Introduction
The incidence of lumbar degenerative diseases is
increasing annually, and with an ever-aging population and longer
life expectancies, this trend will further continue (1). Lumbar spinal stenosis is the most
common cause of lumbar spinal disease in patients aged >65 years
who require surgical treatment (1). The symptoms of lumbar spinal stenosis
include compression of the nerve roots and dural sac as well as
pathological stenosis of the spinal canal (2). Surgical treatment is usually
recommended for patients in whom conservative treatment fails as it
results in better clinical outcomes (3). In contrast, traditional open surgery
requires extensive dissection of the paravertebral muscles,
resulting in muscle ischemia, denervation, and atrophy, leaving
patients with residual back pain (4,5).
Various minimally invasive techniques have been developed in recent
years to overcome these shortcomings. Through small incisions,
arthroscopes, endoscopes, and microscopes are used to provide a
clear working field and reduce tissue damage (4,6,7). The
compression of the nerve caused by lumbar spinal canal stenosis
typically results in lower back pain, leg pain, and other symptoms,
thus affecting the quality of life of patients. Microscopic
decompression (MD) surgery has been widely used in the clinic for
patients with lumbar spinal stenosis and has good outcomes.
However, the operation space is narrow, and the cost of training
surgeons is high. In addition, when performing lumbar spinal canal
decompression using MD, the instrument must first pass through the
working cannula, so the choice of available instruments is greatly
limited (8).
Recently, clinicians in China and other countries
have paid increasing attention to unilateral biportal endoscopic
(UBE) surgery given the improvements introduced in this surgical
method by Korean researchers (9).
In this method, one channel is implanted into the endoscope for
visual field coverage and the other serves as a working channel. In
several cases, the two channels are located 1.0 cm from the midline
and 1.0-1.5 cm from the upper and lower midlines of the lesion gap.
This biportal approach prevents damage to the erector spinae caused
by conventional debridement procedures that crush the important
muscles. Otherwise, variable access angles provide a wider, more
detailed view of the surgeon's contralateral side. It allows a
wider view of the intervertebral foramen, and possible injuries to
the exiting nerve and the radicular artery can be avoided by using
a paraspinal extraforaminal approach (10). As a relatively novel surgical
technique, it has gained popularity in China and other countries
for the treatment of lumbar spinal stenosis (11).
Although the efficacy of these two surgical
procedures has been compared, there are no sufficient literature or
medical records available to reach accurate conclusions. In this
paper, a comprehensive literature search on UBE and MD surgeries
for the treatment of lumbar spinal stenosis was performed. The aim
was to objectively evaluate the two methods' effectiveness and
safety.
Materials and methods
Literature search
The present study was conducted following the PRISMA
guidelines (12). The databases
searched included PubMed, EMBASE, Cochrane Library, Web of Science,
ClinicalTrials.gov, Google Scholar, China
National Knowledge Infrastructure (CNKI), Chinese Biomedical
databases, Cochrane Library and ProQuest Dissertations and Theses
to analyse the efficacy and safety of UBE vs. MD for treating
lumbar spinal stenosis. The literature retrieval strategy was as
follows: [‘UBE’(All Fields) OR ‘BESS’ (All Fields) OR (‘biportal’
(All Fields) AND (‘endoscoped’(All Fields) OR ‘endoscopes’ (MeSH
Terms) OR ‘endoscopes’ (All Fields) OR ‘endoscope’ (All Fields) OR
‘endoscopical’ (All Fields) OR ‘endoscopically’ (All Fields) OR
‘endoscopy’ (MeSH Terms) OR ‘endoscopy’ (All Fields) OR
‘endoscopic’ (All Fields))] AND [‘MD’ (All Fields) OR “MD”
(Journal) OR ‘monde dent’ (Journal) OR ‘md chic’ (Journal) OR
((“microscop” (All Fields) OR ‘microscopal’ (All Fields) OR
‘microscope’ (All Fields) OR ‘microscopes’ (All Fields) OR
‘microscopic’ (All Fields) OR ‘microscopical’ (All Fields) OR
‘microscopically’ (All Fields) OR ‘microscopics’ (All Fields)] AND
[‘decompress’ (All Fields) OR ‘decompressed’ (All Fields) OR
‘decompresses’ (All Fields) OR ‘decompressing’ (All Fields) OR
‘decompression’ (MeSH Terms) OR ‘decompression’ (All Fields) OR
‘decompressions’ (All Fields) OR ‘decompressive’(All Fields))]. The
period for retrieval was the establishment of the database to April
2022, and the retrieval languages were limited to English and
Chinese.
Eligibility criteria
The inclusion criteria for studies were: i) Patients
with clear clinical symptoms and diagnosis of lumbar spinal
stenosis by physical and auxiliary examinations; ii) the research
design was a randomized controlled trial (RCT) or cohort study
(CS); iii) no significant difference in baseline data between the
two groups (UBE and MD); iv) at least 6 months of follow-up time;
and v) availability of full-text. Studies were excluded based on
the following criteria: i) Literature in a language other than
Chinese and English; ii) when there were multiple reports from a
single centre, the study with the largest sample size without
duplication was selected after reading the full text; iii) multiple
similar studies in the same unit; duplicate cases were excluded
after reading the full text; and iv) studies with a sample size
<20.
Data extraction
Following the selection criteria, two authors read
the full text of the literature. They independently searched the
aforementioned databases and the information was extracted from the
literature. Finally, they thoroughly searched and extracted all
relevant information from all the studies by repeatedly checking
them. The two authors discussed the extracted information and any
disagreements were resolved by a third researcher.
Based on the studies reviewed, the following
information was extracted: i) Last name of the first author; ii)
year of publication; iii) country in which the study was conducted;
iv) study design (CS or RCT); and v) patient characteristics
(treatment level, follow-up time, age, and sex).
Quality assessment
The Newcastle-Ottawa Quality Assessment Scale (NOS)
was used to evaluate the quality of the articles included in the
CS. The maximum score was 9, and studies with a NOS score ≥7 were
considered high-quality studies (13). For RCTs, the risk of bias was
assessed using the Cochrane Collaboration Risk of Bias Assessment
Tool (14).
Credibility analysis
Data analysis was implemented using the R version
4.1.3 R Core Team (http://www.R-project.org/). Binomial variables were
analysed by calculating the odds ratios (OR) and 95% confidence
intervals (CI). For continuous variables, the standardized mean
difference (SMD) and 95% CI for analysis were used. Heterogeneity
was assessed using I2 statistics, and a random effects
model was chosen when heterogeneity was significant
(I2>50%); otherwise, a fixed-effects model was
selected. Publication bias was assessed for outcomes in >10
included studies using funnel plots.
Results
Description of included studies
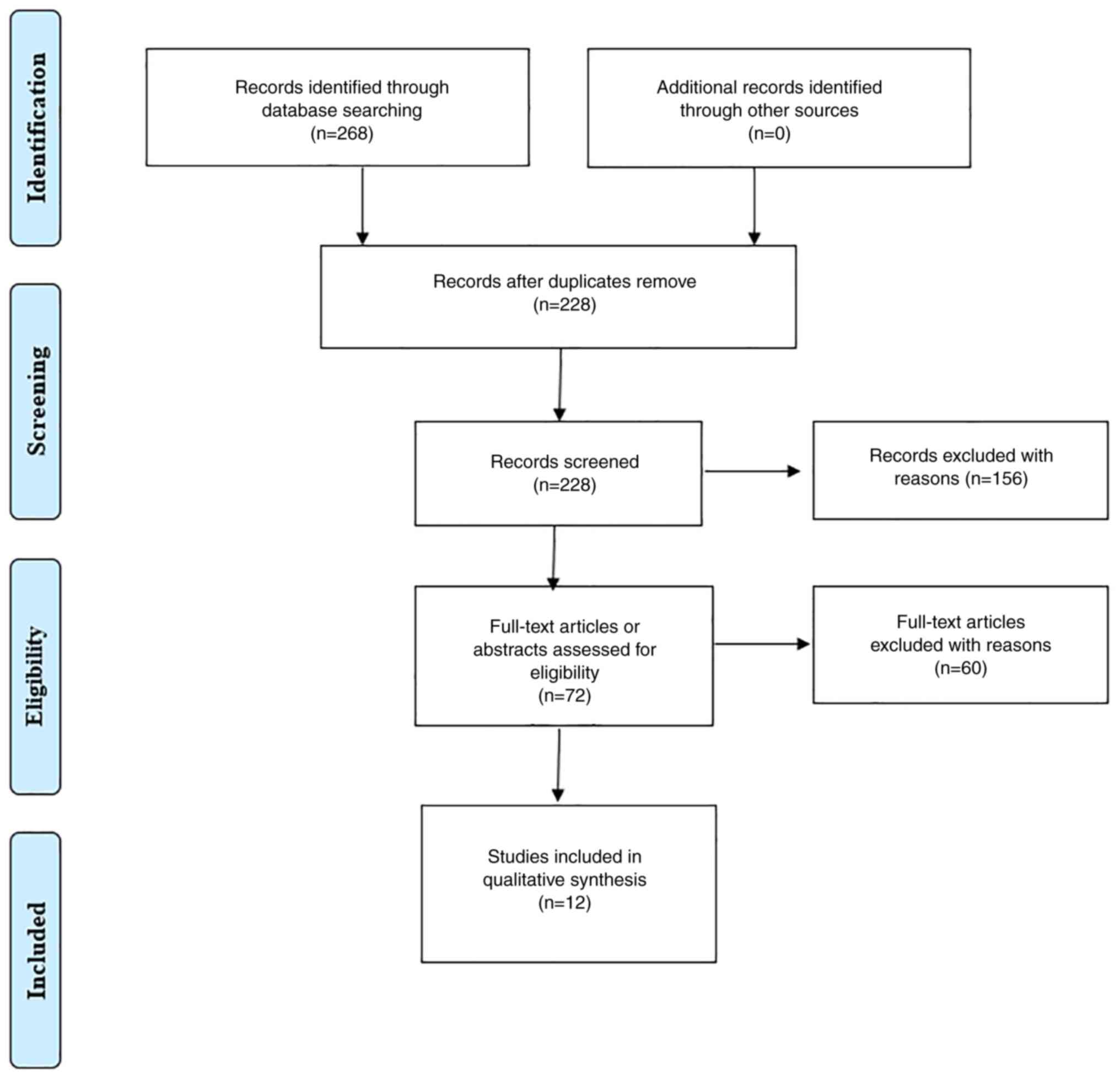
The initial search yielded 268 data points. After
removing duplicates, 228 records were screened, after which 156
were excluded due to irrelevance. Subsequently, 72 full-text
articles or abstracts were assessed for eligibility, and 60
articles were excluded. The remaining 12 studies were included in
the data synthesis. A total of three Chinese articles (15-17)
and nine foreign articles (18-26),
including four RCTs and eight CSs, with a total of 1,067 patients,
including 250 men and 249 women in the UBE group and 290 men and
278 women in the MD group. The screening process and results are
presented in Fig. 1, and the basic
characteristics of the study participants are summarized in
Table I.
 | Table IInformation on the included
studies. |
Table I
Information on the included
studies.
| | Follow-up | |
|---|
| | Treated level | | Sex | |
|---|
| Study | Country | Study design | Group | L1/2 | L2/3 | L3/4 | L4/5 | L5/S1 | Time, month | Age, year, mean ±
SD | Male | Female | NOS score | (Refs.) |
|---|
| Guo et al,
2022 | China |
Retrospective-CS | UBE | | | 9 | 17 | 16 | 12 | 37.5±12.25 | 22 | 20 | 8 | (15) |
| | | | MD | | | 7 | 20 | 18 | 12 | 41.5±1.73 | 23 | 22 | | |
| Wang et al,
2022 | China | Retrospective
-CS | UBE | | | | 27 | 23 | NA | 44.7±14.6 | 26 | 24 | 8 | (16) |
| | | | MD | | | | 28 | 22 | NA | 45.2±11.0 | 27 | 23 | | |
| Aygun et al,
2021 | Saudi Arabia | RCT | UBE | | | NA | | | 24 | 64.64±10.09 | 44 | 33 | Fig.2 | (18) |
| | | | MD | | | NA | | | 24 | 65.05±9.24 | 50 | 27 | | |
| Ito et al,
2021 | Japan | Retrospective
-CS | UBE | | | 13 | 24 | 5 | 6.7±0.6 | 66.3±12.3 | 28 | 14 | 7 | (19) |
| | | | MD | | | 38 | 86 | 15 | 6.9±0.8 | 65.0±11.1 | 71 | 68 | | |
| Yu et al,
2021 | China | Retrospective
-CS | UBE | | | 5 | 10 | 7 | 12 | 59.1±11.7 | 12 | 10 | 8 | (17) |
| | | | MD | | | 6 | 11 | 8 | 12 | 58.3±8.7 | 11 | 14 | | |
| Kim et al,
2020 | Korea | Retrospective
-CS | UBE | | 2 | 8 | 18 | 2 | 12 | 64.23±5.26 | 13 | 17 | 8 | (20) |
| | | | MD | | 4 | 8 | 16 | 2 | 12 | 66.20±6.01 | 12 | 18 | | |
| Min et al,
2020 | Korea | RCT | UBE | | 1 | 7 | 43 | 2 | 27.2±5.4 | 65.74±10.52 | 27 | 27 | Fig.2 | (21) |
| | | | MD | | 1 | 7 | 24 | 3 | 31.5±7.3 | 66.74±7.96 | 19 | 16 | | |
| Park et al,
2020 | Korea | RCT | UBE | 0 | 2 | 5 | 25 | 0 | 12 | 66.2 (41-80) | 13 | 19 | Fig.2 | (22) |
| | | | MD | 3 | 3 | 7 | 17 | 2 | 12 | 67.1 (45-79) | 18 | 14 | | |
| Choi, et al,
2019 | Korea | Retrospective
-CS | UBE | | | NA | | | 6 | 65.4±11.8 | 14 | 21 | 7 | (23) |
| | | | MD | | | NA | | | 6 | 65.2±12.0 | 17 | 13 | | |
| Heo et al,
2019 | Korea | Retrospective
-CS | UBE | | | | 37 | | 12 | 66.7±9.4 | 15 | 22 | 8 | (24) |
| | | | MD | | | | 33 | | 12 | 63.4±11.1 | 12 | 21 | | |
| Kang et al,
2019 | Korea | RCT | UBE | | | 4 | 16 | 12 | 6 | 65.1±8.6 | 18 | 14 | Fig.2 | (25) |
| | | | MD | | | 5 | 15 | 10 | 6 | 67.2±9.5 | 14 | 16 | | |
| Heo et al,
2018 | Korea | Prospective-CS | UBE | | 1 | 8 | 33 | 4 | 14.5±2.3 | 65.4±11.8 | 18 | 28 | 7 | (26) |
| | | | MD | | 2 | 7 | 30 | 3 | 14.5±2.3 | 65.2±12.0 | 16 | 26 | | |
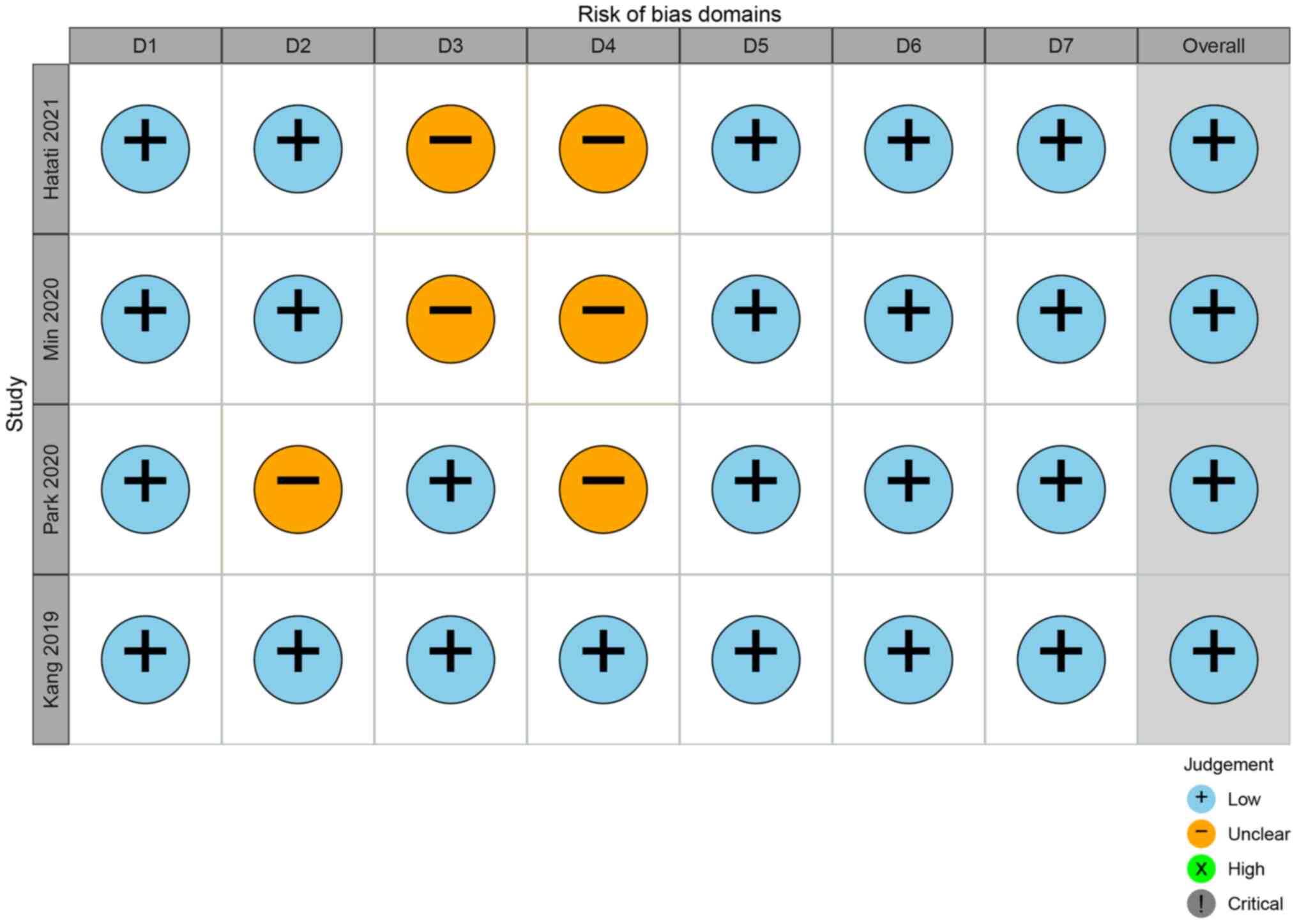
Quality evaluation of the included
literature
This was a high-quality study, in that all included
studies were RCTs or CSs, and all included studies met the
inclusion and exclusion criteria (Fig.
2 and Table I).
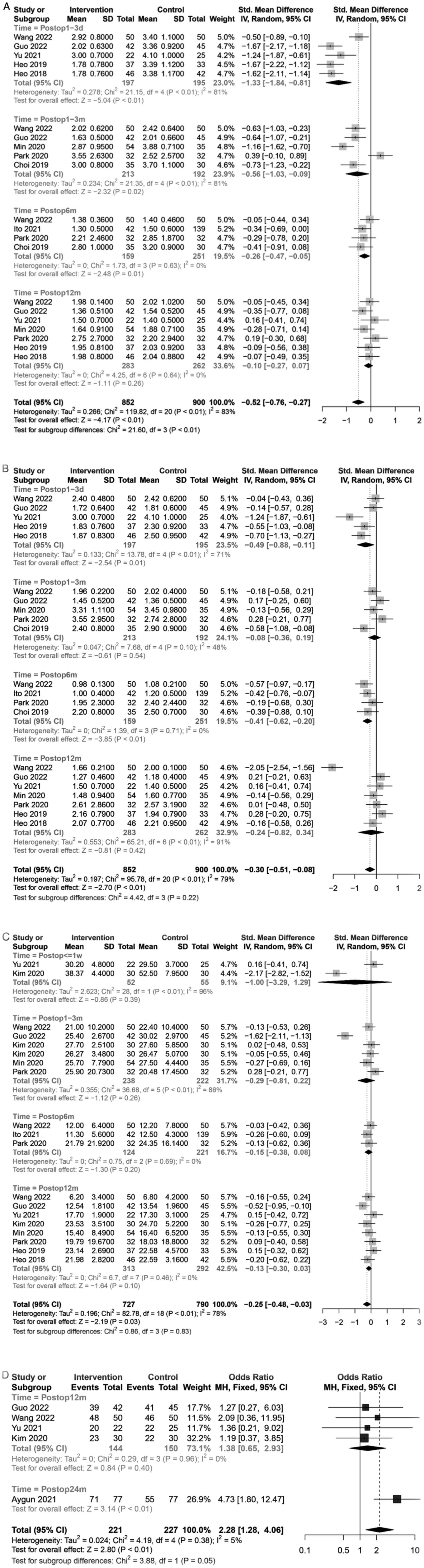
Curative effect after operation
The curative effects of surgery from four aspects
(VAS score for back pain, VAS score for leg pain, ODI, and the
modified MacNab score) were evaluated.
A total of nine studies (15-17,19,21-24,26)
presented postoperative VAS scores for back pain. The total
meta-analysis showed that the postoperative VAS scores of the UBE
group were lower than those of the MD group [SMD=-0.52, 95% CI
(-0.76, -0.27), P<0.01]. Subgroup analysis was performed by
follow-up time. The postoperative VAS score for back pain in the
UBE group was lower than that in the MD group as follows: 1-3 days
[SMD=-1.33, 95% CI (-1.84, -0.81], P<0.01], 1-3 months
[SMD=-0.56, 95% CI (-1.03, 0.09), P=0.02], and 6 months [SMD=-0.26,
95% CI (-0.47, -0.05), P=0.01] after operation. No significant
differences were observed between the UBE and MD groups after 12
months [SMD=-0.10, 95% CI (-0.27, 0.07), P=0.26] (Fig. 3A). In terms of overall data, the
postoperative back pain of UBE was lighter than that of MD within 6
months of operation, but both techniques had similar VAS scores for
back pain after 12 months. A total of nine studies (15-17,19,21-24,26)
presented postoperative VAS scores for leg pain. The total
meta-analysis showed that the postoperative VAS score for leg pain
was lower in the UBE group than that in the MD group [SMD=-0.30,
95% CI (-0.51, -0.08), P<0.01]. Subgroup analysis performed by
the follow-up time showed that the postoperative VAS score for leg
pain in the UBE group was lower than that in the MD group; 1-3 days
[SMD=-0.49, 95% CI (-0.88, -0.11), P=0.01] and 6 months [SMD=-0.41,
95% CI (-0.62, -0.20), P<0.01]. However, no significant
difference was observed in the VAS score for leg pain between the
two groups at 1-3 months [SMD=-0.08, 95% CI (-0.36, 0.19), P=0.54]
and 12 months [SMD=-0.24, 95% CI (-0.82, 0.34), P=0.42] after the
operation (Fig. 3B). In terms of
overall data, the postoperative leg pain of UBE was lighter than
that of MD in the first 3 days and half a year. The patients
treated with UBE achieved satisfactory curative effects in the
early stage.
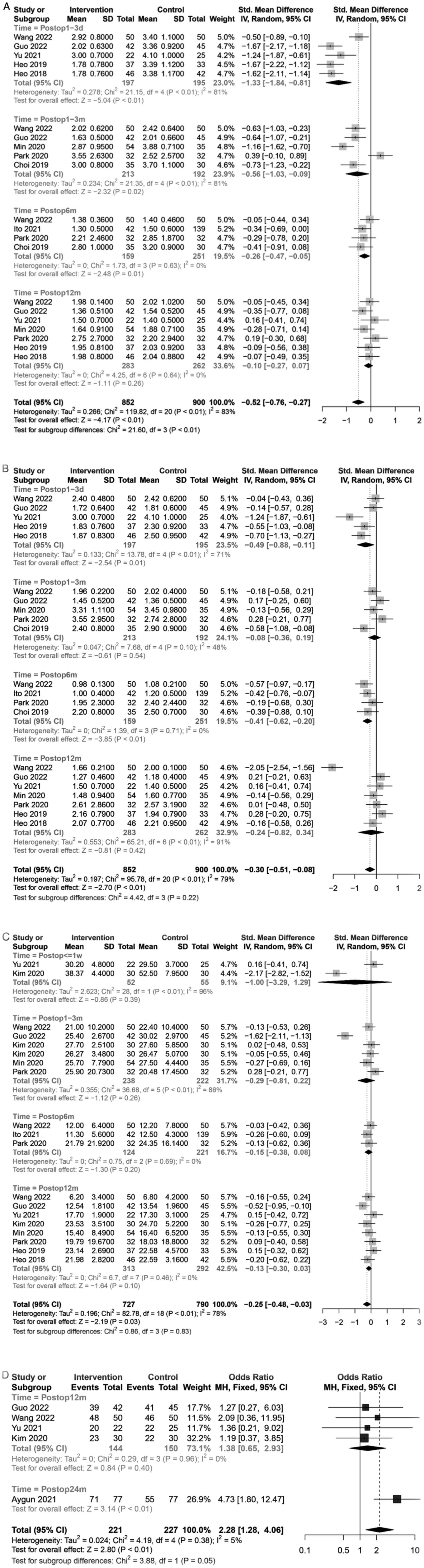 | Figure 3Forest plot of the curative effect
after operation. (A) Analysis of the postoperative VAS score for
back pain between UBE and MD in the treatment of lumbar spinal
stenosis. (B) Analysis of the postoperative VAS score for leg pain
between UBE and MD in the treatment of lumbar spinal stenosis. (C)
Analysis of the postoperative ODI between UBE and MD in the
treatment of lumbar spinal stenosis. (D) Analysis of the modified
MacNab score between UBE and MD in the treatment of lumbar spinal
stenosis. Intervention=UBE group, Control=MD group. UBE, unilateral
biportal endoscopic; MD, microscopic decompression; VAS, visual
analogue scale; CI, confidence interval; IV, inverse-variance
weighting; MH, Mantel-Haenszel; d, days; m, months; w, weeks;
postop, postoperative time; df, degrees of freedom. |
A total of nine studies (15-17,19-22,24,26)
included the postoperative ODI data. The total meta-analysis showed
that the postoperative ODI was lower in the UBE group than that in
the MD group [SMD=-0.25, 95% CI (-0.48, -0.03), P=0.03]. Follow-up
time-based subgroup analysis did not reveal significant differences
in ODI between the UBE and MD groups during the ≤1 week, 1-3
months, 6 months, and 12 months periods (Fig. 3C). In terms of overall data, the
postoperative ODI of UBE was lower than that of MD, but based on
the subgroup analysis, the two techniques had a similar
postoperative ODI. A total of five studies (15-18,20)
presented the modified MacNab score data. The total meta-analysis
showed that the modified MacNab score was better in the UBE group
than that in the MD group [SMD=2.28, 95% CI (1.28, 4.06),
P<0.01]. Subgroup analysis showed no significant difference in
the 12 months postoperative modified MacNab score between the UBE
and MD groups [SMD=1.38, 95% CI (0.65, 2.93), P=0.40] (Fig. 3D). In terms of overall data, the
modified MacNab score of the UBE group was better than that of the
MD group.
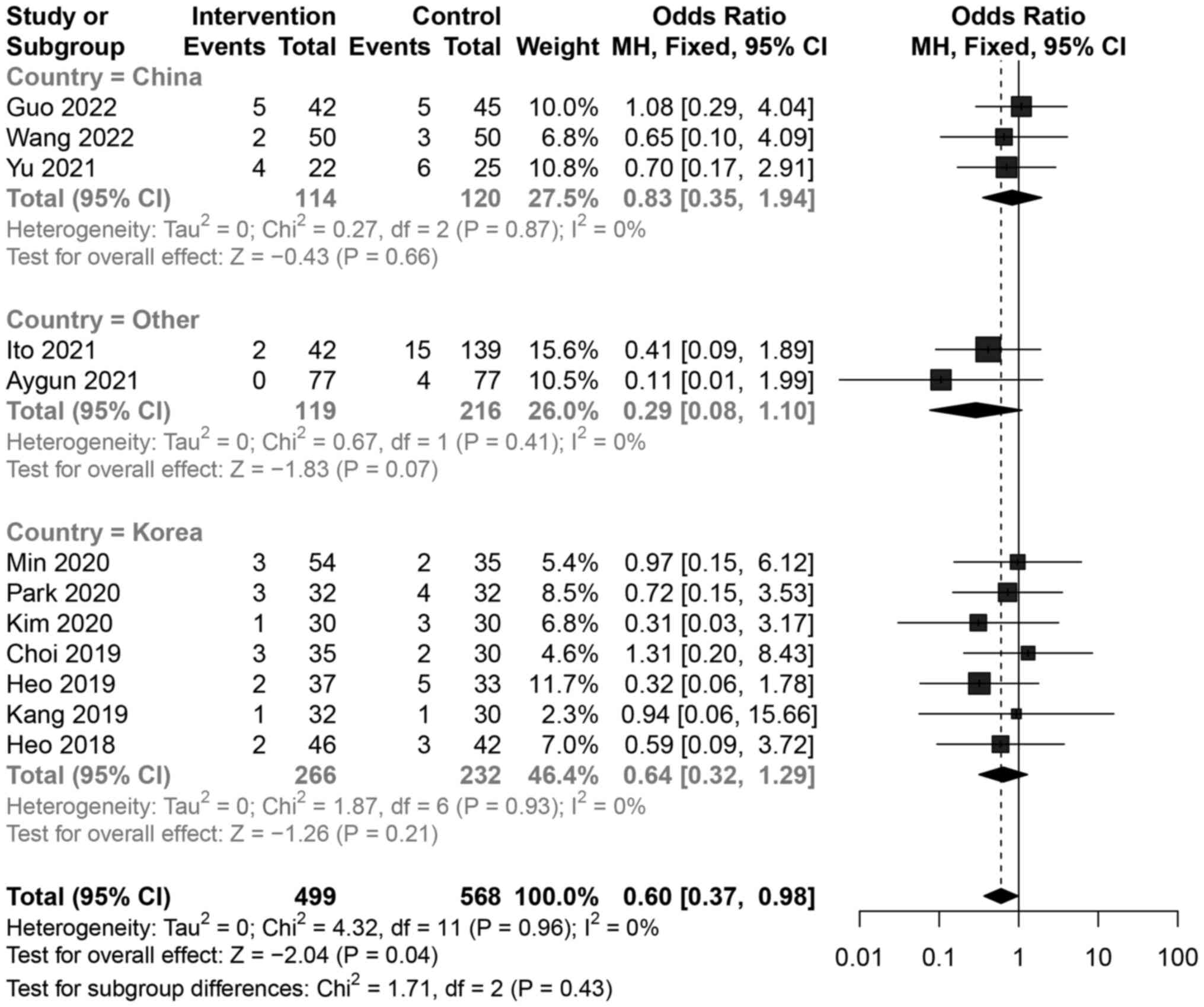
Complications
All 12 studies (15-26)
presented the complication data. The total meta-analysis revealed
that the UBE group had fewer complications than those in the MD
group [SMD=-0.60, 95% CI (0.37, 0.68), P=0.04]. Country-based
subgroup analysis showed no significant differences between the UBE
and MD groups in China [SMD=-0.83, 95% CI (0.35, 1.94), P=0.66],
Korea [SMD=0.64, 95% CI (0.32, 1.29), P=0.21], and the other two
countries [SMD=0.29,95% CI (0.08, 1.10), P=0.07] (Fig. 4). In terms of overall data, the
complications of UBE were lower than that of the MD group. This
reduces the patient's pain and greatly reduced the financial burden
of dealing with complications.
Intraoperative condition
The intraoperative situation of the two operations
based on the amount of intraoperative blood loss and the operation
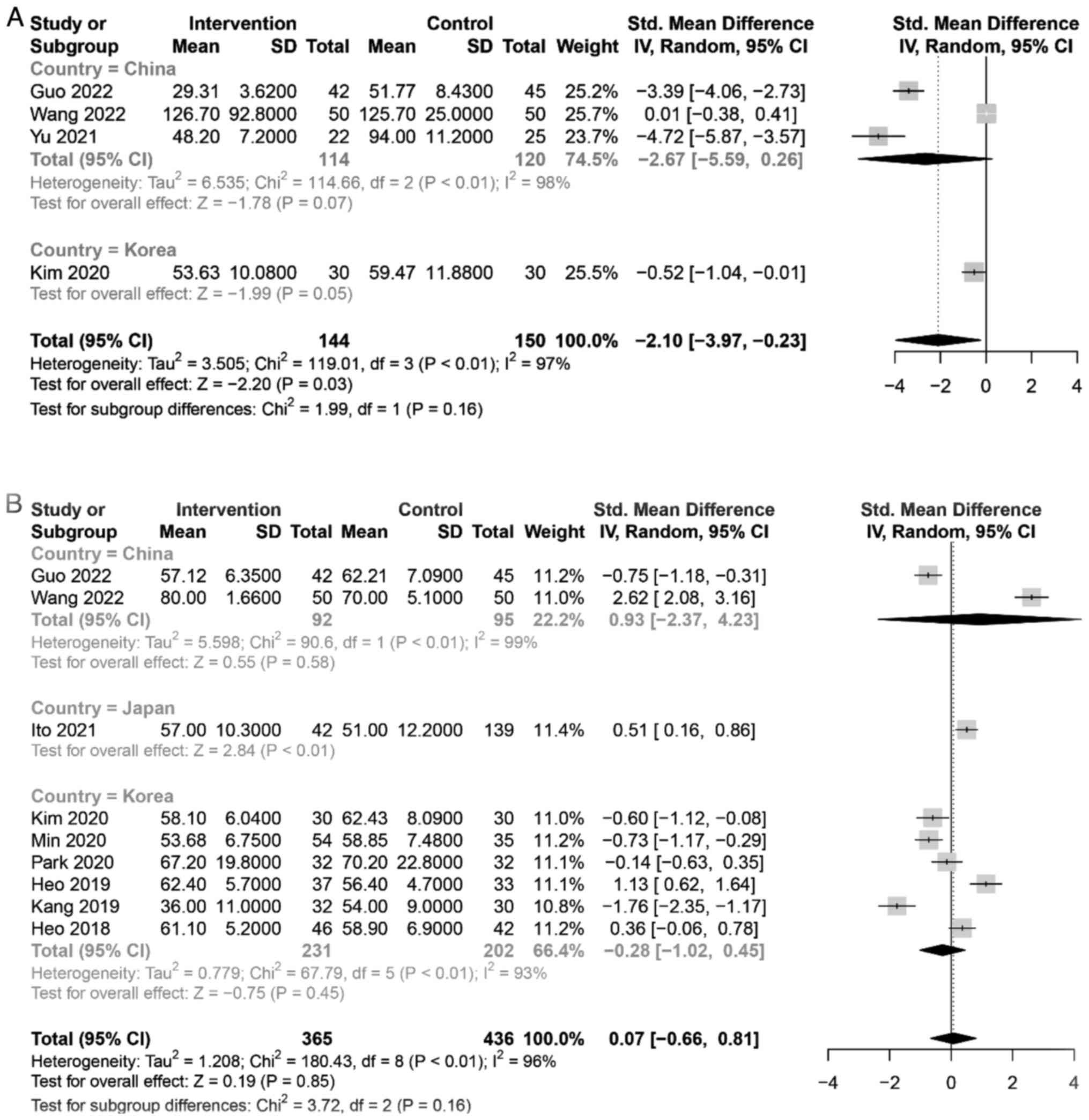
time was evaluated. A total of four studies (15-17,20)
reported data on mean blood loss. The meta-analysis found that
patients with UBE experienced less blood loss than patients with MD
[SMD=-2.10, 95% CI (-3.97, -0.23), P=0.03]. When subgroup analysis
was conducted on the mean blood loss by country, no significant
difference was observed between the UBE and MD groups in China
[SMD=-2.67, 95% CI (-5.59, 0.26), P=0.07, (Fig. 5A)]. In terms of overall data, UBE
resulted in less blood loss than MD, and that was conducive to the
rapid recovery of patients. A total of nine studies (15,16,19,20-22,24-26)
presented the mean operative time data. The meta-analysis showed no
significant difference in operation time between the UBE and MD
groups [SMD=0.07, 95% CI (-0.66, 0.81), P=0.85]. Country-based
subgroup analysis showed no significant difference between the UBE
and MD groups in China [SMD=0.93, 95% CI (-2.37, 4.23), P=0.58] and
Korea [SMD=-0.28, 95% CI (-1.02, 0.45), P=0.45, (Fig. 5B)]. In terms of overall data, the
operation time of the UBE and MD were basically the same.
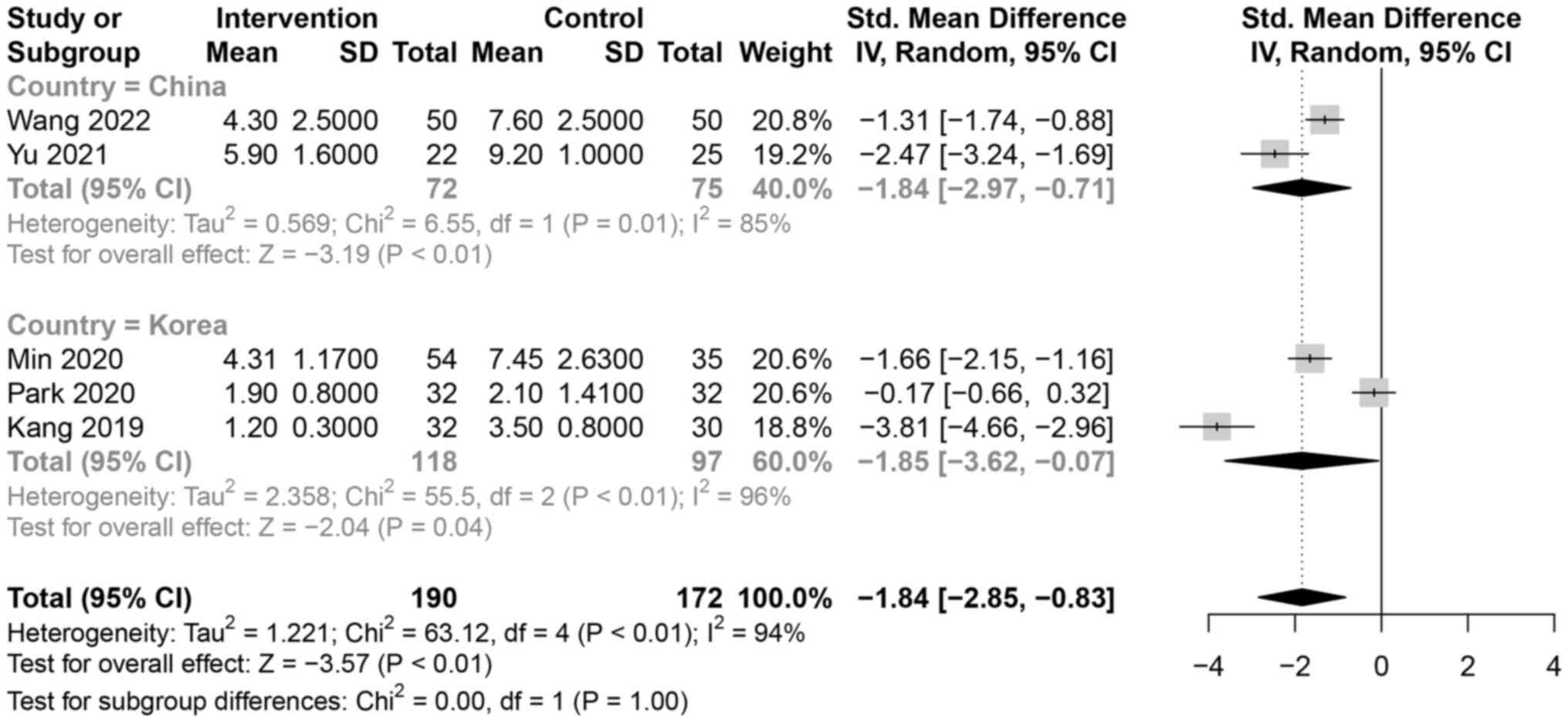
Hospital stays and CRP
A total of five studies (16,17,21,22,25)
presented hospital stay data. Hospital stays were shorter in the
UBE group than those in the MD group [SMD=-1.84, 95% CI (-2.85,
-0.83), P<0.01]. Country-based subgroup analysis revealed
shorter hospital stays in the UBE group than that in the MD group
in China [SMD=-1.84, 95% CI (-2.97, -0.71), P<0.01) and Korea
[SMD=-1.85, 95% CI (-3.62, -0.07), P=0.04, (Fig. 6)]. In terms of overall data, the
patients staying in the hospital in the UBE group was shorter than
that of MD, so UBE could relieve the patient's pain that would
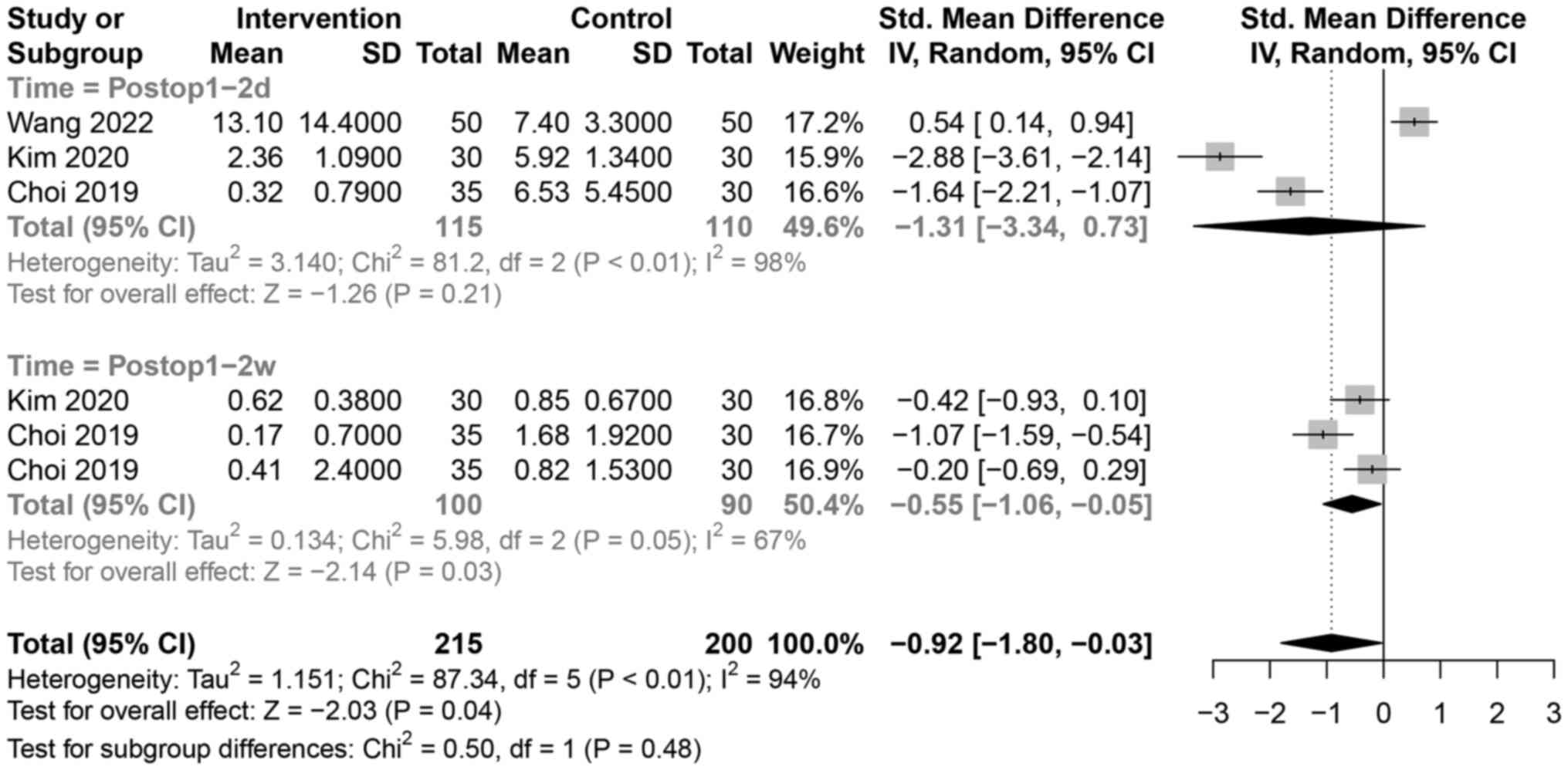
otherwise require long-term hospitalization. A total of three
studies (16,20,23)
presented CRP data. The meta-analysis showed that the postoperative
CRP levels were lower in the UBE group than those in the MD group
[SMD=-0.92, 95% CI (-1.80, -0.03), P=0.04]. Follow-up time-based
subgroup analysis showed that the postoperative CRP levels in the
UBE group were lower than those in the MD group in the 1-2-week
time point [SMD=-0.55, 95% CI (-1.06, -0.05), P=0.03], with no
significant difference at 1-2 days after the operation [SMD=-1.31,
95% CI (-3.34, 0.73), P=0.21, (Fig.
7). In terms of overall data, the postoperative CRP levels in
the UBE were lower than that in the MD group.
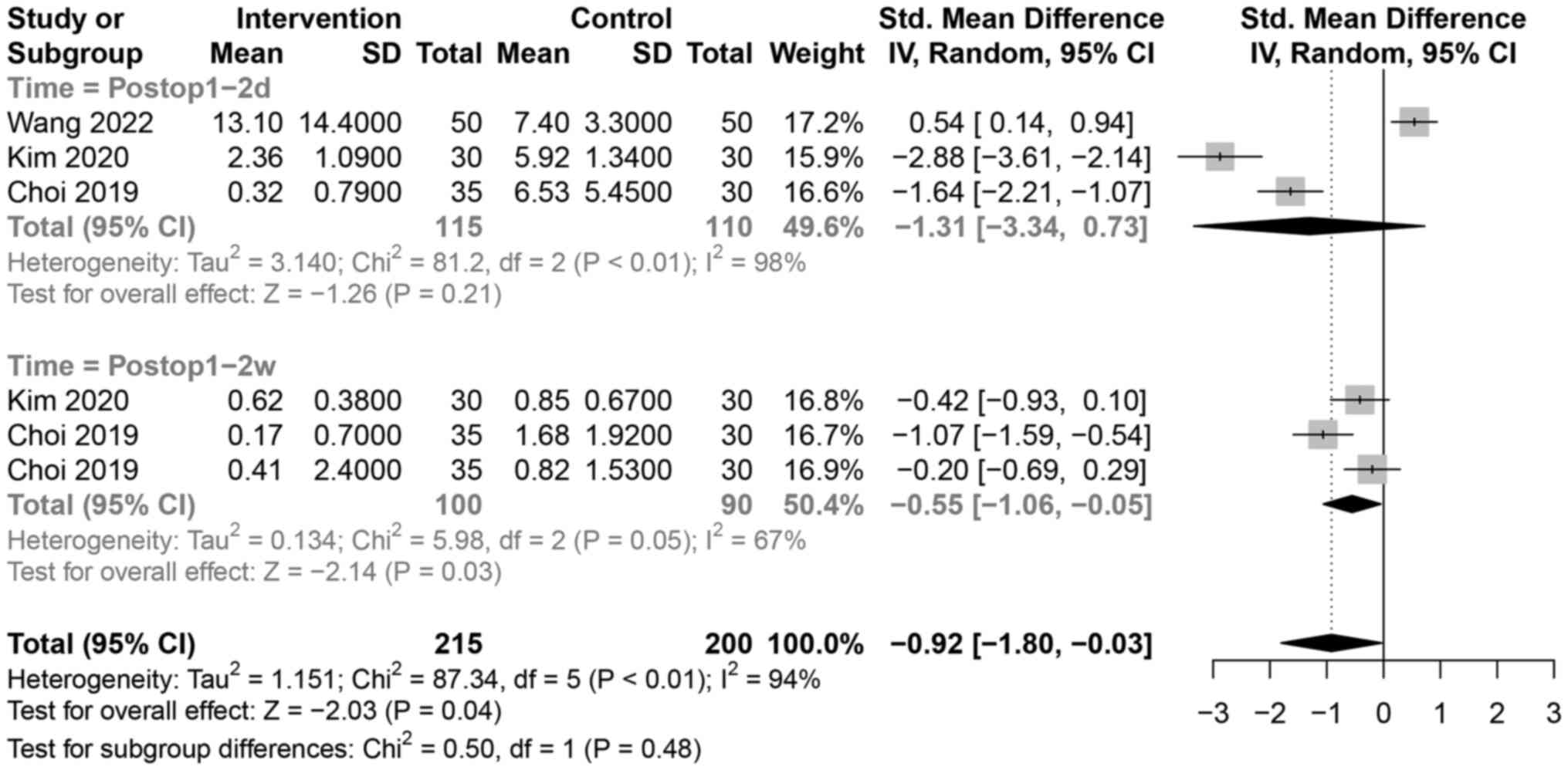 | Figure 7Analysis of the postoperative CRP
between UBE and MD in the treatment of lumbar spinal stenosis;
Intervention=UBE group, Control=MD group. UBE, unilateral biportal
endoscopic; MD, microscopic decompression; CI, confidence interval;
IV, inverse-variance weighting. d, days; m, months; w, weeks;
postop, postoperative time; df, degrees of freedom. |
Heterogeneity and sensitivity
analyses
High heterogeneity was observed in the mean blood
loss (I2=97%), postoperative VAS score for back pain
(I2=83%), postoperative VAS score for leg pain
(I2=79%), ODI (I2=79%), postoperative CRP
(I2=94%), hospital stay (I2=94%), and
operation time (I2=96%). When literature was excluded
individually for these parameters followed by merging of the
remaining literature, the heterogeneity remained high, indicating
that the results of this meta-analysis were stable. Surgeons'
surgical techniques or perioperative care in the hospital may have
contributed to the heterogeneity of the results.
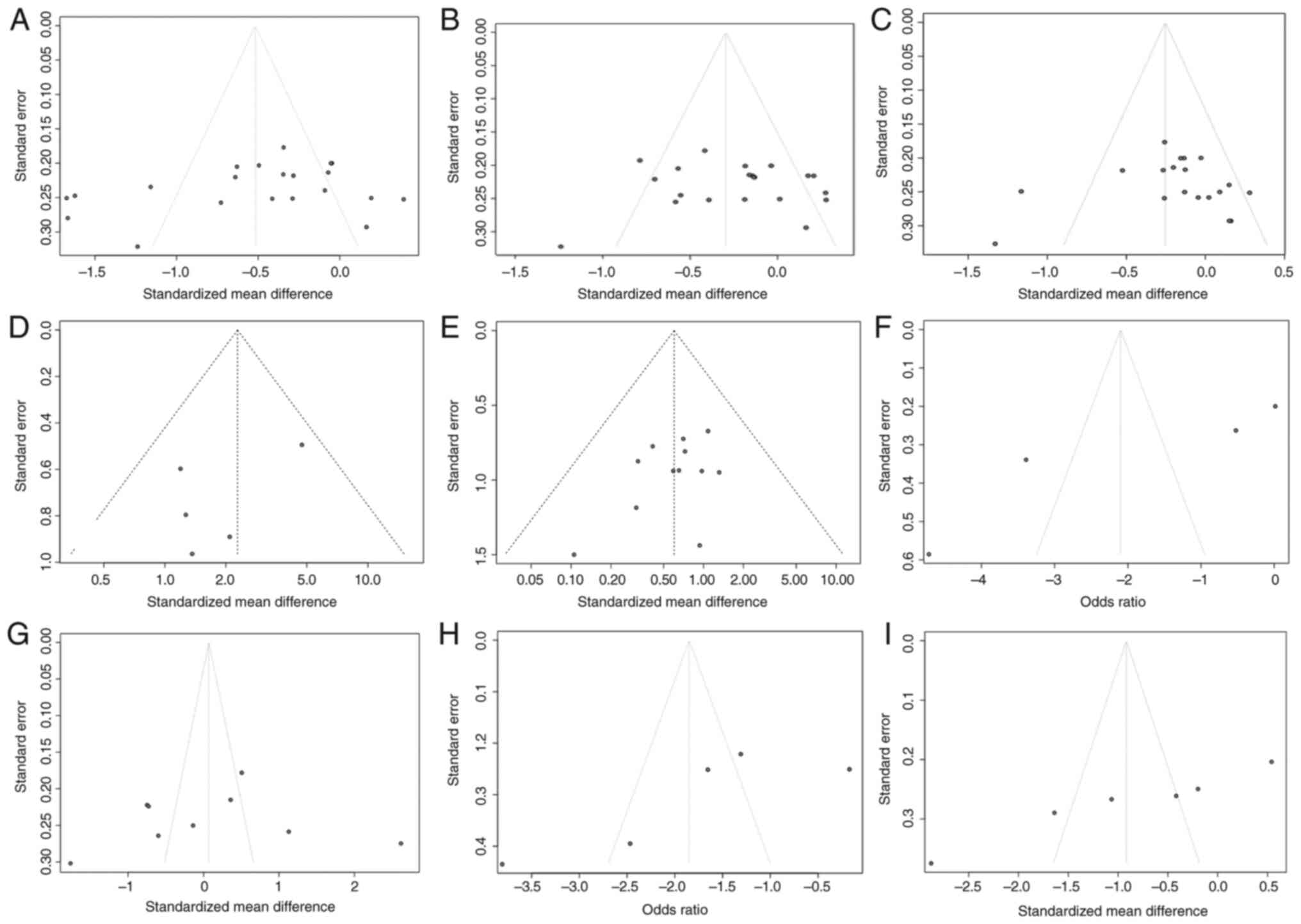
Publication bias
All comparisons were included, and publication bias
was estimated using a funnel plot test (Fig. 8). Although funnel plots are
symmetrical, publication bias may still have been present given the
inclusion of more studies by Korean researchers.
Discussion
The development of UBE. Minimally invasive spine
surgery has been widely used in the treatment of degenerative
diseases of the lumbar spine. It can preserve the structural
integrity of the spine to the greatest extent possible and allows
for a faster recovery (27,28).
Since its conception, MD surgery has been widely promoted and
applied owing to its better vision and lesser surgical trauma than
those associated with open surgery. However, the procedure is
associated with several shortcomings that hamper its clinical
application, such as limited scope regarding indications and
incomplete decompression. More recently, less invasive UBE surgery
has increasingly been used for the treatment of lumbar spinal
stenosis, which has been shown to provide better clinical results
(29). Using an endoscope to look
into the channel and flush it continuously with normal saline, a
clear field of view can be achieved. Conventional spinal surgical
instruments are used for the operation through the working channel,
similar to traditional posterior fenestrations (30,31).
Regardless of the minimally invasive approach used to relieve
lumbar spinal stenosis, the goal was to provide extensive
decompression of the spinal canal while minimizing damage to the
posterior ligament muscle structure (32).
Lower intraoperative blood loss, ODI, CRP changes,
and shorter hospital stays were associated with UBE than with MD,
indicating a less traumatic and rapid recovery process. This may be
due to the flexibility of UBE. In addition, UBE offers a wider
operating space, and the surgical procedure is similar to
traditional open surgery, which allows for easier identification of
the anatomical structures, thus preventing damage to adjacent
tissues. UBE has a larger field of vision under a normal saline
medium of 25-30 mmHg, and it is easier to find the bleeding point
and stop the bleeding as soon as possible in this medium (33-35).
Within 1-3 days after surgery, the UBE group had a
lower VAS score for leg pain. The UBE operation channel is smaller
than the MD channel (1.0 cm vs. 1.8 cm). This allows for reduced
damage to the tissues, a clearer operation field to avoid nerve
contact during operation, and effective reduction of early
postoperative pain. However, within 1-3 months after surgery, the
VAS score for leg pain in the UBE group was similar to that in the
MD group. However, as a result of soft tissue injury healing, the
pain gradually eased and the oppressed nerve root was decompressed,
showing that both UBE and MD treatments were very effective.
Compared with MD however, UBE resulted in less postoperative back
pain, irrespective of whether it manifested early (days) or later
(months) after the operation because of the preservation of the
back muscle and a smaller incision.
All the included articles mentioned complications
such as nerve root injury, dural tear, epidural hematoma, and wound
infection (15-26).
According to the present meta-analysis, UBE had a lower overall
incidence of complications than MD. MD may be associated with a
higher rate of complications due to limitations in the surgical
field of view and mechanical damage caused by constraints of the
limited surgical space. UBE solves this problem by providing a
clear surgical field of view (11,36).
Interestingly, subgroup analyses in China, Korea, and the other two
countries did not show any significant differences between the UBE
and MD groups, indicating that the data included in the subgroup
analysis were limited; that is, it was not sufficient to show the
overall effect. In the present study, cases from several countries
were included, and the results showed that the UBE group had fewer
complications than the MD group, as determined by the analyses.
The present study has some limitations. First, it
included primarily Korean and Chinese studies, and this is not
reflective of surgical procedures in other countries around the
world. Each subgroup had a smaller sample size in the subgroup
analysis and may not be sufficient in power to reflect the
real-world scenario. Second, a publication bias exists since
small-scale studies are prone to remain unpublished, which could
account for language limitations in the inclusion criteria or
selective publication. Third, in this study, four RCTs were
included, whereas the rest of the studies were CSs. Since it is
difficult to completely apply randomized and blinded controls in
practice, observational studies were included, which limited the
quality of the literature included. In certain studies, only
descriptive analyses were performed, precluding accurate clinical
data extraction. The use of different surgical procedures can also
lead to bias. Finally, the absence of ethical approvals may have
affected data analysis, causing inevitable bias. Therefore, the
conclusions of this study need to be further verified using a large
sample prospective RCT. It is important to note that this
evaluation was based on a small number of studies; therefore,
caution should be exercised when interpreting and extrapolating the
results.
In conclusion, compared with MD surgery, UBE is less
prone to intraoperative bleeding and has a shorter postoperative
hospital stay, milder short-term pain symptoms, faster recovery,
and fewer postoperative complications. UBE surgery may replace MD
surgery as a better treatment option for lumbar spinal stenosis.
The results confirm that the UBE technique is a viable option for
lumbar surgery. This technology is not only applicable to the
lumbar spine but can also be used to treat diseases such as the
cervical and thoracic spine. However, existing studies are limited
to small cohort studies with short-term follow-ups, and further
large cohort prospective studies and long-term follow-up studies
are required to evaluate the relative benefits and harms of UBE. It
is hypothesized that as UBE technology is further developed, it
will usher in a new era in spinal endoscopy. However, at present,
additional randomized controlled studies are required to compare
these two technologies.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analysed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
YPW and SLQ designed the study, performed the
research, collected and analysed the data, and wrote the
manuscript. SY collected and analysed the data. YPW, SLQ and SY
confirm the authenticity of all the raw data. YFX and PFH conceived
the study, performed the interpretation of data and reviewed the
article. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hennemann S and de Abreu MR: Estenose
degenerativa do canal lombar. Rev Bras Ortop. 56:9–17.
2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Deer T, Sayed D, Michels J, Josephson Y,
Li S and Calodney AK: A review of lumbar spinal stenosis with
intermittent neurogenic claudication: Disease and diagnosis. Pain
Med. 20:S32–S44. 2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Weinstein NJ, Tosteson TD, Lurie JD,
Tosteson ANA, Blood E, Hanscom B, Herkowitz H, Cammisa F, Albert T,
Boden SD, et al: Surgical versus nonsurgical therapy for lumbar
spinal stenosis. N Engl J Med. 358:794–810. 2008.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Zhu X, Lu J, Xu H, Tang Q, Song G, Deng C,
Wu H, Xu Y, Chen H and Wang J: A comparative study between
minimally invasive spine surgery and traditional open surgery for
patients with spinal metastasis. Spine (Phile Pa 1976). 46:62–68.
2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Kanemura T, Satake K, Nakashima H, Segi N,
Ouchida J, Yamaguchi H and Imagama S: Understanding retroperitoneal
anatomy for lateral approach spine surgery. Spine Surg Relat Res.
1:107–120. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Lee MJ, Mok J and Patel P: Transforaminal
lumbar interbody fusion: Traditional open versus minimally invasive
techniques. J Am Acad Orthop Surg. 26:124–131. 2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
McAfee PC, Garfin SR, Rodgers WB, Allen
RT, Phillips F and Kim C: An attempt at clinically defining and
assessing minimally invasive surgery compared with traditional
‘open’ spinal surgery. SAS J. 5:125–130. 2011.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Lin GX, Huang P, Kotheeranurak V, Park CW,
Heo DH, Park CK, Park JY and Kim JS: A systematic review of
unilateral biportal endoscopic spinal surgery: Preliminary clinical
results and complications. World Neurosurg. 125:425–432.
2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Pao JL, Lin SM, Chen WC and Chang CH:
Unilateral biportal endoscopic decompression for degenerative
lumbar canal stenosis. J Spine Surg. 6:438–446. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Choi CM: Biportal endoscopic spine surgery
(BESS): Considering merits and pitfalls. J Spine Surg. 6:457–465.
2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Pao JL: A review of unilateral biportal
endoscopic decompression for degenerative lumbar canal stenosis.
Int J Spine Sur. 15 (Suppl 3):S65–S71. 2021.PubMed/NCBI View
Article : Google Scholar
|
|
12
|
Selçuk AA: A guide for systematic reviews:
PRISMA. Turk Arch Otorhinolaryngol. 57:57–58. 2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Lo CKL, Mertz D and Loeb M:
Newcastle-ottawa scale: Comparing reviewers' to authors'
assessments. BMC Med Res Methodol. 14(45)2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Cumpston M, Li T, Page MJ, Chandler J,
Welch VA, Higgins JP and Thomas J: Updated guidance for trusted
systematic reviews: A new edition of the cochrane handbook for
systematic reviews of interventions. Cochrane Database Syst Rev.
10(ED000142)2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Guo W, Zhang X, Bao X, Yan K, Qiao H, Zhao
H, Dong X and Liao B: Comparison of unilateral double-channel
endoscopic technique and microscopic nucleus pulposus excision in
the treatment of lumbar spinal stenosis. J Xi'an Jiaotong Univ
(Medical Edition). 43:430–435. 2022.(In Chinese).
|
|
16
|
Wang B, He P, Liu X, Wu Z and Fang X:
Clinical analysis of unilateral double-channel endoscopy and
discoscopy in the treatment of lumbar spinal stenosis. Southeast
National Defense Med. 24:142–146. 2022.(In Chinese).
|
|
17
|
Yu W, Zhou L, Liu D, Gu LW, Xue X and Cao
H: A preliminary study of unilateral double-channel endoscopy in
the treatment of lumbar spinal stenosis. Chin J Minimally Invasive
Surg. 21:56–60. 2021.(In Chinese).
|
|
18
|
Aygun H and Abdulshafi K: Unilateral
biportal endoscopy versus tubular microendoscopy in management of
single level degenerative lumbar canal stenosis: A prospective
study. Clin Spine Sur. 34:E323–E328. 2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Ito Z, Shibayama M, Nakamura S, Yamada M,
Kawai M, Takeuchi M, Yoshimatsu H, Kuraishi K, Hoshi N, Miura Y and
Ito F: Clinical comparison of unilateral biportal endoscopic
laminectomy versus microendoscopic laminectomy for single-level
laminectomy: A single-center, retrospective analysis. World
Neurosurg. 148:e581–e588. 2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Kim HS, Choi SH, Shim DM, Lee IS, Oh YK
and Woo YH: Advantages of new endoscopic unilateral laminectomy for
bilateral decompression (ULBD) over conventional microscopic ULBD.
Clin Orthop Surg. 12(330)2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Min WK, Kim JE, Choi DJ, Park EJ and Heo
J: Clinical and radiological outcomes between biportal endoscopic
decompression and microscopic decompression in lumbar spinal
stenosis. J Orthop Sci. 25:371–378. 2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Park SM, Park J, Jang HS, Heo YW, Han H,
Kim HJ, Chang BS, Lee CK and Yeom JS: Biportal endoscopic versus
microscopic lumbar decompressive laminectomy in patients with
spinal stenosis: A randomized controlled trial. Spine J.
20:156–165. 2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Choi DJ and Kim JE: Efficacy of biportal
endoscopic spine surgery for lumbar spinal stenosis. Clin Orthop
Surg. 11:82–88. 2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Heo DH, Lee DC and Park CK: Comparative
analysis of three types of minimally invasive decompressive surgery
for lumbar central stenosis: Biportal endoscopy, uniportal
endoscopy, and microsurgery. Neurosurg Focus. 46(E9)2019.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Kang T, Park SY, Kang CH, Lee SH, Park JH
and Suh SW: Is biportal technique/endoscopic spinal surgery
satisfactory for lumbar spinal stenosis patients?: A prospective
randomized comparative study. Medicine (Baltimore).
98(e15451)2019.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Heo DH, Quillo-Olvera J and Park CK: Can
percutaneous biportal endoscopic surgery achieve enough canal
decompression for degenerative lumbar stenosis? Prospective
case-control study. World Neurosurg. 120:e684–e689. 2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Alimi M, Hofstetter CP, Pyo SY, Paulo D
and Härtl R: Minimally invasive laminectomy for lumbar spinal
stenosis in patients with and without preoperative
spondylolisthesis: Clinical outcome and reoperation rates. J
Neurosurg Spine. 22:339–352. 2015.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Storzer B and Schnake KJ: Microscopic
bilateral decompression by unilateral approach in spinal stenosis.
Eur Spine J. 25 (Suppl 2):S270–S271. 2016.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Heo DH, Son SK, Eum JH and Park CK: Fully
endoscopic lumbar interbody fusion using a percutaneous unilateral
biportal endoscopic technique: Technical note and preliminary
clinical results. Neurosurg Focus. 43(E8)2017.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Kim JE and Choi DJ: Unilateral biportal
endoscopic spinal surgery using a 30˚ arthroscope for L5-S1
foraminal decompression. Clin Orthop Surg. 10:508–512.
2018.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Kim JE and Choi DJ: Clinical and
radiological outcomes of unilateral biportal endoscopic
decompression by 30˚ arthroscopy in lumbar spinal stenosis: Minimum
2-year follow-up. Clin Orthop Surg. 10:328–336. 2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Kim SK, Kang SS, Hong YH, Park SW and Lee
SC: Clinical comparison of unilateral biportal endoscopic technique
versus open microdiscectomy for single-level lumbar discectomy: A
multicenter, retrospective analysis. J Orthop Surg Res.
13(22)2018.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Heo DH, Ha JS, Lee DC, Kim HS and Chung
HJ: Repair of incidental durotomy using sutureless nonpenetrating
clips via biportal endoscopic surgery. Global Spine J. 12:452–457.
2022.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Kang MS, Chung HJ, Jung HJ and Park HJ:
How I do it? Extraforaminal lumbar interbody fusion assisted with
biportal endoscopic technique. Acta Neurochir. 163:295–299.
2021.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Kim JE, Choi DJ, Kim MC and Park EJ: Risk
factors of postoperative spinal epidural hematoma after biportal
endoscopic spinal surgery. World Neurosurg. 129:e324–e329.
2019.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Wang MC, Yu KY, Zhang JG and Wang YP:
Progression and clinical application in unilateral biportal
endoscopic. Zhonghua Wai Ke Za Zhi. 58:892–896. 2020.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|