Introduction
Skeletal class III malocclusion is highly prevalent
in China, with an incidence of ~15.67%, and maxillary sagittal
deficiency accounts for 42-67% of all class III malocclusion cases
(1). Malocclusion has been
associated with clinical changes of masticatory muscles or the
temporomandibular joint and temporomandibular disorders that are
accompanied by joint and muscle pain, and limitations of mouth
opening (2). Studies suggest that
the management of class III malocclusion improves temporomandibular
joint conditions (3,4). It is well-established that
malocclusion symptoms associated with maxillary sagittal
deficiency, such as malocclusion itself, midfacial depression and
nasal collapse, significantly impact the physical and mental
wellbeing of adolescent patients with skeletal class III
malocclusion (5,6). Therefore, early intervention is
typically recommended for such patients.
Rapid expansion combined with maxillary protraction
has emerged (7) as an effective
approach for treating skeletal class III malocclusion. While
maxillary protraction efficiently improves facial aesthetics and
occlusion in younger patients (8),
there is a lack of sufficient research on the effects of anterior
distraction in patients during the post-pubertal stage. The
development of the micro-implant anchorage has increased the use of
maxillary skeletal expansion combined with protraction in
post-pubertal patients and improved the overall treatment effect.
By comparing bone anchorage and dental anchorage in class III
patients, Seiryu et al (9)
found that facemask therapy and a miniscrew provided more
orthopedic force and controlled the side effects of alveolar bone.
However, based on clinical observations by our group, certain
post-pubertal patients still refuse this invasive procedure and
choose to use dental anchorage protraction, which is associated
with a potential risk of recurrence (10,11).
Therefore, it is crucial to determine whether post-pubertal
patients would benefit from dental anchorage-forward distraction
therapy. Various factors influence growth and development, and even
individuals of the same age may exhibit varying degrees of skeletal
maturity (12-15).
In recent years, the prevalence of precocious puberty in children
has increased, rendering physiological age an insufficient
criterion for assessing their growth and development status
(16-18).
Jang et al (19) used cone
beam computed tomography (CBCT) and confirmed a correlation between
the cervical vertebral bone age stage and the maturity of multiple
maxillary sutures. The cervical vertebral maturation (CVM) method
offers higher accuracy compared to physiological age and greater
convenience compared to carpal bone age in determining children's
growth and development stage (20). In a previous publication by our
group that provided a research basis for the current study
(21), patients with
maxillomandibular transverse width incoherence who were treated
with rapid maxillary expansion were examined, and they were grouped
according to cervical vertebral maturation. The results showed that
the effect of maxillary transverse expansion was different in
patients with different bone ages, and the effect of skeletal
expansion decreased gradually with the increase of bone age.
Therefore, in the present study, the CVM method was
also used to group skeletal class III patients and investigate
whether the treatment effect of maxillary sagittal distraction
differed in patients with different bone ages. In addition, the
present study aimed to assess the feasibility of maxillary
protraction in a specific population of patients in the later stage
of growth and development to provide favorable evidence for using
rapid expansion combined with maxillary protraction therapy in
post-pubertal patients.
Patients and methods
Patients
According to the pre-determined eligibility criteria
(listed later), clinical records of skeletal class III patients who
underwent rapid expansion combined with maxillary protraction at
the Department of Orthodontics of the Second Hospital of Jiaxing
(Jiaxing, China) from January 2019 to June 2022 were
retrospectively screened. Records of 45 eligible skeletal class III
adolescent patients were retrospectively collected and grouped
according to the cervical spine bone age shown by their lateral
cephalograms.
Inclusion criteria
Patients were included if they met the following
criteria: i) Skeletal class III malocclusion based on the A point
to B point to nasion; the angle that relates the anterior limit of
the maxillary bone (A point) and mandibular bone (B point) with the
anterior limit of the nasofrontal suture (N point) (ANB) as
-3°<ANB<0°; ii) facial profile exhibiting midfacial
depression, with maxillary sagittal deficiency, maxillary
prominence [distance from the point of the A point to the Nasion
perpendicular (ANP) <1 mm (McNamara analysis) (22)]; iii) the mandibular growth pattern
was defined as average or horizontal growth, mandibular plane angle
(MPA) <32°; iv) lateral cephalograms indicating the growth and
development stage of the cervical spine; v) rapid palatal expansion
treatment combined with anterior distraction was performed for more
than 1 year.
Exclusion criteria
Patients were included if the following applied: i)
Patients did not cooperate; ii) temporomandibular joint disease;
iii) cleft lip and palate and maxillofacial or growth and
development defects; iv) a previous history of surgery, trauma,
orthodontic treatment, maxillofacial defects or growth defects; v)
a family history of mandibular hyperdevelopment [patients with
overgrowth of the mandible were excluded, according to Jaraback's
analysis (23)].
Grouping
According to the CVM method, 45 patients who met the
inclusion and exclusion criteria were divided into three groups.
The pre-pubertal group consisted of 15 patients (8 males and 7
females; mean age, 7.3 years) with CVM stages I-II; the pubertal
group included 15 patients (6 males and 9 females; mean age, 9.4
years) with CVM stage III; and the post-pubertal group had 15
patients (5 males and 10 females; mean age, 12.2 years) with CVM
stages IV-VI (24).
Therapeutic method
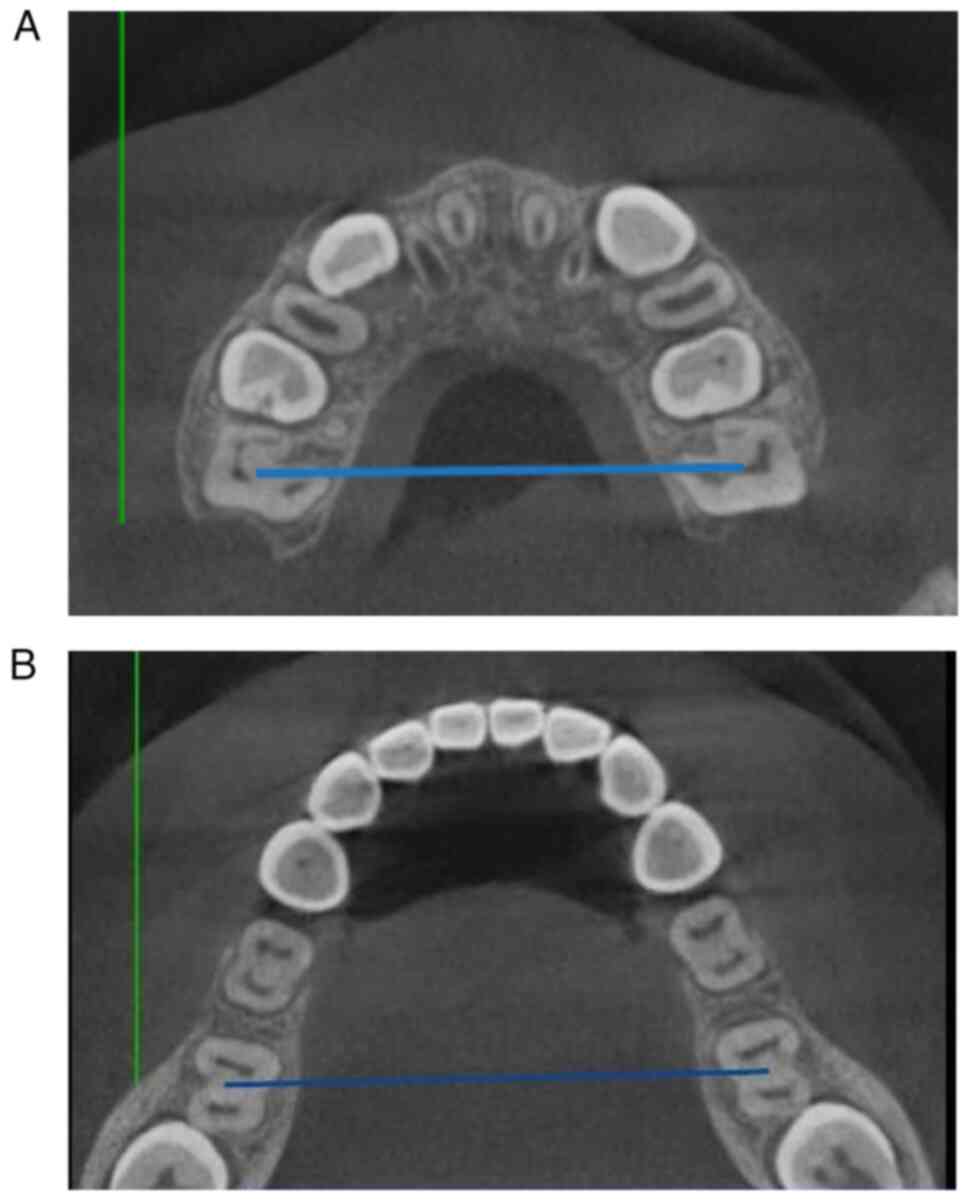
As previously described (25), lateral cephalograms and CBCT were
taken before the treatment to examine the sagittal and transverse
imbalance of the upper and lower jaw. CBCT was used to measure the
width of each patient's maxillary and mandibular basal bone arches
(the width of the connection between the root furcations of the
bilateral first molars) prior to treatment (Fig. 1A and B, respectively) (26). Rapid maxillary expansion was first
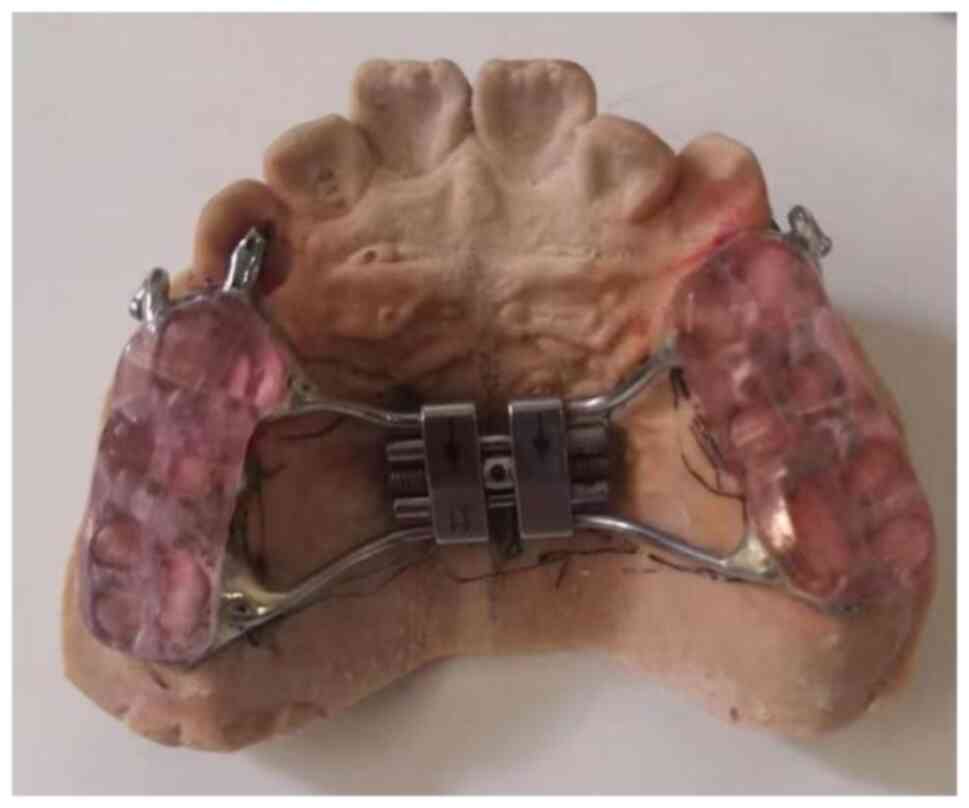
used for each patient included in the study (Fig. 2) with an occlusal pad for maxillary
rapid expansion. The coil spring was required to be opened 0.5 mm
(2 revolutions/day) daily. The width of the upper and lower jaws
was adjusted to make the width of the maxillary base bone arch 2 mm
larger than that of the mandibular base bone arch. After completing
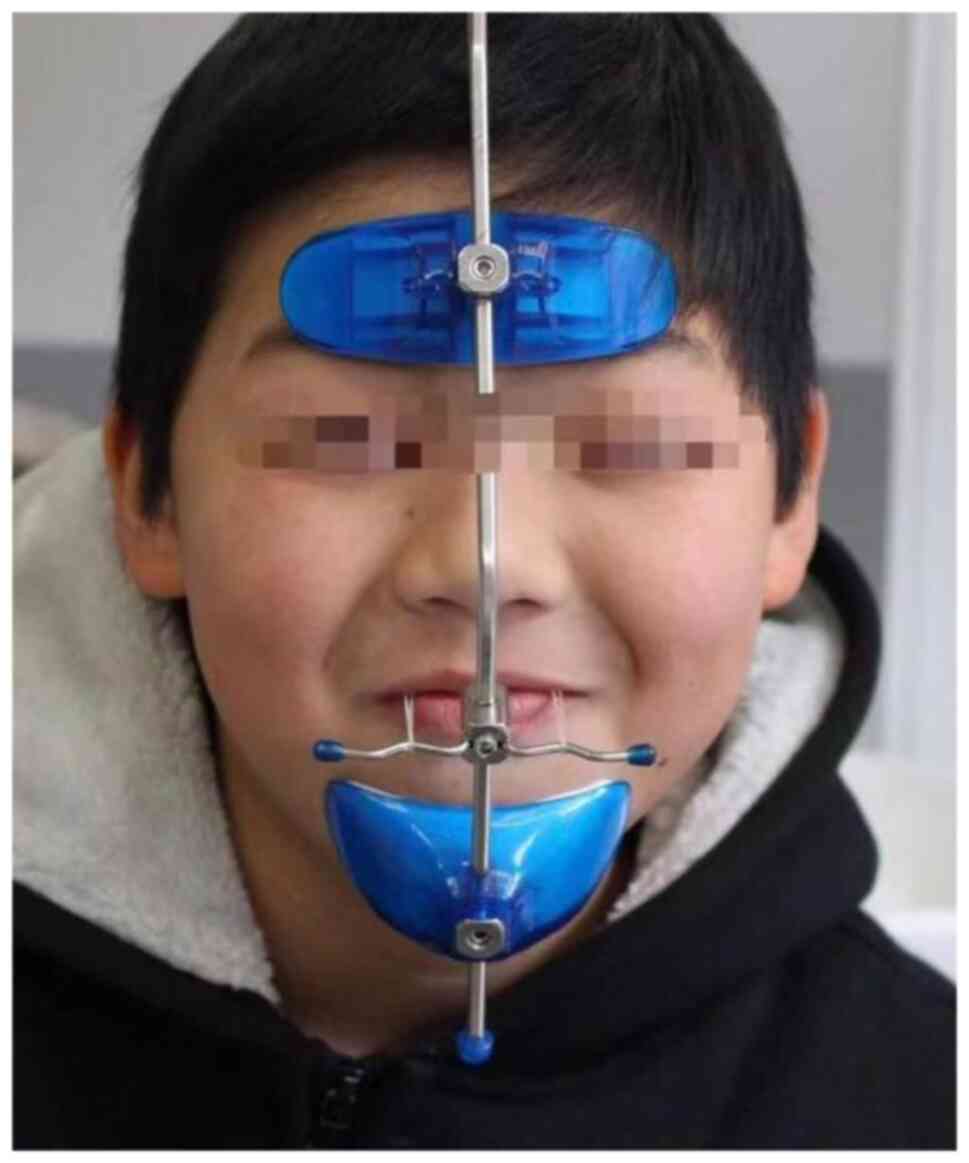
the maxillary expansion, the Petit-type facemask (Hangzhou West
Lake Biological Material Co., Ltd.) (Fig. 3) was implemented with a force of
450 g on each side at an angle of 20-30° downward to the maxillary
plane. Traction lasted for 14 h per day (27). Lateral cephalograms were taken
after about one year of traction.
Measurements and collected
indexes
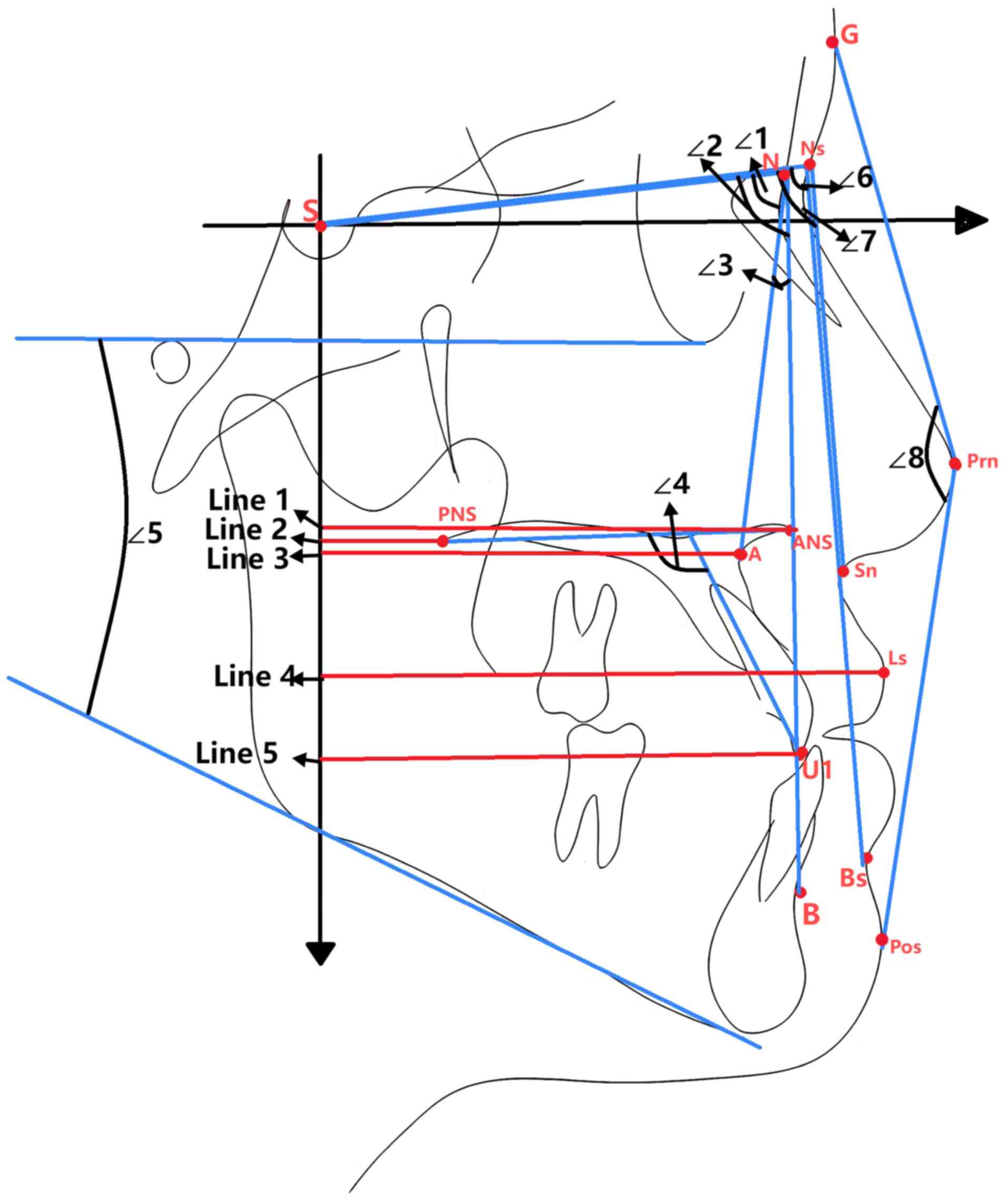
Tracing and lining segment measurements were
performed on lateral cephalograms of each patient prior to
treatment and at the one-year follow-up visit. Based on previous
studies (28,29), the following measurement indicators
were selected (Fig. 4): The
relatively stable horizontal reference (HR) plane (7° downward
rotation of the line connecting the sellar point and nasion point)
and vertical reference (VR) plane (sellar point perpendicular to
the HR plane) were used as horizontal and vertical reference axes,
respectively. The following were measured: Sella-Nasion-A Point
angle (SNA angle), Sella-Nasion-B Point angle (SNB angle), A
Point-Nasion-Point B angle (ANB angle), Upper Anterior
Teeth-Palatal Plane angle (U1-PP angle), Mandibular Plane Angle
(MPA angle), Sella-Nasion-Nasion-Sn Point angle (S-Ns-Sn angle),
Sella-Nasion-Nasion-Bs Point angle (S-Ns-Bs angle),
Glabella-Pronasale-Pogonion of soft tissue angle [Angle of
convexity (G-Prn-Pos angle)], Anterior Nasal-VR plane (ANS-VR),
Posterior Nasal-VR plane (PNS-VR), A Point-VR plane (A-VR), Labial
Superior-VR (Ls-VR) and Upper Anterior Teeth-VR plane (U1-VR).
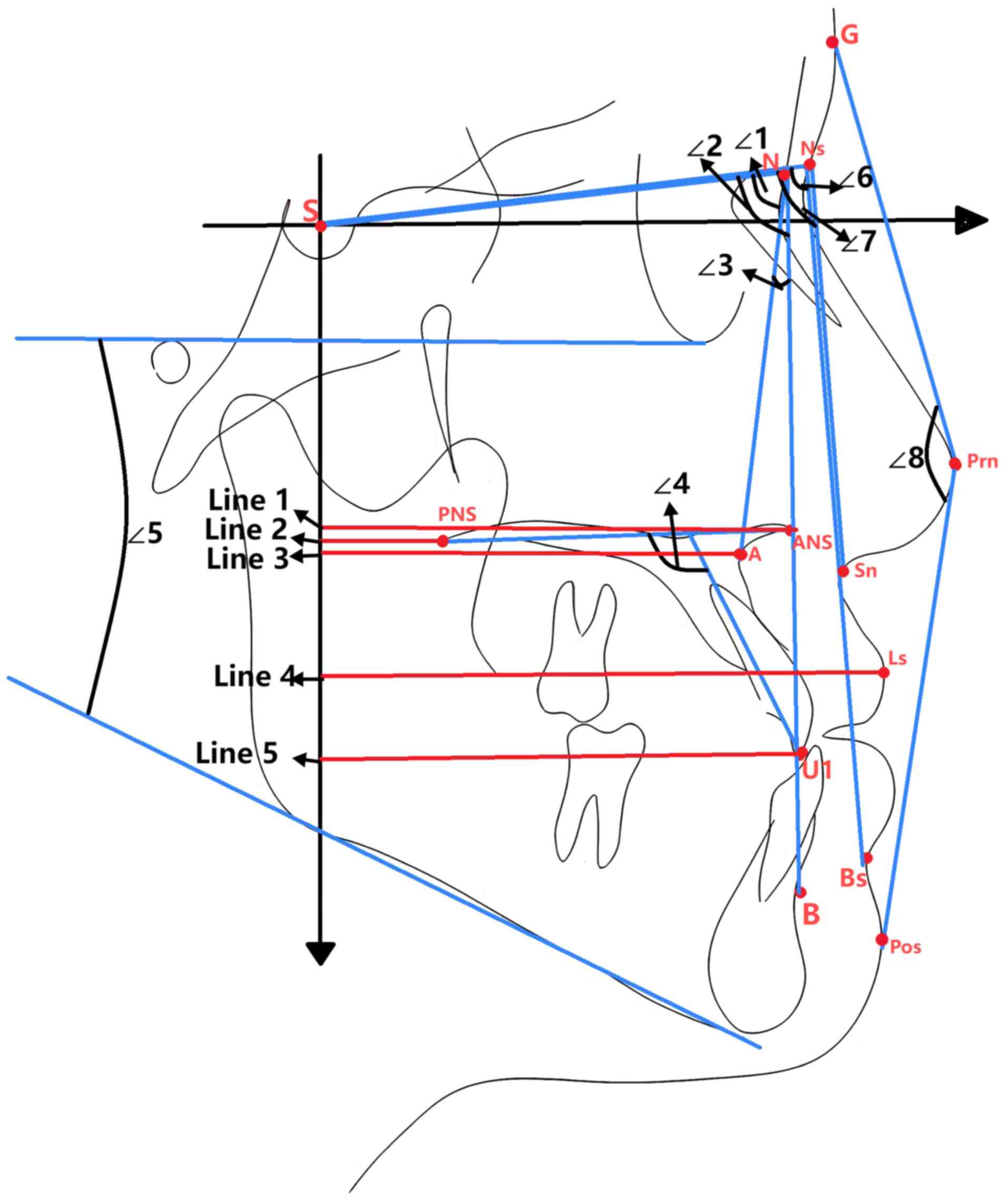 | Figure 4An example of the lateral cephalogram
measurement. ∠1, SNA angle; ∠2, SNB angle; ∠3, ANB angle; ∠4, U1-PP
angle; ∠5, MPA; ∠6, S-Ns-Sn angle; ∠7, S-Ns-Bs angle; ∠8: G-Prn-Pos
angle; line segment 1, ANS-VR; line segment 2, PNS-VR; line segment
3, A-VR; line segment 4, Ls-VR; line segment 5, U1-VR. SNA,
Sella-Nasion-Apoint; SNB, Sella-Nasion-B point; ANB, A
Point-Nasion-Point B; U1-PP, Upper Anterior Teeth Palatal Plane;
MPA, Mandibular Plane Angle; S-Ns-Sn, Sella-Nasion-Nasion-Sn Point;
S-Ns-Bs, Sella-Nasion-Nasion-Bs Point; Angle of convexity
(G-Prn-Pos), Glabella-Pronasale-Pogonion of soft tissue; VR,
Vertical Reference; ANS-VR, Anterior Nasal-VR plane; PNS-VR,
Posterior Nasal VR plane; A-VR, A Point VR plane; Ls-VR, Labial
Superior VR; U1-VR, Upper Anterior Teeth VR plane. |
The same orthodontic doctor positioned and measured
the patients' lateral cephalograms (pre- and post-treatment
cephalograms of the same patient were measured on the same day) to
minimize errors to get a more accurate comparison. The measurements
were performed three times, with the final results presented as the
average of the three measurements.
Statistical analysis
Statistical analysis was conducted using SPSS 25.0
software (IBM Corp.). Measurement data following a normal
distribution were expressed as the mean ± standard deviation. A
paired-samples t-test was used for within-group comparisons and
one-way ANOVA for multiple groups, with the least-significant
differences post hoc t-test for pairwise comparisons between
groups, and a 95% confidence interval was selected. P<0.05 was
considered to indicate a statistically significant difference.
Results
Intra-group comparison of bone indexes
in the three groups before and after treatment
As shown in Table
I, in all three groups, the treatment was associated with a
significant increase in the ANB and SNA angles, a decrease in the
SNB angle and an increase in the MPA (P<0.05). The results
indicated that maxillary anteriorization occurred at the same time
as mandibular anteriorization after treatment, which made certain
data reach the normal level after treatment, like the ANB angle
reaches a positive value in most patients after treatment. The
position of the upper anterior teeth (U1-VR) increased after
treatment.
 | Table IChanges in dental and bony parameters
before and after treatment in the three groups. |
Table I
Changes in dental and bony parameters
before and after treatment in the three groups.
| | Pre-pubertal
group | Pubertal group | Post-pubertal
group |
|---|
| Angle | T1 | T2 | P-value | T1 | T2 | P-value | T1 | T2 | P-value |
|---|
| ANB angle | -2.25±1.97 | 0.95±1.43 | <0.001 | -1.97±0.46 | 1.25±0.32 | <0.001 | -2.04±0.59 | -0.19±0.51 | <0.001 |
| SNA angle | 80.35±3.19 | 82.57±3.35 | 0.007 | 78.67±0.89 | 80.49±0.98 | 0.001 | 79.35±0.83 | 80.27±0.76 | <0.001 |
| SNB angle | 82.75±2.79 | 81.08±2.54 | 0.003 | 80.65±1.09 | 79.26±1.00 | 0.003 | 81.39±1.06 | 80.47±1.00 | 0.005 |
| U1-PP angle | 115.15±1.58 | 116.14±1.18 | 0.475 | 114.93±1.72 | 117.11±1.28 | 0.042 | 117.84±1.24 | 119.63±1.27 | 0.049 |
| MPA angle | 27.46±1.46 | 31.23±0.97 | 0.012 | 30.32±1.19 | 32.29±1.07 | 0.005 | 30.18±0.99 | 31.69±1.08 | 0.011 |
| A-VR | 59.35±1.15 | 61.54±1.19 | 0.001 | 60.91±1.69 | 63.19±2.00 | 0.015 | 60.52±1.25 | 61.89±1.22 | 0.001 |
| ANS-VR | 65.47±1 24 | 67.89±1.16 | 0.001 | 66.78±1.78 | 69.11±2.14 | 0.018 | 66.05±1.12 | 66.59±1.18 | 0.049 |
| PNS-VR | 17.89±0.79 | 19.29±0.79 | <0.001 | 19.64±0.94 | 20.77±1. 00 | 0.030 | 17.69±0.81 | 18.23±0.76 | 0.108 |
| U1-VR | 60.98±2.36 | 63.20±2.41 | 0.001 | 61.89±2.12 | 66.28±2.04 | 0.00 3 | 64.67±1.79 | 67.23±1.89 | 0.001 |
| Ls-VR | 77.09±1.79 | 80.39±1.74 | <0.001 | 79.23±2.21 | 81.82±2.39 | 0.0 09 | 79.29±1.35 | 81.24±1.31 | 0.002 |
| G-Prn-Pos
angle | 144.89±2.25 | 139.94±1.65 | 0.002 | 147.64±2.38 | 143.53±2.15 | <0.001 | 153.89±1.32 | 150.49±1.61 | 0.001 |
| S-Ns-Sn angle | 88.31±0.72 | 90.32±0.87 | 0.002 | 85.80±1.76 | 88.42±1.80 | 0.002 | 84.72±1.69 | 86.19±1.58 | 0.029 |
| S-Ns-Bs angle | 85.07±2.88 | 83.66±3.39 | 0.011 | 85.10±1.09 | 82.69±1.04 | 0.003 | 82.91±1.39 | 81.87±1.43 | 0.023 |
In the pre-pubertal and the pubertal groups,
treatment led to significantly increased indexes of ANS-VR, PNS-VR
and A-VR (P<0.05), indicating that the maxilla grew forward and
moved forward in these two groups. In the post-pubertal group, the
ANS-VR and A-VR increased significantly. By contrast, no such
increase was observed for the PNS-VR [an increase of only 0.54±1.21
mm (P>0.05)], indicating that in the post-pubertal group, the
alveolar bone grew and the maxilla did not move forward. In
addition, the post-pubertal and pubertal groups had a significantly
larger change in the U1-PP Angle than the prepubertal group,
suggesting that lip inclination of the upper anterior teeth
occurred in these two groups due to the action of dental anchorage
(9).
Intra-group comparison of soft tissue
indexes in the three groups before and after treatment
As summarized in Table
I, the G-Prn-Pos angle in the pre-pubertal, pubertal and
post-pubertal groups decreased significantly after the treatment.
In addition, there was a significant increase in the S-Ns-Sn angle
of the upper lip. Furthermore, the S-Ns-Bs angle decreased
significantly (P<0.05). This indicated that the mid-facial
depression was improved and the nasal base position was moved
forward. The Ls-VR, as the index representing the position of the
upper lip, increased significantly, suggesting that the upper lip
had moved forward substantially after treatment (30).
Intergroup comparisons before and
after treatment
There was no statistically significant difference in
any of the indexes between the pre-pubertal and the pubertal
groups. The changes in the ANS-VR and PNS-VR in the post-pubertal
group were significantly different from and the change in the
post-pubertal group was significantly lower than that in the other
two groups. There was no significant difference in the changes in
facial soft tissue among the three groups (Table II).
 | Table IIIntergroup comparison of differences
before and after treatment in the three groups (T2-T1). |
Table II
Intergroup comparison of differences
before and after treatment in the three groups (T2-T1).
| Angle | Pre-pubertal
group | Pubertal group | Post-pubertal
group | P-value |
|---|
| ANB angle | 3.21±1.93 | 3.22±1.84 | 1.85±1.01 | >0.05 |
| SNA angle | 2.21±2.69 | 1.82±1.78 | 0.92±0.77 | >0.05 |
| SNB angle | -1.66±1.76 | -1.39±1.48 | -0.93±1.08 | >0.05 |
| U1-PP angle | 0.99±5.22 | 2.17±3.77 | 1.79±3.21 | >0.05 |
| MPA angle | 3.77±5.09 | 1.97±2.27 | 1.51±2.00 | >0.05 |
| A-VR | 2.18±1.91 | 2.27±3.18 | 1.37±1.19 | >0.05 |
| ANS-VR | 2.43±2.11 | 2.33±3.35 |
0.55±0.98a,b | <0.05 |
| PNS-VR | 1.40±1.19 | 1.13±1.81 |
0.54±1.21c,d | <0.05 |
| U1-VR | 2.87±2.56 | 4.39±4.84 | 2.56±2.46 | >0.05 |
| Ls-VR | 3.29±2.56 | 2.59±3.32 | 1.95±1.92 | >0.05 |
| G-Prn-Pos | -4.95±5.19 | -4.11±3.21 | -3.40±3.25 | >0.05 |
| S-Ns-Sn angle | 2.01±2.03 | 2.61±2.68 | 1.47±2.35 | >0.05 |
| S-Ns-Bs angle | -1.41±1.88 | -2.41±2.65 | -1.04±1.58 | >0.05 |
Discussion
Skeletal class III malocclusion can be classified
into maxillary sagittal deficiency, mandibular overgrowth and mixed
types (31). However, the length
of the mandible is mainly determined by genetics and the mandibular
growth of patients with class III malocclusion has a longer
duration (32). In addition,
clinical studies have shown that chincap appliances therapy for
patients with mandibular overgrowth is not effective in inhibiting
mandibular growth (33).
Therefore, the early treatment of skeletal class III malocclusion
mainly focuses on the sagittal deficiency of the maxilla to
stimulate its growth and development (25), and the treatment of rapid expansion
combined with maxillary protraction is the most common.
Patients with overgrowth of the mandible were
excluded from the present study. The results of this study showed
that rapid maxillary expansion combined with protraction could
improve the sagittal imbalance of the upper and lower jaws, correct
the malocclusion of the anterior teeth and improve the facial
profile of the patients in three different growth and development
stages within ~1 year. However, the bone and dental effects differ
in patients of various ages after treatment. The results revealed
that the ANB angles of the pre-pubertal and pubertal patients
reached normal values after the treatment. By contrast, the ANB
angles of patients in the post-pubertal group significantly
increased after rapid expansion combined with maxillary protraction
therapy for ~1 year. However, certain patients did not attain the
normal range. In this study, the sagittal changes of the A point
were significant in all three groups. The changes in the A-VR were
2.18±1.91, 2.27±3.18 and 1.37±1.19 mm in the pre-pubertal, pubertal
and post-pubertal groups, respectively. The change in the SNA angle
in the three groups was 2.21±2.69, 1.82±1.78 and 0.92±0.77°,
respectively, and the differences before and after treatment within
each of the groups were statistically significant (P<0.05).
Baccetti et al (34)
observed untreated patients with class III malocclusion and
demonstrated that the change value of point A was only 0.5±2.1 mm
during the natural growth (from CVM stage I to stage VI). This
indicates that even after removing the effects of growth and
development, the A point of all three groups experienced a growth
promotion after protraction treatment. However, the forward
movement of point A does not match the forward movement of the
maxilla, and point A represents the alveolar effect rather than the
bone effect (35). A previous
study compared 26 patients with class III malocclusion treated with
forward distraction with 15 patients with class III malocclusion
without the treatment and concluded that the most significant
change in the movement of the maxillary complex after forward
distraction treatment was the movement of the posterior nasal spine
and pterygomaxillary fissure points (36). This parameter represented the
overall movement of the maxilla, which was the expected bone effect
of forward distraction treatment. In the present study, the PNS-VR
changed significantly after the treatment in the pre-pubertal
(1.40±1.19 mm) and the pubertal group (1.13±1.81 mm). At the same
time, the U1-VR value, representing the dental changes, also
considerably changed in the two groups. Comparison of the changes
in PNS-VR, A-VR and U1-VR revealed an order of magnitude of U1-VR
> A-VR > PNS-VR in the pre-pubertal and pubertal groups.
These results indicate that the forward traction treatment led to
the maxilla moving forward and caused a certain degree of alveolar
reaction due to the forward movement of the upper anterior teeth.
In addition, a study provided a 3D finite element analysis of
tooth-anchored maxillary protraction and bone-anchored maxillary
protraction, showing that both dental and bony anchorage have
forces on the position of the bonded fixed molar and the occurrence
of dental effects is difficult to avoid (37). In the present study, the treatment
led to a slight insignificant change in the PNS point in the
post-pubertal group (0.54±1.21 mm), while the A and the ANS points
changed significantly [1.45±0.87 and 0.72±0.55 mm, respectively].
The results suggest that there was only small maxillary movement in
the post-pubertal group, but the alveolar response was larger. Cha
(38) also found that 84.0% of
bone remodeling and 16.0% of alveolar remodeling were observed in
patients at the growth peak. By contrast, in the late stages of
growth, 63.6% of the patients had bone remodeling and 36.4% had
alveolar remodeling. The results of comparisons among the three
groups of patients showed that the PNS-VR of the patients in the
post-pubertal group was significantly smaller than that in the
other two groups (P<0.05), further indicating that the bone
effect of the treatment in the post-pubertal group was worse than
that in the other two groups.
Previously, a U1-SN angle was used to reflect the
labial inclination effect of the upper anterior teeth. However,
both the palatal plane rotation and the labial inclination of the
upper anterior teeth caused a change in the U1-SN angle (27). Therefore, in the present study, the
U1-PP angle was selected to remove the influence of the palatal
plane rotation and better represent the labial inclination of the
upper anterior teeth. The present results showed that the U1-PP
angle increased by 2.17+3.77 and 1.79±3.21° in the pubertal and the
post-pubertal groups, respectively (P<0.05). However, no
significant change was observed in the pre-pubertal group of
patients, which differed from previous studies (39). There are several possible reasons
for this discrepancy. First, most patients in the pre-pubertal
group of this study were in the early mixed dentition stage.
Furthermore, the bone effect of rapid maxillary expansion was more
significant in the early stage of growth and development (40), and more space was obtained in the
upper anterior tooth area, which reduced the crowding of the upper
anterior teeth and caused the self-retraction of the upper anterior
teeth that initially compensated for lip inclination. Combined with
the bone and dental effects, for the patients in the pre-pubertal
group, the bone effect was obvious and the dental effect was small
after treatment; for the patients in the pubertal group, a good
bone effect was obtained after treatment, but the phenomenon of
dental compensation also occurred; for the patients in the
post-pubertal group, the treatment produced a small amount of bone
effect but a significant dental effect. Therefore, for
post-pubertal patients whose upper anterior teeth have been
compensated by lip inclination, measures such as bone anchorage or
alternate rapid maxillary expansion and contraction should still be
selected to increase the bony effect (29,41).
As the maxillary complex moves, the overlying
midface soft tissue changes accordingly (42). Regarding concave profile changes,
G-Prn-Pos angle, which represents facial prominence, was
significantly reduced in all three groups, indicating that midface
depression was improved after forward traction, and the profile
gradually tended toward the type I facial profile. The present
results were consistent with the conclusions of most previous
studies. A study by Pavoni et al (43) included untreated skeletal class III
malocclusion patients as a control group. It showed that the facial
process angle of the untreated class III patients increased,
indicating that the concave facial pattern would become more
serious if left untreated. This study found that following the
treatment, the upper lip position of patients moved forward due to
the movement of the naso-maxillary complex and the upper front
teeth, resulting in a gradual coordination between the upper and
lower lips. This is similar to the conclusion of Li et al
(30). Çelebi and Çelikdelen
(44) found that rapid expansion
combined with anterior distraction can lead to maxillary and dental
changes in skeletal class III patients, and changes in bone bring
changes in soft tissue. Forward and downward movement of the
maxilla is helpful to improve class III facial type. In contrast to
the skeletal parameters, no significant treatment-related
differences were found in the soft tissue parameters between the
post-pubertal, the pre-pubertal and the pubertal groups, indicating
that the skeletal advancement and the dental compensation had
similar effects on the improvement of the facial profile after the
traction treatment.
The current study has significant clinical
implications. It is inevitable to encounter skeletal class III
malocclusion patients in the late stage of growth and development
in clinical practice. However, certain patients and their families
may decline combined orthodontic-orthognathic treatment in
adulthood due to various reasons, such as the high cost of the
treatment. Such patients may prefer non-invasive treatment to
improve their facial shape and occlusion. This study contributes to
a better understanding of whether traditional treatment methods can
be used for such patients to achieve patient satisfaction, reduce
pain to a certain extent and avoid orthognathic surgery in
adulthood. The results of the present comprehensive study showed
that, although the skeletal effect of the patients in the
post-pubertal group was not as good as that of the patients in the
pre-pubertal and pubertal groups, their class III malocclusion was
also significantly improved (ANB angle increased by 1.85±1.01°
after treatment, and the ANB angle after treatment was-0.19±0.51°).
At the same time, a good treatment effect was achieved from the
soft tissue point of view (the G-Prn-Pos Angle increased by
3.40±3.25°), which was acceptable for the patients. Therefore, if
invasive treatments such as bone anchorage rapid expansion and
traction or orthodontic treatment are not considered, rapid
expansion combined with maxillary protraction therapy can also mask
the facial defects of patients with mild maxillary deficiency in
the post-pubertal stage.
Of note, the present study has certain limitations.
It is a retrospective study with a small sample size. Additionally,
the study lacked a control group of untreated class III
malocclusion patients, and the influence of growth and development
could not be fully excluded, highlighting the need for further
research.
In conclusion, treating patients with skeletal class
III malocclusion at different growth stages using protraction
combined with rapid maxillary expansion could efficiently correct
the sagittal jaw imbalance, improve unfavorable facial profiles and
achieve favorable therapeutic outcomes. Of note, substantial bone
effects were observed in the pre-pubertal and pubertal groups. By
contrast, the bone effects were diminished, and alveolar and dental
reactions were prominent after the growth peak period.
Nevertheless, improved facial aesthetics still benefit patients'
physical and mental health.
Acknowledgements
Not applicable.
Funding
Funding: The study was supported by the Research Fund of the
Zhejiang Provincial Education Department (grant no. Y202249619) and
the Postgraduate Research Innovation Project of Bengbu Medical
College (grant no. Byycx22149).
Availability of data and materials
The datasets used and/or analyzed during the current
study may be requested from the corresponding author.
Authors' contributions
XY conceived and designed the study. YC collected
the data. CM and WZ performed the analysis. XY was involved in
writing the manuscript. XY and YC confirm the authenticity of all
the raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
This retrospective study was approved by the Ethics
Committee of the Second Affiliated Hospital of Jiaxing University
(Jiaxing, China; approval no. JXEY-2022JYT006; date, 9th October
2022). Each patient's legal guardian provided written informed
consent before the treatment.
Patient consent for publication
The legal guardian of the patient depicted in
Fig. 3 provided written consent
for publication of the patient image.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zere E, Chaudhari PK, Sharan J, Dhingra K
and Tiwari N: Developing class III malocclusions: Challenges and
solutions. Clin Cosmet Investig Dent. 10:99–116. 2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Mehdipour A, Khosroshahian S, Pourhossein
H, Mohammadbeigi A and Karimi A: Prevalence and association of
temporomandibular disorders with malocclusion and anxiety in
children and adolescents: A cross-sectional observational study.
Gen Dent. 70:65–71. 2022.PubMed/NCBI
|
|
3
|
Shroff B: Malocclusion as a cause for
temporomandibular disorders and orthodontics as a treatment. Oral
Maxillofac Surg Clin North Am. 30:299–302. 2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Yoon SY, Song JM, Kim YD, Chung IK and
Shin SH: Pusan Korea Pusan National University. Clinical changes of
TMD and condyle stability after two jaw surgery with and without
preceding TMD treatments in class III patients. Maxillofac Plast
Reconstr Surg. 37(9)2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Duarte V, Zaror C, Villanueva J, Werlinger
F, Vidal C, Solé P, O Ryan JA, Requena R, Dallaserra M, Rojas R, et
al: Changes in health-related quality of life after orthognathic
surgery: A multicenter study. Clin Oral Investig. 26:3467–3476.
2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Bernabé E, Sheiham A and de Oliveira CM:
Condition-specific impacts on quality of life attributed to
malocclusion by adolescents with normal occlusion and class I, II
and III malocclusion. Angle Orthod. 78:977–982. 2008.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Dogan E and Seckin O: Maxillary
protraction in patients with unilateral cleft lip and palate:
Evaluation of soft and hard tissues using the Alt-RAMEC protocol. J
Orofac Orthop. 81:209–219. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Fu L, Yu J and Lv H: The clinical effect
of anterior distraction combined with arch expansion in the
treatment of skeletal class III malocclusion in mixed dentition
aged 8 to 11 years old. Chin Mod Med. 29:120–123+127. 2022.(In
Chinese).
|
|
9
|
Seiryu M, Ida H, Mayama A, Sasaki S,
Sasaki S, Deguchi T and Takano-Yamamoto T: A comparative assessment
of orthodontic treatment outcomes of mild skeletal class III
malocclusion between facemask and facemask in combination with a
miniscrew for anchorage in growing patients: A single-center,
prospective randomized controlled trial. Angle Orthod. 90:3–12.
2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Büyükçavuş MH: Alternate rapid maxillary
expansion and constriction (Alt-RAMEC) protocol: A comprehensive
literature review. Turk J Orthod. 32:47–51. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Sung SJ and Baik HS: Assessment of
skeletal and dental changes by maxillary protraction. Am J Orthod
Dentofacial Orthop. 114:492–502. 1998.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Manzoor Mughal A, Hassan N and Ahmed A:
Bone age assessment methods: A critical review. Pak J Med Sci.
30:211–215. 2014.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Cavallo F, Mohn A, Chiarelli F and
Giannini C: Evaluation of bone age in children: A mini-review.
Front Pediatr. 9(580314)2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kumar V, Patil K and Munoli KB:
Comparative evaluation of dental age, bone age, and chronological
age in the human immunodeficiency virus positive children. J Pharm
Bioallied Sci. 6 (Suppl 1):S90–S96. 2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Mays S: The effect of factors other than
age upon skeletal age indicators in the adult. Ann Hum Biol.
42:332–341. 2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Carel JC, Lahlou N, Roger M and Chaussain
JL: Precocious puberty and statural growth. Hum Reprod Update.
10:135–147. 2004.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Wit JM: Should skeletal maturation be
manipulated for extra height gain? Front Endocrinol (Lausanne).
12(812196)2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Arisaka O, Nakayama Y, Tokita A and Yabuta
K: Bone mineralization and bone maturation in precocious puberty.
Arch Pediatr Adolesc Med. 151:101–102. 1997.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Jang HI, Kim SC, Chae JM, Kang KH, Cho JW,
Chang NY, Lee KY and Cho JH: Relationship between maturation
indices and morphology of the midpalatal suture obtained using
cone-beam computed tomography images. Korean J Orthod. 46:345–355.
2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Szemraj A, Wojtaszek-Słomińska A and
Racka-Pilszak B: Is the cervical vertebral maturation (CVM) method
effective enough to replace the hand-wrist maturation (HWM) method
in determining skeletal maturation?-A systematic review. Eur J
Radiol. 102:125–128. 2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Zhang X, He JM and Zheng WY: Comparison of
rapid maxillary expansion and pre-fabricated myofunctional
appliance for the management of mouth breathers with class II
malocclusion. Eur Rev Med Pharmacol Sci. 25:16–23. 2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
McNamara JA Jr: A method of cephalometric
evaluation. Am J Orthod. 86:449–469. 1984.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Jarabak JR and Fizzel JA: Technique and
treatment with light wire edgewise appliances. 2nd edition. St.
Louis: Mosby, 1972.
|
|
24
|
Baccetti T, Franchi L and McNamara JA Jr:
The cervical vertebral maturation (CVM) method for the assessment
of optimal treatment timing in dentofacial orthopedics. Semin
Orthod. 11:119–129. 2005.
|
|
25
|
Tarraf NE, Dalci O, Dalci K, Altug AT and
Darendeliler MA: A retrospective comparison of two protocols for
correction of skeletal class III malocclusion in prepubertal
children: Hybrid hyrax expander with mandibular miniplates and
rapid maxillary expansion with face mask. Prog Orthod.
24(3)2023.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Miner RM, Al Qabandi S, Rigali PH and Will
LA: Cone-beam computed tomography transverse analyses. Part 2:
Measures of performance. Am J Orthod Dentofacial Orthop.
148:253–263. 2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Wen X, Yang C and Qian Y: Evaluation of
the effect of maxillary protraction in patients with maxillary
hypoplasia at different stages. Chin J Pract Stomatol. 15:551–557.
2022.(In Chinese).
|
|
28
|
Kircelli BH and Pektas ZO: Midfacial
protraction with skeletally anchored face mask therapy: A novel
approach and preliminary results. Am J Orthod Dentofacial Orthop.
133:440–449. 2008.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Lee SH, Koh SD, Chung DH, Lee JW and Lee
SM: Comparison of skeletal anchorage and tooth-borne maxillary
protraction followed by fixed appliance in class III malocclusion.
Eur J Orthod. 42:193–199. 2020.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Li J, Qi Y, Zhang X, Liu D, Li J and Zhang
L: Maxillary protraction and rapid palatal expansion on the facial
soft tissue changes for class III skeletal malocclusion
patients-CNKI. Clin Res. 02:38–41. 2023.(In Chinese).
|
|
31
|
Li C, Cai Y, Chen S and Chen F:
Classification and characterization of class III malocclusion in
Chinese individuals. Head Face Med. 12(31)2016.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Doraczynska-Kowalik A, Nelke KH, Pawlak W,
Sasiadek MM and Gerber H: Genetic factors involved in mandibular
prognathism. J Craniofac Surg. 28:e422–e431. 2017.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Liu W, Zhou Y, Wang X, Liu D and Zhou S:
Effect of maxillary protraction with alternating rapid palatal
expansion and constriction vs. expansion alone in maxillary
retrusive patients: A single-center, randomized controlled trial.
Am J Orthod Dentofacial Orthop. 148:641–651. 2015.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Baccetti T, Franchi L and McNamara JA:
Growth in the untreated class III subject. Semin Orthod.
13:130–142. 2007.
|
|
35
|
De Clerck H, Cevidanes L and Baccetti T: .
Dentofacial effects of bone-anchored maxillary protraction: a
controlled study of consecutively treated Class III patients. Am J
Orthod Dentofacial Orthop. 138:577–81. 2010.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Baccetti T, De Clerck HJ, Cevidanes LH and
Franchi L: Morphometric analysis of treatment effects of
bone-anchored maxillary protraction in growing class III patients.
Eur J Orthod. 33:121–125. 2011.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Bai L, Bao H, Xie N, Ge Y and Zhu X:
Three-dimensional finite element analysis of the effects of three
types of rapid maxillary expansion combined with protraction. Chin
J Stomatol. 41:32–37. 2021.(In Chinese).
|
|
38
|
Cha KS: Skeletal changes of maxillary
protraction in patients exhibiting skeletal class III malocclusion:
A comparison of three skeletal maturation groups. Angle Orthod.
73:26–35. 2003.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Li X: The effect of protraction for
skeletal class III malocclusion at various time: A meta-analysis,
2021.
|
|
40
|
Chen YN, Yang XW and Zheng WY: Comparison
of patients with different cervical spine bone ages before and
after arch expansion treatment based on cone-beam computed
tomography. Eur Rev Med Pharmacol Sci. 27:1269–1277.
2023.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Masucci C, Franchi L, Franceschi D,
Pierleoni F and Giuntini V: Post-pubertal effects of the
Alt-RAMEC/FM and RME/FM protocols for the early treatment of class
III malocclusion: A retrospective controlled study. Eur J Orthod.
44:303–310. 2022.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Moshkelgosha V, Raoof A, Sardarian A and
Salehi P: Photogrammetric comparison of facial soft tissue profile
before and after protraction facemask therapy in class III children
(6-11 years old). J Dent (Shiraz). 18:7–16. 2017.PubMed/NCBI
|
|
43
|
Pavoni C, Gazzani F, Franchi L, Loberto S,
Lione R and Cozza P: Soft tissue facial profile in class III
malocclusion: Long-term post-pubertal effects produced by the face
mask protocol. Eur J Orthod. 41:531–536. 2019.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Çelebi F and Çelikdelen M: Comparison of
the Changes following two treatment approaches: Rapid Maxillary
expansion versus alternate rapid maxillary expansion and
constriction. Turk J Orthod. 33:1–7. 2020.PubMed/NCBI View Article : Google Scholar
|