1. Introduction
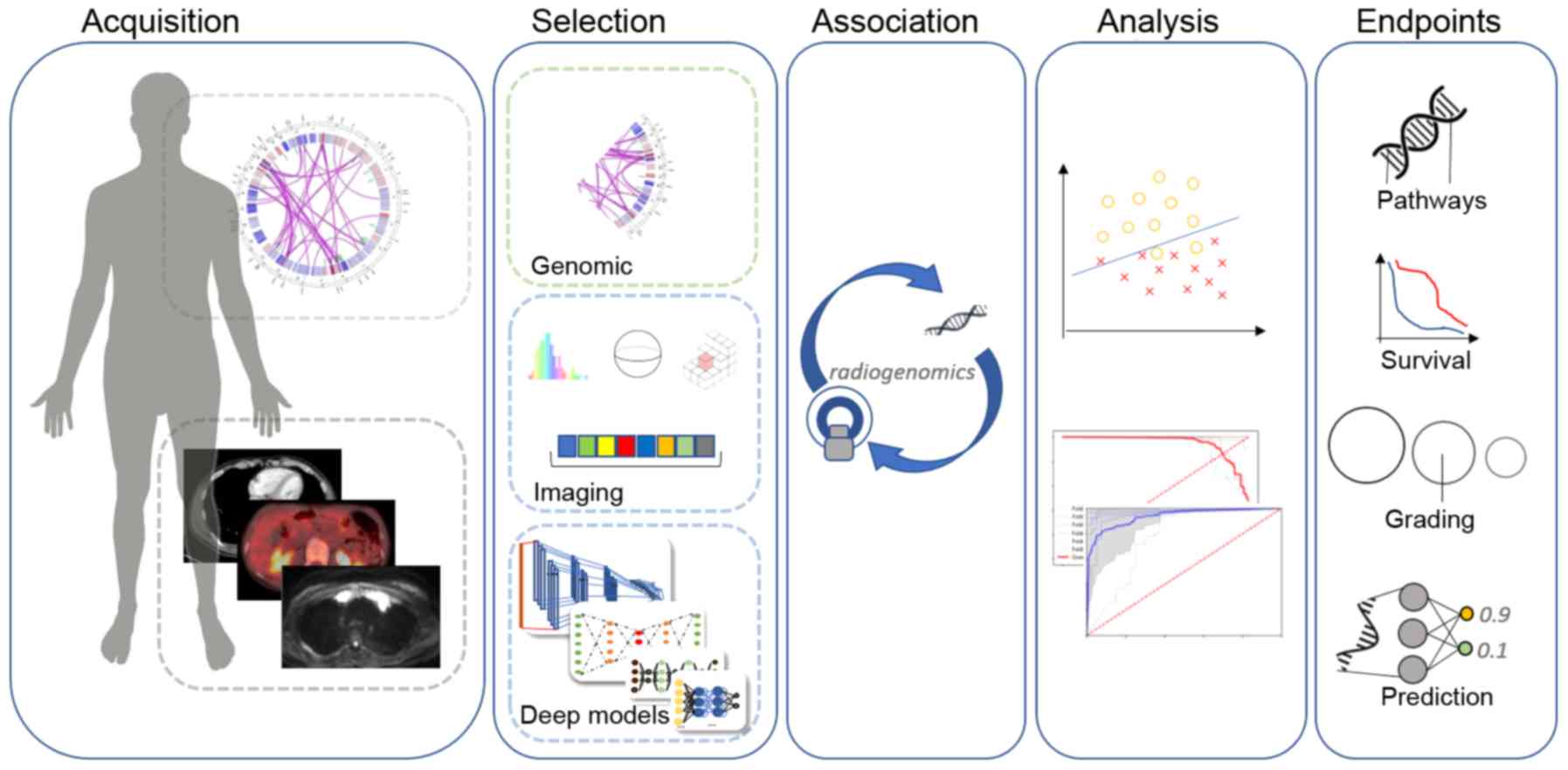
Radiogenomics is an emerging research field focusing
on establishing multi-scale associations between medical imaging
and gene expression data. Deciphering the interplay of radiological
and genetic/molecular features is of utmost importance in oncology
and can be achieved through the fusion of selected genomic and
radiomics features in a unified feature-space leading to more
precise decision support systems. Furthermore, radiogenomics can
enhance diagnosis (1), the
non-invasive prediction of molecular background (2) and survival prediction (3) in oncology by associating genomic data
with radiomics features acquired in a non-invasive fashion shedding
light on underling oncogenic mechanisms.
Despite advances in both multimodal-imaging
technologies involving novel agents, powerful protocols and
computer-aided diagnostic tools, there is a critical knowledge gap
between imaging information at the tissue level and the underlying
molecular and genetic disease biomarkers. This information gap has
important socio-economic consequences since in a number of cases,
only imaging information is available in the diagnostic setting,
rendering decisions such as the administration of expensive
treatments challenging, while risking under- or overtreatment. For
this reason, the vision of precision medicine is closely linked
with the understanding of the interplay and the joint effect of
multi-scale pathophysiological disease biomarkers. To this end,
radiogenomics approaches aim to link the imaging phenotype with
underlying molecular/genetic characteristics of disease entities,
particularly in oncologic applications in order to enhance
precision in the early diagnosis and management of patients. In
this context, several studies have tried to establish statistically
significant associations of image-derived features, such as the
shape and texture of a lesion with molecular or genetic information
based on usually small, but information-rich patient cohorts, where
both imaging [e.g., ultrasound (US), computed tomography (CT)
magnetic resonance imaging (MRI) and positron emission tomography
(PET)/CT] and molecular or genetic information [e.g.,
deoxyribonucleic (DNA) microarrays, micro-ribonucleic acid (miRNA),
ribonucleic acid sequencing (RNA-seq)] are available.
The fundamental hypothesis in radiogenomics research
is that certain molecular/genetic alterations induce alterations at
the tissue level that can be computationally detected in terms of
radiological appearance by properties, such as tissue shape and
texture (Fig. 1). Such changes can
however be very subtle or even invisible to the human eye. For this
reason, artificial intelligence (AI) techniques, such as deep
learning have provided the means to detect and decode these
changes/patterns in medical images and associate them with
molecular/genetic characteristics, paving the way for the
development of robust decision support systems and hybrid
prognostic, predictive and diagnostic signatures. In particular, in
recent years, the introduction and widespread availability in
oncologic care of hybrid clinical diagnostic imaging systems, such
as PET/CT and PET/MRI provides rich opportunities for AI-based
strategies aiming to enhance effectiveness and precision in the
management of oncologic patients (4-6).
Deep learning models are data-driven architectures
with state-of-the-art performance in almost all modern
data-processing tasks. These innovative approaches offer
end-to-end, fully automated data analysis pipelines by computing
exhaustively discriminative features to achieve the highest
performance on the given task. The model's parameters are learned
only from the data by updating its inner representation during the
optimization process aiming to approximate the optimal convergence
state. Additionally, multi-path architectures enable diverse data
types to coexist in the same model providing new opportunities to
combine imaging, clinical, laboratory, molecular and genetic data
towards unified AI decision-support systems extending the available
frameworks. Although the majority of radiogenomics studies are
based on traditional radiomics approaches (7) i.e., high throughput hand-crafted
image feature extraction followed by association with
genomic/molecular markers, the application of AI techniques, such
as deep learning in the field is still limited, due to the lack of
large multi-modal cross-sectional and/or longitudinal datasets. The
main aims of the present review were to summarize the most
important results concerning the application of deep learning in
radiogenomics, to highlight the clinical significance of
associating molecular or genetic information with imaging
phenotype, to emphasize the potential for the discovery of novel,
highly discriminative combined biomarkers and at the same time, to
discuss the main limitations concerning the state-of-the-art
research in the field. Furthermore, representative DL-based studies
focusing on cancer tissue differentiation or therapy prediction
solely from medical images have been included. This is due to the
fact that such clinical issues are attractive for radiogenomics
research, since they involve molecular/genetic mechanisms and have
been also studied with in vitro tumor phenotyping involving
the in vitro assay of tumor biopsy material. As an example,
a previous study (8) provided a
deep learning study based on a convolutional neural network (CNN),
which predicts the neoadjuvant therapy response in esophageal
cancer with fluorodeoxyglucose positron emission tomography
(18F-FDG PET) imaging data and achieves 80% sensitivity and
specificity. In a gene expression study (9) on the same clinical problem, a
17-molecule was found to be predictive of complete response to
neoadjuvant chemotherapy for esophageal cancer with docetaxel,
cisplatin and 5-fluorouracil, while a recent study reported that
on-treatment genetic biomarkers can predict complete response in
neoadjuvant breast cancer (10).
Similarly, it has been reported (11) that tumor mutational burden
information can differentiate between primary and metastatic breast
cancer and for this reason, the present review includes deep
learning efforts to differentiate primary from metastatic cancer
directly from medical imaging data [such as previously done
(12) for liver cancer]. In
addition, apart from the limited deep learning-based radiogenomics
studies available, representative deep learning studies on cancer
type classification or therapy prediction in oncology are included,
since these studies can be extended towards associating imaging
phenotype and genetic/molecular markers.
2. Research methodology
The search was performed in widely used databases,
such as PubMed and Google Scholar. Initially, articles including a
subset or a combination of the terms noted in the title or abstract
(Table I) were identified. The
Abstracts and conclusions of 123 studies were examined during the
first screening process. Although the bulk of these manuscripts
included a subset or a combination of the examined keywords, the
second screening revealed that the methodology of a number of these
papers was not relevant to deep learning radiogenomics analysis and
these were therefore excluded. The exclusion criteria used in the
present review are summarized as follows: i) Studies focusing on
radiomics, deep learning segmentation with radiomics, handcrafted
features associated with genomic data or traditional image analysis
with machine learning techniques; ii) studies where deep learning
was used only for data augmentation and synthetic data generation
paired with radiomics or other analysis; and iii) studies on tissue
classification (normal, benign, malignant tissue), scoring
[Gleason, breast imaging reporting and data system (BI-RADS)] or
genomic data analyses without involving image-derived features.
 | Table IKeywords used in the present review
article. |
Table I
Keywords used in the present review
article.
| Deep learning | Cancer | Magnetic resonance
imaging | Radiogenomics |
|---|
| Artificial
intelligence | Carcinoma | Positron emission
tomography | Therapy
response |
| Convolutional
neural networks | | Computer
tomography | Treatment
response |
| Recurrent neural
networks | | Medical
imaging | Tissue
classification |
| | | Molecular
signatures |
As a result, 25 studies were selected for the
presented deep learning radiogenomics in-depth review. Information
related to the examined malignancy, patient cohort size, imaging
modalities and deep network architecture type is presented in
Table II. The objective and
performance of the examined studies are described in Table III, including evaluation results
in terms of accuracy (ACC) and area under the curve (AUC)
scores.
 | Table IIOverview of the studied malignancies,
imaging modalities and proposed deep architectures. |
Table II
Overview of the studied malignancies,
imaging modalities and proposed deep architectures.
| Author (Refs.) | Anatomical
area | Patient cohort | Imaging
modality | Deep architecture
type |
|---|
| Chang et al
(18) | Brain | 496 | MRI: FLAIR, T2, T1
pre-contrast, T1 post-contrast | Multiple residual
CNN with decision fusion |
| Grinband et
al (19) | Brain | 155 | MRI: T1, FLAIR | Residual CNN |
| Li et al
(20) | Brain | 119 | MRI: T1, T2 | ROI-only CNN |
| Liang et al
(21) | Brain | 167 | MRI: T1, T2, T1Gd,
FLAIR | Multi-channel
ROI-only 3D DenseNet |
| Korfiatis et
al (22) | Brain | 155 | MRI: T2 | ResNet50 |
| Akkus et al
(23) | Brain | 159 | MRI: T1C, T2 | Multi-kernel
CNN |
| Bonte et al
(25) | Brain | 285 | MRI: T1ce | VGG-11 |
| Smedley et
al (26) | Brain | 528 | MRI: T1WI+c, T2WI,
FLAIR | AE, DNN |
| Zhou et al
(27) | Brain | 233 | MRI: T1, T2,
FLAIR | DenseNet AE,
LSTM |
| Momeni et al
(28) | Brain | 47 | H&E, MRI: T1C,
FLAIR | DenseNet,
3D-CNN |
| Afshar et al
(29) | Brain | 233 | MRI | ROI-only Capsule
Network |
| Yu et al
(31) | NSCLC | 684 | CT | Patch-2D CNN |
| Zhu et al
(34) | Breast | 270 | DCE-MRI | GooLeNet, VGG,
pre-trained, fine-tuned |
| Ha et al
(35) | Breast | 216 | Pre-contrast
MRI | Residual CNN |
| Yoon et al
(36) | Breast | 213 | MRI: T1WI | CNN with feature
fusion (image and genetic) |
| Zhu et al
(37) | Breast | 131 | MRI: T1WI | Pre-trained
GooLeNet |
| Ypsilantis et
al (8) | Esophagus | 107 | 18F-FDG PET | Multi-channel
3-slice CNN |
| Bibault et
al (38) | Rectal | 95 | CT | DNN |
| Chen et al
(39) | Pancreas | 48 | MRI: T1, T2 | ROI detection
faster-RCNN, ROI-only inception layers |
| Trivizakis et
al (12) | Liver | 130 | MRI: b1000 | Patch-2D, 2D and 3D
CNN |
| Cha et al
(40) | Bladder | 82 | CT | CNN
transfer-learning |
| Cha et al
(41) | Bladder | 170 | CT | CNN and
radiomics |
| Banerjee et
al (42) | RMS | 21 | DWI, T1W | CNN
transfer-learning |
| Zhou et al
(43) | Head and neck | 31 | PET and CT | Evidential
reasoning: 3D CNN and radiomics |
 | Table IIIAggregated results for comparison of
the reviewed articles. |
Table III
Aggregated results for comparison of
the reviewed articles.
| Author (Refs.) | Study
objective | Performance
(ACC/AUC %) |
|---|
| Chang et al
(18) | IDH1 mutation |
85.7-89.1/94-95 |
| Grinband et
al (19) | IDH1 mutation | 94/91 |
| Li et al
(20) | IDH1 mutation |
82.4-92.4/92-95 |
| Liang et al,
(21) | IDH1 mutation |
84.6,91.4/85.7,94.8 |
| Korfiatis et
al (22) | MGMT state | 94.9/- |
| Grinband et
al (19) | MGMT state | 83/84 |
| Akkus et al
(23) | 1p19q codeletion
status | 87.7/- |
| Grinband et
al (19) | 1p19q codeletion
status | 92/88 |
| Bonte et al
(25) | Glioma grading |
91.1,93.5/82,86.1 |
| Zhou et al
(27) |
Metastatic/glioma/meningioma | 92.1/- |
| Momeni et al
(28) |
Oligendroglioma/astrocytoma | 85/92 |
| Afshar et al
(29) |
Glioma/pituitary/meningioma | 86.6/- |
| Yu et al
(31) | EGFR mutation
status | 76.1/82.8 |
| Wang et al
(32) | EGFR mutation
status | 73.9/81 |
| Zhu et al
(34) | Luminal A vs
others | -/58-65 |
| Ha et al
(35) | Luminal A vs. B vs.
HER2+ vs. Basal | 70/87.1 |
| Yoon et al
(36) | Pathological state,
ER, PR, HER2 | -/69.7, 97.6, 89.9,
84.2 |
| Zhu et al
(37) | Occult invasive
disease status | -/70 |
| Ypsilantis et
al (8) | Neoadjuvant
chemotherapy response | 73.4/66.3 |
| Bibault et
al (38) | Neoadjuvant
chemoradiation response | 80/72 |
| Chen et al
(39) | Subtype
prediction | 80, voting:
92.3/- |
| Trivizakis et
al (12) |
Primary/metastasis | 83/80 |
| Cha et al
(40) | Chemotherapy
response | -/62-77 |
| Cha et al
(41) | Chemotherapy
response | -/62-79 |
| Banerjee et
al (42) | Subtype
prediction | 85/- |
| Zhou et al
(43) | Lymph node
metastasis | 72.7-93/65-92 |
3. Deep architectures used in current
radiogenomics studies
Deep learning methodologies are very attractive for
advancing radiogenomics studies, particularly when taking into
consideration the large search-space due to the abundance of
features in both images and genetic/molecular data. Critically, in
contrast to handcrafted feature-based machine learning techniques,
the whole process is fully automated and through exhaustive
analysis, non-intuitive correspondences between medical image
features and genetic/molecular information can be established.
Thus, a higher-level modeling is achieved through computational
analysis of the high complexity raw radiogenomics data, allowing
focusing on particular disease properties for outcome prediction by
leveraging pathways, molecular or meta-gene convergence objectives.
The main deep learning architectures in the reviewed studies are
listed below:
Convolutional neural network (CNNs)
CNNs were originally designed by LeCun et al,
as a fully automated image analysis network for classifying
handcrafted digits (13). The
fundamental principle of this deep architecture is to massively
compute and combine feature maps inferring non-linear associations
between the input signal and the targeted output. This type of
network is popular for the automatic extraction, selection and
reduction of discriminative features from high-dimensional input
data providing state-of-the-art classification performance in
demanding fields.
Recurrent neural networks (RNNs)
RNNs exhibit similar functionality with the regular
feedforward neural networks, where every hidden state will be fed
as an input for the next state but in addition, they integrate
internal memory. This short-term memory allows recurrent networks
to remember information from the previously analyzed states, a
perfect fit for sequential signal analysis and predictive
models.
CapsuleNet
A capsule is a set of neurons that models a part of
an object of the input by activating a small subset of its
properties. The CapsuleNet (14)
consists of independent sets of capsules instead of kernels
propagating information to the successive higher-level capsules
through the routing-by-agreement process. This architecture is the
newest evolvement in the deep learning field and to date, has not
been extensively tested by the medical research community.
Autoencoders (AEs)
AEs learn a compact representation of their input by
reconstructing it. The encoder part of the AE has a decreasing
number of neurons after every successive hidden layer, reducing the
dimensionality of the incoming state. The decoder part reconstructs
the resulted compact representation to an approximation of the
initial input by backpropagating the reconstruction error.
Artificial neural networks (ANNs)
ANNs or deep neural networks (DNNs) were inspired by
the alleged learning functionality of the biological brain. The ANN
constitutes of a set of fully-connected nodes modelling the stimuli
propagation of brain synapses -fire or not- across the neural
network to perform a specific task. It can be used for feature
selection, classification or dimensionality reduction as a
submodule of a deeper architecture (CNN and AE) or as a stand-alone
module with hand-crafted features.
Multi-model decision fusion
A meta-analysis of a set of models can accumulate
the predictive power of a number of diverse models built on
different data types, but aiming at a single objective. Decision
fusion combines the outcome of multiple classifiers into a singular
final prediction forming a meta-estimator by utilizing statistical
methods to amplify the individual classifiers. This leads to an
improved accumulated predictive power and can resolve uncertainties
or disagreements among singular analyses.
Pre-trained models
A source model trained with widely available
'natural' images can be transferred to a target model that will
perform similar tasks but in the medical imaging domain. The learnt
feature detectors of these deep architectures as a result of their
low-level status can be an alternative and viable option for tasks
with small dataset. In this context two major methodologies can be
followed: Off-the-self models (for classification or feature
extraction) and fine-tuned models. There are several available
pre-trained models [video geometry group (VGG)-16 (http://www.robots.ox.ac.uk/~vgg/research/very_deep/),
Inception (15), DenseNet
(16), Mask R-CNN (17)] and more employed by several
authors, claiming mixed results for the off-the-self method with
fine-tuning being the most promising due to its supplementary
adaptation to the targeted model.
4. Clinical applications of deep
learning-based radiogenomics
Brain neoplasms
Isocitrate dehydrogenase (IDH) isozyme
mutation status
Patients with glioma carrying IDH1 or IDH2 mutations
have a relatively favorable survival, when compared to glioma
patients with wild-type IDH1/2 genes. For this reason, the
non-invasive prediction of the IDH1 mutation status at the
pre-treatment stage is critical for treatment planning.
Discriminating between wild-type and mutation status of IDH1 can be
challenging. The architecture proposed by Chang et al
(18), consists of multiple
residual convolutional neural networks, one for each MRI modality,
with decision fusion evaluated on multi-institutional data of grade
II-IV glioma. A traditional CNN approach trained on segmented
regions of interest (ROI) of wild-type vs. mutation 2D slices was
applied by Grinband et al (19) and a hybrid architecture was
proposed by Li et al (20),
including a convolutional network trained with patches of ROI/no
ROI, a fisher vector module for encoding the extracted salience
maps and a support vector machine classifier for predicting the
IDH1 mutation status. During inference the convolutional-only
network with multi-scale input produces feature maps encoded by the
fisher vector module in a compact representation similar to bag of
visual words. The patches and ROIs were extracted from multi-modal
low-grade glioma MRIs. Liang et al (21), utilized a multi-channel 3D DenseNet
architecture for predicting the IDH1 status trained on segmented 3D
ROIs with multi-modal [T1, T2, T1Gd and fluid-attenuated inversion
recovery (FLAIR)].
Methylguanine methyltransferase (MGMT)
methylation state
MGMT is a gene responsible for repairing the
mismatched DNA molecules and its methylation status. Clinically, it
is used as a predictive biomarker for response to chemotherapy with
temozolamide, which is the standard for glioblastoma multiforme
(GBM) following therapy. A 50-layer ResNet was previously used
(22) and a CNN trained with
ROIs-only (19) as mentioned
earlier.
1p19q chromosome
The co-deletion status (the combined loss of the
short arm chromosome 1 and the long arm of chromosome 19) of 1p19q
in low-grade glioma has been associated with an improved response
to therapy and a higher survival rate. A proposed multi-kernel CNN
(23) predicts the 1p19q
chromosomal expression from multi-modal (T1C and T2) low-grade
glioma MRI. In a previous study (19), a similar approach was followed to
the previously mentioned IDH1 and MGMT by utilizing the same deep
architecture to predict the 1p19q codeletion.
Glioma grading
Glioma is a type of tumor that begins in glial cells
and is the most common type of brain tumor associated with a poor
prognosis (24). The
classification of the glioma type (e.g., glioblastoma, astrocytoma
and oligodendroglioma), and grade is critical for the treatment
plan, which consists of external radiation therapy, surgery,
chemotherapy, or a combination of these. In a previous study
(25), a pre-trained VGG-11 CNN
with a random forest classifier was used for glioma grading.
Genetic association with MR imaging
features
A novel application of radiogenomics analysis by the
deep learning reconstruction of genetic data and MR imaging
features in patients with GBM has been previously proposed
(26). An AutoEncoder architecture
was trained to match the tumor gene expression with the extracted
morphological MRI features including volume, surface area, surface
area to volume (SA:V) ratio, sphericity, spherical disproportion,
max diameter, major and minor axes and compactness for both cancer
region and edema. According to the authors of that study, the
network was able to capture predictive radiogenomics associations,
linking the genetic profile to MRI morphology of the examined
lesion better than traditional statistical methods, such as linear
regression or pairwise comparison.
Tissue characterization
Furthermore, selected studies dealing with cancer
tissue characterization have been included in the current review,
since in such cases, both differences in imaging phenotype and
gene-expression have been linked with cancer tissue
characterization. In particular, for brain tumor deferential
diagnosis, several deep learning architectures have been proposed,
including a DenseNet AutoEnconder combined with Long-Short Term
Memory (27) for metastatic vs.
glioma vs. meningioma, a two-path CNN with a dropout meta-estimator
for combined histopathology and radiology images discrimination
between oligendroglioma vs. astrocytoma (28) and CapsuleNet (29) for meningioma vs. pituitary vs.
glioma differentiation.
Non-small cell lung cancer
(NSCLC)
NSCLC is the most common type of lung cancer (up to
85% globally) with a high mortality rate among the cases diagnosed
(30). Effective staging is
challenging for therapy decision therefore imaging (CT and PET),
laboratory and molecular biomarkers are of utmost importance.
epithelial growth factor receptor (EGFR) is a protein involved in
cell growth located on the cell surface and is associated with
malignancy. The prediction of the EGFR mutation profile can lead to
better, more effective and targeted treatment. Yu et al
(31), proposed a 2D CNN trained
on CT nodule patches labeled by the mutation state of EGFR. The
study identified deep learning imaging features related to the EGFR
profile of NSCLC, verifying the mutational status determined by
biopsy with the additive benefit of a non-invasive examination
Wang et al (32), used the DenseNet architecture and
in particular the first 20 layers with weights acquired from the
ImageNet dataset in a transfer learning scheme. Additionally,
fine-tuning was applied with a dataset comprised of approximately
15,000 CT images towards identifying the EGFR mutation status
(mutation vs. wild-type). The authors also presented a framework
for visualizing the areas with high probability of lesion presence
extracted from feature maps of the deep architecture as an
additional level for evaluating the AI predictions. The aim of
extending the main classification framework is to provide the
clinicians with interpretable visual cues and novel attention maps
of the inference path followed by the deep model.
Breast cancer
Discriminating molecular subtypes of breast cancer
has a significant effect on the clinical management of patients.
Some of these subtypes include luminal A and B, the expression of
human epidermal growth factor receptor 2 (HER2) and triple-negative
types [estrogen receptor (ER)-, progesterone receptor (PR)- and
HER2-]. Breast cancer subtypes can be determined by genetic testing
or by immunohistochemistry markers. The catalyst for promoting
breast cancer research is the availability of open-access data,
such as The Cancer Genomic Atlas-Breast Invasive Carcinoma
(TCGA-BRCA) (33) database which
offers interdisciplinary research opportunities for the medical and
the computational/AI research community. Deep learning molecular
subtype classification has been introduced in several studies, such
as in a previous study (34) where
GoogLeNet architectures (pre-trained and fine-tuned, from scratch,
off-the-shelf) and inception-based residual CNN (35) were used for differentiating luminal
and other subtypes based on dynamic contrast enhanced magnetic
resonance imaging (DCE-MRI) and pre-contrast MRI data,
respectively. Yoon et al (36), incorporated 3D CNN feature maps
from MRI data and the corresponding gene expression at the
fully-connected neural part of the deep network through feature
space fusion to predict several clinical associations such as the
pathological stage, ER status, PR status and HER2. Zhu et al
(37), proposed a pre-trained
GooLeNet architecture fine-tuned using data augmentation techniques
based on MR image patches extracted from the examined region of
interest. Additionally, an 'off-the-shelf' deep learning module for
feature extraction was combined with an SVM classifier to predict
the status of occult invasive disease following the diagnosis of
ductal carcinoma in situ (DCIS).
Oral cancer
Ypsilantis et al (8), investigated the therapeutic response
and survivability of examined esophageal cancer patients by
stratifying them into responders vs. non-responders. The proposed
3-slice CNN (3sCNN) was trained with a subset of the 18F-FDG PET
examinations targeting the metabolic activity of the malignancy.
This was achieved by selecting from each examination three slices
representative of the intra-tumor region and applying concatenation
in the color space to introduce them as a unified image to the
network.
Colorectal cancer
The rectal cancer therapeutic strategy may include a
combination of chemotherapy, radiation and surgery. The
non-invasive prediction of complete response of neo-adjuvant
therapy can affect the therapeutic algorithm, avoiding unnecessary
medical procedures. This application can significantly improve the
quality of life and/or survival rate of the patients, spare organ
function, reduce the cost of treatment and minimize the toxicity
risk or local and distant recurrences. A deep neural network
(38) trained on radiomics,
clinical and radiological semantic features was used to predict
complete therapy response following chemoradiation in colorectal
cancer patients.
Pancreatic cancer
Tissue classification for pancreatic neoplasms from
routine imaging data can lead to therapy response prediction. In
particular, based on the type of cystic lesions different
strategies for treatment and/or follow-up are followed. An
inception-style architecture with feature space fusion (39) was trained on multi-modal (T1 and
T2) ROI images of pancreatic cystic neoplasms (PCNs) to
discriminate tissue sub-types such as mucinous cystic neoplasms,
intraductal papillary mucinous neoplasm and serous cystic
neoplasms. Given the difficulties and morbidity of biopsy procedure
in the pancreas, the importance of this application is critically
high.
In addition, over the past decade, effective
systemic treatment protocols have been developed, and more
accurate, effective and less toxic radiotherapeutic strategies have
been applied. Due to the poor prognosis of pancreatic cancer, there
is a growing effort being made to improve the efficacy of
neoadjuvant chemotherapy or chemoradiotherapy, particularly in
'marginally' resectable or even in clearly resectable pancreatic
adenocarcinomas. Radiogenomics may play a crucial role in the
selection of patients with a higher probability of response to
these approaches.
Liver cancer
The diagnosis of liver cancer with traditional
machine learning techniques is extremely challenging considering
its multifocal distribution. Tissue discrimination between primary
and metastatic liver cancer was performed by utilizing 3D-CNN
(12) with no pre-processing or
segmentation from raw high b-value MRI volumes (b=1,000
sec/mm2) achieving state-of-the-art performance through
a fully automated analysis.
Bladder cancer
The analysis of the pre and post-treatment routine
imaging examinations elucidates the effectiveness of the followed
treatment. Bladder chemotherapy response prediction was previously
performed using contrast enhanced CT of pre-treated cancer patients
following two different transfer learning approaches (40) and applying feature fusion from deep
models combined with radiomic signatures (41).
Rhabdomyosarcoma (RMS)
2D CNN with transfer-learning and multimodal MRI was
previously proposed by Banerjee et al (42), to determine embryonal (ERMS) or
alveolar (ARMS) genetic expression of RMS contributing to
individualized therapy decision making and survival prediction for
patients with the aforementioned subtypes.
Head and neck cancer
Zhou et al (43), combined 3D CNN and image processing
features through evidential reasoning to predict lymph node
metastasis (LNM) of head and neck cancer patients from routine PET
and CT. This multi-modal image analysis framework comprised of
novel AI models and commonly accepted radiomics for establishing a
robust model. The authors of that study claimed an improved
diagnosis with the advantage of a non-invasive method sparing
patients from unnecessary or ineffective medical procedures.
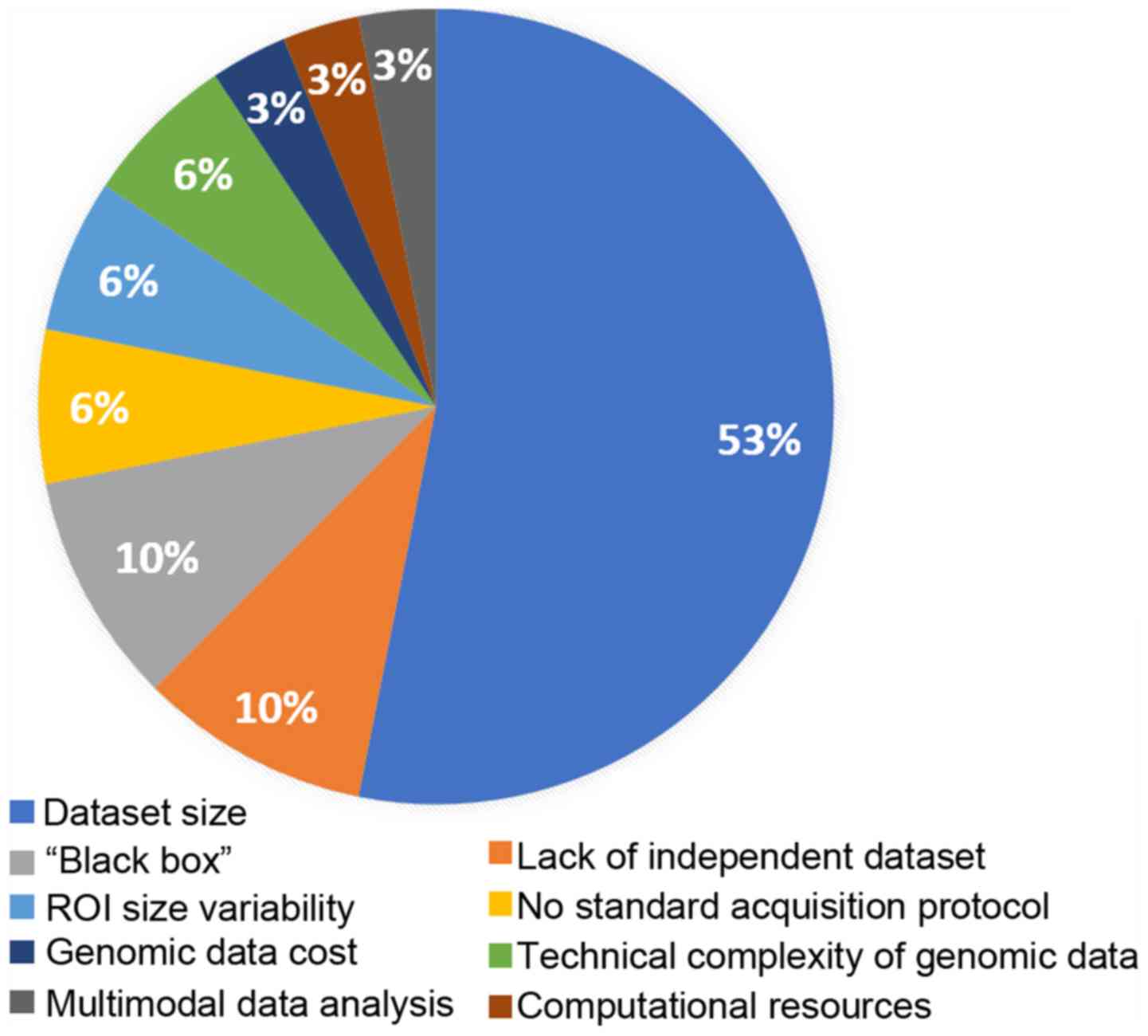
5. Limitations of radiogenomic research
The most pronounced limitation for deep learning
radiogenomics, as highlighted in Fig.
2, is related to the size of the available datasets. The lack
of the required volume of data can lead to inadequate
stratification (19,35,37)
among training, validation and testing datasets compromising the
model adaptation, optimization and evaluation process respectively.
For this reason, the numbers of studies on diseases with limited
datasets such as rectal cancer, rhabdomyosarcoma, head and neck
malignancies, pancreatic and esophageal cancers included in the
present review are limited. For comparison, the study of one of the
most common types of cancer, NSCLC, examines 684 cases, brain and
breast studies on average include >200 patients in contrast to
other cancer types, where the samples vary from 21 to 170 cases at
most, as evidenced in Table II.
Additionally, limited-size datasets can be a source of concern
regarding the fitting status of deep neural networks, potentially
leading to a high risk of model overfitting and poor generalization
ability due to the wide biological variability of cancer (tumor
heterogeneity). This can lead to incompetent decision support
systems with high false-positive rate for examinations from
diagnostic centers with different imaging protocols or devices.
Open-access, curated and high-quality public benchmark databases
with complete genomic and imaging data across disease types need to
be made available in order to promote radiogenomic research and
introduce comparable metrics among studies. For instance, a large
number of radiogenomics publications examine brain (44) and breast (45) cancer as widely available
open-access databases are available.
The infamous 'black box' (19,29,37)
systems, as commonly deep learning and ANN are known, compute and
propagate high-throughput features calculated during a continuously
evolving learning process producing an inner representation
uninterpretable by traditional statistical analysis or other
mathematical methods. A deep learning model throughout the training
process incorporates changes on tens of millions of parameters
adapted solely in analyzing the retrospective input data with no
a-priory knowledge. The fully automated nature of the analysis
poses a great drawback in the medical domain where each decision is
led by a diverse set of various laboratory, clinical, imaging data
in multiple time points, knowledge of malignancy biology and
accumulated empirical patient outcomes. Moreover, translating deep
learning technologies to clinical practice poses significant
challenges considering the 'explainability' of clinical
requirements for AI decision support tools (46). The recommendation of a personalized
therapeutic care plan can be challenging even for expert
clinicians. For this reason, novel methods, algorithms and tools
for supporting explainable AI are needed in order to accelerate the
clinical evaluation and translation of DL-based radiogenomics
technologies.
The demand for computational power and
high-throughput infrastructure (28) in these types of models can also be
a limiting factor regarding the available resources, particularly
in an ensemble or meta-model environment where inference with
different data analysis paths may coincide. Investing in
specialized infrastructure for enabling access to large data
repositories or patient registries by highly qualified scientific
personnel is required for conducting AI research and deploying
scalable models towards advancing traditional oncology to
data-driven precision medicine.
Contemporary artificial intelligence decision
support systems have limitations related to the 'ground truth' for
the studied region of interest (26,27).
The differences in pixel-wise labeling (inter-observer variability
and bias) for lesion delineation, uncertainty in the examined
anatomical areas of malignances (surrounding area, necrosis),
disregarding location-based information of the tumor and dependence
on morphological features from ROIs may introduce additional
variability and misdirection during the convergence process of a
fully automated data-driven AI model. Fusing imaging modalities
(21) with no a-priori knowledge
or evidence about their optimal combination for the targeted
clinical question can lead to unnecessary, redundant analysis with
a negative effect on the final decision. Thus, clinicians should
provide insight and be in active cooperation with the data science
engineers regarding specific lesions attributes with respect to the
followed diagnosis protocols. Other types of data, such as
laboratory (blood exam results), anthropomorphic (height and
weight), demographic (age and sex) and supplementary imaging
modalities can introduce diversity and complementarity towards
achieving better problem formulation, improved predictive power and
a robust decision support process (21).
Finally, a limited number of laboratories (22) can conduct genomic research since it
is a challenging and costly task (35) requiring adequate expertise and
laboratory certifications. At the same time, in a number of cases,
genomic and molecular analyses take place outside the hospital
environment in different laboratories, rendering data integration
challenging due to the implementation of different proprietary
genome sequencing technology by commercialized platforms. Such
limiting factors may partially explain the lack of combined genomic
and imaging databases which in turn limits current deep learning
radiogenomics efforts.
6. Discussion and future directions
The initial successful paradigm of DL in natural
images paved the way for the clinical research community to adopt
this novel methodology, leading to unprecedented advancements
related to computer aided diagnosis or detection (CAD or CADe)
systems. Furthermore, advanced data analysis methodologies on
medical images of cancer patients can provide insight or
associations with molecular and genetic characteristics of the
disease. Such radiogenomics analyses can lead to the identification
of novel hybrid biomarkers based on the association of the radiomic
signature with genomic information of a lesion, sparing patients
from unnecessary invasive procedures. Several methods, such as
statistical analysis, machine learning and deep learning, aim to
find statistically significant correlations or patterns among these
high-throughput and high-dimensional features.
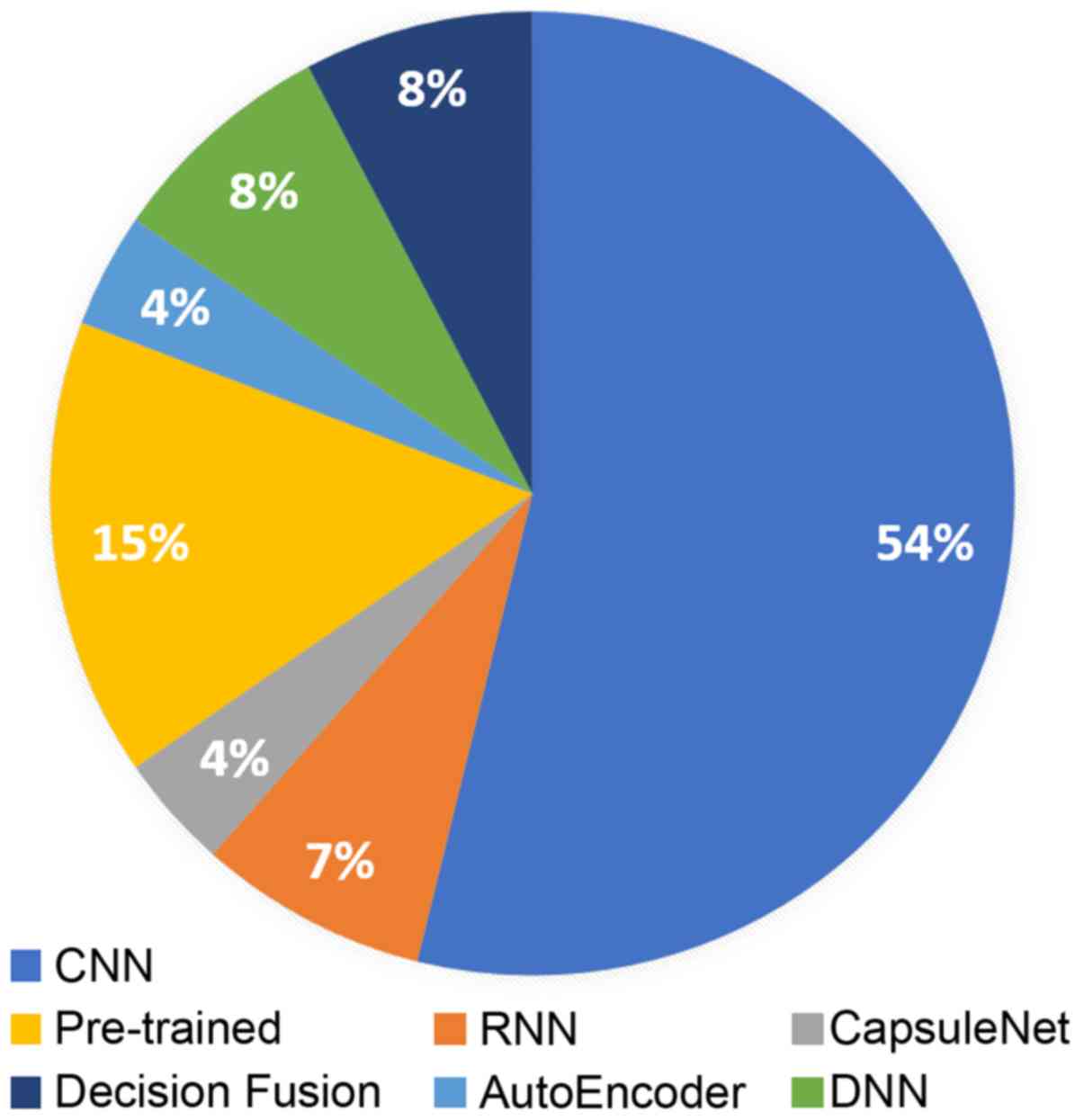
The present review summarizes recent literature in
radiogenomics focusing on deep learning methodologies. Deep
learning-based radiogenomics is a relatively understudied field, as
it has become evident by the limited literature. However, the rise
of AI and the association of diverse data, such as imaging
phenotypes/features with genomic information can lead to a positive
outlook regarding the clinical value of the radiogenomic models.
CNNs are by far the most popular architecture in the literature
(Fig. 3), due to their efficiency
in learning meaningful representations that can demonstrate
state-of-the-art results in many image analysis tasks.
Additionally, pre-trained models are widely used due to the lack of
large medical imaging and genomic datasets providing a valuable
alternative in the small dataset setting. Brain and breast are the
most commonly studied anatomical areas mainly because of the
availability of publicly open and standardized databases.
The most important limiting factors as referred by
the examined studies concern the number of available patients with
both imaging and genomic data available and lack of independent
benchmark databases that can provide a performance baseline for
comparing different approaches or modeling methodologies.
Furthermore, an important concern especially in the clinical
practice is the lack of explainability and transparency regarding
the fully automated inference in modern AI techniques. This can
pose trust and legal issues by either the clinicians or the health
authorities respectively. In addition, other concerns raised by the
authors of the examined studies included the availability of
computational resources, the lack of standardized methodologies for
multimodal data analysis, interobserver variability in regions of
interest for the studied problem, variations in image acquisition
protocol, and issues related to the cost and technical challenges
in genomic data acquisition.
Despite all the aforementioned drawbacks,
exceptional performance has been achieved in studies regarding the
prediction of IDH1 expression with an AUC of 91-94% (18-21),
as well as a codeletion of 1p19q (19) with an AUC of 94% in brain gliomas
with residual CNN. Korfiatis et al (22), reported an ACC of 94.9% for MGMT
methylation status prediction by applying residual learning. The
subtyping of invasive breast cancer was investigated by Yoon et
al (36), demonstrating an AUC
performance between 84 and 97.6%. Finally, the challenging tissue
classification in lymph node metastasis was addressed by Zhou et
al (43), achieving an AUC
performance up to 92% with the combinations of 3D CNN and radiomics
on PET/CT examinations. These studies highlight the discriminative
ability of deep learning architectures and its robustness as
computational framework supporting radiogenomics studies.
In data-driven models it is crucial to transparently
describe the methodology for the data handling by providing details
about subject stratification and data augmentation increasing trust
in the proposed experimental protocol and promoting reproducibility
of the results. In this regard, certain studies present limited
evidence regarding the fitting status of the examined models. In
particular, in a subset of the examined binary classification
problems (22,23,42)
the performance analysis is assessed only in terms of accuracy,
raising concerns for the employed model evaluation method. Deep
learning models are prone to overfitting and memorization
especially in small datasets or due to the adopted experimental
protocol. Moreover, details about the proposed data stratification
process in a subject or sample basis for splitting the original
dataset into training, validation and testing set are crucial
information with impact on the validity of the study.
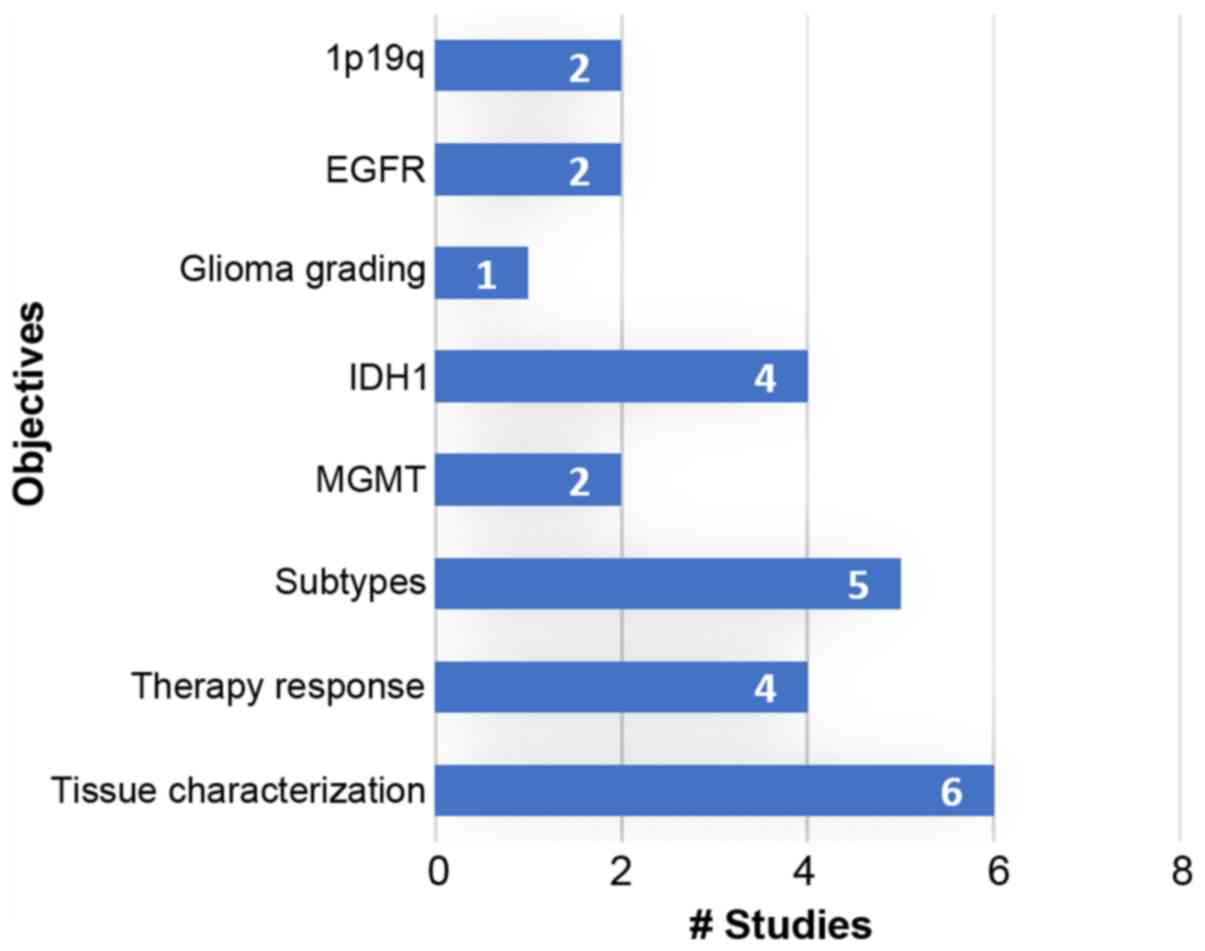
Specialized and open-access databases with
multimodal data (imaging, genomics, clinical and laboratory)
suitable for radiogenomics analysis could increase the interest of
the scientific community in this field. Novel research paradigms
are expected to exploit such high-dimensional data by discovering
novel associations and interplays among pathways and imaging
phenotypes contributing towards robust and accurate computer-aided
diagnosis systems. The majority of the current studies investigate
brain, breast and lung cancer for deep learning-based radiogenomic
analyses, as evidenced in Table
II and Fig. 4, mainly due to
the high prevalence of these cancers and the availability of
open-access databases. More efforts should be made to collect and
investigate such combined datasets, also from rare malignancies, in
order to enhance the role of DL-based radiogenomics in oncology
decision support systems.
Funding
Part of the present review was financially supported
by the Stavros Niarchos Foundation within the framework of the
project ARCHERS ('Advancing Young Researchers' Human Capital in
Cutting Edge Technologies in the Preservation of Cultural Heritage
and the Tackling of Societal Challenges').
Availability of data and materials
Not applicable.
Authors' contributions
ET and KM conceived and designed the study. ET and
KM researched the literature, performed analysis and interpretation
of data and drafted the manuscript. GZP, IS, AHK, LK, NP, DAS and
AT critically revised the article for important intellectual
content, and assisted in the literature search for this review
article. All authors agree to be accountable for all aspects of the
work in ensuring that questions related to the accuracy or
integrity of any part of the work are appropriately investigated,
and finally approved the version of the manuscript to be
published.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
DAS is the Editor-in-Chief for the journal, but had
no personal involvement in the reviewing process, or any influence
in terms of adjudicating on the final decision, for this article.
All the other authors declare that they have no competing
interests.
Acknowledgments
Not applicable.
Abbreviations:
|
RMS
|
rhabdomyosarcoma
|
|
ERMS
|
embryonal rhabdomyosarcoma
|
|
ARMS
|
alveolar rhabdomyosarcoma
|
|
NSCLC
|
non-small cell lung cancer
|
|
GBM
|
glioblastoma multiforme
|
|
DCIS
|
ductal carcinoma in situ
|
|
PCN
|
pancreatic cystic neoplasms
|
|
LNM
|
lymph node metastasis
|
|
IDH
|
isocitrate dehydrogenase MGMT
methylguanine methyltransferase
|
|
EGFR
|
epidermal growth factor receptor
|
|
HER2
|
human epidermal growth factor receptor
2
|
|
ER
|
estrogen receptor
|
|
PR
|
progesterone receptor
|
|
DNA
|
deoxyribonucleic
|
|
miRNA
|
micro-ribonucleic acid
|
|
RNA-seq
|
ribonucleic acid sequencing
|
|
H&E
|
hematoxylin and eosin
|
|
DCE-MRI
|
dynamic contrast enhanced magnetic
resonance imaging
|
|
DWI
|
diffusion weighted imaging
|
|
MRI
|
magnetic resonance imaging
|
|
FLAIR
|
fluid-attenuated inversion
recovery
|
|
18F-FDG PET
|
fluorodeoxyglucose positron emission
tomography
|
|
PET
|
positron emission tomography
|
|
CT
|
computerized tomography
|
|
AI
|
artificial intelligence
|
|
CNN
|
convolutional neural networks
|
|
AE
|
autoencoders
|
|
RNN
|
recurrent neural networks
|
|
LSTM
|
long-short term memory
|
|
ANN
|
artificial neural network
|
|
DNN
|
deep neural network
|
|
VGG
|
video geometry group
|
|
ResNet
|
residual network
|
|
SVM
|
support vector machine
|
|
ROI
|
region of interest
|
|
ACC
|
accuracy
|
|
AUC
|
area under the curve
|
|
SA:V
|
surface area to volume
|
|
BI-RADS
|
breast imaging reporting and data
system
|
|
TCGA-BRCA
|
The Cancer Genome Atlas Breast
Invasive Carcinoma
|
References
|
1
|
Woodard GA, Ray KM, Joe BN and Price ER:
Qualitative Radiogenomics: Association between Oncotype DX Test
Recurrence Score and BI-RADS Mammographic and Breast MR Imaging
Features. Radiology. 286:60–70. 2018. View Article : Google Scholar
|
|
2
|
Gevaert O, Echegaray S, Khuong A, Hoang
CD, Shrager JB, Jensen KC, Berry GJ, Guo HH, Lau C, Plevritis SK,
et al: Predictive radiogenomics modeling of EGFR mutation status in
lung cancer. Sci Rep. 7:416742017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zhou M, Leung A, Echegaray S, Gentles A,
Shrager JB, Jensen KC, Berry GJ, Plevritis SK, Rubin DL, Napel S,
et al: Non-small cell lung cancer radiogenomics map identifies
relationships between molecular and imaging phenotypes with
prognostic implications. Radiology. 286:307–315. 2018. View Article : Google Scholar
|
|
4
|
Hussein S, Green A, Watane A, Reiter D,
Chen X, Papadakis GZ, Wood B, Cypess A, Osman M and Bagci U:
Automatic segmentation and quantification of white and brown
adipose tissues from PET/CT scans. IEEE Trans Med Imaging.
36:734–744. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nitipir C, Niculae D, Orlov C, Barbu MA,
Popescu B, Popa AM, Pantea AMS, Stanciu AE, Galateanu B, Ginghina
O, et al: Update on radionuclide therapy in oncology. Oncol Lett.
14:7011–7015. 2017.
|
|
6
|
El-Maouche D, Sadowski SM, Papadakis GZ,
Guthrie L, Cottle-Delisle C, Merkel R, Millo C, Chen CC, Kebebew E
and Collins MT: 68Ga-DOTATATE for tumor localization in
tumor-induced osteomalacia. J Clin Endocrinol Metab. 101:3575–3581.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Jansen RW, van Amstel P, Martens RM, Kooi
IE, Wesseling P, de Langen AJ, Menke-Van der Houven van Oordt CW,
Jansen BHE, Moll AC, Dorsman JC, et al: Non-invasive tumor
genotyping using radiogenomic biomarkers, a systematic review and
oncology-wide pathway analysis. Oncotarget. 9:20134–20155. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ypsilantis PP, Siddique M, Sohn HM, Davies
A, Cook G, Goh V and Montana G: Predicting response to neoadjuvant
chemotherapy with PET imaging using convolutional neural networks.
PLoS One. 10:e01370362015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Fujishima H, Fumoto S, Shibata T, Nishiki
K, Tsukamoto Y, Etoh T, Moriyama M, Shiraishi N and Inomata M: A
17-molecule set as a predictor of complete response to neoadjuvant
chemotherapy with docetaxel, cisplatin, and 5-fluorouracil in
esophageal cancer. PLoS One. 12:e01880982017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bownes RJ, Turnbull AK, Martinez-Perez C,
Cameron DA, Sims AH and Oikonomidou O: On-treatment biomarkers can
improve prediction of response to neoadjuvant chemotherapy in
breast cancer. Breast Cancer Res. 21:732019. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Angus L, Smid M, Wilting SM, van Riet J,
Van Hoeck A, Nguyen L, Nik-Zainal S, Steenbruggen TG, Tjan-Heijnen
VCG, Labots M, et al: The genomic landscape of metastatic breast
cancer highlights changes in mutation and signature frequencies.
Nat Genet. 51:1450–1458. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Trivizakis E, Manikis GC, Nikiforaki K,
Drevelegas K, Constantinides M, Drevelegas A and Marias K:
Extending 2D convolutional neural networks to 3D for advancing deep
learning cancer classification with application to MRI liver tumor
differentiation. IEEE J Biomed Health Inform. 23:923–930. 2018.
View Article : Google Scholar
|
|
13
|
Lecun Y, Bottou L, Bengio Y and Haffner P:
Gradient-based learning applied to document recognition.
Proceedings of the IEEE. 86:2278–2324. 1998. View Article : Google Scholar
|
|
14
|
Sabour S, Frosst N and Hinton GE: Dynamic
routing between capsules. In: Proceedings of the 31st International
Conference on Neural Information Processing Systems; Curran
Associates Inc; Red Hook, NY. pp. 3856–3866. 2017
|
|
15
|
Szegedy C, Vanhoucke V, Ioffe S, Shlens J
and Wojna Z: Rethinking the inception architecture for computer
vision. In: Proceedings of the Conference on Computer Vision and
Pattern Recognition (CVPR); Las Vegas, NV. pp. 2818–2826. 2016
|
|
16
|
Huang G, Liu Z, van der Maaten L and
Weinberger KQ: Densely connected convolutional networks. In:
Proceedings of the Conference on Computer Vision and Pattern
Recognition (CVPR); Honolulu, HI. pp. 2261–2269. 2017
|
|
17
|
He K, Gkioxari G, Dollar P and Girshick R:
Mask R-CNN. In: Proceedings of the IEEE International Conference on
Computer Vision. IEEE International Conference on Computer Vision
(ICCV); pp. 2980–2988. 2017
|
|
18
|
Chang K, Bai HX, Zhou H, Su C, Bi WL,
Agbodza E, Kavouridis VK, Senders JT, Boaro A, Beers A, et al:
Residual convolutional neural network for the determination of IDH
status in low- and high-grade gliomas from mr imaging. Clin Cancer
Res. 24:1073–1081. 2018. View Article : Google Scholar
|
|
19
|
Chang P, Grinband J, Weinberg BD, Bardis
M, Khy M, Cadena G, Su MY, Cha S, Filippi CG, Bota D, et al:
Deep-learning convolutional neural networks accurately classify
genetic mutations in gliomas. AJNR Am J Neuroradiol. 39:1201–1207.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Li Z, Wang Y, Yu J, Guo Y and Cao W: Deep
Learning based Radiomics (DLR) and its usage in noninvasive IDH1
prediction for low grade glioma. Sci Rep. 7:54672017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Liang S, Zhang R, Liang D, Song T, Ai T,
Xia C, Xia L and Wang Y: Multimodal 3D densenet for IDH genotype
prediction in gliomas. Genes (Basel). 9:1–17. 2018. View Article : Google Scholar
|
|
22
|
Korfiatis P, Kline TL, Lachance DH, Parney
IF, Buckner JC and Erickson BJ: Residual deep convolutional neural
network predicts MGMT methylation status. J Digit Imaging.
30:622–628. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Akkus Z, Ali I, Sedlar J, Kline TL,
Agrawal JP, Parney IF, Giannini C and Erickson BJ: Predicting 1p19q
chromosomal deletion of low-grade gliomas from MR Images using deep
learning. arXiv:1611.06939. Accessed November 21, 2016.
|
|
24
|
Gupta T and Sarin R: Poor-prognosis
high-grade gliomas: Evolving an evidence-based standard of care.
Lancet Oncol. 3:557–564. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Decuyper M, Bonte S and van Holen R:
Binary glioma grading: Radiomics versus pre-trained CNN features.
In: Proceedings of the 21st International Conference. Part III;
Granada, Spain. pp. 498–505. 2018
|
|
26
|
Smedley NF and Hsu W: Using deep neural
networks for radiogenomic analysis. In: Proceedings of the 15th
International Symposium on Biomedical Imaging (ISBI 2018);
Washington, DC. pp. 1529–1533. 2018
|
|
27
|
Zhou Y, Li Z, Zhu H, Chen C, Gao M, Xu K
and Xu J: Holistic brain tumor screening and classification based
on densenet and recurrent neural network. In: Proceedings of the
International MICCAI Brainlesion Workshop; Springer; Cham. pp.
208–217. 2018
|
|
28
|
Momeni A, Thibault M and Gevaert O:
Dropout-enabled ensemble learning for multi-scale biomedical data.
In: Proceedings of the International MICCAI Brainlesion Workshop;
Springer; Cham: pp. 407–415. 2018
|
|
29
|
Afshar P, Mohammadi A and Plataniotis KN:
Brain tumor type classification via capsule networks. In:
Proceedings of the International Conference on Image Processing,
ICIP; IEEE; pp. 3129–3133. 2018
|
|
30
|
Molina JR, Yang P, Cassivi SD, Schild SE
and Adjei AA: Non-small cell lung cancer: Epidemiology, risk
factors, treatment, and survivorship. Mayo Clin Proc. 83:584–594.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Yu D, Zhou M, Yang F, Dong D, Gevaert O,
Liu Z, Shi J and Tian J: Convolutional neural networks for
predicting molecular profiles of non-small cell lung cancer. In:
Proceedings of the 14th International Symposium on Biomedical
Imaging (ISBI 2017); Melbourne, VIC. pp. 569–572. 2017
|
|
32
|
Wang S, Shi J, Ye Z, Dong D, Yu D, Zhou M,
Liu Y, Gevaert O, Wang K, Zhu Y, et al: Predicting EGFR mutation
status in lung adenocarcinoma on CT image using deep learning. Eur
Respir J. 53:18009862019. View Article : Google Scholar
|
|
33
|
Lingle W, Erickson BJ, Zuley ML, Jarosz R,
Bonaccio E, Filippini J and Gruszauskas N: Radiology data from the
cancer genome atlas breast invasive carcinoma [TCGA-BRCA]
collection. Cancer Imaging Arch. View Article : Google Scholar
|
|
34
|
Zhu Z, Albadawy E, Saha A, Zhang J,
Harowicz MR and Mazurowski MA: Deep learning for identifying
radiogenomic associations in breast cancer. Comput Biol Med.
109:85–90. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Ha R, Mutasa S, Karcich J, Gupta N,
Pascual Van Sant E, Nemer J, Sun M, Chang P, Liu MZ and
Jambawalikar S: Predicting breast cancer molecular subtype with MRI
dataset utilizing convolutional neural network algorithm. J Digit
Imaging. 32:276–282. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Yoon H, Ramanathan A, Alamudun F and
Tourassi G: Deep radiogenomics for predicting clinical phenotypes
in invasive breast cancer. In: Proceedings of the 14th
International Workshop on Breast Imaging (IWBI 2018); pp.
752018
|
|
37
|
Zhu Z, Harowicz M, Zhang J, Saha A, Grimm
LJ, Hwang ES and Mazurowski MA: Deep learning analysis of breast
MRIs for prediction of occult invasive disease in ductal carcinoma
in situ. Comput Biol Med. 115:1034982019. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Bibault JE, Giraud P, Durdux C, Taieb J,
Berger A, Coriat R, Chaussade S, Dousset B, Nordlinger B and Burgun
A: Deep Learning and Radiomics predict complete response after
neo-adjuvant chemoradiation for locally advanced rectal cancer. Sci
Rep. 8:1–8. 2018.
|
|
39
|
Chen W, Ji H, Feng J, Liu R, Yu Y, Zhou R
and Zhou J: Classification of pancreatic cystic neoplasms based on
multimodality images. In: Proceedings of the International Workshop
on Machine Learning in Medical Imaging (MLMI 2018); pp. 161–169.
2018
|
|
40
|
Cha KH, Hadjiiski LM, Chan H-P, Samala RK,
Cohan RH, Caoili EM, Paramagul C, Alva A and Weizer AZ: Bladder
cancer treatment response assessment using deep learning in CT with
transfer learning. In: Proceedings Volume 10134, Medical Imaging
2017: Computer-Aided Diagnosis; pp. 10134042017
|
|
41
|
Cha KH, Hadjiiski L, Chan HP, Weizer AZ,
Alva A, Cohan RH, Caoili EM, Paramagul C and Samala RK: Bladder
cancer treatment response assessment in CT using radiomics with
deep-learning. Sci Rep. 7:87382017. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Banerjee I, Crawley A, Bhethanabotla M,
Daldrup-Link HE and Rubin DL: Transfer learning on fused
multiparametric MR images for classifying histopathological
subtypes of rhabdomyosarcoma. Comput Med Imaging Graph. 65:167–175.
2018. View Article : Google Scholar
|
|
43
|
Zhou Z, Chen L, Sher D, Zhang Q, Shah J,
Pham NL, Jiang S and Wang J: Predicting lymph node metastasis in
head and neck cancer by combining many-objective radiomics and
3-dimensioal convolutional neural network through evidential
reasoning. arXiv180507021. Accessed May 18, 2018.
|
|
44
|
Pedano N, Flanders AE, Scarpace L,
Mikkelsen T, Eschbacher JM, Hermes B and Ostrom Q: Radiology data
from The Cancer Genome Atlas Low Grade Glioma [TCGA-LGG]
Collection. Cancer Imaging Arch. View Article : Google Scholar
|
|
45
|
Newitt D and Hylton N: Multi-center breast
DCE-MRI data and segmentations from patients in the I-SPY 1/ACRIN
6657 trials. Cancer Imaging Arch. View Article : Google Scholar
|
|
46
|
London AJ: Artificial intelligence and
black-box medical decisions: Accuracy versus explainability.
Hastings Cent Rep. 49:15–21. 2019. View Article : Google Scholar : PubMed/NCBI
|