Minim Access Surg. 16:152–159.
2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Melvin WS: Laparoscopic resection of a
pelvic schwannoma. Surg Laparosc Endosc. 6:489–491. 1996.PubMed/NCBI
|
|
14
|
Harris MS, Moberly AC and Adunka OF:
Partial resection in microsurgical management of vestibular
schwannomas. JAMA Otolaryngol Head Neck Surg. 143:863–864.
2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Jia Z, Lyu X, Xu Y, Leonardi R and Zhang
X: Robot-assisted laparoscopic resection of a huge pelvic tumor: A
case report. Arch Ital Urol Androl. 88:144–146. 2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Houcine M, Yacine O, Mahdi H, Alia Z, Seif
B, Mourad Z, Samir FF and Kacem M: Surgical treatment of a
presacral schwannoma: A case report. Ann Med Surg.
83(104609)2022.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Zhang TT, Wang ZS, Wang R, Wu X, Zhao ML
and Su F: Malignant peripheral nerve sheath tumor of the cervix. J
Coll Physicians Surg Pak. 32:S24–S27. 2022.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Deboudt C, Labat JJ, Riant T, Bouchot O,
Robert R and Rigaud J: Pelvic schwannoma: Robotic laparoscopic
resection. Neurosurgery. 72 (1 Suppl Operative):2–5.
2013.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Perrin H, Brunner P, Ortega JC, Mercier B,
Clement N, Robino C and Chazal M: Robotic resection of an obturator
schwannoma with preservation of normal nerve fascicles and
function. J Robot Surg. 11:479–483. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Konstantinidis KM, Hiridis S and
Karakitsos D: Robotic-assisted surgical removal of pelvic
schwannoma: A novel approach to a rare variant. Int J Med Robot.
7:55–59. 2011.PubMed/NCBI View
Article : Google Scholar
|