Introduction
Almost 3 million people worldwide receive
haemodialysis treatment every year, and this number is expected to
double by the year 2030(1). More
than half of all haemodialysis patients are elderly (aged ≥65
years) (1). For this population,
well-timed placement of an arteriovenous (AV) vascular access by AV
graft (AVG) or AV fistula (AVF) may limit the usage of a tunnelled
central venous catheter (CVC) (2).
This is important as a well-timed placement of AV access in elderly
haemodialysis patients may reduce the risk of complications, such
as infection and thrombosis, that are associated with prolonged use
of tunnelled CVCs, thereby improving the quality of care and
overall prognosis of the patient (2). Currently, the general guidelines for
selecting a dialysis vascular access include a categorized
preference order, where AVF, AVG and CVC are the first, second and
last choice, respectively (3).
AVFs are often selected as the first choice due to their longer
patency and lower infection rates. However, AVF maturation process
can be slow and unpredictable, posing unique challenges for elderly
patients. On the other hand, AVGs, while quicker to mature, are
traditionally associated with a higher rate of complications, which
often makes them a less preferred method of dialysis vascular
access (3).
This categorized preference order for the placement
of vascular access has become a major point of debate worldwide
(4,5). For decades, AVF placement was
considered a preferred method of choice for the majority of
patients that required haemodialysis for treating end-stage kidney
disease (ESKD). However, recent advances in the treatment of ESKD
led to the changes in the incidence and prevalence of patients with
advanced renal conditions (6).
Changes in the treatment of ESKD have also changed our
understanding of the pros and cons associated with different
vascular access options. With increasing complexity of the health
profiles of patients, particularly among elderly populations, it is
necessary to reassess the efficacy and safety of AVGs and AVFs.
Haemodialysis is now offered to elderly ESKD
patients with various comorbidities, such as diabetes mellitus,
hypertension, cardiovascular disease, chronic respiratory
conditions, osteoporosis, and autoimmune disorders such as lupus.
Age is a major biological variable that can affect the outcomes of
vascular access (7). The optimal
vascular access (VA) strategy in elderly dialysis patients is still
unclear due to their shorter life expectancy, difficulties in VA
maturation and significantly higher risk of primary AVF failure
compared to younger adults (8).
Recent studies in elderly patients suggest that AVF may not
demonstrate clear advantage over AVG in terms of patency.
Therefore, patients can still benefit from AVG, as it is associated
with a shorter time to maturation (9-11).
To the best of our knowledge, there are no reviews that pool data
on the difference in outcomes, such as overall survival, mortality
rates, access survival, primary patency, maturation failure and
risk of infection in elderly patients. The goal of the present
study is to summarize data from individual studies to compare the
outcomes of AVG versus AVF for haemodialysis access in elderly
patients.
Materials and methods
Eligibility criteria
Study design. Randomized controlled
trials/non-randomized trials/cross-sectional/cohort/case-control
studies were included if they satisfied the inclusion criteria
listed below.
Study participants. Studies containing data
of elderly patients (≥60 years) requiring haemodialysis access were
incorporated.
Exposure. Studies evaluating the difference
in outcomes between AVF and AVG access for elderly patients were
included.
Outcomes. Studies reporting any of the
following outcomes: Overall survival/mortality rates, access
survival, primary patency, maturation failure and infection, were
eligible for inclusion.
Exclusion criteria. Case reports, case
series, conference abstracts, letters to editors, commentaries and
studies not reporting any of the aforementioned outcomes were
excluded from the analysis.
Search strategy
Systematic literature search was conducted in EMBASE
(https://www.embase.com/), Cochrane library
(https://www.cochranelibrary.com/search), MEDLINE
(https://pubmed.ncbi.nlm.nih.gov/),
Google Scholar (https://scholar.google.com/) and ScienceDirect
(https://www.sciencedirect.com/)
databases and search engines (Appendix S1). The search strategy used a
combination of medical subject headings (MeSH) and free-text terms
using the suitable Boolean operators (‘AND’ and ‘OR’). The
following filters were applied during the search: Time point
(January 1954 to January 2022), language (English only).
Bibliography of the retrieved articles was also searched to find
additional relevant studies (Data
S1).
Study selection process
The title and abstract were screened by two
independent investigators (JL and HL). Full text of the studies
that met the inclusion criteria were retrieved and further screened
by the same investigators (JL and HL) for studies that satisfied
the inclusion criteria. Disagreements were solved by discussion
with the third investigator (ZX). The review was reported based on
the Preferred Reporting Items for Systematic Reviews and
Meta-Analyses (PRISMA) statement 2020(12).
Data extraction process
Data was manually extracted using a pre-defined
structured data extraction form and included authors, title of
study, year of publication, study period, study design, setting,
country/region, total sample size, outcome assessment details,
average age, primary and secondary outcomes in each group. Data
entry was done by the first author (JL) and checked for any
potential errors by the second author (HL).
Risk of bias assessment
Two independent authors (ZX and QL) carried out
assessment of the risk of bias using Newcastle Ottawa (NO) scale
for observational studies and Cochrane Risk of bias 2 (RoB 2 tool)
for randomized controlled trials. NO scale included the following
domains: Selection (four stars), comparability (two stars) and
outcome (three stars). The final score ranged from zero to eight
stars. Studies ranging from 7-9 stars indicated ‘good quality’.
Quality of the studies with 5-6 stars were considered
‘satisfactory’, and studies with 0-4 stars were considered
‘unsatisfactory’ (13).
The RoB-2 tool was structured into a following
domains of bias: Process of randomization, variation from the
intended intervention, missing data on outcomes, outcome
measurements and selection of the reported results.
Based on results of the NO scale and RoB2 tool
assessment, quality of evidence of each study was then categorised
as having ‘low bias risk’, ‘high bias risk’, and ‘some concerns’
(14).
Statistical analysis
Meta-analysis was performed using STATA version 14.2
(StataCorp LLC). For the binary outcomes, the data were reported as
pooled odds ratio (OR) with 95% confidence interval (CI). For time
to event data (mortality and access free survival), pooled estimate
were calculated using natural logarithm of hazard ratio (ln{HR})
and standard error of ln(HR). First, HR with 95% Confidence
interval (CI) was retrieved from the included studies. Natural
logarithm of HR was calculated for each of the HR estimate.
Standard error of ln(HR) was calculated using the following
equations (15):
Variance of logarithmic HR was calculated as
follows: Variance (ln{HR})=[ln(upper CI of HR)-ln(lower CI of
HR)/2x1.96]
Standard error (SE) of logarithmic HR was calculated
as follows: SE (ln{HR})=√Variance (ln{HR})
Values of ln(HR)and SE were then entered into the
STATA software to estimate the pooled effect. Random effects model
was applied, and the data were reported as pooled HR with 95% CI
for both outcomes. Visual representation of the pooled estimates
were performed using Forest plots.
Heterogeneity was evaluated using χ2 test
and I2 statistic. I2<25% indicated mild
heterogeneity; 25-75% indicated moderate heterogeneity; and >75%
indicated substantial heterogeneity (16). Sensitivity analysis was performed
to evaluate the robustness of pooled estimate. Assessment of
publication bias through funnel plot and Egger's test could not be
performed for any of outcomes due to an insufficient (<10)
number of studies reporting each outcome.
Results
Study selection
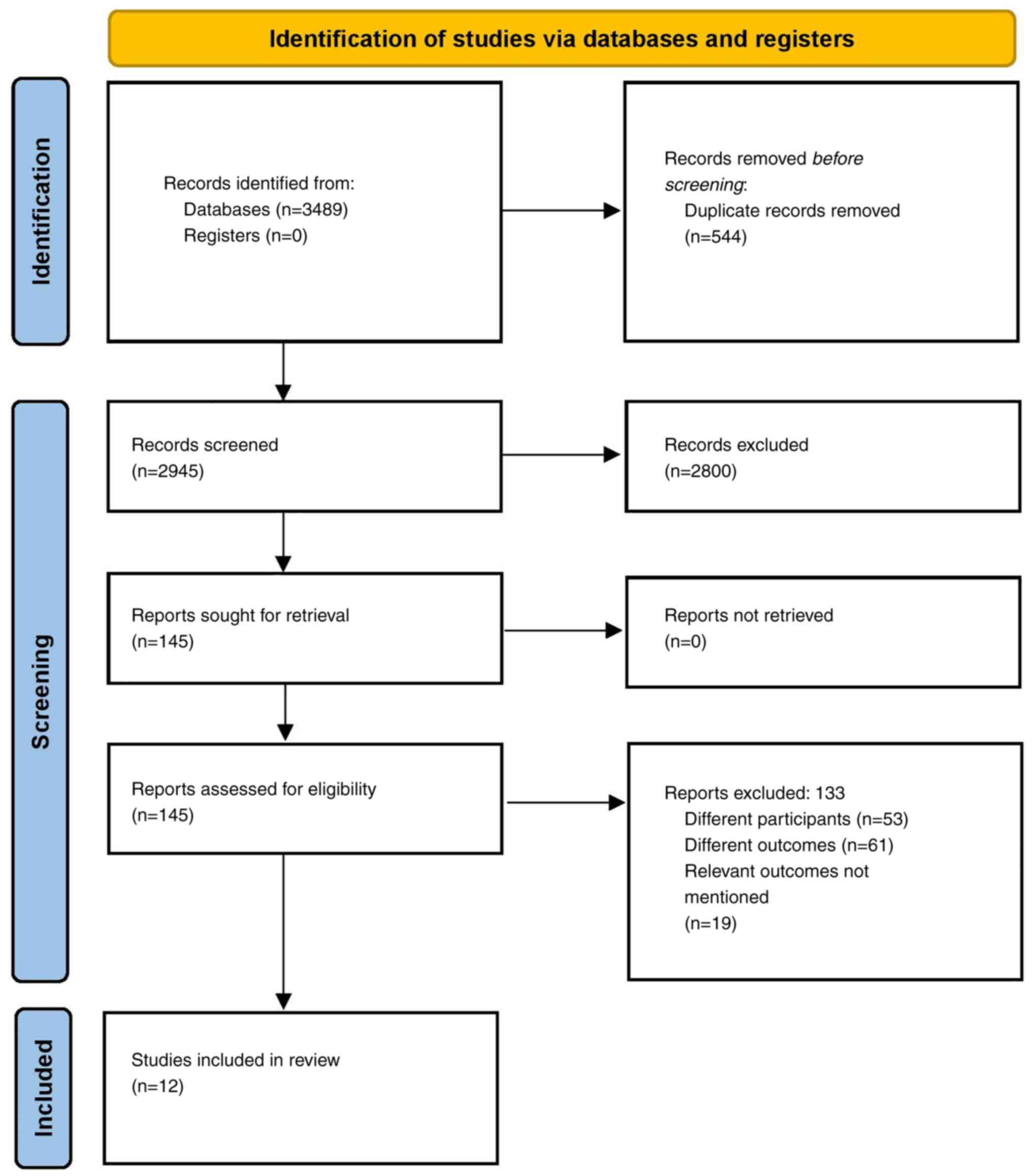
Literature search identified 3,489 papers. Of them,
145 studies were eligible for full text evaluation. In addition,
six more articles were retrieved by screening the references of the
full texts during primary screening. After the final screening, 12
studies containing 95,449 participants met the eligibility criteria
and were included in the analysis (Fig. 1) (9-11,17-25).
Characteristics of the included
studies
All studies, except Murea et al (17) and Robinson et al (18), were retrospective. Most (eight out
of 12) were conducted in the USA followed by South Korea (3
studies). The range of sample sizes was 29 to 25,226. The majority
of the studies were conducted in patient cohorts with >65 years
cut-off followed by >75 years cut-off. The follow-up duration
ranged from 215 days to 5 years (Table
I). Overall, nine out of 12 studies had higher risk of bias
(Table II and III).
 | Table ICharacteristics of the included
studies (n=12). |
Table I
Characteristics of the included
studies (n=12).
| First author,
year | Country | Study design | Sample size | Age cut-off,
years | Mean age, years | Males, % | Mean BMI,
kg/m2 | DM, % | HTN, % | CAD, % | Cancer, % | Follow-up
duration | Outcomes
measured | (Refs.) |
|---|
| Arhuidese et
al, 2019 | USA | Retrospective | 23,653 | >75 | AVG=82.2 | AVG=45.4 | AVG=26.9 | AVG=48 | AVG=87.3 | AVG=28 | AVG=10.7 | 5-year | Overall survival,
infection, primary patency | (9) |
| | | | | | AVF=82.0 | AVF=65.8 | AVF=26.8 | AVF=43 | AVF=88.9 | AVF=29.5 | AVF=11.7 | | | |
| Bae et al,
2018 | South Korea | Retrospective | 361 | >65 | AVG=74.9 | AVG=57.7 | AVG=22.7 | AVG=55.7 | AVG=72.2 | AVG=28.9 | AVG=18.3 | 5-year | Overall survival,
Maturation failure | (10) |
| | | | | | AVF=74.2 | AVF=54.8 | AVF=22.8 | AVF=55.4 | AVF=78 | AVF=19 | AVF=23.2 | | | |
| Choi et al,
2020 | South Korea | Retrospective | 878 | >65 | AVG=61 | AVG=52.9 | NR | AVG=71.2 | NR | AVG=20.4 | NR | NR | Access free
survival | (11) |
| | | | | | AVF=59 | AVF=60.9 | | AVF=62.7 | | AVF=16 | | | | |
| Cui et al,
2016 | China | Retrospective | 182 | >75 | NR | AVG=56.8 | NR | AVG=56.8 | AVG=93.2 | AVG=52.3 | NR | 2-year | Maturation
failure | (22) |
| | | | | | | AVF=65.2 | | AVF=47.1 | AVF=93.5 | AVF=55.8 | | | | |
| Jadlowiec et
al, 2016 | USA | Retrospective | 186 | >70 | AVG=78 | AVG=42.9 | NR | AVG=59.5 | AVG=89.2 | AVG=75.7 | NR | NR | Mortality,
Infection, patency, maturation failure | (21) |
| | | | | | AVF=78.8 | AVF=59.7 | | AVF=57 | AVF=94 | AVF=73.2 | | | | |
| Jhee et al,
2019 | South | Retrospective | 4,026 | >65 | AVG=74.3 | AVG=52.2 | AVG=21.9 | AVG=41.1 | AVG=52.4 | AVG=13.8 | AVG=2.5 | NR | Overall
survival | (25) |
| | Korea | | | | AVF=73 | AVF=58.4 | AVF=22.3 | AVF=40.3 | | AVF=14 | AVF=2.8 | | | |
| Lee et al,
2019 | USA | Retrospective | 14,370 | 65-74 | AVG=65 | AVG=87.5 | NR | NR | NR | NR | NR | NR | Overall survival,
access free survival | (23) |
| | | | | | AVF=60 | AVF=54.4 | | | | | | | | |
| Murea et al,
2020 | USA | RCT | 44 | >65 | AVG=72.8 | AVG=52.2 | AVG=30.9 | AVG=65.2 | AVG=87 | AVG=13 | AVG=26.1 | 215 days | Mortality | (17) |
| | | | | | AVF=78.9 | AVF=71.4 | AVF=25.5 | AVF=76.2 | AVF=90.5 | AVF=9.5 | AVF=23.8 | | | |
| Robinson et
al, 2021 | USA | RCT | 29 | >65 | AVG=77.5 | AVG=56 | AVG=30.3 | AVG=56 | AVG=82 | AVG=11 | AVG=22 | 321 days | Mortality,
infection, maturation failure | (18) |
| | | | | | AVF=75.4 | AVF=78 | AVF=27.6 | AVF=67 | AVF=89 | AVF=22 | AVF=22 | | | |
| Saleh et al,
2017 | USA | Retrospective | 10,030 | 70-80 | AVG=70.7 | AVG=91 | NR | AVG=67 | NR | AVG=26 | AVG=26 | NR | Overall
survival | (20) |
| | | | | | AVF=70.2 | AVF=96 | | AVF=66 | | AVF=24 | AVF=25 | | | |
| Woo et al,
2015 | USA | Retrospective | 16,464 | >66 | AVG=78 | AVG=55.6 | NR | AVG=77.5 | AVG=99.1 | AVG=82.9 | AVG=15.8 | 1 year | Mortality | (19) |
| | | | | | AVF=77.1 | AVF=40.6 | | AVF=73.2 | AVF=99 | AVF=79.8 | AVF=15 | | | |
| Xue et al,
2003 | USA | Retrospective | 25,226 | >67 | AVG=74.9 | AVG=57 | NR | AVG=39.2 | NR | NR | NR | 1 year | Mortality | (24) |
| | | | | | AVF=74.6 | AVF=62.2 | | AVF=37.8 | | | | | | |
 | Table IIQuality assessment for observational
studies amongst the included studies (n=10). |
Table II
Quality assessment for observational
studies amongst the included studies (n=10).
| Study no. | First author,
year |
Representativeness | Sample size
justification | Non-response | Ascertainment of
exposure | Control for
confounding | Assessment of
outcome | Statistical
tests | Overall
Quality | (Refs.) |
|---|
| 1 | Arhuidese et
al, 2019 | 0 star | 0 star | 0 star | 1 star | 1 star | 1 star | 1 star | Poor | (9) |
| 2 | Bae et al,
2018 | 0 star | 1 star | 1 star | 1 star | 1 star | 1 star | 1 star | Poor | (10) |
| 3 | Choi et al,
2020 | 0 star | 0 star | 1 star | 0 star | 0 star | 1 star | 1 star | Poor | (11) |
| 4 | Cui et al,
2016 | 0 star | 1 star | 0 star | 0 star | 0 star | 1 star | 0 star | Poor | (22) |
| 5 | Jadlowiec et
al, 2016 | 0 star | 0 star | 0 star | 1 star | 1 star | 1 star | 1 star | Satisfactory | (21) |
| 6 | Jhee et al,
2019 | 0 star | 0 star | 0 star | 1 star | 2 stars | 1 star | 1 star | Satisfactory | (25) |
| 7 | Lee et al,
2019 | 0 star | 1 star | 1 star | 1 star | 0 star | 1 star | 0 star | Poor | (23) |
| 8 | Saleh et al,
2017 | 0 star | 0 star | 1 star | 1 star | 0 star | 1 star | 1 star | Poor | (20) |
| 9 | Woo et al,
2015 | 0 star | 0 star | 0 star | 0 star | 0 star | 1 star | 1 star | Poor | (19) |
| 10 | Xue et al,
2003 | 0 star | 0 star | 0 star | 0 star | 0 star | 1 star | 0 star | Poor | (24) |
 | Table IIIQuality assessment for RCTs amongst
the included studies (n=2). |
Table III
Quality assessment for RCTs amongst
the included studies (n=2).
| Study no. | First author,
year | Randomization
process | Deviation from
intended intervention | Missing outcome
data | Measurement of
outcome | Selection of
reported result | Overall risk of
bias | (Refs.) |
|---|
| 1 | Murea et al,
2020 | Low risk | Low risk | Some concerns | High risk | High risk | High risk | (17) |
| 2 | Robinson et
al, 2021 | Low risk | Low risk | Low risk | Some concerns | Low risk | Some concerns | (18) |
Overall survival
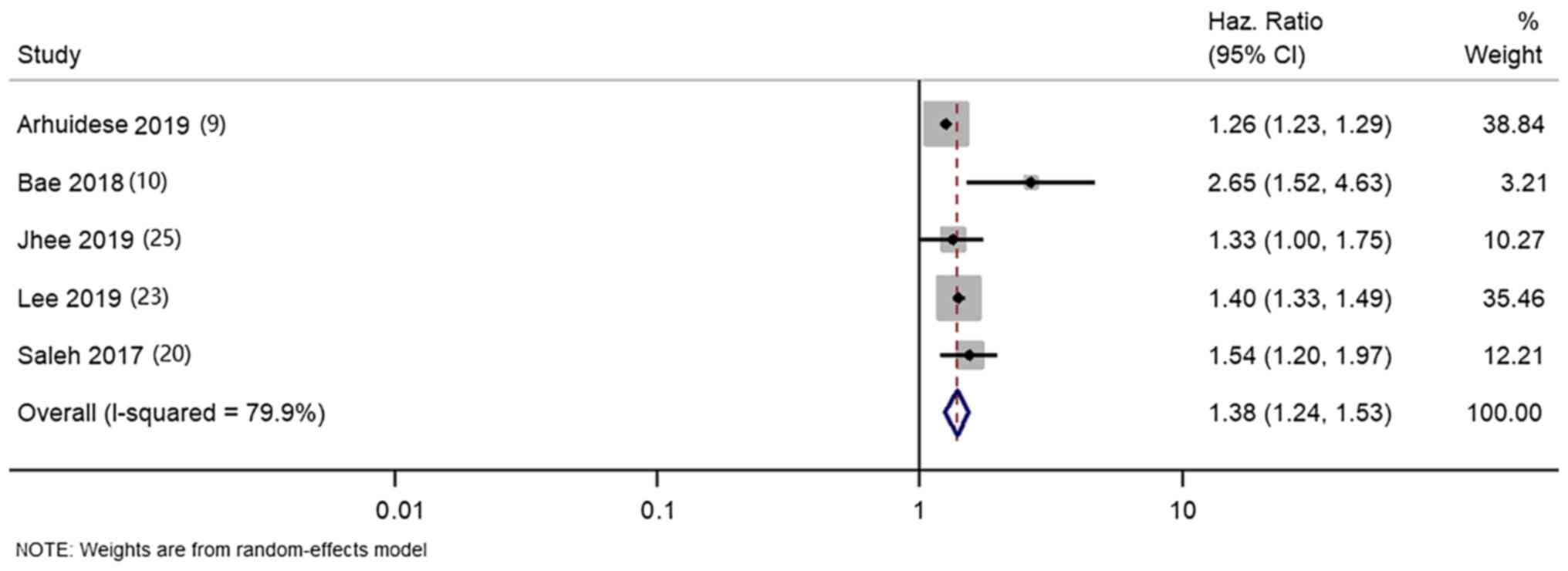
Firstly, five studies (9,10,20,23,25)
reported the difference in overall survival between elderly
patients that received AVG and AVF for haemodialysis access. The
pooled HR was 1.38 (95% CI, 1.24-1.53; I2=79.9%), which
suggested that AVG was associated with significantly decreased
survival compared with AVF in elderly patients (Fig. 2).
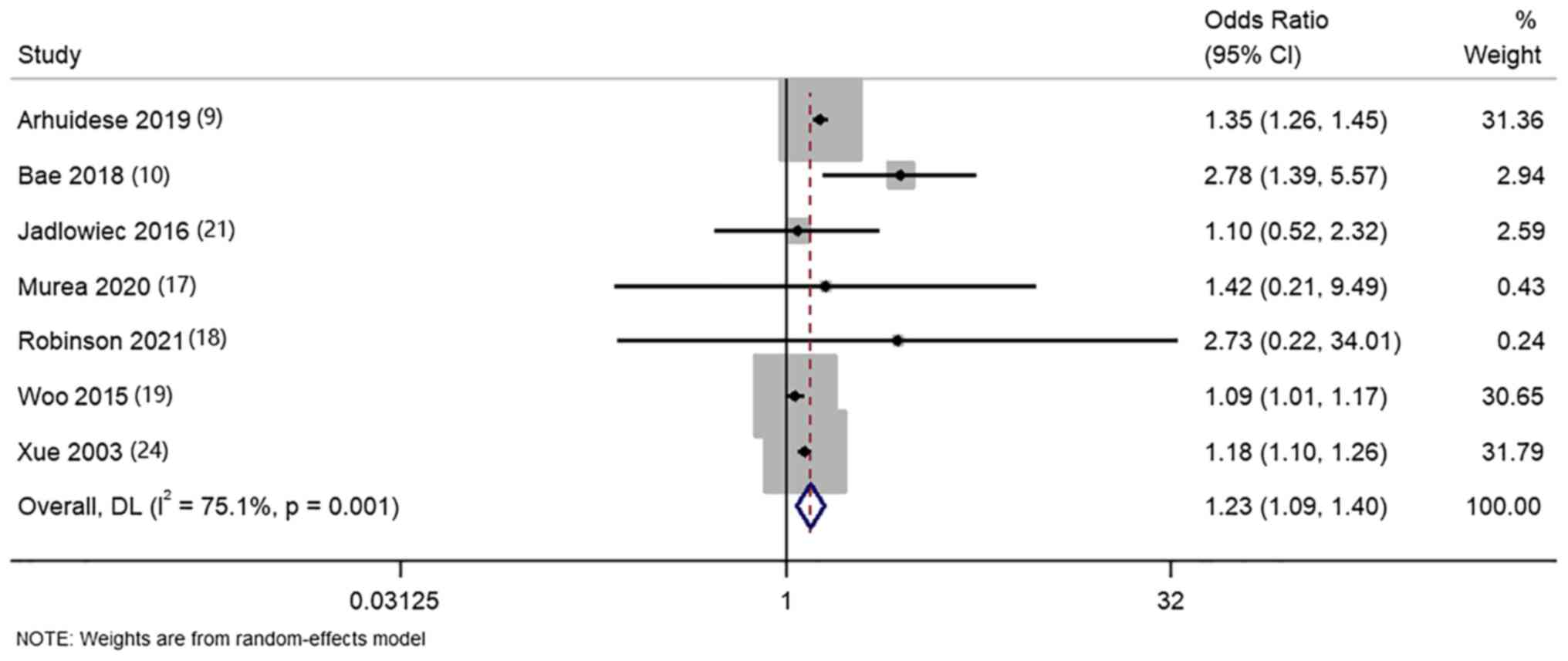
Then, seven studies (9,10,17-19,21,24)
compared the mortalities in elderly patients that received AVG and
AVF for haemodialysis access. The pooled OR was 1.23 (95% CI,
1.09-1.40; I2=75.1%), further confirming that elderly
patients receiving AVG access for haemodialysis had significantly
higher rate of mortality when compared with patients with AVF
(Fig. 3).
Access survival
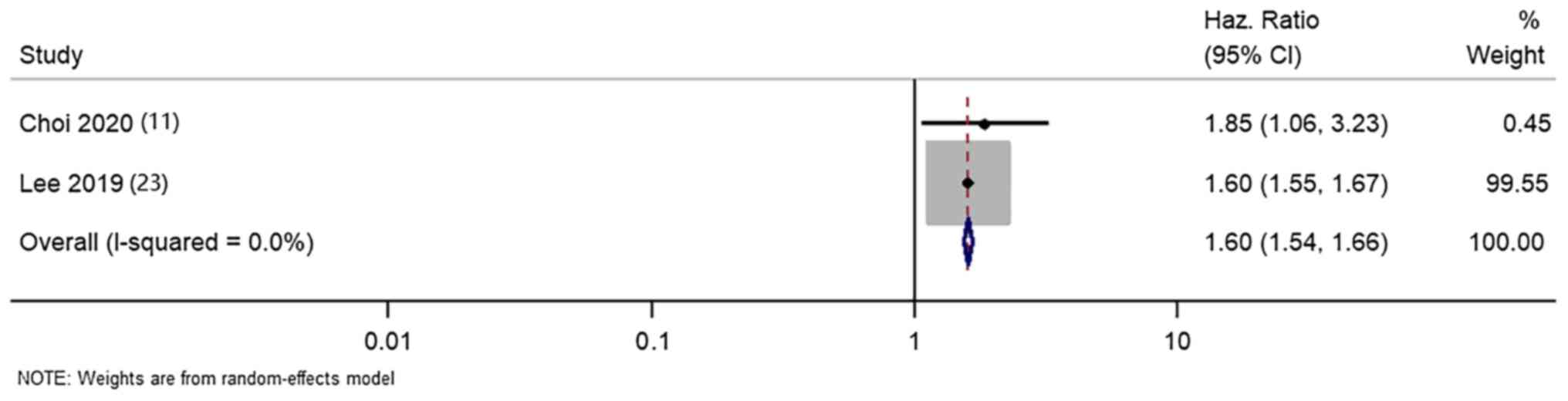
Next, two studies (11,23)
compared the access survival in AVG and AVF groups of elderly
patients. The pooled HR of 1.60 (95% CI, 1.54-1.66;
I2=0%) indicated that AVG was associated with
significantly worse access survival compared with AVF in elderly
haemodialysis patients (Fig.
4).
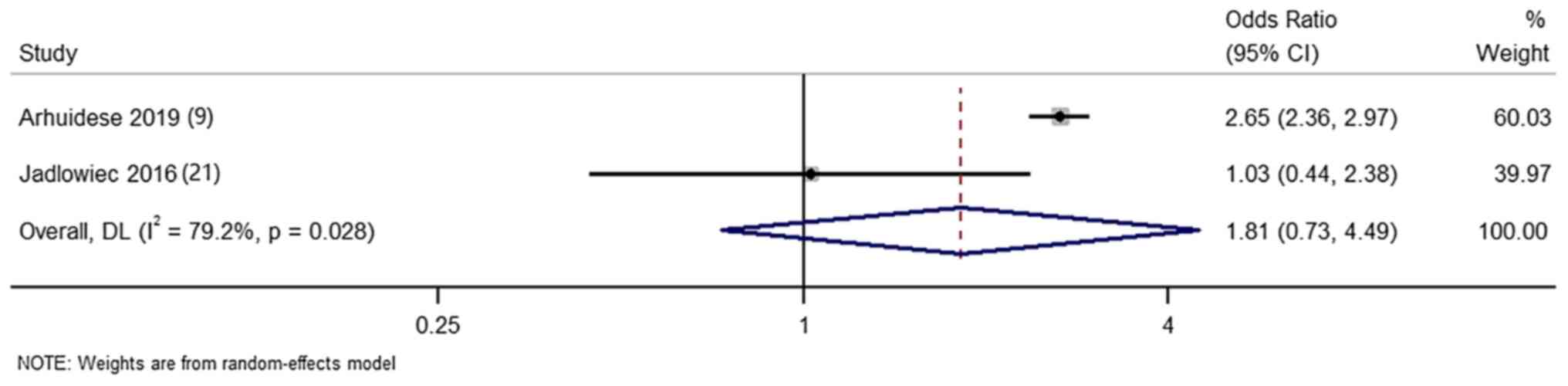
Two additional studies (9,21)
have reported the difference in primary patency rate
(intervention-free access survival) in terms of count outcomes
between the two groups of patients. The pooled OR was 1.81 (95% CI,
0.73-4.49; I2=79.2%), not indicating any significant
difference in terms of primary patency rate between AVG and AVF
groups (Fig. 5).
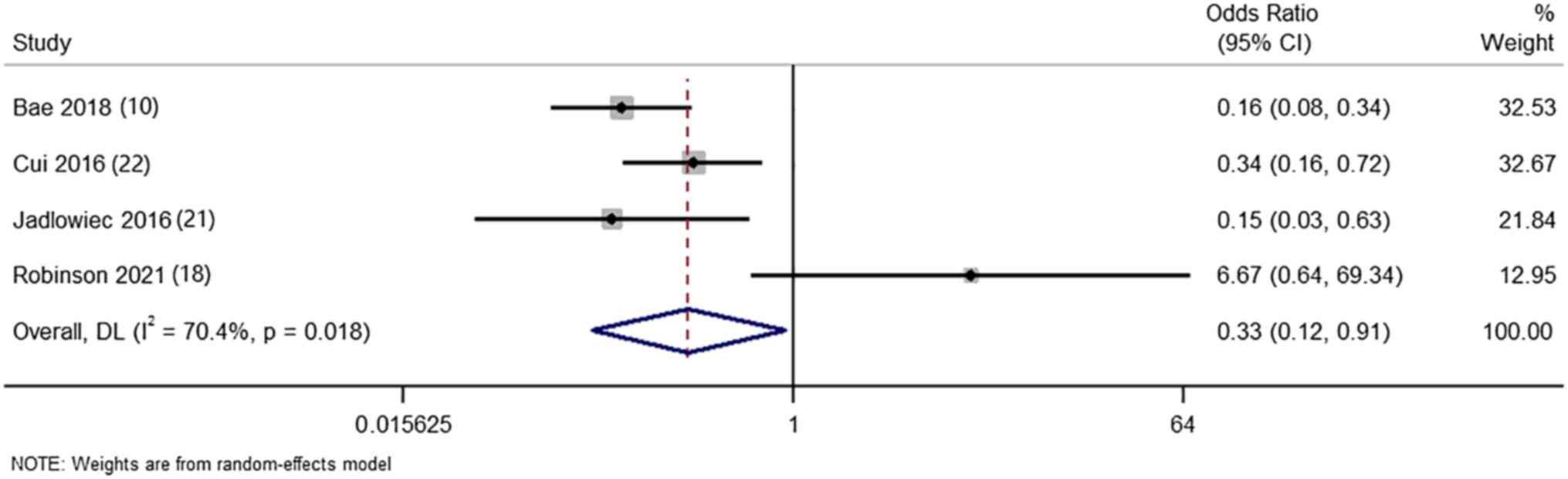
Maturation failure
There were four studies (10,11,18,21)
that reported the difference in maturation failure between AVG and
AVF groups of elderly haemodialysis patients. The pooled OR was
0.33 (95% CI, 0.12-0.91; I2=70.4%) indicating that
patients undergoing AVG had significantly lower risk of maturation
failure when compared with patients undergoing AVF (Fig. 6).
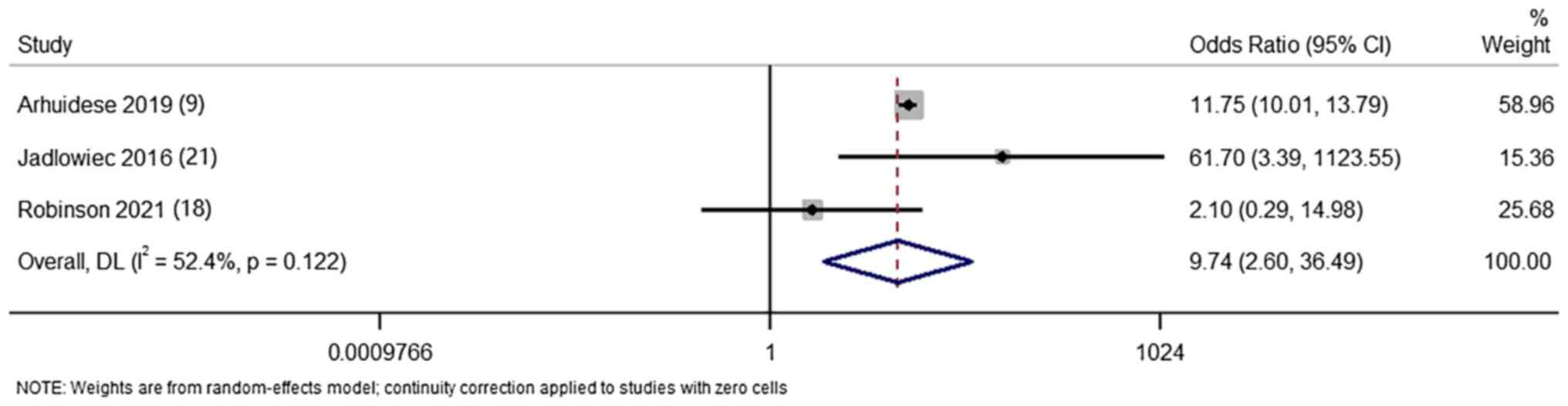
Infection
Finally, three studies (9,18,21)
reported the difference in infection rate in terms of count
outcomes between AVG and AVF groups of elderly patients. The pooled
OR was 9.74 (95% CI, 2.60-36.49; I2=52.4%) indicating
that there is 9-fold higher risk of infection in patients who
received AVG haemodialysis access compared with patients with AVF
(Fig. 7).
Additional analysis
Sensitivity analysis was performed to check the
small study effects by removing each of the studies one-by-one for
all outcomes. No significant variation in the effect size
(magnitude and direction) was detected by the sensitivity analysis.
This indicated a lack of single study effect on the overall
estimate for any of the outcomes.
Discussion
The current recommended guidelines for vascular
access do not provide any specific age-based recommendations for
the preferred placement of AVF over the AVG (3). Elderly patients undergoing
haemodialysis present unique challenges, such as diminished vein
and elasticity, high prevalence of atherosclerosis, increased risk
of infection and comorbidities, for the establishment and usage of
the vascular access (4). The
present systematic review assessed the risk of survival outcomes
associated with AVG and AVF access for haemodialysis among elderly
patients.
The present study investigated 12 studies that
fulfilled the eligibility criteria. The majority of these studies
were conducted in the USA followed by South Korea and China. Almost
all the studies [except for Murea et al (17) and Robinson et al (18)] were retrospective, and the majority
of them were of poorer quality with a high risk of bias. It was
revealed that AVG was associated with significantly higher risk of
mortality, lower access survival and higher rate of infection. At
the same time, AVG access in these patients correlated with
significantly lower risk of maturation failure. Though subgroup
analysis was not possible due to limited number of studies for each
outcome, there was some variation in the individual study estimates
based on the age cut-off, with higher magnitude of association in
higher-age group of patients. Sensitivity analysis did not reveal
significant effect of any single study on the magnitude or
direction of association.
These results were further confirmed by using
adjusted HR for the pooling of effect size. The crude estimates are
prone for confounding as they are not adjusted for any important
risk factors. The use of adjusted HR takes into account these
relevant confounding factors, and thus provides more reliable
estimate of the differences between the two vascular access methods
in elderly patients. While there are no existing reviews to compare
the observations of the present study in an elderly age group, the
current results were in agreement with the reviews that focused on
adult patients and compared AVG and AVF for haemodialysis access
(26-28).
A possible explanation for the observed differences in the outcomes
between these two haemodialysis access types may be due to a higher
rate of infections as a result of the colonization of the foreign
materials within the vascular space by skin microorganisms. This
may lead to poor overall survival and access survival in patients
undergoing AVG for haemodialysis access (26).
The increased mortality rate associated with AVG
when compared with AVF in the elderly population cannot be solely
attributed to the choice of vascular access. It is important to
consider that the selection between AVG and AVF is typically
dictated by patient-specific factors such as vascular health,
comorbidities, and the overall clinical profile of the patient
(4). This introduces an inherent
selection bias that may lead to worse outcomes in patients approved
for AVG.
An important finding of the present study is the
higher rate of infection in patients with AVG. However, the present
analysis did not distinguish between infections at the access site
and systemic events, nor was the severity of these infections
graded. Future studies should consider investigating these aspects
in more detail, as the type and severity of infection could
influence the decision-making process regarding the choice of
access type.
AVFs have a significantly higher risk of the
maturation failure, often requiring various intercurrent guidelines
strongly recommend AVF as a first-line and optimal vascular access
method for haemodialysis. There is insufficient information
available for evaluating the qualities of this methods (29). Since AVF is associated with higher
maturation failure and frequently requires repetitive
interventions, its indiscriminate use might result in the
ineffective usage of the services and resources (29).
The major strength of the present review was the
rigorous methodology and comprehensive literature search that adds
to the limited evidence available on the comparison these two
methods of vascular access. The present study did not detect any
significant changes in the effect size, as indicated by the
sensitivity analysis. This further enhanced the credibility of
these results. However, there are some limitations in the current
study. Substantial between-study variability was found for most of
the outcomes. The majority of the studies were of poorer quality
and limited heterogeneity. This might affect the external validity
(generalisability) of the findings. In addition, publication bias
was unable to be assessed due to the small number of studies, which
further limits the credibility of the evidence. The retrospective
nature of the included studies made it challenging to establish the
causal association. Hence, longitudinal evidence is required for
the identification of reliable effect size. This will allow making
evidence-based recommendations for deciding on the appropriate
vascular access type for elderly haemodialysis patients at the
hospital setting. Finally, the results of the present review may
not be credible as nine out of the 12 studies had high-risk of
bias. Given these limitations, it is crucial to stress that the
present results should not be interpreted as definitive evidence
for the decision-making in the clinical setting. The small number
and the retrospective design of most of the included studies, and
other potential biases restrict us from deriving firm
evidence-based recommendations from this meta-analysis.
Nevertheless, the present study had certain
important implications for the healthcare professionals treating
elderly haemodialysis patients. A stronger association of survival
outcomes was revealed with AVG compared with AVF in elderly
patients. However, the maturation failure was higher with AVF and
limited evidence was available in terms of RCTs. The potential
confounding effect of infections on survival analyses was also
notable. Although the meta-analysis showed a worse survival rate
with AVG, whether this was influenced by the increased rate of
infections in this group was not specifically investigated. Thus,
the impact of infections on survival outcomes remains unclear. In
the future, more rigorous statistical methods may be necessary to
control for such confounding factors and accurately determine the
individual effects of AVG and AVF on survival rates in the
elderly.
While the current analysis revealed a stronger
association of survival outcomes with AVG compared with AVF in
elderly patients, a higher maturation failure rate was observed
with AVF. The limited availability of RCTs evidence restricted the
current study from deriving firm evidence-based recommendations
from the results. However, importantly, the KDOQI guidelines
recommend basing the decision on vascular access not only on the
age of the patient or access type but to follow a comprehensive,
individualized life plan that takes into consideration the history
of the patient, comorbidities, vascular health, life expectancy and
future needs. These guidelines should be considered when deciding
on the appropriate access type for each elderly haemodialysis
patient.
Supplementary Material
Data S1
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JL conceived and designed the study. HL, ZX, QL and
HS collected the data and performed the literature search. JL was
involved in the writing of the manuscript. All authors have read
and approved the final manuscript. JL,HL, ZX, QL and HS confirm the
authenticity of all the raw data.
Ethical approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Liyanage T, Ninomiya T, Jha V, Neal B,
Patrice HM, Okpechi I, Zhao MH, Lv J, Garg AX, Knight J, et al:
Worldwide access to treatment for end-stage kidney disease: A
systematic review. Lancet. 385:1975–1982. 2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Besarab A: Resolved: Fistulas are
preferred to grafts as initial vascular access for dialysis. Pro. J
Am Soc Nephrol. 19:1629–1633. 2008.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Vascular Access 2006 Work Group. Vascular
access 2006 work group: Clinical practice guidelines for vascular
access. Am J Kidney Dis. 48 (Suppl 1):S176–S247. 2006.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ethier J, Mendelssohn DC, Elder SJ,
Hasegawa T, Akizawa T, Akiba T, Canaud BJ and Pisoni RL: Vascular
access use and outcomes: An international perspective from the
dialysis outcomes and practice patterns study. Nephrol Dial
Transplant. 23:3219–3226. 2008.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Lok CE: Fistula first initiative:
Advantages and pitfalls. Clin J Am Soc Nephrol. 2:1043–1053.
2007.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Bikbov B, Purcell CA and Levey AS:
HYPERLINK ‘https://www.researchgate.net/scientific-contributions/Mari-Smith-2131815162’.
Smith M and Abdoli A: HYPERLINK ‘https://www.researchgate.net/profile/Molla-Abebe’.
Abebe M, Adebayo O, Afarideh M, Agarwal S, Agudelo-Botero M, et al:
Global, regional, and national burden of chronic kidney disease,
1990-2017: A systematic analysis for the global burden of disease
study 2017. The Lancet. 395:709–733. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Cortés MJ, Viedma G, Perales MC, Borrego
FJ, Borrego J, del Barrio PP, Cunquero JMG, Liébana A and Bañasco
VP: Fistulae or catheter for elderly who start hemodialysis without
permanent vascular access? Nefrologia. 25:307–314. 2005.PubMed/NCBI(In Spanish).
|
|
8
|
Murea M and Satko S: Looking beyond
‘fistula first’ in the elderly on hemodialysis. Semin Dial.
29:396–402. 2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Arhuidese IJ, Cooper MA, Rizwan M, Nejim B
and Malas MB: Vascular access for hemodialysis in the elderly. J
Vasc Surg. 69:517–525.e1. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Bae E, Lee H, Kim DK, Oh KH, Kim YS, Ahn
C, Han JS, Min SII, Min SK, Kim HC and Joo KW: Autologous
arteriovenous fistula is associated with superior outcomes in
elderly hemodialysis patients. BMC Nephrol. 19(306)2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Choi J, Ban TH, Choi BS, Baik JH, Kim BS,
Kim YO, Park CW, Yang CW, Jin DC and Park HS: Comparison of
vascular access patency and patient survival between native
arteriovenous fistula and synthetic arteriovenous graft according
to age group. Hemodial Int. 24:309–316. 2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Page MJ, McKenzie JE, Bossuyt PM, Boutron
I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan
SE, et al: The PRISMA 2020 statement: An updated guideline for
reporting systematic reviews. BMJ. 372(n71)2021.PubMed/NCBI View
Article : Google Scholar
|
|
13
|
Wells G, Shea B, O'Connell D, Peterson J,
Welch V, Losos M and Tugwell P: The Newcastle-Ottawa Scale (NOS)
for assessing the quality of nonrandomized studies in meta-
analysis. The Ottawa Hospital Research Institute. 21:2021.
|
|
14
|
Sterne JAC, Savović J, Page MJ, Elbers RG,
Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge
SM, et al: RoB 2: A revised tool for assessing risk of bias in
randomised trials. BMJ. 366(l4898)2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Parmar MK, Torri V and Stewart L:
Extracting summary statistics to perform meta-analyses of the
published literature for survival endpoints. Stat Med.
17:2815–2834. 1998.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Higgins JPT and Green S: Cochrane Handbook
for Systematic Reviews of Interventions, 2022.
|
|
17
|
Murea M, Geary RL, Houston DK, Edwards MS,
Robinson TW, Davis RP, Hurie JB, Williams TK, Velazquez-Ramirez G,
Bagwell B, et al: A randomized pilot study to evaluate graft versus
fistula vascular access strategy in older patients with advanced
kidney disease: Results of a feasibility study. Pilot Feasibility
Stud. 6(86)2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Robinson T, Geary RL, Davis RP, Hurie JB,
Williams TK, Velazquez-Ramirez G, Moossavi S, Chen H and Murea M:
Arteriovenous fistula versus graft access strategy in older adults
receiving hemodialysis: A pilot randomized trial. Kidney Med.
3:248–256.e1. 2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Woo K, Goldman DP and Romley JA: Early
failure of dialysis access among the elderly in the era of fistula
first. Clin J Am Soc Nephrol. 10:1791–1798. 2015.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Saleh T, Sumida K, Molnar MZ, Potukuchi
PK, Thomas F, Lu JL, Gyamlani GG, Streja E, Kalantar-Zadeh K and
Kovesdy CP: Effect of age on the association of vascular access
type with mortality in a cohort of incident end-stage renal disease
patients. Nephron. 137:57–63. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Jadlowiec CC, Mannion EM, Lavallee M and
Brown MG: Hemodialysis access in the elderly: Outcomes among
patients older than seventy. Ann Vasc Surg. 31:77–84.
2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Cui J, Steele D, Wenger J, Kawai T, Liu F,
Elias N, Watkins MT and Irani Z: Hemodialysis arteriovenous fistula
as first option not necessary in elderly patients. J Vasc Surg.
63:1326–1332. 2016.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Lee HS, Song YR, Kim JK, Joo N, Kim C, Kim
HJ and Kim SG: Outcomes of vascular access in hemodialysis
patients: Analysis based on the Korean national health insurance
database from 2008 to 2016. Kidney Res Clin Pract. 38:391–398.
2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Xue JL, Dahl D, Ebben JP and Collins AJ:
The association of initial hemodialysis access type with mortality
outcomes in elderly Medicare ESRD patients. Am J Kidney Dis.
42:1013–1019. 2003.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Jhee JH, Hwang SD, Song JH and Lee SW: The
impact of comorbidity burden on the association between vascular
access type and clinical outcomes among elderly patients undergoing
hemodialysis. Sci Rep. 9(18156)2019.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Ravani P, Palmer SC, Oliver MJ, Quinn RR,
MacRae JM, Tai DJ, Pannu NI, Thomas C, Hemmelgarn BR, Craig JC, et
al: Associations between hemodialysis access type and clinical
outcomes: A systematic review. J Am Soc Nephrol. 24:465–473.
2013.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Bylsma LC, Gage SM, Reichert H, Dahl SLM
and Lawson JH: Arteriovenous Fistulae for Haemodialysis: A
systematic review and meta-analysis of efficacy and safety
outcomes. Eur J Vasc Endovasc Surg. 54:513–522. 2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Almasri J, Alsawas M, Mainou M, Mustafa
RA, Wang Z, Woo K, Cull DL and Murad MH: Outcomes of vascular
access for hemodialysis: A systematic review and meta-analysis. J
Vasc Surg. 64:236–243. 2016.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Palmer SC, McGregor DO, Macaskill P, Craig
JC, Elder GJ and Strippoli GFM: Meta-analysis: Vitamin D compounds
in chronic kidney disease. Ann Intern Med. 147:840–853.
2007.PubMed/NCBI View Article : Google Scholar
|