Introduction
In lung cancer patients, metastases to the
peritoneum as well as to the spinal space are rare (1–10).
Carcinomatous meningitis, which attracts increasing attention as a
recurrence site in patients who received treatment with epidermal
growth factor receptor-tyrosine kinase inhibitors (EGFR-TKIs)
(2–8), is a devastating event occurring in
lung cancer patients (9–10) for which currently available
treatment options are limited and the prognosis remains poor
(1,9–10).
This is the presentation of a case of peritoneal and meningeal
relapse from lung adenocarcinoma following response to gefitinib
therapy. This case report conformed to the Ethical Guidelines for
Clinical Studies issued by the Ministry of Health, Labor and
Welfare of Japan. Comprehensive informed consent with regard to
clinical significance was obtained from the patient.
Case report
A 72-year-old woman was admitted to our hospital
complaining of a persistent cough that had appeared 2 months
before. The patient had never been a smoker and had no other
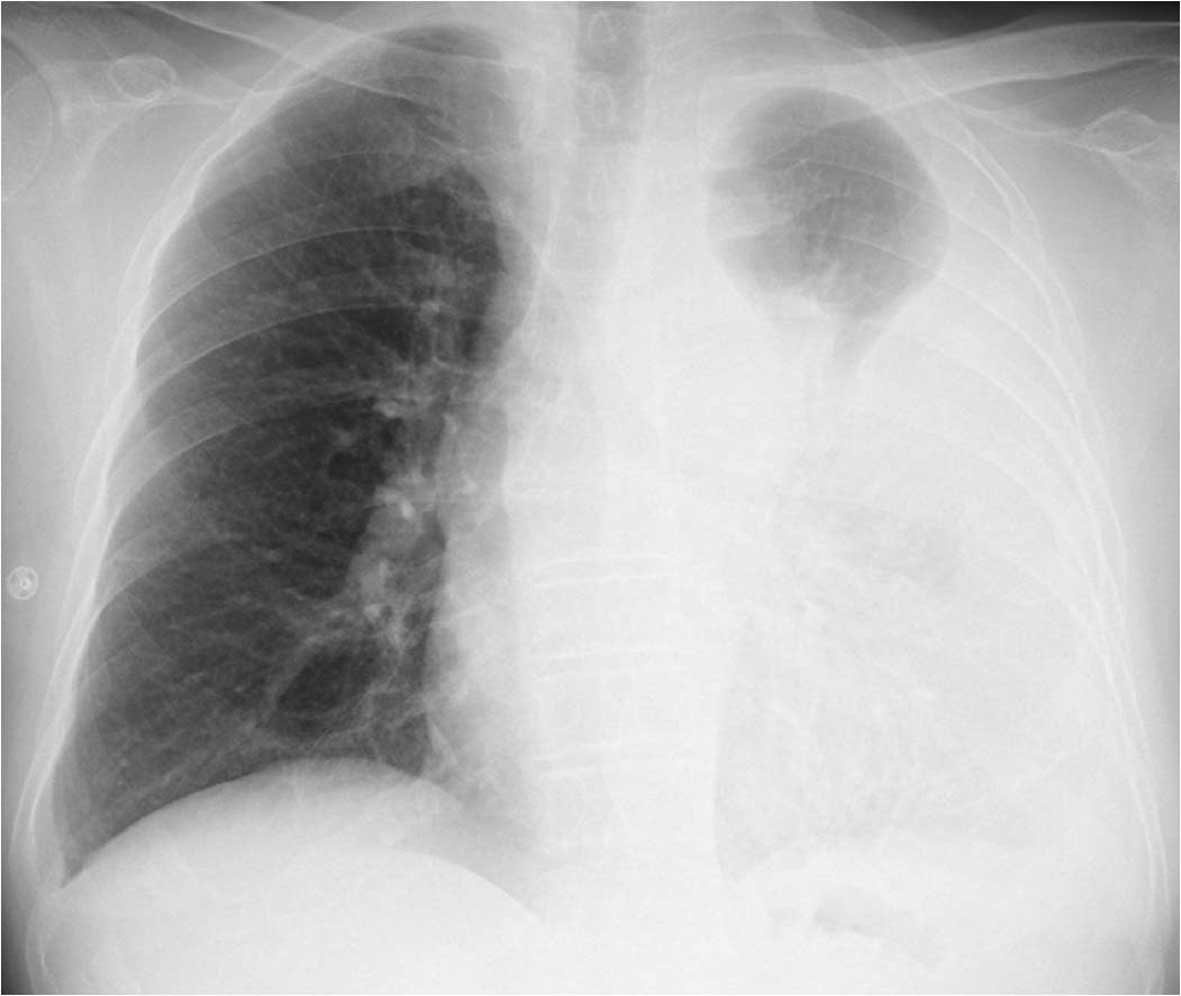
significant medical history. Chest radiograph at admission revealed
a loculated pleural effusion in the left hemithorax (Fig. 1). The cytological diagnosis of the
pleural fluid specimen was adenocarcinoma. Since there were no
distant metastases or tumorous lesions in other organs where
adenocarcinoma may develop, the diagnosis was lung
adenocarcinoma.
The patient received 4 courses of cisplatin-based
chemotherapy and the response was evaluated as partial. Two months
following the completion of chemotherapy, the patient developed
dyspnea on exertion due to reaccumulation of left pleural fluid and
the cytological pleural fluid specimens showed an EGFR mutation
(L858R point mutation in exon 21). Therefore, the patient was
started on 250 mg/day gefitinib therapy and the dyspnea disappeared
within 2 weeks. A grade 1 (National Cancer Institute common
toxicity criteria version 2.0) skin rash was observed, but it was
tolerable. Eight months after the initiation of gefitinib, the
patient developed abdominal distension, gait disturbance and visual
disorder of the right eye. Massive ascites were revealed by
abdominal computed tomography (CT) scan (Fig. 2). Positive lymph nodes were
identified around the abdominal aorta, although no metastatic
lesions were detected in the abdominal organs on the CT scan.
Adenocarcinoma cells were detected in the ascitic and pleural
fluids. Due to the deterioration of the performance status (PS 4),
the patient received supportive care and succumbed to the disease 2
months following peritoneal and meningeal relapse.
Discussion
Carcinomatous meningitis occurs in ∼5% of cancer
patients (11) and is considered
to be an oncological emergency requiring immediate treatment
(12). Treatment options include
whole-brain irradiation, systemic chemotherapy and intrathecal
chemotherapy, such as methotrexate (12). However, despite these treatments,
focal neurological dysfunctions do not improve in the majority of
cases (13) and the prognosis
remains poor, with a median survival of 2–3 months (12). Recently, the benefits of EGFR-TKIs
in the treatment of carcinomatous meningitis in patients with
non-small-cell lung cancer (NSCLC) have attracted attention,
although all studies were case reports or case series (2–8).
Furthermore, there is a high incidence of disease recurrence in the
brain and leptomeninges in NSCLC patients after response to
gefitinib treatment (14).
Metastatic involvement of the peritoneum is not a
rare autopsy finding (15–17). Based on previous studies, the
incidence of carcinomatous peritonitis is 2.7–16% in lung cancer
patients (15–17). However, carcinomatous peritonitis
from lung cancer is infrequently encountered and clinical reports
on this type of distant metastasis are rare. We previously reported
that 12 (1.2%) out of 1,041 patients with lung cancer developed
carcinomatous peritonitis (1). The
incidence of peritoneal carcinomatosis was high among patients with
adenocarcinoma. The median survival time from the diagnosis of
carcinomatous peritonitis was 2 months (1). Our previous and present findings,
taken together, suggest that ascites accompanying metastasis to
abdominal organs and pleural seeding in a patient with known lung
cancer should be regarded as metastasis (1).
A previous study by Su et al (18) also reported clinicopathological
findings in 30 lung cancer patients with carcinomatous peritonitis.
According to their findings, the most frequent abdominal symptom of
carcinomatous peritonitis was abdominal distension and the most
common histological type of lung cancer was adenocarcinoma. Eighty
percent of the patients developed malignant pleural effusions prior
to the diagnosis of carcinomatous peritonitis. Notably, 4 patients
with lung adenocarcinoma and carcinomatous peritonitis were treated
with gefitinib. Two of them, who responded to therapy, demonstrated
improved abdominal conditions with gradually diminishing ascites
and survived for 203 and 343 days, in marked contrast to the
previously reported poor median survival of 15 days (18). There is also another previous
report of a patient with lung adenocarcinoma and carcinomatous
peritonitis who responded to gefitinib therapy (19). It should be noted that these
patients were successfully treated for carcinomatous peritonitis by
gefitinib (18,19). However, there were also patients
with peritoneal recurrence following successful treatment with
gefitinib, such as the present case report. The existence of two
different responses (good response of peritonitis to gefitinib and
peritoneal recurrence following a good response to gefitinib),
seems to be similar to the observations made in lung cancer
patients with carcinomatous meningitis.
Irrespective of the peritoneal or subarachnoid
space, there may be other uncommon recurrence sites in lung cancer
patients. This suggests that such an unusual recurrence may be
associated with insufficient concentration of gefitinib at these
sites. Although it is rarely encountered, clinicians should remain
vigilant for this type of recurrence in lung cancer patients, even
following the successful treatment with EFFR-TKIs.
References
|
1.
|
Satoh H, Ishikawa H, Yamashita YT, et al:
Peritoneal carcinomatosis in lung cancer patients. Oncol Rep.
8:1305–1307. 2001.PubMed/NCBI
|
|
2.
|
Kim MK, Lee KH, Lee JK, et al: Gefitinib
is also active for carcinomatous meningitis in NSCLC. Lung Cancer.
50:265–269. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Yi HG, Kim HJ, Kim YJ, et al: Epidermal
growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) are
effective for leptomeningeal metastasis from non-small cell lung
cancer patients with sensitive EGFR mutation or other predictive
factors of good response for EGFR TKI. Lung Cancer. 65:80–84. 2009.
View Article : Google Scholar
|
|
4.
|
Langer C and Soria JC: The role of
anti-epidermal growth factor receptor and anti-vascular endothelial
growth factor therapies in the treatment of non-small-cell lung
cancer. Clin Lung Cancer. 11:82–90. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Katayama T, Shimizu J, Suda K, et al:
Efficacy of erlotinib for brain and leptomeningeal metastases in
patients with lung adenocarcinoma who showed initial good response
to gefitinib. J Thorac Oncol. 4:1415–1419. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Ruppert AM, Beau-Faller M, Neuville A, et
al: EGFR-TKI and lung adenocarcinoma with CNS relapse: interest of
molecular follow-up. Eur Respir J. 33:436–440. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Togashi Y, Masago K, Fukudo M, et al:
Cerebrospinal fluid concentration of erlotinib and its active
metabolite OSI-420 in patients with central nervous system
metastases of non-small cell lung cancer. J Thorac Oncol.
5:950–955. 2010.PubMed/NCBI
|
|
8.
|
Masuda T, Hattori N, Hamada A, et al:
Erlotinib efficacy and cerebrospinal fluid concentration in
patients with lung adenocarcinoma developing leptomeningeal
metastases during gefitinib therapy. Cancer Chemother Pharmacol.
67:1465–1469. 2011. View Article : Google Scholar
|
|
9.
|
Ano S, Satoh H, Nakazawa K, et al:
Malignant meningitis secondary to lung adenocarcinoma: an unusual
relapse. Intern Med. 46:1749–1751. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Jiménez Mateos A, Cabrera Naranjo F,
González Hernández A, et al: Neoplastic meningitis. Review of a
clinical series. Neurologia. 26:227–232. 2011.
|
|
11.
|
Grossman SA and Krabak MJ: Leptomeningeal
carcinomatosis. Cancer Treat Rev. 25:103–119. 1999. View Article : Google Scholar
|
|
12.
|
Wasserstrom WR, Glass JP and Posner JB:
Diagnosis and treatment of leptomeningeal metastases from solid
tumors: experience with 90 patients. Cancer. 49:759–772. 1982.
View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Strik H and Prömmel P: Diagnosis and
individualized therapy of neoplastic meningitis. Expert Rev
Anticancer Ther. 10:1137–1148. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Omuro AM, Kris MG, Miller VA, et al: High
incidence of disease recurrence in the brain and leptomeninges in
patients with nonsmall cell lung carcinoma after response to
gefitinib. Cancer. 103:2344–2248. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
McNeill PM, Wagman LD and Neifeld JP:
Small bowel metastases from primary carcinoma of the lung. Cancer.
59:1486–1489. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Abrams HL, Spiro R and Goldstein N:
Metastases in carcinoma; analysis of 1000 autopsied cases. Cancer.
3:74–85. 1950. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Warren S and Gates O: Lung cancer and
metastasis. Arch Pathol. 78:467–473. 1964.PubMed/NCBI
|
|
18.
|
Su HT, Tsai CM and Perng RP: Peritoneal
carcinomatosis in lung cancer. Respirology. 13:465–467. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Nakata H, Tuji T and Ohsaki Y: A case of
peritonitis carcinomatosa of pulmonary adenocarcinoma in which
gefitinib was effective. Cancer Chemother. 31:87–89. 2004.(In
Japanese).
|