Introduction
With the increasing prevalence of cardiovascular
disease, coronary artery disease (CAD) has become a leading cause
of premature morbidity and mortality worldwide (1). The diagnosis and treatment of
coronary heart disease have become increasingly important. Amongst
them, the assessment of plaque burden, degree of stenosis, and the
resulting consequences of coronary arteries is crucial, as they are
closely related to the risk of a cardiovascular event in patients
(1). Single photon emission
computed tomography (SPECT) myocardial perfusion imaging (MPI) is
an important non-invasive imaging tool widely applied to the
diagnosis, risk stratification, prognosis, and outcome assessment
of CAD (2,3). Conventional SPECT MPI is typically
used to diagnose CAD by visual assessment and/or semi-quantitative
analysis (4), including summed
stress score (SS), summed rest score (RS), and summed different
score (DS; DS=SS-RS), to evaluate whether myocardial ischemia
exists and the severity of myocardial ischemia (5). However, the accuracy of assessing the
extent and severity of myocardial ischemia requires improvement
(6). Positron emission tomography
and CT (PET/CT) allow for quantitative myocardial blood flow (MBF)
measurement, determination of the coronary flow reserve (CFR), and
the ratio between hyperemic and baseline coronary flow, markedly
improving the diagnosis of myocardial ischemia (6,7).
PET/CT is therefore considered the gold standard for the
non-invasive determination of both MBF and CFR (8). Nevertheless, PET/CT remains
infrequently used in routine clinical practice, primarily due to
the high cost of equipment and limited availability of
radiopharmaceuticals.
In recent years, the emergence of the novel
cardiac-specific cadmium-zinc-telluride SPECT (CZT-SPECT) method
has significantly improved the performance of SPECT devices
(9,10). It has been widely adopted worldwide
in clinical practice due to its optimal sensitivity and spatial
resolution, as well as its fast temporal resolution
characteristics. CZT-SPECT enables fast and dynamic tomographic
imaging for quantitative measurement of MBF (11). Furthermore, the CZT-SPECT
measurements exhibit consistency with the gold standard (12,13)
in diagnosing myocardial ischemia through quantitative blood flow
assessment from PET, as well as with the results regarding coronary
stenosis obtained from coronary angiography (CAG) (14).
As the literature on clinical applications related
to MPI and CFR measurement by CZT-SPECT remains limited, the
present study was designed to investigate the relationship between
parameters obtained from CZT-SPECT and the level of coronary
stenosis.
Patients and methods
Study population
The clinical data of 98 consecutive patients with
suspected or confirmed stable CAD who successfully completed
resting-load MPI and CFR measurements by CZT-SPECT at The First
Affiliated Hospital of Nanjing Medical University (Nanjing, China)
between March 2022 and September 2022 were retrospectively
collected. Participants aged ≥18 years old who had a history of CAG
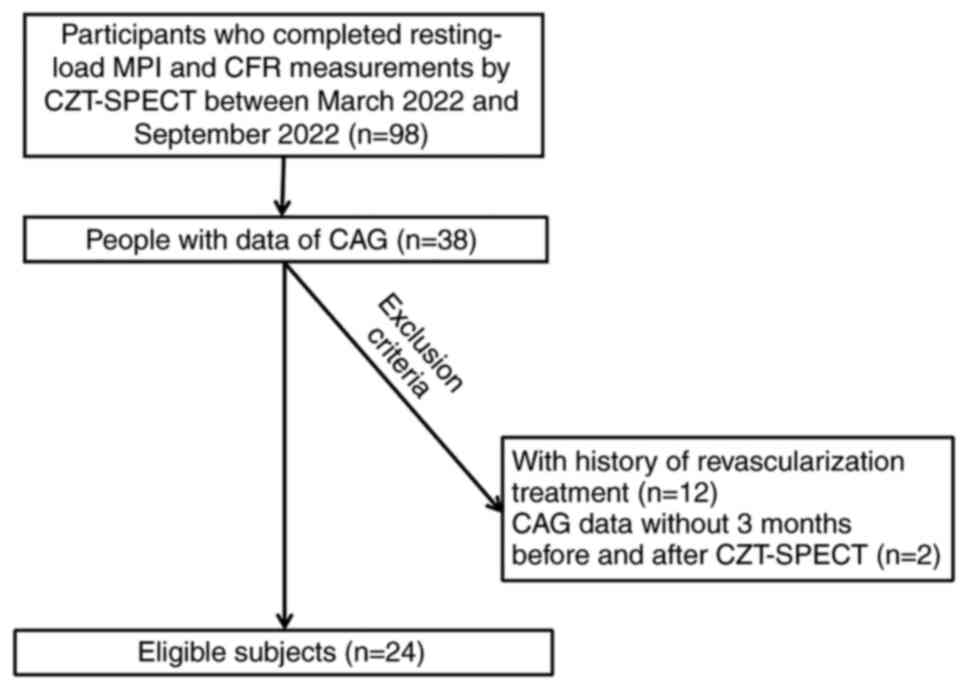
assessment were included in the study (n=38). The flowchart of
patient inclusion is shown in Fig.
1. Further exclusions were made for those patients who had a
history of revascularization treatment (n=12) and for those who did
not undergo CAG assessment 3 months before or after CZT-SPECT
(n=2). After exclusions were made, 24 patients (median age: 65
years; range: 46-79 years) were eligible for inclusion in the
study. The present study was approved by The Ethics Committee of
People's Hospital of Jiangsu Province (The First Affiliated
Hospital of Nanjing Medical University), and all patients signed an
informed consent form (approval no. 2022-SR-748).
Clinical data
The clinicopathological characteristics were
collected from the hospital's electronic medical record system.
This information included sex, age, body mass index, past medical
history, smoking history, alcohol consumption history, clinical
symptoms, and admission blood pressure. The 10-year cardiovascular
score was also calculated. Laboratory examination results included
total cholesterol, triglycerides, low-density lipoprotein,
high-density lipoprotein, and the systolic blood and diastolic
blood pressure of the patients. The CAG results were used as the
gold standard reference for coronary stenosis.
CZT-SPECT examination
The imaging device used was a cardiac-dedicated
SPECT (D-SPECT; Spectrum Dynamics Medical Company) equipped with a
CZT detector, and the radionuclide imaging agent used was
99Tc-methoxy isobutyl isonitrile (Nanjing Senke
Pharmaceutical Co., Ltd). Routine preparation of patients for
imaging involved: Discontinued administration of cardiovascular
drugs (dihydropyridine calcium antagonists and β-blockers for ≥24
h, and nitrates for ≥6 h); fasting from caffeinated beverages, tea,
food, and other medications for ≥24 h; and discontinued
administration of methylxanthines for ≥36 h prior to examination.
The patients consumed 300 ml water before the examination (for
patients with heart failure or poor diet, the water intake was
reduced or eliminated and the acquisition was delayed depending on
the image quality). A ‘single-day’ protocol of image acquisition
(load after rest in the same day) or a ‘two-day’ protocol (rest on
day 1 and load on day 2) was used. The types of imaging included:
i) Rest imaging-patients were instructed to consume high-fat meals,
and 40-60 min after the meal, routine resting gated tomography was
performed and images were acquired for 6 min; and ii) stress
imaging-at the end of rest imaging, patients had a 1-4 h interval
and they were injected with ATP using an intravenous pump at 0.16
mg/kg.min for 5 min. Meanwhile, the dynamic acquisition was
initiated at the peak of loading in the 3rd min, followed by rapid
injection of 1,110 MBq imaging agent through a pre-buried
intravenous channel for 10-15 sec, and images were acquired in list
mode for 6 min. During the whole process, a 12-lead ECG was
monitored in real-time. Routine stress-gated tomography was also
performed 15-30 min after the end of the stress dynamic
acquisition. A total of 5 ml Regadenoson (Nanjing Hailong
Pharmaceutical Technology Co., Ltd.) was rapidly injected (10 sec)
through a pre-built intravenous channel during the stress test, and
dynamic acquisition mode was initiated 20-30 sec later.
Image processing
The MPI images and CFR were interpreted by two
experienced nuclear medicine physicians in consultation. In case of
disagreement, a third physician was consulted and provided the
final decision. Quantitative parameters, including regional CFR,
were automatically analyzed by image processing software
(quantitative perfusion SPECT; Cedars-Sinai Medical Center; version
2017). A 17-region model and a 5-point scale of perfusion image
were used to evaluate myocardial ischemia as routine (5). The 17 segments were grouped into
territories of the three main coronary arteries to match the
results of the CAG, including the circumflex artery (LCX), the left
anterior descending artery (LAD), and the right coronary artery
(RCA). The scores of the regional segments in the stress and rest
images were added to create the regional semi-quantitative
parameters known as the regional SS, RS, and DS.
Evaluation of CAG
CAG was performed using the standard Judkins method
(15), and stenosis of coronary
arteries was visually assessed by two intervention-experienced
cardiologists in collaboration. The stenosis was calculated at the
most severe point, and the degree of stenosis of the left main stem
was considered as stenosis of both the LAD and LCX. According to
the results of CAG, the coronary arteries were divided into two
groups: i) The negative group with stenosis <50%; and ii) the
positive group with stenosis ≥50%. In addition to this, a second
approach to grouping based on a stenosis criterion of 75% was
implemented.
Statistical analysis
Descriptive statistics were used to summarize the
baseline data, including percentages for categorical data, means
and standard deviations for normally distributed continuous data,
and medians and interquartile range for skewed data. A Student's
t-test was used for comparisons between the positive stenosis group
and the control group.
The factors related to the degree of coronary
stenosis at the vascular level were primarily investigated and the
sensitivity, specificity, positive predictive value, negative
predictive value, and accuracy of DS, CFR, and DS combined with CFR
for the diagnosis of positive coronary stenosis under the two
stenosis criteria (50 and 75%) were calculated. The receiver
operating characteristic (ROC) curves of the predictive value of
DS, CFR, and the combination thereof for coronary stenosis were
plotted separately, to assess the discriminative ability of the
parameters. The diagnostic efficacy was also calculated based on
the optimal cut-off value.
To further compare the predictive ability of
semi-quantitative and quantitative parameters (continuous variable)
on the degree of coronary stenosis (dichotomous variable), net
reclassification improvement (NRI) and integrated discrimination
index (IDI) were calculated (16).
All data management and statistical analyses were conducted in R,
version 4.1.2 (https://www.r-project.org/). P<0.05 was considered
to indicate a statistically significant difference.
Results
Characteristics of the study
population
A total of 24 patients, aged 46-79 years old,
including 19 males and 5 females, with a history of hypertension in
19 patients (79.2%), diabetes mellitus in 8 patients (33.3%),
stroke in 1 patient (4.2%), smoking in 11 patients (45.8),
alcoholism in 3 patients (12.5%), angina in 13 patients (54.2%) and
chest tightness in 18 patients (75.0%), were included in the
present study, as shown in Table
I. The 10-year atherosclerotic cardiovascular disease score
ranged from 4.9 to 10.34. Of the total 72 major vessels of all the
included patients, 34 (47.2%) had stenosis ≥50%, and 16 (22.2%) had
stenosis ≥75%. A total of 57 vessel supply regions had a normal RS
and 15 were abnormal; 41 regions had a normal SS and 31 were
abnormal; DS was present in 27 regions and 45 regions had no change
in resting load score.
 | Table IClinicopathological characteristics of
the patients. |
Table I
Clinicopathological characteristics of
the patients.
| Variable | Value |
|---|
| Agea, years | 65, (46-79) |
| Maleb | 19 (79.2) |
| Body mass index,
kg/m2c | 24.75±3.94 |
|
Hypertensionb | 19 (79.2) |
| Diabetes
mellitusb | 8 (33.3) |
| Strokeb | 1 (4.2) |
| Smokeb | 11 (45.8) |
| Consumed
alcoholb | 3 (12.5) |
| Anginab | 13 (54.2) |
| Chest
tightnessb | 18 (75.0) |
| 10-year ASCVD risk
calculationb | 7.62±2.72 |
Clinical and CZT-SPECT parameters
under the two stenosis criteria
As shown in Table
II, there were no significant statistical differences in
clinical indices, including systolic blood pressure, diastolic
blood pressure, triglyceride, high-density lipoprotein, nor
low-density lipoprotein levels. However, there was a significant
difference for total cholesterol levels (P=0.029) between the two
groups when 50% was used as the criterion for positive coronary
stenosis. Diastolic blood pressure levels were significantly
different (P=0.006) when the criterion of positive stenosis was
75%. Among the parameters obtained from CZT-SPECT, CFR was lower in
the positive stenosis group under both stenosis criteria (both
P<0.01), and DS was higher (both P<0.01). Under a stenosis
criterion of 75%, stress coronary flow (SCF) was lower (P=0.010)
while the SS was higher (P=0.036) in the positive stenosis group.
There was no significant difference under the criterion of 50%
(SCF, P=0.115; SS, P=0.068). The parameters measured in the resting
state also did not reveal any statistically significant
differences. These findings suggested that CZT-SPECT parameters
might be more sensitive in detecting coronary stenosis than
clinical indices, and this may potentially serve as a useful tool
in the diagnosis and management of CAD.
 | Table IIComparisons of clinical and CZT-SPECT
parameters using two different coronary stenosis criteria at the
vascular level. |
Table II
Comparisons of clinical and CZT-SPECT
parameters using two different coronary stenosis criteria at the
vascular level.
| | ≥50% as the criterion
for positive stenosisd | ≥75% as the criterion
for positive stenosisd |
|---|
| Variable | Reference, n=38 | Positive group,
n=34 | t | P-value | Reference, n=56 | Positive group,
n=16 | t | P-value |
|---|
| SBP, mmHg | 127.21 (15.23) | 127.91 (17.02) | -0.183 | 0.854 | 126.39 (14.88) | 131.56 (19.37) | -0.988 | 0.335 |
| DBP, mmHg | 74.37 (9.33) | 77.03 (8.50) | -1.266 | 0.212 | 74.11 (8.76) | 80.94 (7.89) | -2.977 | 0.006b |
| TC, mmol/l | 3.59 (0.63) | 3.25 (0.65) | 2.225 | 0.029a | 3.48 (0.69) | 3.25 (0.51) | 1.457 | 0.155 |
| TG, mmol/l | 1.48 (1.06) | 1.36 (0.66) | 0.597 | 0.562 | 1.43 (0.95) | 1.38 (0.64) | 0.242 | 0.81 |
| HDL-C, mmol/l | 1.17 (0.27) | 1.07 (0.28) | 1.494 | 0.139 | 1.15 (0.28) | 1.02 (0.26) | 1.738 | 0.094 |
| LDL-C, mmol/l | 2.14 (0.47) | 1.95 (0.45) | 1.693 | 0.096 | 2.07 (0.49) | 1.97 (0.37) | 0.941 | 0.354 |
| SS | 1.16 (2.37) | 3.12 (5.68) | -1.873 | 0.068 | 1.12 (2.26) | 5.44 (7.42) | -2.294 | 0.036a |
| RS | 0.74 (2.13) | 1.29 (4.73) | -0.633 | 0.530 | 0.57 (1.80) | 2.50 (6.76) | -1.129 | 0.276 |
| DS | 0.42 (0.83) | 1.82 (2.48) | -3.145 | 0.003b | 0.55 (1.16) | 2.94 (2.82) | -3.307 | 0.004b |
| SCF | 1.93 (0.75) | 1.67 (0.65) | 1.596 | 0.115 | 1.91 (0.71) | 1.42 (0.60) | 2.778 | 0.010b |
| RCF | 0.72 (0.34) | 0.84 (0.29) | -1.554 | 0.126 | 0.77 (0.32) | 0.78 (0.31) | -0.025 | 0.980 |
| CFR | 2.88 (1.06) | 2.15 (0.75) | 3.381 | 0.001c | 2.68 (1.01) | 2.02 (0.73) | 2.878 | 0.007b |
ROC curve analysis for the diagnosis
of coronary stenosis
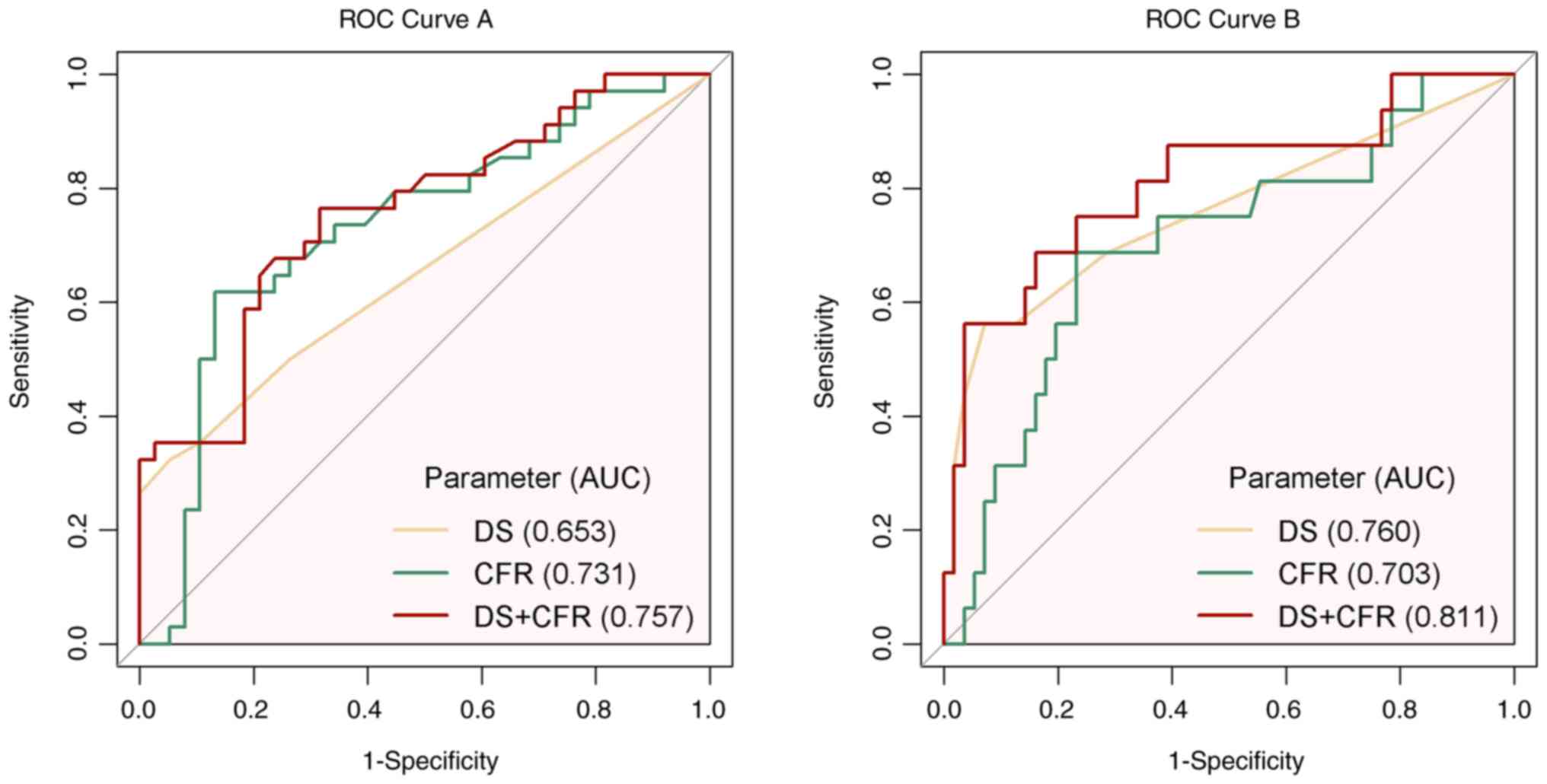
The ROC curve analysis for diagnosing coronary
stenosis (Fig. 2) demonstrated
that the area under the curve (AUC) and 95% confidence intervals
(CIs) of DS, CFR, and their combination were 0.653 (CI,
0.541-0.766), 0.731 (CI, 0.610-0.852), and 0.757 (CI, 0.645-0.869),
respectively, under the stenotic criterion of 50%, and 0.760 (CI,
0.614-0.906), 0.703 (CI, 0.550-0.855) and 0.811 (CI, 0.676-0.947),
respectively, for the stenotic criterion of 75%. The optimal
cut-off value for DS was 2.50 for the two criteria and the
respective cut-off values for CFR were 2.16 for the stenotic
criterion of 50% and 2.08 for the stenotic criterion of 75%. The
diagnostic efficacy for the optimal cut-off value is shown in
Table III. These findings
suggested that a combination of DS and CFR may be a useful tool for
the diagnosis of coronary stenosis, and could potentially improve
the accuracy and reliability of non-invasive tests for CAD.
 | Table IIIDiagnostic efficacy of DS, CFR, and
their combination for positive stenosis using two different
criteria. |
Table III
Diagnostic efficacy of DS, CFR, and
their combination for positive stenosis using two different
criteria.
| A, ≥50% as the
criterion for positive stenosis, n=72 (%) |
|---|
| Parameter | Cut-off value | Sensitivity | Specificity | PPV | NPV | Accuracy |
|---|
| DS | 2.50 | 32.4 (11/34) | 94.7 (36/38) | 84.6 (11/13) | 61.0 (36/59) | 65.3 (47/72) |
| CFR | 2.16 | 61.8 (21/34) | 86.8 (33/38) | 80.8 (21/26) | 71.7 (33/46) | 75.0 (54/72) |
| DS+CFR | | 76.5 (26/34) | 68.4 (26/38) | 68.4 (26/28) | 76.5 (26/44) | 72.2 (52/72) |
| B, ≥75% as the
criterion for positive stenosis, n=72 (%) |
| Parameter | Cut-off value | Sensitivity | Specificity | PPV | NPV | Accuracy |
| DS | 2.50 | 56.2 (9/16) | 92.9 (52/56) | 69.2 (9/13) | 88.1 (52/59) | 84.7 (61/72) |
| CFR | 2.08 | 68.8 (11/16) | 76.8 (43/56) | 45.8 (11/24) | 89.6 (43/48) | 75.0 (54/72) |
| DS+CFR | | 68.8 (11/16) | 83.9 (47/56) | 55.0 (11/20) | 90.4 (47/52) | 80.6 (58/72) |
Reclassification and discrimination
statistics for coronary stenosis
For the comparison of DS, CFR, and the combination
thereof, NRI and IDI were calculated to assess the predictive
ability, as shown in Table IV.
Compared with DS, no statistically significant difference was found
in the predictive power elevation of CFR when CAG stenosis ≥50% was
defined as the positive criterion among the complete study vessels.
However, CFR decreased the predictive power when the study criteria
were 75%, with an IDI of -0.339 to -0286 (P<0.05). Notably, the
combination of the two indices increased the stenosis prediction
with an NRI of 0.197-1.060 (P<0.01) and an IDI of 0.015-0.139
(P<0.05) within the 50% stenosis criteria, and an NRI of
0.031-1.076 (P<0.01) within the 75% stenosis criteria. These
findings suggested that DS was not absolutely inferior to CFR for
diagnostic accuracy of coronary stenosis, and the combination of DS
and CFR had a higher predictive ability for the diagnosis of
coronary stenosis than either DS or CFR alone.
 | Table IVComparison of the predictive
capability of coronary artery stenosis using different parameters
from CZT-SPECT. |
Table IV
Comparison of the predictive
capability of coronary artery stenosis using different parameters
from CZT-SPECT.
| A, ≥50% as the
criterion for positive stenosis |
|---|
| Parameter | DS | CFR | DS+CFR |
|---|
| NRI | 1 (ref) | 0.0124
(-0.4474-0.4722) | 0.6285
(0.1966-1.0604)b |
| IDI | 1 (ref) | 0.0126
(-0.0913-0.1165) | 0.0771
(0.0150-0.1391)a |
| B, ≥75% as the
criterion for positive stenosis |
| Parameter | DS | CFR | DS+CFR |
| NRI | 1 (ref) | -0.3214
(-0.8706-0.2278) | 0.5536
(0.0313-1.0758)a |
| IDI | 1 (ref) | -0.1839
(-0.3392-0.2860)a | 0.0171
(-0.0241-0.0584) |
Typical case
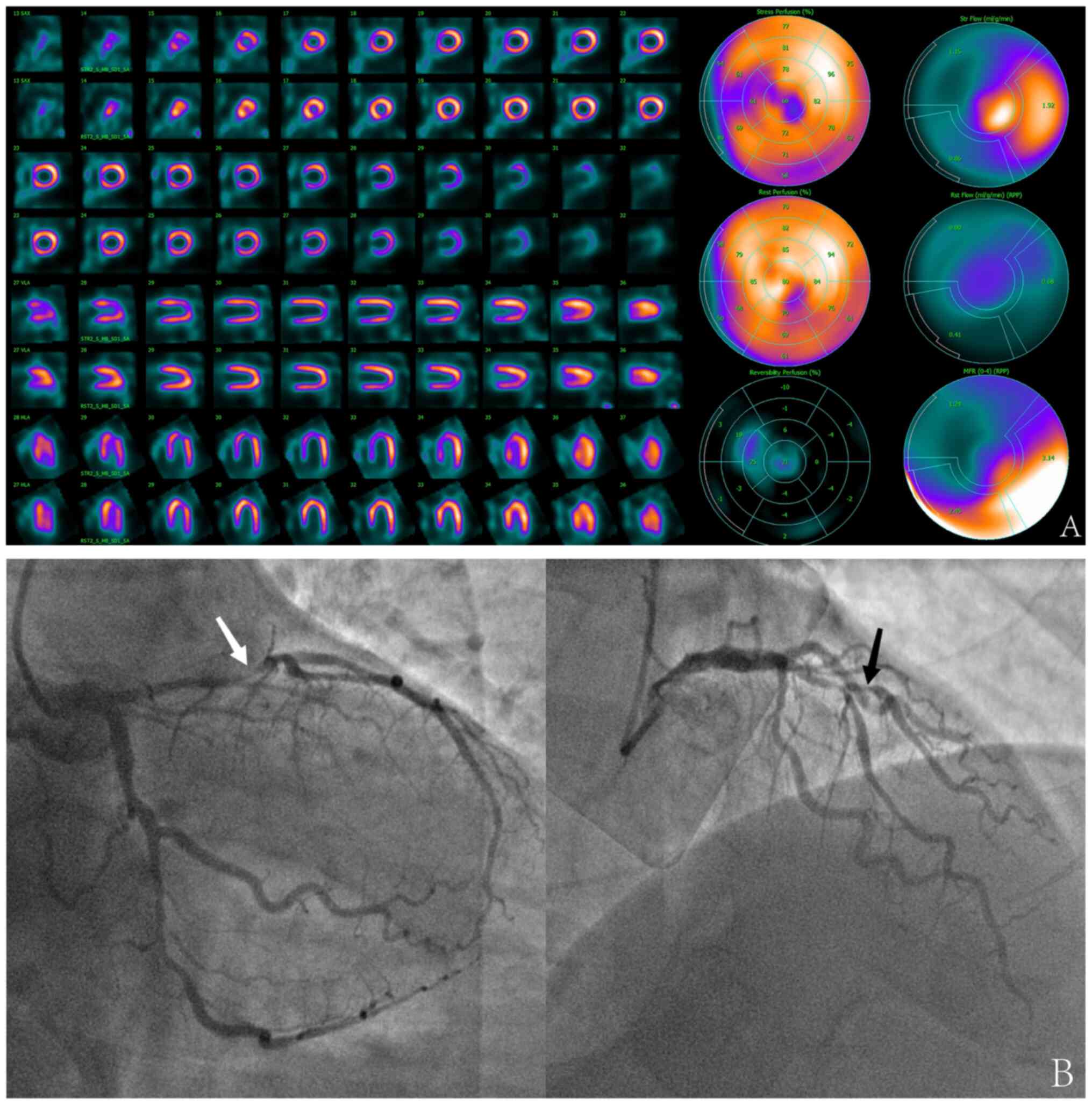
A 59-year-old male without a known history of
hypertension or diabetes complained of typical angina after mild
exertion over a period of 2 weeks. CZT-SPECT MPI in routine
Regadenoson stress and rest images showed moderate myocardial
ischemia only in the territory of LAD with DS=6, the quantitative
flow parameter was abnormally decreased in the territory of LAD
(CFR=1.24), and was almost normal in the territories of LCX
(CFR=3.14) and RCA (CFR=2.45) (Fig.
3A). Invasive CAG suggested a narrowed lesion in LAD with 85%
proximal limited stenosis and 70% proximal limited stenosis in the
first diagonal branch, and diffuse stenosis of 50-70% in LCX, with
no significant stenosis in RCA (Fig.
3B). This case highlighted the importance of early detection
and diagnosis of myocardial ischemia, which can help guide
appropriate treatment and management strategies. CZT-SPECT MPI can
serve as a useful tool for non-invasive diagnosis and risk
stratification of patients with suspected or known CAD.
Discussion
The quantitative flow parameters and the
semi-quantitative flow parameters are important in the diagnosis
and treatment of CAD and have been extensively studied (1,2,5,10).
This study focused on the concordance of these parameters measured
using the advanced cardiac-specific CZT-SPECT method with coronary
stenosis and their clinical values in CAD. Other potential clinical
parameters should not theoretically reflect the degree of coronary
stenosis since they do not directly correlate with coronary
stenosis and may be confounded by medications, which are consistent
with our findings.
The present study demonstrated the significant value
of CZT-SPECT MFPI in diagnosing and treating coronary heart
disease. As the difference between CFR and DS were statistically
significant under both stenosis criteria, the comparative analysis
of their diagnostic ability for positive stenosis was performed.
When considering coronary artery stenosis ≥50% as a positive
outcome, the diagnostic value of CFR for coronary stenosis was
comparable to DS, and the combination of the two indices increased
the predictive power compared with DS alone. When the positive
stenosis was defined as ≥75%, CFR was inferior to DS. However, the
combination of the two indices improved the predictive power.
Advanced CZT-SPECT can obtain continuous and dynamic
tomographic data acquisition, which increases the accuracy and
convenience of quantitative MBF measurements and greatly
compensates for the shortcomings of conventional SPECT. Its
excellent agreement with PET/CT in quantifying MBF has led to its
increasing use in clinical practice (12,13).
In a healthy coronary system, peak blood flow under stress can
increase up to more than three times than that at rest. Gould et
al (17) first demonstrated
the relationship between CFR and the degree of coronary stenosis in
1974, suggesting that CFR is barely affected in coronary stenosis
<50%, but decreases significantly in more severe stenosis,
primarily due to the reduction in stress blood flow. Therefore, it
was hypothesized that DS, the difference between stress and rest
measurements, may be more valuable than other MPI indices, which
was also confirmed by the results of the present study.
The assessment of the severity of coronary stenosis
can currently be discussed under two aspects: Anatomical and
functional. In clinical practice, a coronary angiographic finding
of 50% coronary stenosis is typically defined as the threshold for
the diagnosis of CAD, and a finding of coronary stenosis >70% is
considered severe stenosis, which may seriously affect the blood
fluid dynamics of the coronary artery. Thus, stenosis >70% is
typically regarded as the stenosis reference standard for
performing interventional therapy for patients with CAD, and
treatment modalities for stenosis between these two criteria
require a combination of clinical evidence of ischemia to make the
final decision (18). Given the
aforementioned guidelines, the present study was conducted under
two stenotic reference standards and it was found that both DS and
CFR were associated with the coronary stenosis of CAG.
A previous study that examined the left ventricular
blood flow as a whole concluded that quantitative parameters
obtained with CZT-SPECT presented certain diagnostic values for CAD
and demonstrated an improved ability compared with
semi-quantitative indicators (19). Another study demonstrated that
individuals with abnormal MPI after classification by the CAD
Prognostic Index had a decreased CFR compared with healthy
individuals [2.01 (CI, 1.48-2.77) vs. 2.94 (CI, 2.38-3.64);
P=0.002], and ROC analysis indicated that the overall best critical
value of CFR for high-risk CAD was 2.08 and the regional value was
2.2(20). One study analyzed 91
patients with suspected or confirmed CAD who had undergone CAG and
CZT-SPECT and found that MFR was lower in the coronary group
(stenosis ≥70%) than in the control group (1.96±0.7 vs. 2.74±0.9;
P<0.05) and the best cut-off value for CFR was 2.1(21). The results of the present study
were comparable to these previous studies and the ROC analysis also
demonstrated favorable diagnostic efficiency. In addition, studies
have demonstrated that CFR may improve the diagnostic efficacy of
SPECT MPI semi-quantitative parameters for CAD (19,22),
and the overall diagnostic efficacy of quantitative myocardial flow
analysis was higher than that of semi-quantitative analysis, which
is consistent with the findings of the present study. However, the
results of the present study suggested that the diagnostic value of
DS was overall improved compared with that of CFR at the stenosis
criterion of 75%, unlike in one previous study (19). It was indicated in the present
study that when evaluating coronary arteries with potentially
severe stenosis, DS was more likely to be an appropriate
non-invasive index due to its higher efficacy and lower cost than
CFR, which may shed light on current clinical decisions of
diagnosis and therapy. Finally, it was further demonstrated that
the power to jointly diagnose was best.
The present study has some limitations. Coronary
microvascular disease or collateral circulation may lead to
inconsistencies amongst coronary stenosis, DS, and CFR (23). Additionally, stenosis of the
coronary branch vessels was not considered here. Given the limited
sample size of the present study, sex differences could not be
demonstrated as in a previous study (24).
In conclusion, both the DS obtained with traditional
MPI and the CFR obtained with CZT-SPECT had certain diagnostic
values for coronary artery stenosis. DS was better than CFR in
predicting severe coronary stenosis, and the combined diagnostic
effect of DS and CFR was the best.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
ZF and WC conceived the study and wrote the
manuscript. BC, CL and JZ performed the statistical analysis. ZT,
LC and JB collected the data. DL and ZZ developed the concept and
methodology of the present study, provided guidance and revised the
manuscript.
Ethics approval and consent to
participate
The present study was approved by The Ethics
Committee of People's Hospital of Jiangsu Province (The First
Affiliated Hospital of Nanjing Medical University), and all
patients signed an informed consent form (approval no.
2022-SR-748).
Patient consent for publication
All patients provided a form giving informed
consent.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lawton JS, Tamis-Holland JE, Bangalore S,
Bates ER, Beckie TM, Bischoff JM, Bittl JA, Cohen MG, DiMaio JM,
Don CW, et al: 2021 ACC/AHA/SCAI guideline for coronary artery
revascularization: executive summary: A report of the American
college of cardiology/American heart association joint committee on
clinical practice guidelines. Circulation. 145:e4–e17.
2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Taqueti VR and Di Carli MF: Radionuclide
myocardial perfusion imaging for the evaluation of patients with
known or suspected coronary artery disease in the era of
multimodality cardiovascular imaging. Prog Cardiovasc Dis.
57:644–653. 2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Al Badarin FJ and Malhotra S: Diagnosis
and prognosis of coronary artery disease with SPECT and PET. Curr
Cardiol Rep. 21(57)2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ghadri JR, Pazhenkottil AP, Nkoulou RN,
Goetti R, Buechel RR, Husmann L, Herzog BA, Wolfrum M, Wyss CA,
Templin C and Kaufmann PA: Very high coronary calcium score unmasks
obstructive coronary artery disease in patients with normal SPECT
MPI. Heart. 97:998–1003. 2011.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Dorbala S, Ananthasubramaniam K, Armstrong
IS, Chareonthaitawee P, DePuey EG, Einstein AJ, Gropler RJ, Holly
TA, Mahmarian JJ, Park MA, et al: Single photon emission computed
tomography (SPECT) myocardial perfusion imaging guidelines:
Instrumentation, acquisition, processing, and interpretation. J
Nucl Cardiol. 25:1784–1846. 2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Alam L, Omar AMS and Patel KK: Improved
performance of PET myocardial perfusion imaging compared to SPECT
in the evaluation of suspected CAD. Curr Cardiol Rep. 25:281–293.
2023.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ziadi MC: Myocardial flow reserve (MFR)
with positron emission tomography (PET)/computed tomography (CT):
Clinical impact in diagnosis and prognosis. Cardiovasc Diagn Ther.
7:206–218. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Murthy VL, Bateman TM, Beanlands RS,
Berman DS, Borges-Neto S, Chareonthaitawee P, Cerqueira MD, deKemp
RA, DePuey EG, Dilsizian V, et al: Clinical quantification of
myocardial blood flow using PET: Joint position paper of the SNMMI
cardiovascular council and the ASNC. J Nucl Cardiol. 25:269–297.
2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Herzog BA, Buechel RR, Husmann L,
Pazhenkottil AP, Burger IA, Wolfrum M, Nkoulou RN, Valenta I,
Ghadri JR, Treyer V, et al: Validation of CT attenuation correction
for high-speed myocardial perfusion imaging using a novel
cadmium-zinc-telluride detector technique. J Nucl Cardiol.
51:1539–1544. 2010.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Fiechter M, Ghadri JR, Kuest SM,
Pazhenkottil AP, Wolfrum M, Nkoulou RN, Goetti R, Gaemperli O and
Kaufmann PA: Nuclear myocardial perfusion imaging with a novel
cadmium-zinc-telluride detector SPECT/CT device: First validation
versus invasive coronary angiography. Eur J Nucl Med Mol Imaging.
38:2025–2030. 2011.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ben-Haim S, Murthy VL, Breault C, Allie R,
Sitek A, Roth N, Fantony J, Moore SC, Park MA, Kijewski M, et al:
Quantification of myocardial perfusion reserve using dynamic SPECT
imaging in humans: A feasibility study. J Nucl Cardiol. 54:873–879.
2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Nkoulou R, Fuchs TA, Pazhenkottil AP,
Kuest SM, Ghadri JR, Stehli J, Fiechter M, Herzog BA, Gaemperli O,
Buechel RR and Kaufmann PA: Absolute myocardial blood flow and flow
reserve assessed by gated SPECT with cadmium-zinc-telluride
detectors using 99mTc-tetrofosmin: Head-to-head comparison with
13N-ammonia PET. J Nucl Cardiol. 57:1887–1892. 2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Agostini D, Roule V, Nganoa C, Roth N,
Baavour R, Parienti JJ, Beygui F and Manrique A: First validation
of myocardial flow reserve assessed by dynamic
99mTc-sestamibi CZT-SPECT camera: head to head
comparison with 15O-water PET and fractional flow
reserve in patients with suspected coronary artery disease. The
WATERDAY study. Eur J Nucl Med Mol Imaging. 45:1079–1090.
2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Miyagawa M, Nishiyama Y, Uetani T, Ogimoto
A, Ikeda S, Ishimura H, Watanabe E, Tashiro R, Tanabe Y, Kido T, et
al: Estimation of myocardial flow reserve utilizing an ultrafast
cardiac SPECT: Comparison with coronary angiography, fractional
flow reserve, and the SYNTAX score. Int J Cardiol. 244:347–353.
2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Garrett J, Knight E, Fawzy EM, Pridie RB,
Raftery EB and Towers MK: Proceedings: Coronary angiography using
Judkins method. Br Heart J. 36(399)1974.PubMed/NCBI
|
|
16
|
Miller TD and Askew JW: Net
reclassification improvement and integrated discrimination
improvement: new standards for evaluating the incremental value of
stress imaging for risk assessment. Circ Cardiovasc Imaging.
6:496–498. 2013.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Gould KL, Lipscomb K and Hamilton GW:
Physiologic basis for assessing critical coronary stenosis.
Instantaneous flow response and regional distribution during
coronary hyperemia as measures of coronary flow reserve. Am J
Cardiol. 33:87–94. 1974.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Pang Z, Wang J, Li S, Chen Y, Wang X and
Li J: Diagnostic analysis of new quantitative parameters of
low-dose dynamic myocardial perfusion imaging with CZT SPECT in the
detection of suspected or known coronary artery disease. Int J
Cardiovasc Imaging. 37:367–378. 2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Wang J, Li S, Chen W, Chen Y, Pang Z and
Li J: Diagnostic efficiency of quantification of myocardial blood
flow and coronary flow reserve with CZT dynamic SPECT imaging for
patients with suspected coronary artery disease: A comparative
study with traditional semi-quantitative evaluation. Cardiovasc
Diagn Ther. 11:56–67. 2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
de Souza ACDAH, Gonçalves BKD, Tedeschi AL
and Lima RSL: Quantification of myocardial flow reserve using a
gamma camera with solid-state cadmium-zinc-telluride detectors:
Relation to angiographic coronary artery disease. J Nucl Cardiol.
28:876–884. 2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Acampa W, Assante R, Mannarino T, Zampella
E, D'Antonio A, Buongiorno P, Gaudieri V, Nappi C, Giordano A,
Mainolfi CG, et al: Low-dose dynamic myocardial perfusion imaging
by CZT-SPECT in the identification of obstructive coronary artery
disease. Eur J Nucl Med Mol Imaging. 47:1705–1712. 2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Pang ZK, Wang J, Chen Y, Chu HX, Zhang MY
and Li JM: Diagnostic efficiency and incremental value of
myocardial blood flow quantification by CZT SPECT for patients with
coronary artery disease. Zhonghua Xin Xue Guan Bing Za Zhi.
50:494–500. 2022.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
23
|
Taqueti VR and Di Carli MF: Coronary
microvascular disease pathogenic mechanisms and therapeutic
options: JACC State-of-the-Art review. J Am Coll Cardiol.
72:2625–2641. 2018.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Gimelli A, Bottai M, Quaranta A, Giorgetti
A, Genovesi D and Marzullo P: Gender differences in the evaluation
of coronary artery disease with a cadmium-zinc telluride camera.
Eur J Nucl Med Mol Imaging. 40:1542–1548. 2013.PubMed/NCBI View Article : Google Scholar
|