Introduction
The pathogenesis of esophageal cancer has not been
fully elucidated and, despite the advances in surgical techniques
and treatments, its prognosis remains poor, since the disease is
usually diagnosed at an advanced stage (1–5).
Thus, prevention plays an important role in reducing mortality.
Numerous risk factors for esophageal cancer have been identified,
including tobacco smoking, alcohol intake, hot beverage intake,
family history of cancer and low fruit and vegetable intake
(4–8), the first two are considered to be the
most significant factors. These habits are correlated with the
disease at the individual level and are potentially modifiable
(9). Notably, the incidence of
esophageal squamous cell carcinoma (ESCC) is on the decrease in the
USA in association with a decline in smoking and alcohol intake
(10).
Several studies investigating the effects of smoking
and alcohol intake on the risk of esophageal cancer have
demonstrated that long duration, high consumption and the
interaction of these habits may increase the risk of ESCC (9,11–17).
However, with the exception of two studies which demonstrated that
the effects of smoking and alcohol intake on esophageal cancer may
differ according to gender (9,18),
to the best of our knowledge, only a limited number of large-scale
studies have investigated the association of the amount and
duration of smoking and alcohol intake with the risk of esophageal
cancer, while accounting for gender-specific effects.
In this study, the incidence of ESCC among Chinese
males was investigated by performing conditional logistic
regression analysis of the combined effects of the amount and
duration of smoking and alcohol intake on ESCC risk in a relatively
large study population of 1,070 males from a hospital-based
casecontrol study. The combined effects were estimated using a
variable that combined amount and duration. The reliability of our
results was subsequently confirmed by means of a simulation. The
aim of investigating the combined effects of amount and duration of
smoking and alcohol intake on the risk of ESCC was to provide
sufficient data to guide improvements in prevention strategies.
Materials and methods
Design
In this case-control study, each patient was
age-matched to a control subject (1:1 ratio) and a total of 535
pairs were enrolled.
Participants
A total of 571 Chinese male ESCC patients, aged
<60 years, were enrolled from the Fourth Hospital of Hebei
Medical University in Shijiazhuang, China. They were all residents
of Shijiazhuang and between January, 2002 and December, 2006 had
been diagnosed with histologically confirmed primary invasive ESCC,
as defined by the International Classification of Diseases, 10th
revision (ICD-10) diagnostic code (code, C15). In addition, 1,307
healthy male subjects, aged <60 years, were selected from the
same area and during the same time to serve as controls. All
controls had undergone medical checkups that verified the absence
of any medical conditions. The participants were informed on the
study objectives and content and provided informed consent prior to
enrollment. The study protocol was approved by the local Ethics
Committee and the Research Committee of Hebei Medical
University.
Risk factors
Trained interviewers used a structured questionnaire
to interview the participants. The questionnaire included questions
on demographic factors such as age, gender, smoking behavior (age
of initiation and cessation of smoking, duration of smoking and the
number of cigarettes per day), alcohol intake (age of initiation
and cessation of alcohol intake, duration of alcohol intake and
type and the quantity of alcoholic beverages consumed) and the
family history of esophageal cancer. A non-drinker was defined as
someone who consumed <1 alcoholic drink/month. Daily alcohol
intake (g ethanol/day) was calculated by considering the beverage
type and daily consumption. Beverage type was classified as
baijiu (the most popular Chinese alcoholic beverage), beer
or other hard liquor. One unit of consumption was defined as 50 ml
of baijiu, 400 ml of beer or 50 ml of hard liquor. The
content of pure alcohol was calculated as follows: 40% for
baijiu, 5% for beer and 40% for hard liquor. The resulting
values were expressed in grams by converting 1 ml of pure ethanol
to 0.789 g.
All continuous variables (number of cigarettes/day,
duration of smoking, daily alcohol intake and duration of alcohol
consumption) were assigned to categories of zero, low and heavy.
Absence of smoking or alcohol intake was categorized as zero
(reference group). To ensure equal sample sizes, median values were
used to divide tobacco smokers and alcohol drinkers into low and
heavy groups. Values ranging from >0 to the median were
classified as low and values greater than the median were
classified as heavy. The duration and amount categories were
subsequently combined to investigate the association of duration
and amount of smoking or alcohol intake with ESCC risk. The
combined smoking variable comprised 5 categories: no smoking, ≤20
cigarettes/day for ≤20 years, ≤20 cigarettes/day for >20 years,
>20 cigarettes/day for ≤20 years and >20 cigarettes/day for
>20 years. Five combined categories were created for alcohol
intake: no alcohol intake, ≤53.3 g ethanol/day for ≤20 years, ≤53.3
g ethanol/day for >20 years, >53.3 g ethanol/day for ≤20
years and >53.3 g ethanol/day for >20 years.
Statistical analysis
The individual risk factors for ESCC (i.e., family
history of esophageal cancer, combined smoking variable and
combined alcohol variable) were assessed by univariate conditional
logistic regression analysis, and unadjusted ORs and 95% CIs were
estimated. Multivariate conditional logistic regression analysis
was used to assess the association between the amount and duration
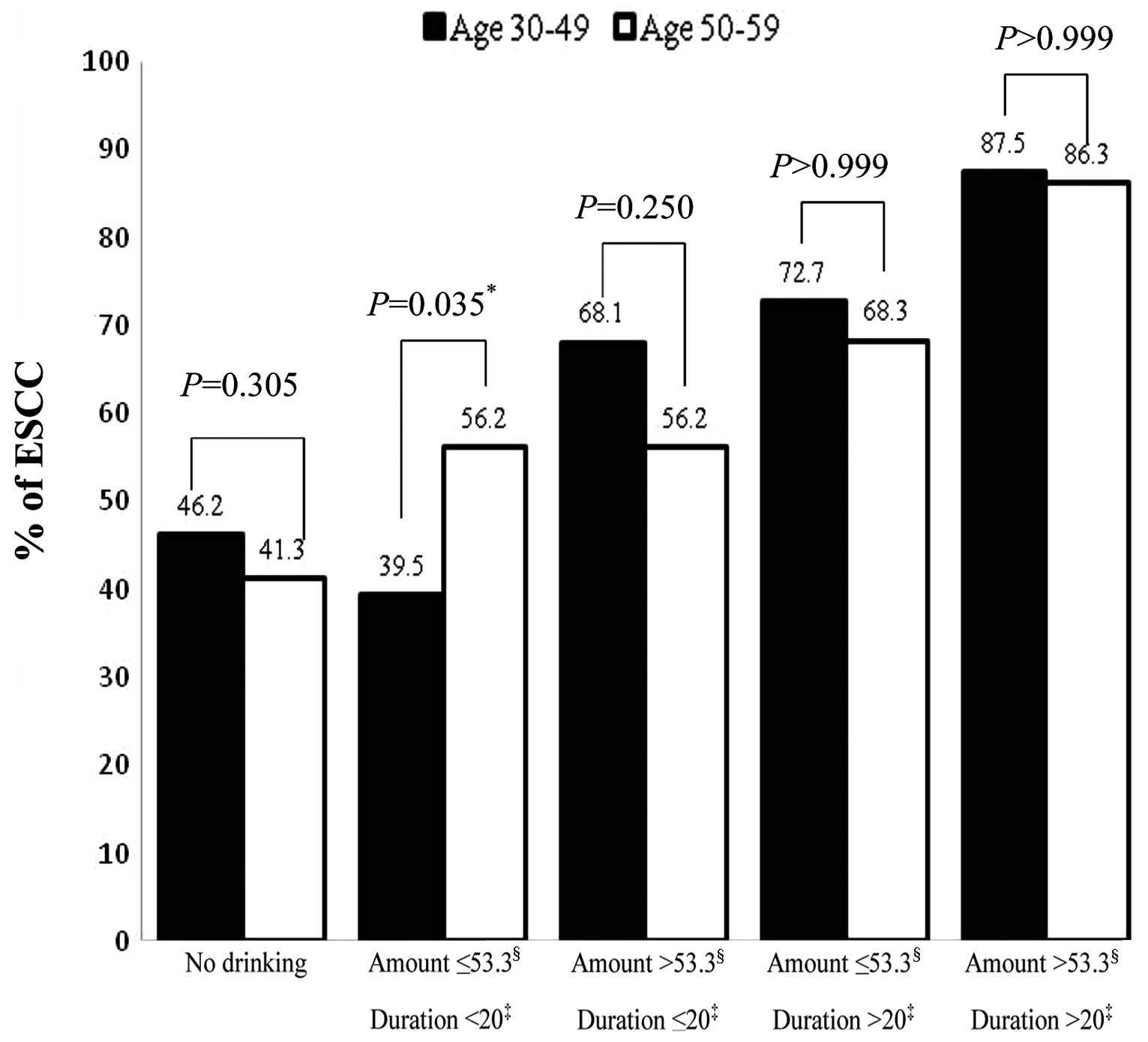
of smoking and alcohol intake and the risk of ESCC. Fisher’s exact
test was used to compare the proportion of ESCC cases between males
aged 30–49 and 50–59 years for each category of the combined
alcohol variable. Each proportion was shown in a bar graph to
demonstrate the likelihood of developing ESCC at a younger or older
age. P<0.05 was considered to indicate a statistically
significant difference. P values were derived from two-sided
statistical tests. Statistical analysis was performed using SAS
statistical software version 9.2 (SAS Institute Inc., Cary, NC,
USA).
Although the control for each case was randomly
selected from the candidate pool comprising several controls of
matching age, the OR estimates may have been inconsistant,
depending on the control selected. Therefore, a simulation study
was performed to evaluate the reliability of the OR estimates
obtained from the multivariate conditional logistic regression
analysis. Each simulation dataset included the 535 age-matched
pairs. The controls were randomly extracted from the original
database of 1,307 male controls, without replacement. For each
dataset, conditional logistic regression analysis was performed
with the previous three variables. This process was repeated 10,000
times, thus generating 10,000 estimates of coefficients and
standard errors for the variables. The simulation generated means
for coefficients and standard errors, which were used to produce a
summary of ORs and 95% CIs.
Results
Participant characteristics
Selected characteristics of patients and controls
are presented in Table I. A total
of 772 subjects (72.2%) were aged 50–59 years and 270 (25.2%) were
aged 40–49 years. These age groups represented 97.4% of the
participants. Overall, 82.8% of the alcohol drinkers also had a
smoking habit.
 | Table IParticipant characteristics and
association between individual risk factors and ESCC. |
Table I
Participant characteristics and
association between individual risk factors and ESCC.
| | | Univariate
conditional logistic regression |
|---|
| | |
|
|---|
| Variable | Control no. (%) | Patient no. (%) | Unadjusted OR (95%
CI) | P-value |
|---|
| Agea (years) |
| 30–39 | 14 (2.6) | 14 (2.6) | | |
| 40–49 | 135 (25.2) | 135 (25.2) | | |
| 50–59 | 386 (72.2) | 386 (72.2) | | |
| Smoking and drinking
status |
| No smoking or
drinking | 179 (33.5) | 119 (22.2) | | |
| Smoking | 185 (34.6) | 150 (28.0) | | |
| Drinking | 37 (6.9) | 38 (7.2) | | |
| Both smoking and
drinking | 134 (25.0) | 228 (42.6) | | |
| Family history of
esophageal cancer <0.001 |
| No | 454 (84.9) | 387 (72.3) | 1.00 (Reference) | |
| Yes | 81 (15.1) | 148 (27.7) | 2.10 (1.55–2.85) | |
| Combined smoking
variable <0.001 |
| No smoking | 216 (40.4) | 157 (29.3) | 1.00 (Reference) | |
| Amountb ≤20/durationc ≤20 | 146 (27.3) | 138 (25.8) | 1.25 (0.91–1.72) | 0.171 |
| Amountb ≤20/durationc >20 | 96 (17.9) | 144 (26.9) | 2.10 (1.49–2.95) | <0.001 |
| Amountb >20/durationc ≤20 | 32 (6.0) | 29 (5.4) | 1.20 (0.69–2.08) | 0.519 |
| Amountb >20/durationc >20 | 45 (8.4) | 67 (12.6) | 2.04 (1.32–3.16) | 0.001 |
| Combined alcohol
variable <0.001 |
| No drinking | 364 (68.0) | 269 (50.3) | 1.00 (Reference) | |
| Amountd ≤53.3/durationc ≤20 | 92 (17.2) | 89 (16.6) | 1.26 (0.89–1.79) | 0.196 |
| Amountd ≤53.3/durationc >20 | 24 (4.5) | 53 (9.9) | 2.71 (1.62–4.54) | <0.001 |
| Amountd >53.3/durationc ≤20 | 47 (8.8) | 73 (13.6) | 1.98 (1.32–2.95) | <0.001 |
| Amountd >53.3/durationc >20 | 8 (1.5) | 51 (9.6) | 8.50
(3.81–18.94) | <0.001 |
Univariate conditional logistic
regression
The univariate conditional logistic regression
analysis revealed that family history of esophageal cancer, the
combined smoking variable and the combined alcohol variable were
significantly associated with ESCC risk (P<0.001) (Table I). With regard to smoking, a
duration of ≤20 years was not a significant risk factor,
irrespective of the quantity of cigarettes smoked. With regard to
alcohol intake, all categories of the combined alcohol variable,
apart from an intake of ≤53.3 g ethanol for ≤20 years, were
significantly associated with ESCC risk.
Multivariate conditional logistic
regression
Multivariate analysis revealed that a family history
of esophageal cancer and the combined alcohol variable were
significantly associated with ESCC risk (P<0.001), although the
combined smoking variable was not (Table II). The OR (95% CI) associated
with a family history of esophageal cancer was 2.06 (1.48–2.85).
With regard to the combined alcohol variable, the OR (95% CI)
associated with an intake of ≤53.3 g ethanol/day for ≤20 years was
1.20 (0.83–1.74); with an intake of ≤53.3 g ethanol/day for >20
years, 2.28 (1.32–3.94); with an intake of >53.3 g ethanol/day
for ≤20 years, 1.91 (1.25–2.92); and with an intake of >53.3 g
ethanol/day for >20 years, 7.25 (3.12–16.83). All the categories
of the combined alcohol variable, apart from an intake of ≤53.3 g
ethanol/day for ≤20 years, were significantly associated with risk.
Alcohol intake for >20 years was a risk factor, as was a heavy
alcohol intake of >53.3 g ethanol/day. Heavy alcohol intake was
significantly associated with ESCC risk, even if the duration of
alcohol intake was ≤20 years.
 | Table IIResults of multivariate conditional
logistic regression analysis and simulation study. |
Table II
Results of multivariate conditional
logistic regression analysis and simulation study.
| | Multivariate
conditional logistic regression |
|---|
| |
|
|---|
| Risk factor | Age (years, means ±
SD) | Adjusted OR (95%
CI) | P-value | Simulation results
[mean OR (95% CI)] |
|---|
| Family history of
esophageal cancer (Reference = no esophageal cancer in
relatives) | | | <0.001 | |
| Yes | 52±5.0 | 2.06
(1.48–2.85)a | <0.001 | 2.08
(1.49–2.90)a |
| Combined smoking
variable (Reference = no smoking) | | | 0.193 | |
| Amountb ≤20/durationc ≤20 | 51±5.2 | 1.10
(0.77–1.56) | 0.601 | 0.97
(0.69–1.37) |
| Amountb ≤20/durationc >20 | 50±3.3 | 1.58
(1.09–2.31)a | 0.017 | 1.51
(1.02–2.22)a |
| Amountb >20/durationc ≤20 | 54±5.1 | 1.06
(0.59–1.90) | 0.857 | 0.85
(0.48–1.52) |
| Amountb >20/durationc >20 | 53±3.3 | 1.30
(0.79–2.12) | 0.302 | 1.33
(0.80–2.18) |
| Combined alcohol
variable (Reference = no drinking) | | | <0.001 | |
| Amountd ≤53.3/durationc ≤20 | 50±5.8 | 1.20
(0.83–1.74) | 0.329 | 1.39
(0.97–2.01) |
| Amountd ≤53.3/durationc >20 | 54±3.4 | 2.28
(1.32–3.94)a | 0.003 | 2.27
(1.30–3.95)a |
| Amountd >53.3/durationc ≤20 | 50±5.3 | 1.91
(1.25–2.92)a | 0.003 | 2.01
(1.30–3.10)a |
| Amountd >53.3/durationc >20 | 53±3.4 | 7.25
(3.12–16.83)a | <0.001 | 6.44
(2.85–14.57)a |
Comparison of the proportion of ESCC
among males aged 30–49 and 50–59 years by category of combined
alcohol variable
Among males who have consumed alcohol for ≤20 years,
the proportion of ESCC cases was higher among older males compared
with younger males with an intake of ≤53.3 g ethanol/day (P=0.035)
(Fig. 1). By contrast, the
proportion was higher among younger males compared with older males
with an intake of >53.3 g ethanol/day, although the difference
was not statistically significant (P=0.250). Thus, heavy alcohol
intake may lead to the development of ESCC at a younger age.
Simulation
The multivariate conditional logistic regression and
corresponding simulation study demonstrated that the same factors
were significantly associated with ESCC risk (Table II).
Discussion
Our analysis indicated that heavy alcohol intake
(>53.3 g ethanol/day) is an important risk factor for ESCC in
middle-aged Chinese males. In addition, heavy alcohol intake, even
of short duration, may lead to the development of ESCC at a younger
age. Smoking was not identified as a significant risk factor for
ESCC.
We investigated ESCC in a cohort of middle-aged
Chinese males, aged <60 years, for the following reasons:
although alcohol intake may be a dominant risk factor for both
sexes, a previous study by Wu et al(18) revealed that alcohol intake
increased the risk of ESCC risk in males, with an OR of 1.76 (95%
CI: 1.48–2.09). However, the association was not significant in
females, a finding which was supported by those of Castellsagué
et al(9), who observed that
alcohol intake was associated with esophageal cancer in males, with
an OR of 4.4 (95% CI: 3.1–6.2) and to a lesser extent in females,
with an OR of 2.2 (95% CI: 1.3–3.9). Against this background,
Chinese males were focused on in this study, as it would appear
that they may be at higher risk of developing ESCC compared to
females. Moreover, with regard to age, patients and controls aged
<60 years were recruited in this study in order to avoid the
numerous factors associated with cancer differentiation and
development in elderly adults.
Our study demonstrated a stronger association of
ESCC development with heavy alcohol intake, compared to long
duration of alcohol intake, confirming the findings of previous
studies (14,16,17).
When daily ethanol consumption exceeded 53.3 g, the risk of
developing ESCC within the next 20 years was increased. The exact
mechanism by which ethanol causes esophageal cancer has not been
elucidated, although several possible pathways have been proposed.
Although ethanol itself is not carcinogenic, its major intermediary
metabolite, acetaldehyde, is a known carcinogen in animals; alcohol
may act as a solvent that enhances the penetration of carcinogens
from other environmental sources; the regular intake of alcohol
consumption may reduce the intake and bioavailability of certain
nutrients that have chemopreventive properties; and alcohol may
directly irritate the esophageal epithelium, creating the potential
for ESCC pathogenesis (20).
Whereas heavy alcohol intake may yield more acetaldehyde and reduce
the intake and bioavailability of certain nutrients, the solvent
properties of alcohol and its ability to directly irritate the
esophageal epithelium are most likely causes for our observations
in middle-aged Chinese males. Firstly, the majority (82.8%) of the
alcohol drinkers in our study population were also smokers. Tobacco
contains the chemical carcinogen nitrosamine, as well as other
cancer-promoting agents (5). These
agents may act synergistically with ethanol to increase ESCC risk
(5) and our results may be
explained by the concurrence of the two habits. Secondly, it has
previously been demonstrated that exposure to a high concentration
of ethanol (40%) severely damaged the esophageal mucosa of rabbits,
whereas a lower concentration (20%) exerted a notably lower adverse
effect (21). Furthermore,
consumption of undiluted hard liquor (>40% ethanol) was found to
be significantly harmful, whereas wine, beer and hard liquor with a
non-alcoholic mixer were not (11,20).
With an ethanol content of 40–60%, baijiu is consumed
undiluted (22) and is the
beverage of choice among Chinese males, accounting for >1/3 of
all alcoholic beverages consumed in China (22). The high concentration of alcohol
may directly irritate the esophageal epithelium and lead to the
development of ESCC within a short period of time, i.e., at a
younger age.
Although a previous meta-analysis of worldwide data
demonstrated that smoking is an established risk factor for
esophageal cancer (23), according
to our data it was not a significant risk factor among our cohort
of middle-aged Chinese males. Evidence on the ESCC risk associated
with smoking in China is inconsistent. Weak associations with
tobacco have been reported in Chinese regions exhibiting a
significantly high risk for esophageal cancer, such as Linxian,
whereas strong associations have been reported in low-risk urban
areas (5,6,20,24).
The reason for the weaker association in these areas compared to
the rest of the world has not yet been elucidated. One hypothesis
is that there are other important risk factors in these high-risk
areas and that these factors account for the majority of ESCC
cases, thus reducing the effect of smoking (6). The lack of association in the present
study may also be due to the effect of other risk factors.
This hospital-based case-control study has several
limitations. Although the age-matched case-control design was used
to decrease the effects of potential confounding factors, ESCC risk
was estimated by only using information on alcohol intake, smoking
and family history of esophageal cancer. Other categories of
smoking and drinking, such as currently or formerly practiced, were
not investigated. Moreover, heavy alcohol intake may be correlated
with nutritional, socioeconomic or educational status, although we
were unable to collect data on other possible risk factors, such as
diet and social status. However, we believe that the limitations
mentioned above did not significantly affect the study findings, as
the differences among groups were too clear to have resulted from
such bias.
In conclusion, heavy alcohol intake, even of short
duration, is an important risk factor for ESCC in middle-aged
Chinese males. Specifically, middle-aged Chinese males who consume
>53.3 g ethanol/day (~170 ml of baijiu) are at high risk
of developing ESCC, even with a duration of heavy alcohol intake of
<20 years. This finding indicates that such individuals are at
high risk of developing ESCC at a younger age. The present findings
strongly suggest that limiting the consumption of undiluted hard
liquor may decrease the incidence of ESCC in the investigated
population.
Acknowledgements
The authors would like to thank the study
participants and the staff at the Fourth Hospital of Hebei Medical
University for their assistance.
Abbreviations:
|
CI
|
confidence interval
|
|
ESCC
|
esophageal squamous cell carcinoma
|
|
OR
|
odds ratio
|
References
|
1
|
Tew WP, Kelsen DP and Ilson DH: Targeted
therapies for esophageal cancer. Oncologist. 10:590–601. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chang AC, Ji H, Birkmeyer NJ, Orringer MB
and Birkmeyer JD: Outcomes after transhiatal and transthoracic
esophagectomy for cancer. Ann Thorac Surg. 85:424–429. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Enzinger PC and Mayer RJ: Esophageal
cancer. N Engl J Med. 349:2241–2252. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kollarova H, Machova L, Horakova D,
Janoutova G and Janout V: Epidemiology of esophageal cancer - an
overview. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub.
151:17–20. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mao WM, Zheng WH and Ling ZQ:
Epidemiologic risk factors for esophageal cancer development. Asian
Pac J Cancer Prev. 12:2461–2466. 2011.PubMed/NCBI
|
|
6
|
Kamangar F, Chow WH, Abnet CC and Dawsey
SM: Environmental causes of esophageal cancer. Gastroenterol Clin
North Am. 38:27–57. 2009. View Article : Google Scholar
|
|
7
|
Melhado R, Alderson D and Tucker O: The
changing face of esophageal cancer. Cancers. 2:1379–1404. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Castellsagué X, Muñoz N, De Stefani E,
Victora CG, Castelletto R and Rolón PA: Influence of mate drinking,
hot beverages and diet on esophageal cancer risk in South America.
Int J Cancer. 88:658–664. 2000.PubMed/NCBI
|
|
9
|
Castellsagué X, Muñoz N, De Stefani E,
Victora CG, Castelletto R, Rolón PA and Quintana MJ: Independent
and joint effects of tobacco smoking and alcohol drinking on the
risk of esophageal cancer in men and women. Int J Cancer.
82:657–664. 1999.PubMed/NCBI
|
|
10
|
Zhang HZ, Jin GF and Shen HB:
Epidemiological differences in esophageal cancer between Asian and
Western populations. Chin J Cancer. 31:281–286. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Castellsagué X, Quintana MJ, Martínez MC,
et al: The role of type of tobacco and type of alcoholic beverage
in oral carcinogenesis. Int J Cancer. 108:741–749. 2004.PubMed/NCBI
|
|
12
|
Franceschi S, Talamini R, Barra S, Barón
AE, Negri E, Bidoli E, Serraino D and La Vecchia C: Smoking and
drinking in relation to cancers of the oral cavity, pharynx,
larynx, and esophagus in northern Italy. Cancer Res. 50:6502–6507.
1990.PubMed/NCBI
|
|
13
|
Muwonge R, Ramadas K, Sankila R, Thara S,
Thomas G, Vinoda J and Sankaranarayanan R: Role of tobacco smoking,
chewing and alcohol drinking in the risk of oral cancer in
Trivandrum, India: a nested case-control design using incident
cancer cases. Oral Oncol. 44:446–454. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zambon P, Talamini R, La Vecchia C, Dal
Maso L, Negri E, Tognazzo S, Simonato L and Franceschi S: Smoking,
type of alcoholic beverage and squamous-cell oesophageal cancer in
northern Italy. Int J Cancer. 86:144–149. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lee CH, Lee JM, Wu DC, Hsu HK, Kao EL,
Huang HL, Wang TN, Huang MC and Wu MT: Independent and combined
effects of alcohol intake, tobacco smoking and betel quid chewing
on the risk of esophageal cancer in Taiwan. Int J Cancer.
113:475–482. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Launoy G, Milan CH, Faivre J, Pienkowski
P, Milan CI and Gignoux M: Alcohol, tobacco and oesophageal cancer:
effects of the duration of consumption, mean intake and current and
former consumption. Br J Cancer. 75:1389–1396. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chen J, Zhang N, Wakai T, Wei L, He Y,
Kumagai N, Kitsu K, Wang S and Akazawa K: Effect of the interaction
between the amount and duration of alcohol consumption and tobacco
smoking on the risk of esophageal cancer: A case-control study. Exp
Ther Med. 1:991–997. 2010.PubMed/NCBI
|
|
18
|
Wu M, Zhao JK, Zhang ZF, et al: Smoking
and alcohol drinking increased the risk of esophageal cancer among
Chinese men but not women in a high-risk population. Cancer Causes
Control. 22:649–657. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lundell LR: Etiology and risk factors for
esophageal carcinoma. Dig Dis. 28:641–644. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Fan Y, Yuan JM, Wang R, Gao YT and Yu MC:
Alcohol, tobacco, and diet in relation to esophageal cancer: the
Shanghai Cohort Study. Nutr Cancer. 60:354–363. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Salo JA: Ethanol-induced mucosal injury in
rabbit oesophagus. Scand J Gastroenterol. 18:713–721. 1983.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Cochrane J, Chen H, Conigrave KM and Hao
W: Alcohol use in China. Alcohol Alcohol. 38:537–542. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gandini S, Botteri E, Iodice S, Boniol M,
Lowenfels AB, Maisonneuve P and Boyle P: Tobacco smoking and
cancer: a meta-analysis. Int J Cancer. 122:155–164. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Tran GD, Sun XD, Abnet CC, Fan JH, Dawsey
SM, Dong ZW, Mark SD, Qiao YL and Taylor PR: Prospective study of
risk factors for esophageal and gastric cancers in the Linxian
general population trial cohort in China. Int J Cancer.
113:456–463. 2005. View Article : Google Scholar : PubMed/NCBI
|