Introduction
Patients with blunt chest trauma commonly experience
rib fractures. In turn, these fractures are associated with
sequelae and organ damage, thus increasing the morbidity and
mortality risks. It has been reported that >250,000 individuals
attend the emergency services in the United States, annually, due
to rib fractures (1). Most
patients with rib fractures are treated with conservative care. On
the other hand, >30% of the above patients suffer from long-term
disability that prevents them from holding down a full-time job,
while up to 50% of patients, particularly those with combination
injuries, such as flail chest, can experience chronic pain or chest
wall deformities (2). In addition,
10-20% of patients who suffer physical trauma have rib fractures,
which is the most common type of bone fracture. In extreme
situations, these fractures can cause concurrent damage to the
abdominal organs (3). In addition
to trauma, rib fractures can result from medical procedures or from
coughing, particularly in individuals with low bone density
(4). In addition, ~40% of patients
with acute chest trauma present with rib fractures, which are
commonly seen in cases of chest trauma (5).
Flail chest is known as the condition where one side
of the chest has more than three successive rib fractures with at
least two fracture lines per rib (6). Multiple rib fractures and flail chest
are considered distinct injuries and are synthesized independently
for every extracted result (7).
Patients with rib fractures present with a wide range of clinical
symptoms. Certain patients who meet the diagnostic criteria for a
flail chest may not exhibit aberrant breathing and they are
therefore well managed with respect to their discomfort (8). Multiple rib fractures with flail or
non-flail chest should be clearly distinguished, as the latter is
associated with a higher mortality rate and considerable morbidity
(9). The use of plating systems
for rib stabilization has shown promising results in reducing both
the short- and long-term consequences of rib fractures, such as the
occurrence of pneumonia, the requirement for a tracheostomy,
prolonged hospital stay, increased dependence on painkillers and
flail chest-related death (10).
In general, rib fractures are treated and managed
with supportive measures, such as administration of local and
systemic analgesics, airway clearance techniques, tube thoracostomy
when pneumothorax or hemothorax is present and artificial breathing
or surgery to reduce discomfort (11). A previous study demonstrated that
the flail section was necessary for paradoxical chest wall motion;
however, it was not sufficient for treating flail chest type rib
fractures (12). The results of
the most recent randomized controlled trial indicated that,
although several previous small, non-randomized cohort studies
supported the use of surgical fixation for improving pain and
quality of life of patients with non-flail rib fractures, surgical
stabilization of rib fractures allowed only a small proportion of
patients to return to their work (13-15).
Rib fixation for flail chest could improve the short-term outcomes,
with the use of clinical results and implications of fixation.
However, which patient subgroup is most likely to benefit from this
technique has remained elusive (16).
Therefore, the present study aimed to analyze the
effectiveness of the surgical treatment strategy in patients with
non-flail chest type of multiple rib fractures at a multivariate
level.
Patients and methods
Patients and diagnosis
In the current randomized study, a total of 40
patients with multiple rib fractures and treated either
conservatively (n=20) or with open surgical fixation (n=20) were
prospectively enrolled from the were prospectively enrolled from
the Adıyaman Training and Research Hospital Thoracic Surgery Clinic
(Adıyaman, Türkiye) between April 2013 and December 2019. In the
emergency clinic, all patients were subjected to three-dimensional
computed tomography of the thorax, abdomen and skull. Patients with
poor oxygen saturation and high injury score were monitored in the
intensive care unit for the first 2-4 days. The remaining patients
received treatment at the Thoracic Surgery clinic. Each patient
underwent clinical and laboratory evaluation. A chest tube was
inserted in every patient who experienced pneumothorax or
hemothorax. In addition, internal or external stabilization of the
limb fractures was performed. On the first or second day after the
first hospitalization, the pain scale scores (17) and respiratory function test
(18) results were recorded.
Feeling comfortable was a dicothomous parameter with ‘yes’ or ‘no’
as the answers selected. Injury Severity Score was used for injury
severity of patients (17). The
total of 40 patients were randomly allocated into two groups,
namely the surgery and conservative therapy groups. The inclusion
criteria were as follows: i) Patients with a mean Injury Severity
Score of 9-18; ii) those with 3-6 fractured ribs, with at least two
being displaced; iii) those with no other complications or drug
administration, which could have affected the results of the study;
and iv) those without serious pulmonary contusion, and any head and
abdominal trauma. Accordingly, if a patient received conservative
therapy, they were then subjected to surgery fixation. Patients who
refused surgery were only treated with conservative therapy and
were included in the conservative therapy group.
A power analysis was performed as previously
described by Li et al (6)
using GPower 3.1.9.2 software (Franz Faul). An effect size of 0.55
was obtained. Based on the above effect size, 95% confidence
interval and Alpha level of 0.05, the minimum patient number for
the study and control groups was 38 (critical t=1.69).
Ethical approval
The present study was approved by the İnönü
University Medical School Ethics Committee (Battalgazi, Türkiye).
All patients in the surgery group were informed about the surgical
procedure and provided written informed consent to undergo surgery.
Since there was no ethics committee at Adıyaman Training and
Research Hospital (Adıyaman, Türkiye), where the data were
collected, the corresponding author applied for and received ethics
committee approval from the nearest academic institution, İnönü
University (Battalgazi, Türkiye). Later, the corresponding author
changed institutions.
Conservative therapy
For analgesic management, narcotic (tramadol,
pethidine) and non-narcotic (paracetamol, diclofenac sodium)
analgesics were used. All patients in the two groups were daily
administered 300 mg intravenous tramadol combined with 3 g
intravenous paracetamol as part of an analgesic management regimen
(19,20). Further intravenous doses of
pethidine (150 mg/day) and diclofenac sodium (225 mg/day) were
administered to particular patients with inadequate pain control
(21,22). For analgesic management, drug
additives (including pharmacological and individual agents for
enhance of physicochemical properties, such as solvent systems)
were used, including intravenous injection of 300 mg tramadol daily
in combination with intravenous infusion of 3 g paracetamol each
day. Treatment for secretion retention included expectorant
therapy, bronchodilator therapy, respiratory physiotherapy and
tracheal aspiration.
Surgery treatment
A single lumen intubation was used for the surgery.
To identify any broken ribs and fix displaced ones with titanium
rib clips, incisions were made based on the location of the
fracture. Following surgery, the patients were transferred to an
intensive care or service unit.
Data set
Age, sex, etiology, accompanied pathologies,
additional interventions, injury severity score, number of
fractured and displaced ribs, pain scale, respiratory function
values, analgesic doses and hospitalization duration were recorded
and analyzed. Pain scale scoring and respiratory function tests
were repeated prior to discharge. The aforementioned factors were
analyzed and compared using the registration system. After
discharge, pulmonary function tests were carried out in an
outpatient clinic and the results were analyzed to evaluate
long-term treatment efficacy. Hospitalization duration, feeling
comfortable, return to workplace, pain and occurrence of
complications were the primary outcome measures of the present
research.
Statistical analysis
Nominal and ordinal parameters were expressed as
frequencies, while continuous variables were expressed as the mean
± standard deviation. The Kolmogorov-Smirnov test was applied to
test for normality of the scale parameters (23). An independent-samples t-test was
carried out to assess the normally distributed scale parameter
differences, while the Mann-Whitney U-test was performed to assess
the non-normally distributed scale parameter differences. The
differences between nominal and ordinal parameters in the two
groups were compared with the Chi-squared test. Spearman's rho
correlation analysis was performed to evaluate the correlation
between different parameters. Due to linearization deviations, a
Generalized Linear Model (Logit) was used for effect analysis
(23,24). All statistical analyses were
performed using SPSS 25.0 (IBM Corp.). P<0.05 was considered to
indicate a statistically significant difference.
Results
Differences in baseline
characteristics between the surgery and conservative treatment
groups
The mean age of the conservative group was
55.60±18.68 and was 55.90±13.97 in the surgery group. A total of 19
males (95%) and 1 female (5%) were included in the conservative
group and 17 males (85%) and 3 females (15%) were included in the
surgery group. Age, sex, the number of fractured and displaced
ribs, injury severity score, chest abbreviated score, forced
expiratory volume in one second (FEV1), narcotic drug dose, long
term FEV and forced vital capacity (FVC) levels, drug additives and
American Society of Anesthesiologists (ASA) scores were not
significantly different between the conservative treatment and
surgery groups (17-20)
(P>0.05; Table I). In addition,
there were no significant differences between the conservative
treatment and surgery groups in terms of hospitalization duration,
feeling comfortable, follow-up duration, time to return to work and
discharge pain score, or pneumothorax and pleural empyema incidence
(P>0.05; Table II).
 | Table IBaseline characteristics of patient
groups and differences between conservative and surgery method
groups. |
Table I
Baseline characteristics of patient
groups and differences between conservative and surgery method
groups.
| Item | Conservative
(n=20) | Surgery (n=20) | P-value |
|---|
| Age, years | 55.60±18.68
(41.50-71.00) | 55.90±13.97
(48.50-65.50) | 0.954a |
| Sex | | | 0.282b |
|
Males | 19 (95.0) | 17 (85.0) | |
|
Females | 1 (5.0) | 3 (15.0) | |
| Number fractured
ribs | 4.60±0.99 4.00
(3.00-6.00) | 5.15±0.93 5.00
(3.00-6.00) | 0.076c |
| Number of displaced
ribs | 2.85±0.67 3.00
(2.00-4.00) | 3.05±0.83 3.00
(2.00-5.00) | 0.529c |
| Injury severity
score | 10.80±3.69 9.00
(9.00-18.00) | 10.90±3.52 9.00
(9.00-18.00) | 0.883c |
| Chest abbreviated
score | 5.60±1.35 6.00
(3.00-9.00) | 5.60±1.10 6.00
(3.00-7.00) | 0.841c |
| FEV1 | 0.55±0.43
(0.22-0.74) | 0.47±0.31
(0.24-0.65) | 0.526a |
| FEV1 percentage | 11.95±9.53 11.00
(1.00-35.00) | 13.70±9.71 9.50
(3.00-38.00) | 0.529c |
| FEV1 improvement,
change | 0.50±0.37 0.37
(0.02-1.42) | 0.42±0.22 0.39
(0.10-0.84) | 0.841c |
| FEV1 improvement
% | 14.10±11.25 10.00
(1.00-40.00) | 15.40±8.93 11.50
(3.00-34.00) | 0.414c |
| Narcotic drug dose,
mg | 22.10±24.58 17.00
(0.00-80.00) | 46.40±51.97 24.00
(0.00-180.00) | 0.149c |
| Long-term FEV | 1.88±0.73 1.71
(0.54-3.08) | 1.68±0.55 1.70
(0.55-2.73) | 0.461c |
| Long-term FVC | 2.35±0.62 2.04
(1.22-3.18) | 2.08±0.77 1.93
(0.81-3.62) | 0.183c |
| Drug additive | 11 (55.0) | 15 (75.0) | 0.185b |
| ASA score | | | |
|
1-2 | 18 (90.0) | 17 (85.0) | 0.632b |
|
>2 | 2 (10.0) | 3 (15.0) | |
 | Table IITreatment outputs and differences
between conservative and surgery method groups. |
Table II
Treatment outputs and differences
between conservative and surgery method groups.
| Item | Conservative
(n=20) | Surgery (n=20) | P-value |
|---|
| Hospitalization
duration, days | 8.20±3.89 | 8.95±3.59 | 0.530a |
| | 8.00
(3.00-18.00) | 9.50
(3.00-15.00) | |
| Feeling
comfortable | 6 (30.0) | 5 (25.0) | 0.723b |
| Follow-up duration,
days | 11.85±7.69 | 9.25±9.12 | 0.108c |
| | 9.00
(2.00-24.00) | 5.00
(1.00-28.00) | |
| Return to
workplace | 61.35±32.79 | 42.75±19.63 | 0.052c |
| | 60.00
(5.00-120.00) | 30.00
(15.00-90.00) | |
| Pain | 3.90±1.94 | 4.85±1.95 | 0.149c |
| | 3.50
(1.00-7.00) | 5.00
(1.00-9.00) | |
| Pneumotorax | 2 (10.0) | 1 (5.0) | 0.545b |
| Pleural
empyema | 2 (10.0) | 1 (5.0) | 0.545b |
| Infection of
osteosynthesis material | 1 (5.0) | - | N/A |
Correlation analysis results
The Spearman's rho correlation analysis results
showed that the pain score was significantly associated with the
FEV1 (r=0.499; P<0.05), drug additives (r=-0.445; P<0.05) and
hospitalization duration (r=0.559; P<0.05) in the conservative
treatment group. By contrast, the discharge pain level was notably
associated with narcotic drug using (r=0.478; P<0.05) and drug
additives (r=0.618; P<0.01) in the surgery group (Table III; Fig. S1, Fig. S2, Fig. S3 and Fig. S4).
 | Table IIISpearman's rho correlation analysis
between discharge pain level and baseline characteristics of
patient groups. |
Table III
Spearman's rho correlation analysis
between discharge pain level and baseline characteristics of
patient groups.
| Item | Conservative, rho
value (n=20) | Surgery, rho value
(n=20) |
|---|
| Sex | 0.244 | 0.123 |
| Number fractured
ribs | 0.062 | 0.371 |
| Number displaced
ribs | 0.174 | 0.077 |
| Injury Severity
Score | -0.011 | 0.057 |
| Chest Abbreviated
Score | 0.112 | 0.184 |
| FEV1 | 0.499a | 0.016 |
| FEV1
percentage | 0.291 | 0.037 |
| FEV1
improvement | 0.327 | 0.229 |
| FEV1 improvement
percentage | 0.178 | 0.233 |
| Narcotic drug
dose | -0.340 | 0.478a |
| Drug additive | -0.445a | 0.618b |
| Non-narcotic
diclofenac | 0.234 | 0.358 |
| Non-narcotic
paracetamol | 0.214 | -0.294 |
| Hospitalization
duration | 0.559a | 0.346 |
| Follow-up
duration | -0.241 | 0.046 |
| Long-term FEV | 0.149 | -0.095 |
| Long-term FVC | 0.021 | -0.062 |
| Return to
workplace | -0.129 | 0.110 |
| Feeling
comfortable | -0.039 | 0.051 |
| Age | -0.203 | -0.160 |
| ASA score | 0.000 | 0.209 |
| Pneumothorax | -0.103 | -0.121 |
| Pleural
empyema | -0.221 | -0.342 |
| Infection of
osteosynthesis material | -0.244 | N/A |
Nonlinear regression analysis
Generalized linear model (Logit) analysis revealed a
statistically significant association between hospitalization
duration and discharge pain levels in the conservative group
(B=0.237; P<0.01). Additionally, in the surgery group, the
effect of drug additives on discharge pain levels was also
statistically significant (B=-2.547; P<0.01). However,
multivariate analysis indicated that the number of fractured and
displaced ribs did not significantly affect the pain level in both
groups (Table IV).
 | Table IVGeneralized linear model (Logit)
analysis for effects of significantly correlated factors on
discharge pain levels according to treatment methods. |
Table IV
Generalized linear model (Logit)
analysis for effects of significantly correlated factors on
discharge pain levels according to treatment methods.
| A, Conservative
group (n=20) |
|---|
| | 95% Wald confidence
interval | Hypothesis
test |
|---|
| Parameter | Beta | Std. error | Lower | Upper | Wald
Chi-square | df | P-value |
|---|
|
Intercepta | 1.100 | 0.791 | -0.451 | 2.651 | 1.931 | 1 | 0.165 |
| Drug additive | 0.940 | 0.680 | -0.393 | 2.273 | 1.910 | 1 | 0.167 |
| FEV1 | 0.784 | 0.803 | -0.790 | 2.358 | 0.954 | 1 | 0.329 |
| Hospitalization
duration | 0.237 | 0.088 | 0.066 | 0.409 | 7.350 | 1 | 0.007 |
| Scaleb | 1.991 | 0.629 | 1.071 | 3.699 | - | - | - |
| B, Surgery group
(n=20) |
| | 95% Wald confidence
interval | Hypothesis
test |
| Parameter | Beta | Std. error | Lower | Upper | Wald
Chi-square | df | P-value |
|
Intercepta | 5.347 | 0.613 | 4.145 | 6.549 | 76.028 | 1 | <0.001 |
| Drug additive | -2.547 | 0.904 | -4.320 | -0.775 | 7.932 | 1 | 0.005 |
| Narcotic drug
dose | 0.003 | 0.008 | -0.012 | 0.018 | 0.151 | 1 | 0.698 |
| Scaleb | 2.210 | 0.699 | 1.189 | 4.107 | - | - | - |
| C, Entire sample
(n=40) |
| | 95% Wald confidence
interval | Hypothesis
test |
| Parameter | Beta | Std. error | Lower | Upper | Wald
Chi-square | df | P-value |
|
Intercepta | 2.046 | 1.7467 | -1.377 | 5.470 | 1.372 | 1 | 0.241 |
| Approach | -0.672 | 0.6054 | -1.859 | 0.514 | 1.233 | 1 | 0.267 |
| Number fractured
ribs | 0.443 | 0.3409 | -0.226 | 1.111 | 1.686 | 1 | 0.194 |
| Number displaced
ribs | 0.172 | 0.4372 | -0.685 | 1.029 | 0.154 | 1 | 0.694 |
| Scaleb | 3.375 | 0.7548 | 2.178 | 5.232 | - | - | - |
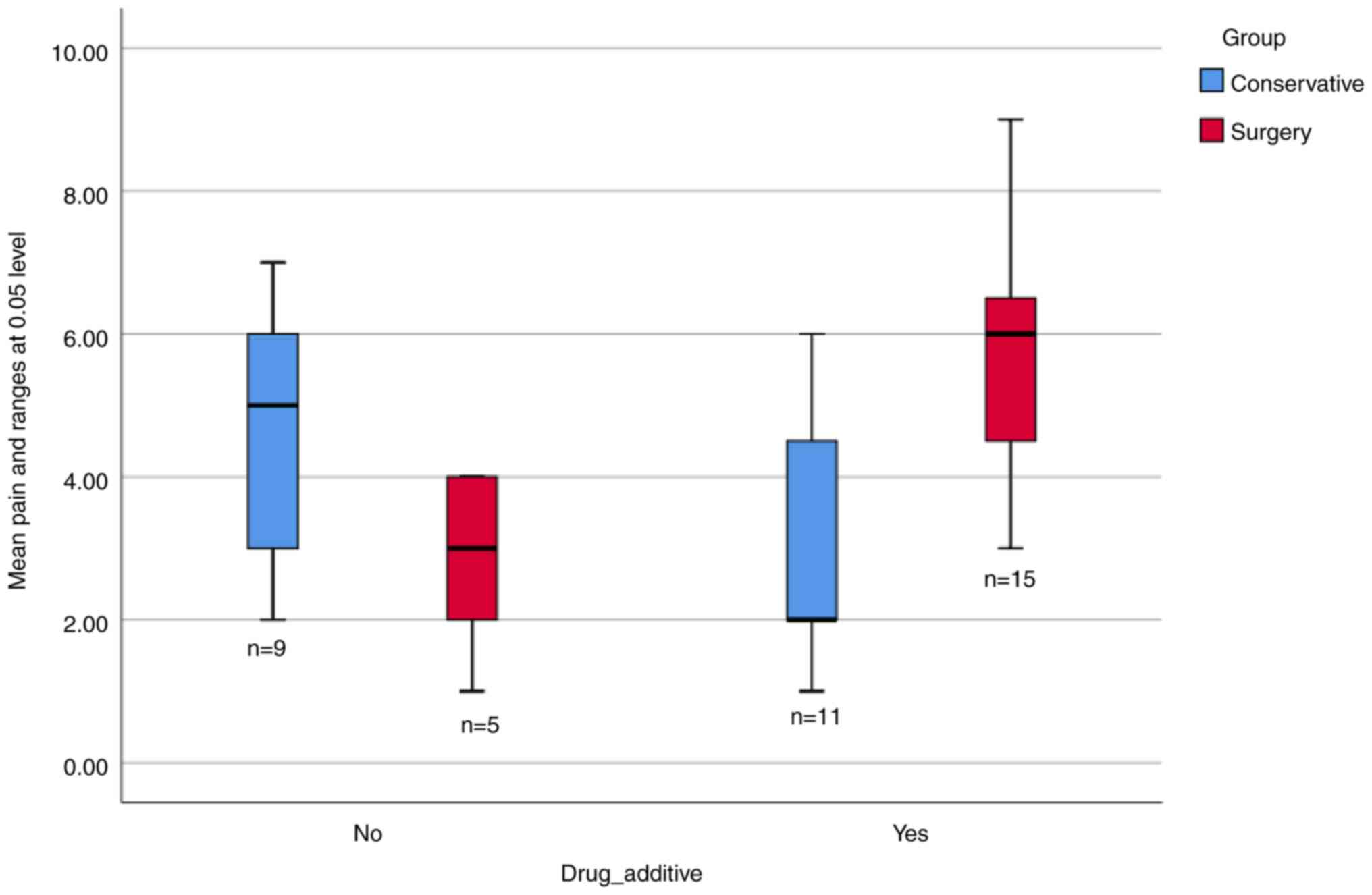
Pain level in the conservative
treatment and surgery groups
Pain levels in the conservative treatment group were
significantly higher compared with the surgery group when no drug
additives were used. By contrast, when drug additives were used,
pain levels were significantly higher (P<0.05) in the surgery
group compared with the conservative treatment group (Fig. 1).
Discussion
In the present study, the differences between
conservative and surgical treatment approaches, which are commonly
used to treat patients with non-flail multiple rib fractures, were
evaluated in terms of pain and treatment outcomes using
multivariate analysis. In this context, the study analyzed the
baseline characteristics, clinical findings and discharge pain
levels of patients who received one of the two treatment
methods.
Previous studies on rib fractures indicated that the
baseline characteristics of patients who underwent surgical
treatment were similar with those receiving conservative therapy in
terms of demographics (25-27).
Therefore, studies on this subject did not reveal any significant
differences in terms of age, sex or clinical history between the
aforementioned therapy groups. In consistency with this, in the
present study, patients in the surgery group and those in the
conservative therapy group displayed similarities in terms of age,
sex, number of fractured and displaced ribs, injury severity score,
chest abbreviated score, FEV1, narcotic drug dose, long-term FEV
and FVC levels, drug additives and ASA classification. The
differences in the above scores were statistically insignificant
between the conservative treatment and surgery groups. This finding
suggested that none of the treatment strategies was associated with
the baseline characteristics of patients with non-flail rib
fractures.
Previous studies also demonstrated that there were
no statistically significant differences in patient outcomes
between the conservative treatment and surgery groups (28,29).
However, a study by Zhang et al (8) reported that the surgical treatment
option was more effective in terms of pain and quality of life.
They recorded lower pain levels and higher quality of life in
patients with non-flail multiple rib fractures who underwent
surgery. In the present study, there were no significant
differences between the conservative and surgical treatment groups
regarding hospitalization duration, comfort level, follow-up
duration, return to workplace, discharge pain score, and
pneumothorax and pleural empyema incidence. This finding aligned
with the existing literature when examined univariately. However, a
multidimensional analysis within the framework of relational
screening should be performed to provide a more comprehensive
understanding.
Correlation analysis revealed that in the
conservative treatment group, the pain level was significantly
associated with the FEV1, drug additives and hospitalization
duration. On the other hand, in the surgery group, the discharge
pain level was notably associated with narcotic drug usage and drug
additives. Regression analysis further indicated that the
hospitalization duration had a statistically significant effect on
discharge pain in the conservative treatment group, while in the
surgery group, drug additives markedly affected discharge pain. The
above results suggested that although surgery was able to offer
greater pain management benefits, these outcomes could be largely
affected by pain management medications. Considering the importance
of pain, the results indicated that there were no statistically and
clinically significant differences between the conservative and
surgical treatment groups in patients with non-flail rib fractures.
However, further research is needed to generalize these findings
and better understand the effects of different treatment
strategies. In addition, the preference for conservative treatment
due to its lower invasiveness warrants further investigation.
Overall, these results may have significant implications for both
clinical practice and the existing literature.
The primary limitation of the present study was the
scarcity of similar studies in the field, making it difficult to
draw comprehensive comparisons. Although there are several studies
on multiple rib fractures, research particularly focusing on
non-flail rib fractures remains limited. In this respect, the
majority of clinical studies in this area have relied on
comparative rather than multivariate analyses (4,8,12,13).
Therefore, more research on this subject is needed to strengthen
the existing literature.
A key contribution of the present study was that it
challenged the hypothesis, suggested in previous univariate
analyses that surgery could provide superior pain management
compared with the conservative treatment approach. The multivariate
analysis results indicated that the observed advantage of surgery
in pain management was primarily associated with drug
additives.
From a clinical perspective, this study could aid
physicians in determining the most appropriate treatment method
based on the physical condition and clinical findings of patients.
Given the lack of a significant difference between the two
treatment methods, the choice should be guided by individual
patient needs rather than a presumed superiority of surgical
intervention. Although surgery is more attractive and it is most
commonly chosen for pain management, the result of the present
study indicated that this benefit could be effectively achieved
through drug additives.
Although surgery could be more effective for pain
management, the multivariate analysis revealed that this effect may
be due to the use of drug additives. This observation indicated
that findings from previous studies suggesting that the surgical
method could improve the quality of life and reduce pain may have
overlooked the role of drug additives due to their reliance on
univariate analysis.
Therefore, it may be argued that there was no
significant difference between surgical and conservative approaches
in treating non-flail multiple rib fractures. However, further
studies and clinical data are needed to verify this conclusion. In
clinical practice, the conservative approach could be preferred due
to the invasiveness and cost of the surgical approach. Overall, the
above findings suggested that the most appropriate treatment
decision should be based on the patient's current physical
condition and clinical findings.
Supplementary Material
Correlation plot of pain levels and
drug additive in patient groups.
Correlation plot of pain levels and
narcotic drug dose in the surgery group.
Correlation plot of pain levels and
hospitalization duration in the conservative group.
Correlation plot of pain levels and
FEV1 in the conservative group. FEV1, forced expiratory volume in 1
sec.
Acknowledgements
We thank Dr Kadir Yilmaz, İstanbul Commerce
University Statistics Department for his valuable help with the
statistical analysis.
Funding
Funding: Not applicable.
Availability of data and materials
The data generated in the present study are included
in the figures and/or tables of this article.
Authors' contributions
AGA and ED collected the data. ED analyzed and
interpreted the results. AGA and ED wrote the final version of the
manuscript and revised it. AGA and ED confirmed the authenticity of
all raw data. Both authors have read and confirmed the final
version of the manuscript.
Ethics approval and consent to
participate
The current study was approved by the İnönü
University Medical School Ethics Committee (Battalgazi, Türkiye;
approval no. 2013/10). All patients in the surgery group provided
written informed consent for their data to be used in the research.
Patients provided written informed consent for publication of their
data be used/published for scientific research purposes.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kim W, Song J, Moon S, Kim J, Cho H, Park
J, Kim S and Ahn S: Characteristics of rib fracture patients who
require chest computed tomography in the emergency department. BMC
Emerg Med. 23(33)2023.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kong LW, Huang GB, Yi YF and Du DY:
Consensus expert group. The Chinese consensus for surgical
treatment of traumatic rib fractures 2021 (C-STTRF 2021). Chin J
Traumatol. 24:311–319. 2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Liebsch C, Seiffert T, Vlcek M, Beer M,
Huber-Lang M and Wilke HJ: Patterns of serial rib fractures after
blunt chest trauma: An analysis of 380 cases. PLoS One.
14(e0224105)2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Van Wijck SFM, Van Lieshout EMM, Prins
JTH, Verhofstad MHJ, Van Huijstee PJ, Vermeulen J and Wijffels MME:
Outcome after surgical stabilization of symptomatic rib fracture
nonunion: a multicenter retrospective case series. Eur J Trauma
Emerg Surg. 48:2783–2793. 2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Fukushima K, Kambe M, Aramaki Y, Ichikawa
Y, Isshiki Y, Nakajima J, Sawada Y and Oshima K: Evaluation of
injury threshold from the number of rib fracture for predicting
pulmonary injuries in blunt chest trauma. Heliyon.
9(e15278)2023.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Li Y, Gao E, Yang Y, Gao Z, He W, Zhao Y,
Wu W, Zhao T and Guo X: Comparison of minimally invasive surgery
for non-flail chest rib fractures: a prospective cohort study. J
Thorac Dis. 12:3706–3714. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ingoe HM, Coleman E, Eardley W, Rangan A,
Hewitt C and McDaid C: Systematic review of systematic reviews for
effectiveness of internal fixation for flail chest and rib
fractures in adults. BMJ Open. 9(e023444)2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Zhang JP, Sun L, Li WQ, Wang YY, Li XZ and
Liu Y: Surgical treatment of patients with severe non-flail chest
rib fractures. World J Clin Cases. 7:3718–3727. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Beks RB, Reetz D, de Jong MB, Groenwold
RHH, Hietbrink F, Edwards MJR, Leenen LPH, Houwert RM and Frölke
JPM: Rib fixation versus non-operative treatment for flail chest
and multiple rib fractures after blunt thoracic trauma: A
multicenter cohort study. Eur J Trauma Emerg Surg. 45:655–663.
2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Adereti C, Fabien J, Adereti J,
Pierre-Louis M, Chacon D and Adereti V: Rib plating as an effective
approach to managing traumatic rib injuries: A review of the
literature. Cureus. 14(e29664)2022.PubMed/NCBI View Article : Google Scholar
|
|
11
|
He W, Yang Y, Salonga R, Powell L,
Greiffenstein P, Prins JTH and Abella SP: Surgical stabilization of
multiple rib fractures in an Asian population: A systematic review
and meta-analysis. J Thorac Dis. 15:4961–4975. 2023.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Seok J, Jeong ST, Yoon SY, Lee JY, Kim S,
Cho H and Kang WS: Novel nomogram for predicting paradoxical chest
wall movement in patients with flail segment of traumatic rib
fracture: A retrospective cohort study. Sci Rep.
13(20251)2023.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Marasco SF, Martin K, Niggemeyer L,
Summerhayes R, Fitzgerald M and Bailey M: Impact of rib fixation on
quality of life after major trauma with multiple rib fractures.
Injury. 50:119–124. 2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Billè A, Okiror L, Campbell A, Simons J
and Routledge T: Evaluation of long-term results and quality of
life in patients who underwent rib fixation with titanium devices
after trauma. Gen Thorac Cardiovasc Surg. 61:345–349.
2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Raza S and Eckhaus J: Does surgical
fixation improve pain and quality of life in patients with
non-flail rib fractures? A best evidence topic review. Interact
Cardiovasc Thorac Surg. 35(ivac214)2022.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Beks RB, Peek J, de Jong MB, Wessem KJP,
Öner CF, Hietbrink F, Leenen LPH, Groenwold RHH and Houwert RM:
Fixation of flail chest or multiple rib fractures: Current evidence
and how to proceed. A systematic review and meta-analysis. Eur J
Trauma Emerg Surg. 45:631–644. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
He S, Renne A, Argandykov D, Convissar D
and Lee J: Comparison of an emoji-based visual analog scale with a
numeric rating scale for pain assessment. JAMA. 328:208–209.
2022.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Rivero-Yeverino D: Espirometría: Conceptos
básicos spirometry: Basic concepts. Rev Alerg Mex. 66:76–84.
2019.
|
|
19
|
Liu YY, Wang JC, Lin YC, Hsiao HT and Liu
YC: Rib soft fixation produces better analgesic effects and is
associated with cytokine changes within the spinal cord in a rat
rib fracture model. Mol Pain. 15(1744806919855204)2019.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Peek J, Smeeing DPJ, Hietbrink F, Houwert
RM, Marsman M and de Jong MB: Comparison of analgesic interventions
for traumatic rib fractures: A systematic review and meta-analysis.
Eur J Trauma Emerg Surg. 45:597–622. 2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Abdelrahman AMF, Omara AFAS and Elzohry
AAM: Safety and efficacy of oral melatonin when combined with
thoracic epidural analgesia in patients with bilateral multiple
fracture ribs. Local Reg Anesth. 13:21–28. 2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Hall EJ and Sykes NP: Analgesia for
patients with advanced disease: 2. Postgrad Med J. 80:190–195.
2004.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Yılmaz K and Turanlı M: A
multi-disciplinary investigation of linearization deviations in
different regression models. Asian J Probab Stat. 22:15–19.
2023.
|
|
24
|
Yılmaz K and Turanlı M: A
multi-disciplinary investigation on minimizing linearization
deviations in different regression models. Change & Shaping
Future, IV. ASC-2022/Fall Congress, 2022.
|
|
25
|
Prins JTH, Van Lieshout EMM, Ali-Osman F,
Bauman ZM, Caragounis EC, Choi J, Christie DB III, Cole PA, DeVoe
WB, Doben AR, et al: Surgical stabilization versus nonoperative
treatment for flail and non-flail rib fracture patterns in patients
with traumatic brain injury. Eur J Trauma Emerg Surg. 48:3327–3338.
2022.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Zhang D, Jiao C, Xi S, Wang L, Li R and
Zhang Q: Evaluation of surgical outcomes in elderly patients with
rib fractures: A single-centre propensity score matching study.
Front Surg. 10(1174365)2023.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Witt CE and Bulger EM: Comprehensive
approach to the management of the patient with multiple rib
fractures: A review and introduction of a bundled rib fracture
management protocol. Trauma Surg Acute Care Open.
2(e000064)2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Qiu M, Shi Z, Xiao J, Zhang X, Ling S and
Ling H: Potential benefits of Rib fracture fixation in patients
with flail chest and multiple non-flail rib fractures. Indian J
Surg. 78:458–463. 2016.PubMed/NCBI View Article : Google Scholar
|
|
29
|
He Z, Zhang D, Xiao H, Zhu Q, Xuan Y, Su
K, Liao M, Tang Y and Xu E: The ideal methods for the management of
rib fractures. J Thorac Dis. 11:S1078–S1089. 2019.PubMed/NCBI View Article : Google Scholar
|