Introduction
Osteoporotic vertebral compression fractures (OVCF)
predominantly occur in the elderly and cause pain, dysfunction,
loss of mobility, as well as a large economic burden (1). Annually, >1.4 million patients
worldwide are affected by OVCF (2). Percutaneous kyphoplasty (PKP) is
widely used to treat OVCF with good clinical results (3,4). The
purpose of OVCF treatment is to maximize pain control and
functional outcome. PKP not only provides rapid pain relief, but
also restores the height of fractured vertebra and corrects the
kyphosis caused by OVCF. Potential advantages of PKP over open
surgery include the minimally invasive procedure, low bleeding,
significant pain relief and faster return to daily life for
patients (5-7).
Several patients with OVCF experience degenerative
lumbar scoliosis, which is a risk factor for osteoporotic
fractures. In patients with OVCF accompanied by scoliosis, the
presence of spinal rotation makes it more difficult to puncture the
vertebral body, thereby increasing the risk of nerve injury during
the positioning of the needle (8,9).
There are two surgical approaches to PKP surgery,
including unilateral PKP and bilateral PKP, both of which have
equally good clinical and radiological outcomes in the treatment of
OVCF (10). However, bilateral PKP
results in improved distribution of bone cement and fracture
reduction compared with that achieved with unilateral PKP, whereas
unilateral PKP has advantages in decreasing the risk of adjacent
vertebral fractures (11-13).
There is no consensus regarding the optimal PKP approach, and to
the best of our knowledge, only a few clinical studies have
compared the effectiveness of both approaches in treating OVCF with
scoliosis (12). Therefore, the
present study aimed to assess the clinical and radiographic
outcomes of unilateral and bilateral PKP in treating OVCF with
scoliosis.
Materials and methods
General information
Data from patients with OVCF accompanied by
scoliosis who underwent PKP at The First Affiliated Hospital of
Soochow University (Suzhou, China) between January 2018 and
December 2020 were retrospectively analysed. Since the choice
between a unilateral or bilateral approach for treatment of
patients with OVCF and scoliosis has always been controversial,
prior to the present study, it was unclear which approach was more
suitable for these patients. The patients were informed about the
advantages and disadvantages of the two surgeries and the bilateral
or unilateral puncture approach was selected following the
patients' decision. According to the inclusion and exclusion
criteria, 52 patients were included in the present study, which was
approved by the Ethics Committee of The First Affiliated Hospital
of Soochow University. Informed written consent was obtained from
all patients. The patients were split into two groups: Unilateral
PKP group (n=26; mean age, 71.7±8.1 years) and bilateral PKP group
(n=26; mean age, 69.2±9.6 years). All patients were followed up for
at least one year with their consent. The preoperative,
intraoperative and postoperative information of these patients was
gathered via radiographic and medical records and routine
outpatient follow-ups.
Inclusion and exclusion criteria
Inclusion criteria were as follows: i) Patients aged
≥50 years with local tenderness, low back pain and lumbar
dysfunction; ii) T-score for bone mineral density (BMD) ≤-2.5,
compliant with the diagnostic criteria of osteoporosis (14); iii) radiograph showing a cobb angle
>10 degrees in the coronal plane, compliant with the diagnostic
criteria of scoliosis without neurological deficits or gross
instability (15); iv) MRI showing
a single-level vertebral body with a fresh vertebral compression
fracture; and v) data integrity of the patients during
preoperative, intraoperative and postoperative periods. Exclusion
criteria were as follows: i) Pathological fractures ascribed to
tuberculosis or tumour; ii) patients with mental illness, such as
depression or Alzheimer's disease; iii) presence of coronary heart
disease; iv) patients with long-term use of glucocorticoids for
treating rheumatic disease and v) abnormal coagulation.
Surgical procedure
The standard procedure of PKP was performed by
senior surgeons as described in a previous study (16). The patient was placed on an
operating table in the prone position. In the bilateral group,
according to the aforementioned surgical methods, symmetrical
incisions were made at 2-2.5 cm proximal to the apical spinous
process. A puncture needle was inserted at an abduction angle of
25-35 degrees into both sides of the vertebral body through the
pedicle with the guidance of a C-arm. Subsequently, a working
channel was established through a guidewire. An appropriate
inflatable balloon was inserted into the vertebral body, which was
inflated to provide space for cement injection into the compressed
vertebral body. OSTEOPAL®V bone cement was used in this
study. The formulation of the bone cement included the powder phase
and the liquid phase. The powder phase was composed of Poly (methyl
acrylate, methyl methacrylate), Zirconium dioxide, Benzoyl
peroxide. The liquid phase was composed of methyl methacrylate
(MMA); a peroxide decomposer, N,N-dimethyl-p-toluidine; and
hydroquinone. The formulation of the bone cement was most effective
when the ratio of powder to liquid was 2:1. The bone cement should
be of ‘tooth paste’ consistency prior to injection (17). High-viscosity cement was slowly
infused into the inflated vertebral body through the working
channel. In the unilateral group, only one incision was made, and
the puncture site was selected on the side with a clear pedicle
shadow under the C-arm fluoroscopy. Under anteroposterior
fluoroscopy, the tunnel was expanded to the anterior part of the
vertebral body using a dilator to reach the middle of the vertebral
body. The balloon was placed as deep as possible in the middle of
the vertebral body. Balloon dilation and bone cement injection were
performed in the same way as in the bilateral approach. After
surgery, all patients received >1 year anti-osteoporosis
treatment with 600 mg of supplemental calcium and 800 IU of vitamin
D daily. All patients received preoperative X-ray, MRI and CT to
identify the fracture segment and postoperative 1-day X-ray to
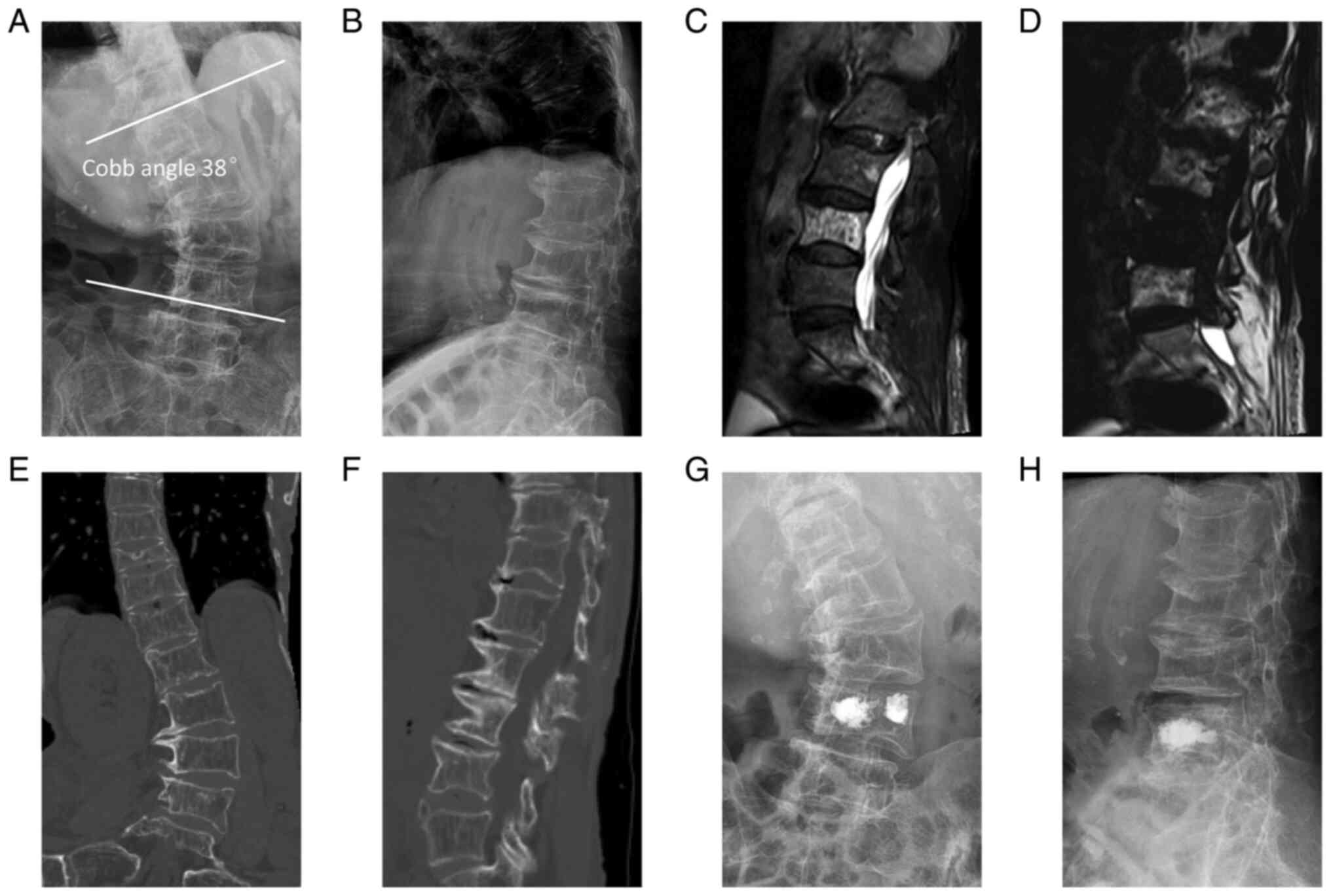
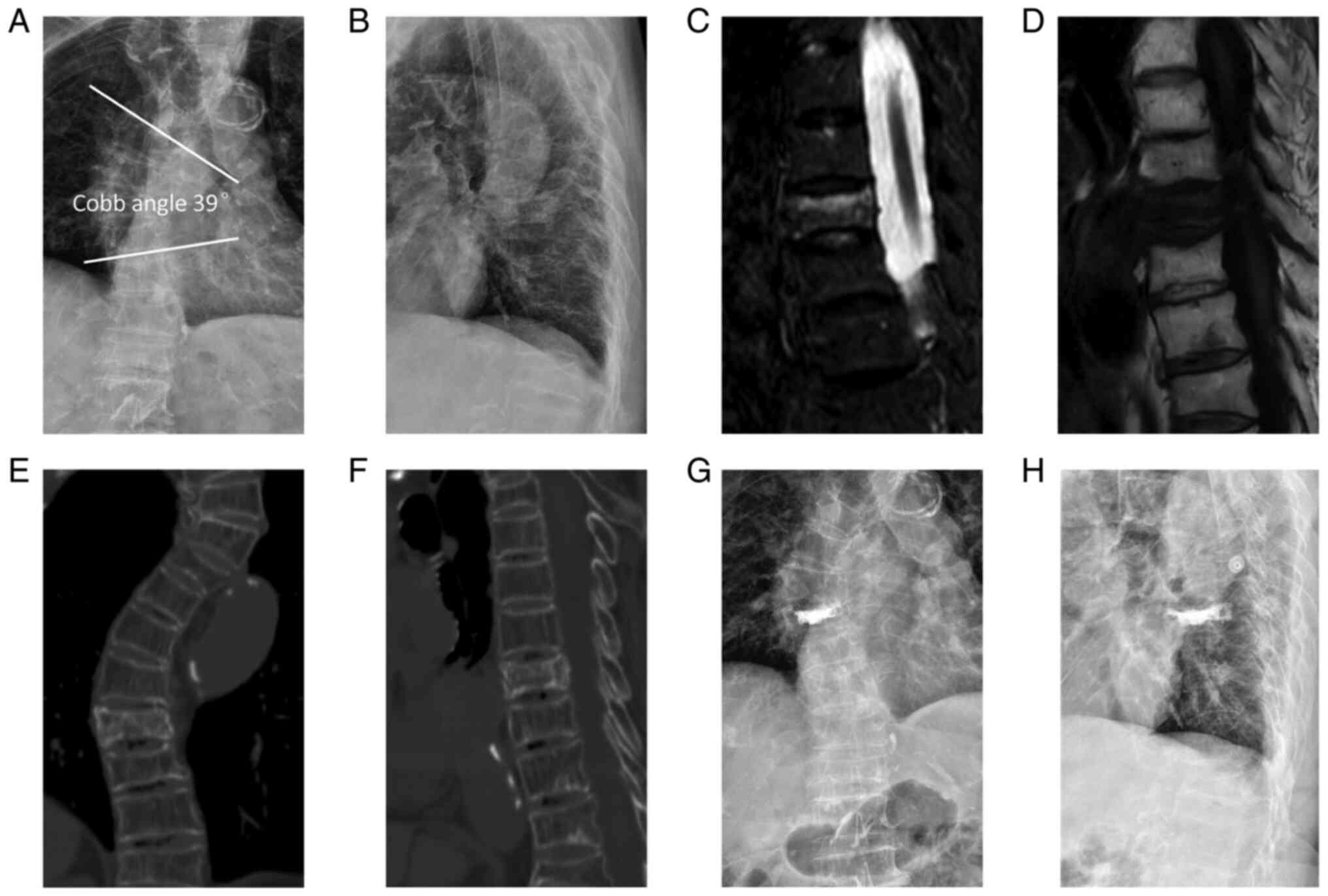
assess the outcome of treatment (Figs.
1 and 2).
Evaluation parameters
The operation time, bone cement injection volume,
intraoperative fluoroscopy frequency, duration of hospital stay and
apical vertebral rotation were recorded. Nash-Moe classification
ranged from 0 (both sides of the pedicles were symmetrical with no
vertebral rotation degree) to 4 (the most severe vertebral rotation
degree) and was used to reflect the vertebral rotation degree
(18). The vertebral body height
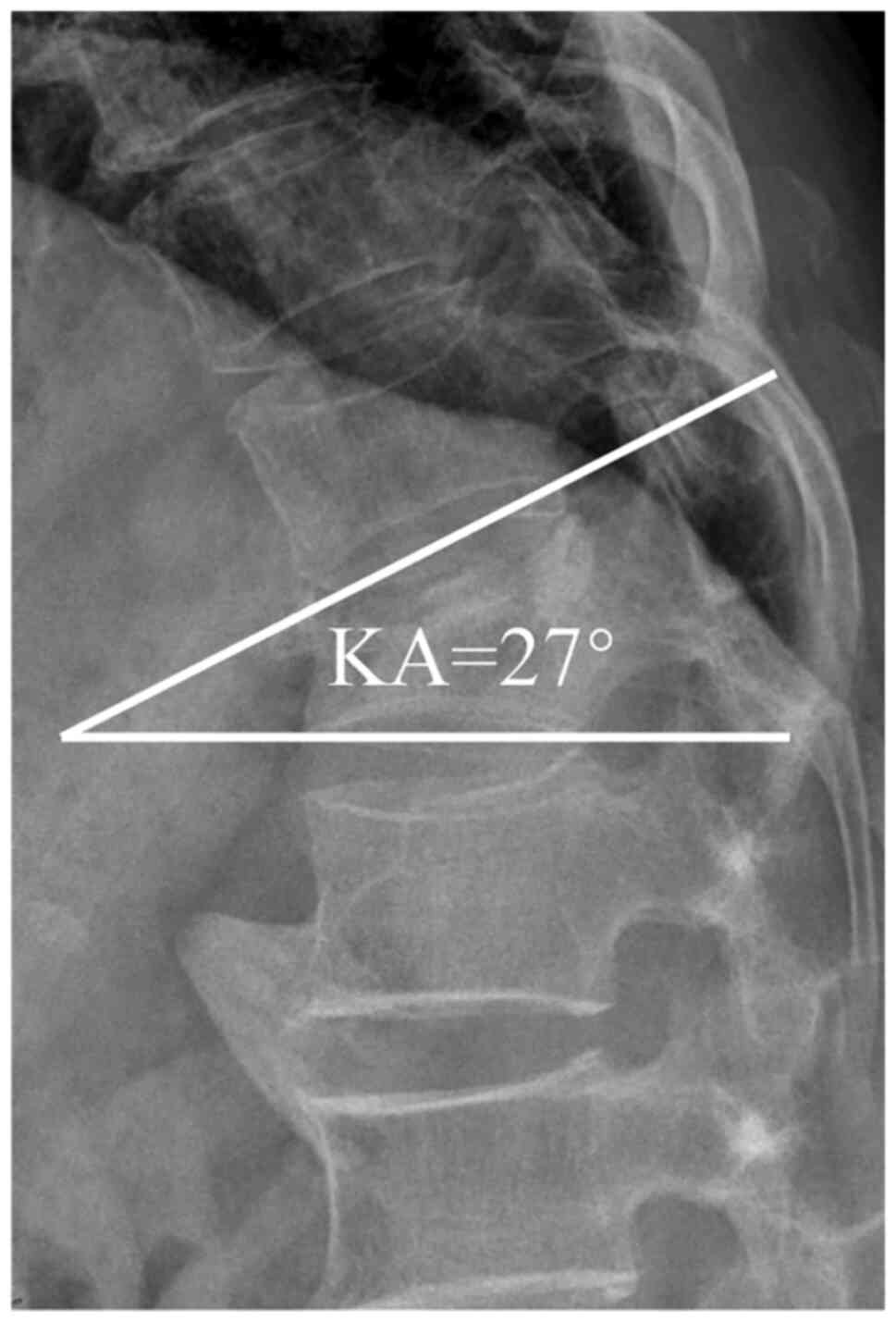
and local kyphotic angle (KA) were measured on a standing lateral
radiograph pre- and postoperatively. The fractured vertebral body
height was measured at the point of most pronounced compression
(anterior or middle). The KA was calculated from the angle of
intersection of the lines parallel to the upper and lower end
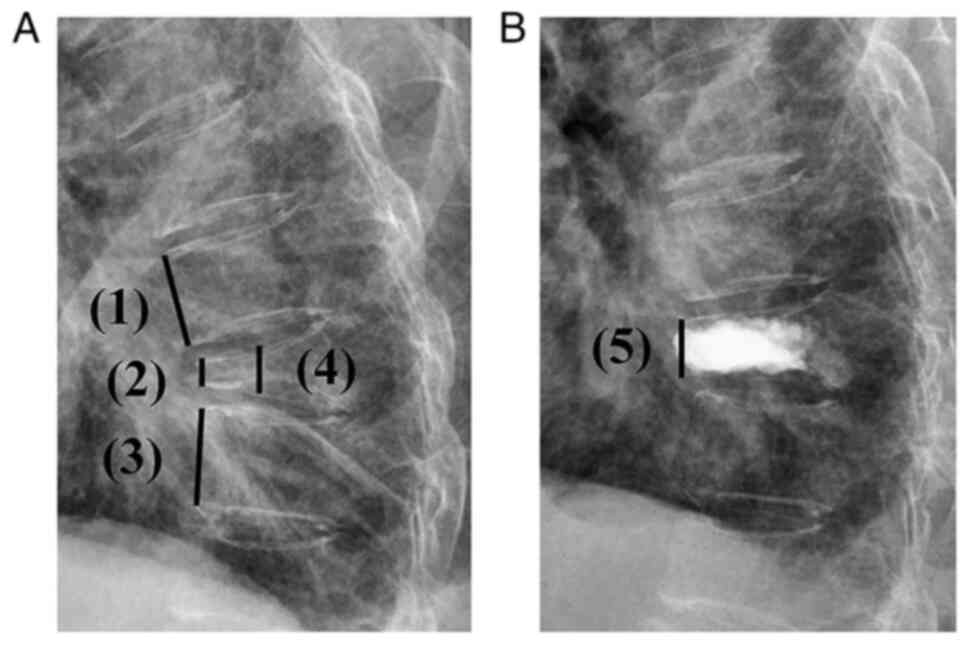
plates of the fractured vertebrae (Fig. 3). The compression rate (CR) was
calculated as the height of each fractured vertebral body divided
by the height of the neighbouring normal vertebral body.
Postoperatively, the restoration rate (RR) was calculated as
follows: (Restored vertebral body height-original fractured
vertebral body height)/adjacent normal vertebral body height
(Fig. 4) (19). The visual analogue scale (VAS) and
Oswestry disability index (ODI) scores were evaluated
preoperatively and postoperatively. VAS ranged from 0 (no pain) to
10 (the worst pain experienced) and was used for measuring back
pain. Daily life function was estimated using the ODI score
(20). The ODI score system
includes 10 sections: Pain intensity, personal care, lifting,
walking, sitting, standing, sleeping, sexual life, social life and
traveling. Each section consists of six statements with a score of
0-5. The score is calculated as follows: (Total score/5x number of
questions answered) x100% (21).
Calculation of the VAS and ODI was described in a previous study
(22). The occurrence rates of the
adjacent vertebral body fractures and bone cement leakage were
calculated postoperatively at follow-up.
Statistical analysis
Statistical analysis was performed using SPSS
(version 25.0; IBM Corp.). Independent sample Student's t-test was
used to compare the age, BMD T-score, intraoperative data, CR and
RR between the two groups. A mixed ANOVA followed by Bonferroni
correction was used for comparing KA and average vertebral height
between the two groups at different time points and within the same
group pre- and postoperatively. The Mann-Whitney U test was used to
compare VAS and ODI scores between the two groups, while the
Wilcoxon signed-rank test was used to compare the preoperative and
postoperative VAS and ODI scores of the same group, and each test
was followed by Bonferroni correction. The variables of Nash-Moe
grade and adjacent vertebral fracture were analysed by Fisher's
exact test, while the remaining variables of sex, fracture
location, scoliosis direction and cement leakage rate were analysed
using the Chi-square test. The parametric numerical data are
presented as mean ± standard deviation, the non-parametric ordinal
data are presented as the median (interquartile range), and the
count data are shown as n (%). P<0.05 was considered to indicate
a statistically significant difference.
Results
Comparison of general data
The mean BMD T-score was -2.9±0.3 in the unilateral
group and -3.0±0.4 in the bilateral group. In the unilateral group,
12 patients had single thoracic fractures whereas 14 patients had
single lumbar fractures. In the bilateral group, 10 patients had
single thoracic fractures whereas 16 patients had single lumbar
fractures. There were no significant differences between the two
groups in terms of BMD and fracture location. An apical vertebral
rotation was present in 76.9% (20/26) of the patients in the
unilateral group and 65.3% (17/26) of the patients in the bilateral
group, with no significant difference between the two groups. The
direction of scoliosis also showed no significant difference
between the two groups (P>0.05) (Table I).
 | Table IBaseline characteristics of the two
groups. |
Table I
Baseline characteristics of the two
groups.
| Characteristic | Unilateral group
(n=26) | Bilateral group
(n=26) | P-value |
|---|
| Sex, n | | | 0.548 |
|
Male | 7 | 9 | |
|
Female | 19 | 17 | |
| Age, years | 71.7±8.1 | 69.2±9.6 | 0.324 |
| BMD T-score | -2.9±0.3 | -3.0±0.4 | 0.223 |
| Follow-up,
months | 13.5±1.6 | 13.5±1.9 | 0.938 |
| Fracture location,
n | | | 0.575 |
|
Thoracic | 12 | 10 | |
|
Lumbar | 14 | 16 | |
| Scoliosis direction,
n | | | 0.165 |
|
Right | 16 | 11 | |
|
Left | 10 | 15 | |
| Apical vertebral
rotation (Nash-Moe grade), n | | | 0.697 |
|
0 | 6 | 9 | |
|
1 | 17 | 15 | |
|
2 | 3 | 2 | |
Comparison of intraoperative data and
assessment of VAS and ODI scores
The operation time in the unilateral group was
shorter than that in the bilateral group (40.5±9.0 vs. 57.2±11.4
min; P<0.001). In addition, the injected cement volume was
significantly lower in the unilateral group than that in the
bilateral group (4.7±0.9 vs. 7.7±1.2 ml; P<0.001). Furthermore,
the frequency of intraoperative fluoroscopy was lower in the
unilateral group than that in the bilateral group (28.3±7.4 vs.
52.6±9.6 times; P<0.001). Regarding the duration of hospital
stay, there was no significant difference between the two groups
(P>0.05). The VAS and ODI scores at 1-day after surgery and
final follow-up improved significantly compared with those before
surgery in both groups (P<0.05). However, these scores did not
vary significantly between the two groups both before and after
surgery (P>0.05; Table
II).
 | Table IIComparisons of intraoperative data,
VAS score and ODI between the two groups. |
Table II
Comparisons of intraoperative data,
VAS score and ODI between the two groups.
| Characteristic | Unilateral group
(n=26) | Bilateral group
(n=26) | P-value |
|---|
| Operation time,
min | 40.5±9.0 | 57.2±11.4 | <0.001 |
| Intraoperative
fluoroscopy frequency, times | 28.3±7.4 | 52.6±9.6 | <0.001 |
| Injected cement
volume, ml | 4.7±0.9 | 7.7±1.2 | <0.001 |
| Hospital stay,
days | 4.9±1.3 | 5.0±1.5 | 0.844 |
| VAS score
(interquartile range) | | | |
|
Preoperative | 7 (6-8) | 7 (7-9) | 0.291 |
|
1-day
postoperative | 3
(3-4)a | 3
(3-4)a | 0.663 |
|
Final
follow-up | 2
(1-3)a | 2
(2-2)a | 0.648 |
| ODI, %
(interquartile range) | | | |
|
Preoperative | 58 (52-65) | 57 (51-66) | 0.993 |
|
1-day
postoperative | 30
(25-33)a | 30
(26-33)a | 0.971 |
|
Final
follow-up | 20
(19-23)a | 20
(17-24)a | 0.650 |
Comparison of radiographic data and
postoperative complications
The CR of the vertebral body before surgery was not
significantly different between the two groups (P>0.05). The
average vertebral body height and KA significantly improved after
surgery in both groups compared with the preoperative measurements
(P<0.05). However, after surgery, RR and KA were not
statistically significant between the two groups (P>0.05).
During a mean follow-up of 13.5 months (range, 12-16 months) after
surgery, the unilateral group included three cases (11.5%) with
bone cement leakage, whereas the bilateral group included nine
cases (34.6%) (P<0.05). In patients with bone cement leakage,
neither clinical nor neurological signs were observed. In the
unilateral group, three of 26 (11.5%) patients exhibited adjacent
vertebral fractures, the first patient at 1 month, the second at 6
months and the third at 12 months postoperatively. In the bilateral
group, two of 26 (7.7%) patients exhibited adjacent vertebral
fractures, one patient at 8 months and the other at 14 months
postoperatively. The incidence of adjacent vertebral fractures did
not vary significantly between the two groups (Table III). Preoperative X-ray, MRI and
CT images of the typical cases of the both groups showed a
single-level vertebral body with a fresh vertebral compression
fracture in a patient with scoliosis. Postoperative 1-day X-ray
showed even distribution of bone cement and partial recovery of the
vertebral height and kyphotic angle (Figs. 1, 2).
 | Table IIIComparisons of radiographic data and
postoperative complications between the two groups. |
Table III
Comparisons of radiographic data and
postoperative complications between the two groups.
| Characteristic | Unilateral group
(n=26) | Bilateral group
(n=26) | P-value |
|---|
| Average vertebral
height, mm | | | |
|
Preoperative | 17.7±3.3 | 17.6±3.4 | 0.981 |
|
1-day
postoperative |
23.2±3.9a |
24.8±3.2a | 0.113 |
|
Final
follow-up |
22.3±3.8a |
24.1±3.2a | 0.072 |
| Kyphotic angle,
degrees | | | |
|
Preoperative | 15.5±5.5 | 13.8±4.5 | 0.229 |
|
1-day
postoperative |
8.2±4.3a |
6.7±2.9a | 0.146 |
|
Final
follow-up |
8.9±4.4a |
7.4±2.6a | 0.129 |
| Compression rate,
% | 36.6±8.0 | 35.3±11.0 | 0.637 |
| Restoration rate,
% | 21.9±6.4 | 26.1±13.0 | 0.146 |
| Cement leakage
rate, n (%) | 3 (11.5) | 9 (34.6) | 0.048 |
| Adjacent vertebral
fracture, n (%) | 3 (11.5) | 2 (7.7) | 1.000 |
Discussion
OVCF associated with scoliosis is common in clinical
practice, but its treatment is still challenging. PKP is considered
to be an effective treatment for OVCF associated with scoliosis
(23). However, unclear pedicle
projection leads to higher risk of puncture injury when performing
PKP for treating OVCF associated with scoliosis. Bilateral PKP is
considered the universal approach for the management of OVCF by
injecting cement via both pedicles, and one important advantage of
this approach is the good distribution of bone cement (19,24).
By contrast, bilateral PKP has certain shortcomings, such as higher
frequency of intraoperative fluoroscopy and risk of cement leakage
(25). Compared with that in
bilateral PKP, unilateral PKP is associated with reduced operation
time and risk of puncture, but the disadvantage of uneven
distribution of bone cement may lead to vertebral refracture. It is
still controversial which surgical approach is more advantageous
for OVCF with scoliosis (10,26).
The present study compared the clinical efficacy and
safety of unilateral and bilateral PKP in treating patients with
OVCF accompanied by scoliosis. The current results indicated that
both unilateral and bilateral PKP had the same efficacy in
restoring vertebral body height and correcting KA. The VAS and ODI
scores improved postoperatively in both groups, but the differences
between the two groups were not statistically significant. Lee
et al (27) reported that
unilateral PKP is equally successful with bilateral PKP in terms of
pain relief and restoration of the vertebra when treating
single-level OVCF. A cadaver study also showed that bilateral and
unilateral PKP are equally effective in restoring vertebral body
strength, stiffness and height (12). Consistently, the results of the
present study showed that for treating OVCF accompanied by
scoliosis, unilateral PKP could achieve the same effect in
relieving clinical symptoms compared with that achieved by
bilateral PKP.
Bone cement leakage is one of the common
complications in PKP and it is affected by the injected cement
volume, fracture severity grade and puncture accuracy (28). The current study found that the
incidence of bone cement leakage in the unilateral group was lower
than that in the bilateral group. This finding may be attributed to
the fact that in OVCF with scoliosis, level of deformity increases
the difficulty of performing the standard intraoperative
fluoroscopy, which elevates the risk of cement leakage when
surgeons puncture through the bilateral pedicles. Moreover, the
mean amount of injection volume in the bilateral group was higher
than that in the unilateral group. Li et al (29) reported that an increase in the
injection volume of polymethyl methacrylate could increase the
probability of cement leakage in PKP. Additionally, the current
study showed that the operation duration in the unilateral group
was shorter than that in the bilateral group, which was similar to
the results of previous studies (11,30).
The present study also found that unilateral PKP could decrease the
intraoperative fluoroscopy frequency compared with that of the
bilateral PKP in the treatment of OVCF accompanied by scoliosis.
Consistently, Yan et al (30) reported that bilateral PKP used
twice the average radiation dosage per patient that was used for
unilateral PKP. In brief, unilateral PKP shortened the operation
time, and decreased the intraoperative fluoroscopy frequency and
bone cement leakage compared with those in bilateral PKP used for
the management of OVCF with scoliosis.
At present, the occurrence of adjacent vertebral
fractures after PKP is gaining significant attention from
researchers. Yu et al (31), in their meta-analysis study, showed
that the incidence of adjacent vertebral fractures after PKP is
3.21-63.00%. Among several risk factors for postoperative adjacent
vertebral fractures, a combination of degenerative lateral bending
is an independent risk factor (32). However, when comparing the
incidence of adjacent vertebral fractures after PKP between the
bilateral and unilateral PKP groups, the present study found that
the difference was not significant. Similarly, certain studies
reported no statistically significant difference between the
unilateral and bilateral PKP groups in terms of the risk ratio of
postoperative adjacent segment fractures (12,27).
The findings of the current retrospective analysis provided
evidence that unilateral PKP may be a preferable option for
treating OVCF with scoliosis and provided a direction for future
research on OVCF combined with scoliosis.
However, the present study had some limitations.
Firstly, the sample size was small because of the strict inclusion
and exclusion criteria. A larger sample size would have helped in
drawing more accurate conclusions. Secondly, the surgeries were not
performed by the same surgeon, although all surgeons had vast
experience in performing this type of surgery. Thirdly, this was a
retrospective study, and it could be affected by selection bias.
Future prospective studies must be conducted to limit the
possibility of selection bias. Therefore, a large, prospective,
randomized control study is warranted to further validate the
present results.
Unilateral PKP was as effective as bilateral PKP in
the treatment of OVCF accompanied by scoliosis. Both procedures
could relieve acute back pain, improve the compressed vertebral
body height and correct the KA. Nevertheless, compared with those
in the bilateral PKP, unilateral PKP could reduce the
intraoperative fluoroscopy and shorten the operation time.
Furthermore, unilateral PKP exerted lower rates of bone cement
leakage and it did not increase the risk of adjacent vertebral
fractures. Altogether, unilateral PKP could be a preferable option
compared with the bilateral PKP in the management of OVCF
associated with scoliosis.
Acknowledgements
Not applicable.
Funding
Funding: This study was supported by the National Nature Science
Foundation of China (grant no. 82272542), the Natural Science
Foundation of Jiangsu Province (grant no. BK 20220095) and Suzhou
Gusu Health Talent Plan talent research project (grant no.
GSWS2022009).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
KC, KZ and JZo designed the study. ZL wrote the
manuscript, collected patient information and interpreted data.
HanL and YT contributed to the clinical and radiological
evaluations. JZh performed the statistical analysis and collected
patient information. HaoL interpreted data and revised the article.
KC and KZ confirm the authenticity of all the raw data. All authors
have read and approved the final manuscript.
Ethics approval and consent to
participate
All procedures involving human participants were
performed in accordance with the Ethical Standards of the present
institute's research committee and the 1964 Helsinki Declaration
and its later amendments. The present study was approved by the
Ethics Committee of the First Affiliated Hospital of Soochow
University (approval no. 137; Suzhou, China). All patients signed
the informed consent form about inclusion in the present study at
the time of follow-up and the usual preoperative consent form prior
to surgery.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ballane G, Cauley JA, Luckey MM and
Fuleihan GEHS: Worldwide prevalence and incidence of osteoporotic
vertebral fractures. Osteoporos Int. 28:1531–1542. 2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Griffith JF: Identifying osteoporotic
vertebral fracture. Quant Imaging Med Surg. 5:592–602.
2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Buchbinder R, Johnston RV, Rischin KJ,
Homik J, Jones CA, Golmohammadi K and Kallmes DF: Percutaneous
vertebroplasty for osteoporotic vertebral compression fracture.
Cochrane Database Syst Rev. 11(CD006349)2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Cao Z, Wang G, Hui W, Liu B, Liu Z and Sun
J: Percutaneous kyphoplasty for osteoporotic vertebral compression
fractures improves spino-pelvic alignment and global sagittal
balance maximally in the thoracolumbar region. PLoS One.
15(e0228341)2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Kim DH and Vaccaro AR: Osteoporotic
compression fractures of the spine; current options and
considerations for treatment. Spine J. 6:479–487. 2006.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Robinson Y, Heyde CE, Försth P and Olerud
C: Kyphoplasty in osteoporotic vertebral compression
fractures-guidelines and technical considerations. J Orthop Surg
Res. 6(43)2011.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Jang HD, Kim EH, Lee JC, Choi SW, Kim HS,
Cha JS and Shin BJ: Management of osteoporotic vertebral fracture:
Review update 2022. Asian Spine J. 16:934–946. 2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Healey JH and Lane JM: Structural
scoliosis in osteoporotic women. Clin Orthop Relat Res.
195:216–223. 1985.PubMed/NCBI
|
|
9
|
Sabo A, Hatgis J, Granville M and Jacobson
RE: Multilevel contiguous osteoporotic lumbar compression
fractures: The relationship of scoliosis to the development of
cascading fractures. Cureus. 9(e1962)2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Chen X, Guo W, Li Q, Ou Z, Lao Z, Liu Y,
Zhu C, Han Z, Chu X and Cai D: Is unilateral percutaneous
kyphoplasty superior to bilateral percutaneous kyphoplasty for
osteoporotic vertebral compression fractures? Evidence from a
systematic review of discordant meta-analyses. Pain Physician.
21:327–336. 2018.PubMed/NCBI
|
|
11
|
Chen L, Yang H and Tang T: Unilateral
versus bilateral balloon kyphoplasty for multilevel osteoporotic
vertebral compression fractures: A prospective study. Spine (Phila
Pa 1976). 36:534–540. 2011.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Cheng X, Long HQ, Xu JH, Huang YL and Li
FB: Comparison of unilateral versus bilateral percutaneous
kyphoplasty for the treatment of patients with osteoporosis
vertebral compression fracture (OVCF): A systematic review and
meta-analysis. Eur Spine J. 25:3439–3449. 2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Lotan R, Haimovich Y, Schorr L, Goldstein
AL and Hershkovich O: Double-balloon kyphoplasty results in better
radiographic outcomes than a single-balloon kyphoplasty in treating
osteo-porotic spinal fractures. J Clin Med. 11(3407)2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Lane NE: Epidemiology, etiology, and
diagnosis of osteoporosis. Am J Obstet Gynecol. 194:S3–S11.
2006.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Aebi M: The adult scoliosis. Eur Spine J.
14:925–948. 2005.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Wang G, Yang H and Chen K: Osteoporotic
vertebral compression fractures with an intravertebral cleft
treated by percutaneous balloon kyphoplasty. J Bone Joint Surg Br.
92:1553–1557. 2010.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Marlin E, Nathoo N and Mendel E: Use of
percutaneous kyphoplasty and vertebroplasty in spinal surgery. J
Neurosurg Sci. 56:105–112. 2012.PubMed/NCBI
|
|
18
|
Marawar SV, Ordway NR, Auston DA, Kurra S,
Wang D, Simpson VM, Tallarico RA, Katz DA, Palomino K, Palumbo M
and Lavelle WF: Assessment of inter- and intraobserver reliability
and accuracy to evaluate apical vertebral rotation using four
methods: An experimental study using a saw bone model. Spine
Deform. 7:11–17. 2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Chen C, Chen L, Gu Y, Xu Y, Liu Y, Bai X,
Zhu X and Yang H: Kyphoplasty for chronic painful osteoporotic
vertebral compression fractures via unipedicular versus bipedicular
approachment: A comparative study in early stage. Injury.
41:356–359. 2010.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Reed MD and Van Nostran W: Assessing pain
intensity with thevisual analog scale: A plea for uniformity. J
Clin Pharmacol. 54:241–244. 2014.PubMed/NCBI View
Article : Google Scholar
|
|
21
|
Fairbank JC and Pynsent PB: The oswestry
disability index. Spine (Phila Pa 1976). 25:2940–2952.
2000.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Pan M, Ge J, Li Q, Li S, Mao H, Meng B and
Yang H: Percutaneous vertebral augmentation in special Genant IV
osteoporotic vertebral compression fractures. J Orthop Translat.
20:94–99. 2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Wang H, Sribastav SS, Ye F, Yang C, Wang
J, Liu H and Zheng Z: Comparison of percutaneous vertebroplasty and
balloon kyphoplasty for the treatment of single level vertebral
compression fractures: A meta-analysis of the literature. Pain
Physician. 18:209–222. 2015.PubMed/NCBI
|
|
24
|
Liu MX, Xia L, Zhong J, Dou NN and Li B:
Is it necessary to approach the compressed vertebra bilaterally
during the process of PKP? J Spinal Cord Med. 43:201–205.
2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Tan B, Yang QY, Fan B, Lei C and Hu ZM: Is
it necessary to approach the severe osteoporotic vertebral
biconcave-shaped fracture bilaterally during the process of PKP? J
Pain Res. 14:1601–1610. 2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Zhang F, Zhao QM, Ni XH, Wang LJ, Ma ZG,
Kang P, Liu XD and Yin S: Comparison of unilateral and bilateral
puncture percutaneous kyphoplasty in the treatment of osteoporotic
vertebral compression fractures. Neurosciences (Riyadh).
26:236–241. 2021.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Lee CH, Kim HJ, Lee MK, Kim HS and Choi
SS: Comparison of efficacies of unipedicular kyphoplasty and
bipedicular kyphoplasty for treatment of single-level osteoporotic
vertebral compression fractures: A STROBE-compliant retrospective
study. Medicine (Baltimore). 99(e22046)2020.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Pang J, Liu B, Chen H, Zhang W, Sun J and
Zhang X: Precise puncture combined with simplified percutaneous
vertebroplasty to treat osteoporotic vertebral compression
fractures: A comparative analysis with conventional percutaneous
vertebroplasty. Am J Transl Res. 13:14195–14202. 2021.PubMed/NCBI
|
|
29
|
Li Z, Xu Y, Xu W, Zhu X and Chen Y: The
correlation between the diffusion coefficient of bone cement and
efficacy in percutaneous vertebroplasty. Orthopedics. 44:e95–e100.
2021.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Yan L, Jiang R, He B, Liu T and Hao D: A
comparison between unilateral transverse process-pedicle and
bilateral puncture techniques in percutaneous kyphoplasty. Spine
(Phila Pa 1976). 39:B19–B26. 2014.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Yu W, Xu W, Jiang X, Liang D and Jian W:
Risk factors for recollapse of the augmented vertebrae after
percutaneous vertebral augmentation: A systematic review and
meta-analysis. World Neurosurg. 111:119–129. 2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Castelein RM, Pasha S, Cheng JC and
Dubousset J: Idiopathic scoliosis as a rotatory decompensation of
the spine. J Bone Miner Res. 35:1850–1857. 2020.PubMed/NCBI View Article : Google Scholar
|