Introduction
Lung cancer is the leading cause of cancer-related
mortality. Lung cancer patients are treated in outpatient clinics,
where systemic chemotherapy is administered. In addition, due to
the short survival time of advanced-stage patients, palliative care
is often provided at home in Japan and other countries.
Cancer patients frequently require emergency medical
care due to acute unbearable symptoms and life-threatening
conditions. In lung cancer particularly, the visits to the
emergency room (ER), admission to hospital from the ER and death in
the ER are more frequent compared to those in other types of cancer
(1,2). Mayer et al (3) investigated 37,760 cancer-related ER
visits in North Carolina, 9,297 of which were made by patients with
lung cancer (26.9%). Temel et al (4) reported that 48% of patients with
advanced non-small-cell lung carcinoma (NSCLC) visited the ER
within the 30 days preceding death. Moreover, only 32% of patients
with lung cancer who were admitted to the intensive care unit (ICU)
survived and only 11% of those who received mechanical ventilation
remained alive after 6 months (5).
Although frequent visits to the ER and poor prognosis are common in
lung cancer, no study has yet discriminated between cancer-related
and -unrelated issues as reasons for the ER visits.
It may be beneficial to avoid aggressive treatment
in end-of-life patients with advanced disease if cancer-related
issues are immediately diagnosed. By contrast, diseases which are
unrelated to cancer should be treated aggressively. For the purpose
of determining the appropriate emergency care of lung cancer
patients, we retrospectively overviewed the characteristics of
their ER visits.
Materials and methods
Sampling data from medical records
The medical records of consecutive lung cancer
patients who visited the ER between January, 2010 and December,
2011 were retrospectively reviewed. All the patients were
classified by histopathology and clinical stage at presentation in
the ER. The time of the visits was divided into night (0–8 h), day
(8–16 h) and evening (16–24 h). The means of arrival at the
hospital (e.g., ambulance or walk-in), admission/discharge from the
ER and hospital mortality were surveyed. The chief complaint was
defined as the main symptom causing the visit to the ER.
The patients’ diagnoses were classified as
cancer-related or -unrelated diseases on arrival at the ER. A
cancer-related issue was defined as symptoms caused by the cancer
itself (primary site and/or distant metastasis), endocrinological
disorders induced by the cancer and/or adverse effects of the
treatment, such as chemotherapy, radiotherapy and surgery.
Cancer-unrelated diseases were defined as comorbidities (chronic
diseases or acute syndromes) incidentally occurring in patients
with cancer.
This retrospective, single-institution,
observational study was approved by the Institutional Review Board
of Saitama Medical University International Medical Center in
2012.
Statistical analyses
The number of visits, proportion of cancer-related
issues, admission and hospital mortality were calculated for
patients at each cancer stage. The differences in the chief
complaints between patients with cancer-related vs. those with
cancer-unrelated diseases were also assessed using the Chi-square
test. The frequency of the major chief complaints in patients at
different clinical stages was visualized by plotting histograms.
The survivals of stage IV patients admitted through the ER were
compared using the Kaplan-Meier method. P<0.05 was considered to
indicate a statistically significant difference.
Results
Patients
Over a period of 2 years (2010–2011), 113 patients
with lung cancer visited the ER a total of 143 times (1.34% of the
total of 10,642 ER visits during that period). The lung cancer
patients were diagnosed as follows: 11 patients had small-cell lung
carcinoma (SCLC) and 102 had NSCLC, of whom 25 had squamous cell
carcinoma, 76 non-squamous cell carcinoma, with one patient
remaining unclassified. Among the 76 non-squamous cell carcinoma
cases, 24 harboured epidermal growth factor receptor (EGFR)
mutations. Of the 143 visits, the time from diagnosis of lung
cancer to visiting the ER was 14.2±17.5 months. The number of
patients at each clinical stage on presentation at the ER was 19
stage I, 13 stage II, 30 stage III and 81 stage IV patients. The
treatments administered within 4 weeks included surgery (10), radiotherapy (7), chemotherapy (46), tyrosine kinase
inhibitor (19) and palliative care alone (61). The majority of the
patients (92.6%) were regularly followed by medical oncologists in
our institution (Table I).
 | Table ICharacteristics of patients (n=113)
and their visits (n=143). |
Table I
Characteristics of patients (n=113)
and their visits (n=143).
| Characteristics | No. |
|---|
| Male/female | 90/23 |
| Age, years (mean ±
SD)a | 67±10 |
| Histology |
| SCLC | 11 |
| NSCLC |
| Squamous | 25 |
| Non-squamous | 76 |
| EGFR
mutation + | 24 |
| EGFR
mutation − | 52 |
| Unknown | 1 |
| Time after diagnosis
of lung cancer, months (mean ± SD) | 13.9±17.4 |
| Stage when visiting
the ER |
| I | 19 |
| II | 13 |
| III | 30 |
| IV | 81 |
| Treatment within 4
weeks |
| Surgery | 10 |
| Radiotherapy | 7 |
| Chemotherapy | 46 |
| Tyrosine kinase
inhibitor | 19 |
| Palliative care
alone | 61 |
| Attending
physician |
| Medical oncologists
in our institution | 131 |
| Doctors in other
institutions | 12 |
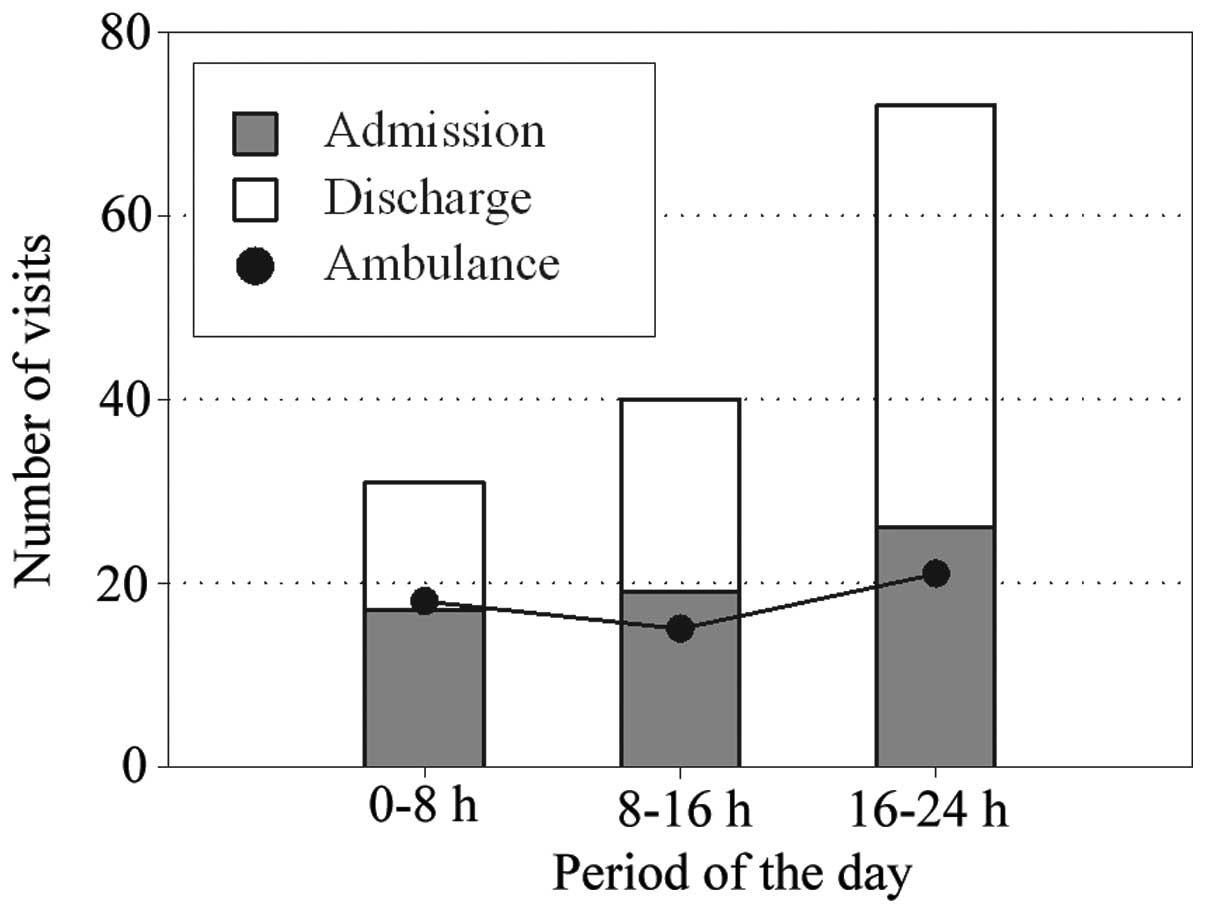
Approximately half of the patients visited the ER in
the evening (16–24 h), although the numbers of those requiring use
of an ambulance and those admitted were independent of the time of
day (Fig. 1).
Chief complaints
Respiratory symptoms (34.3%), pain (24.3%),
gastrointestinal (12.9%) and neurological signs (12.9%) and fever
(10.0%) were the most common complaints in patients with
cancer-related issues, whereas fever (30.1%), respiratory symptoms
(28.8%), pain (16.4%), gastrointestinal (9.6%) and neurological
signs (9.6%) were the predominant cancer-unrelated issues.
The chief complaints were stratified by the defined
criteria of cancer-related and -unrelated issues provided in
Materials and methods. With one exception, there were no
significant differences in the frequency of the complaints; fever
was significantly more frequent among patients with
cancer-unrelated compared to those with cancer-related issues
(P<0.01) (Table II). It was
not possible to distinguish between cancer-related or -unrelated
issues on the basis of the chief complaints at presentation in the
ER.
 | Table IIChief complaints on visiting the
ER. |
Table II
Chief complaints on visiting the
ER.
| Complaints | Cancer-related | Cancer-unrelated | P-value |
|---|
| Respiratory | 24 | 21 | 0.477 |
| Dyspnea | 20 | 19 | |
| Cough | 1 | 1 | |
| Hemoptysis | 3 | 1 | |
| Pain | 17 | 12 | 0.165 |
| Chest | 7 | 2 | |
| Back | 2 | 4 | |
| Abdominal | 2 | 5 | |
| Lumbar | 3 | 0 | |
| Others | 3 | 1 | |
| Gastrointestinal | 9 | 7 | 0.535 |
| Nausea/vomiting | 6 | 3 | |
| Anorexia | 2 | 2 | |
| Diarrhea | 0 | 1 | |
| Constipation | 1 | 0 | |
| Others | 0 | 1 | |
| Neurological | 9 | 7 | 0.535 |
| Unconsciousness | 4 | 2 | |
| Dizziness | 0 | 3 | |
| Seizure | 2 | 0 | |
| Others | 3 | 2 | |
| Malaise | 0 | 1 | 0.326 |
| Fever | 7 | 22 | 0.003 |
| Cardiological | 2 | 2 | 0.966 |
| Cardiac arrest | 2 | 1 | |
| Palpitations | 0 | 1 | |
| Others | 2 | 1 | 0.535 |
| Total | 70 | 73 | |
Causes of cancer-related and -unrelated
issues
A total of 70 visits (49.0%) were classified as
being caused by cancer-related issues and the remaining 73 (51.0%)
as being due to cancer-unrelated diseases (Table III). Among cancer-related issues,
direct invasion or distant metastasis were the most common causes
(n=31). A total of 17 visits were associated with the effects of
cancer treatment, such as chemotherapy, radiotherapy and surgery.
The most common causes of cancer-unrelated issues included
infection, cardiovascular symptoms and gastrointestinal events.
 | Table IIICancer-related and -unrelated causes
of ER visits. |
Table III
Cancer-related and -unrelated causes
of ER visits.
| A, Cancer-related
causes |
|---|
|
|---|
| Causes | No. | Admissions | Deaths |
|---|
| Intrathoracic
invasion | 15 | 10 | 2 |
| Airway
obstruction | 3 | 3 | 0 |
| Massive
hemoptysis | 3 | 1 | 0 |
| Pleuritis
carcinomatosa | 4 | 1 | 0 |
| Lymphangitis
carcinomatosa | 1 | 1 | 0 |
| Pericarditis
carcinomatosa | 2 | 2 | 0 |
| Respiratory
failure, others | 2 | 2 | 2 |
| Metastasis | 16 | 11 | 2 |
| Brain
metastasis | 7 | 7 | 1 |
| Meningitis
carcinomatosa | 1 | 1 | 0 |
| Peritonitis
carcinomatosa | 1 | 1 | 0 |
| Bone
metastasis | 7 | 2 | 1 |
| Cancer-related pain
(excluded above) | 8 | 3 | 0 |
| Advanced disease
(excluded above) | 8 | 3 | 1 |
| Hypercalcemia | 1 | 0 | 0 |
|
Chemotherapy-related | 10 | 3 | 1 |
| Radiation
therapy-related | 2 | 0 | 0 |
| Postoperative
complications | 5 | 1 | 0 |
| Others | 5 | 2 | 2 |
| Total | 70 | 33 | 8 |
|
| B, Cancer-unrelated
causes |
|
| Causes | No. | Admissions | Deaths |
|
| Respiratory
(total) | 34 | 18 | 5 |
|
Cold/pharyngitis | 8 | 0 | 0 |
| Bronchitis | 2 | 0 | 0 |
| Pneumonia | 14 | 10 | 1 |
| Respiratory
failure | 7 | 6 | 4 |
| Pneumothorax | 3 | 2 | 0 |
| Infection
(non-respiratory) | 8 | 3 | 0 |
|
Gastrointestinal | 10 | 2 | 1 |
| Cardiovascular | 6 | 3 | 0 |
| Neuromuscular | 12 | 1 | 0 |
| Endocrine | 1 | 1 | 0 |
| Others | 2 | 1 | 0 |
| Total | 73 | 29 | 6 |
Patients who required admission to the hospital from
the ER included 33 patients with cancer-related issues and 29 with
diseases unrelated to cancer. Brain metastasis was the most
frequent cancer-related issue, whereas respiratory problems were
the main causes of admission for cancer-unrelated reasons. A total
of 8 patients with cancer-related issues and 6 with
cancer-unrelated diseases succumbed in the hospital.
Association between ER use and cancer
stage
With cancer stage progression, the number of ER
visits, admissions, ambulance use and hospital mortalities were
increased. The proportion of patients who visited the ER due to
cancer-related reasons was significantly higher among stage IV
patients compared to that among patients with earlier-stage disease
(P<0.01). This also applied to admission (P<0.05) and
ambulance use (P<0.01) (Table
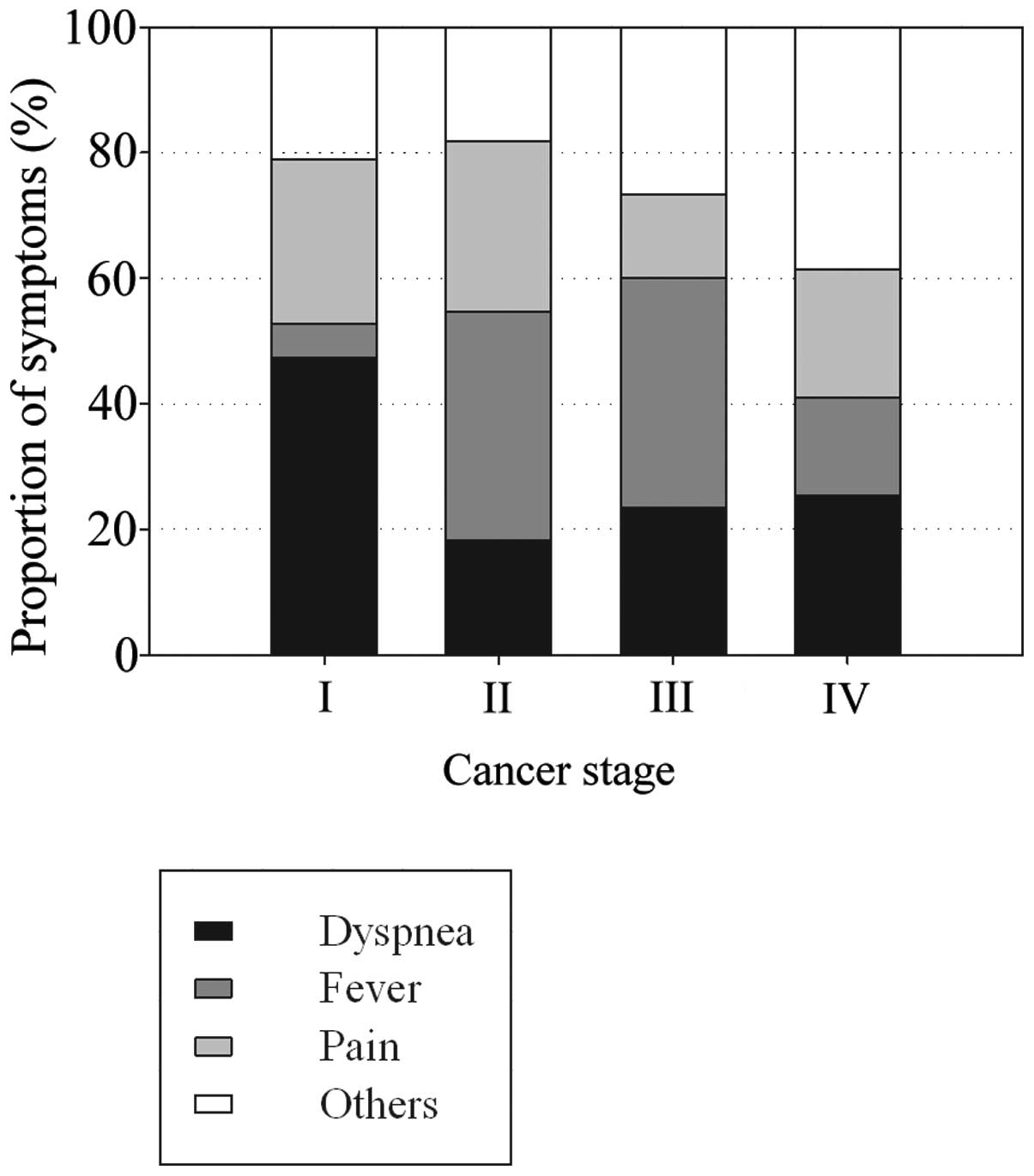
IV). As regards the three major symptoms (dyspnea, fever and
pain), dyspnea was the reason for almost half the visits by stage I
patients, whereas fever was common in stage II/III patients and the
symptoms were variable in stage IV patients (Fig. 2).
 | Table IVAssociation between cancer-related
and -unrelated visits and cancer stage. |
Table IV
Association between cancer-related
and -unrelated visits and cancer stage.
| Stage |
|---|
|
|
|---|
| Variables | I | II | III | IV |
|---|
| Total number of
visits |
|
Cancer-related | 3 | 1 | 12 | 54a |
|
Cancer-unrelated | 16a | 10a | 18 | 29 |
| Total number of
admissions |
|
Cancer-related | 0 | 0 | 5 | 28 |
|
Cancer-unrelated | 4 | 4 | 7 | 14 |
| Ambulance use |
|
Cancer-related | 1 | 0 | 3 | 28a |
|
Cancer-unrelated | 6 | 2 | 5 | 9 |
| Hospital
mortality |
|
Cancer-related | 0 | 0 | 0 | 8 |
|
Cancer-unrelated | 2 | 1 | 1 | 2 |
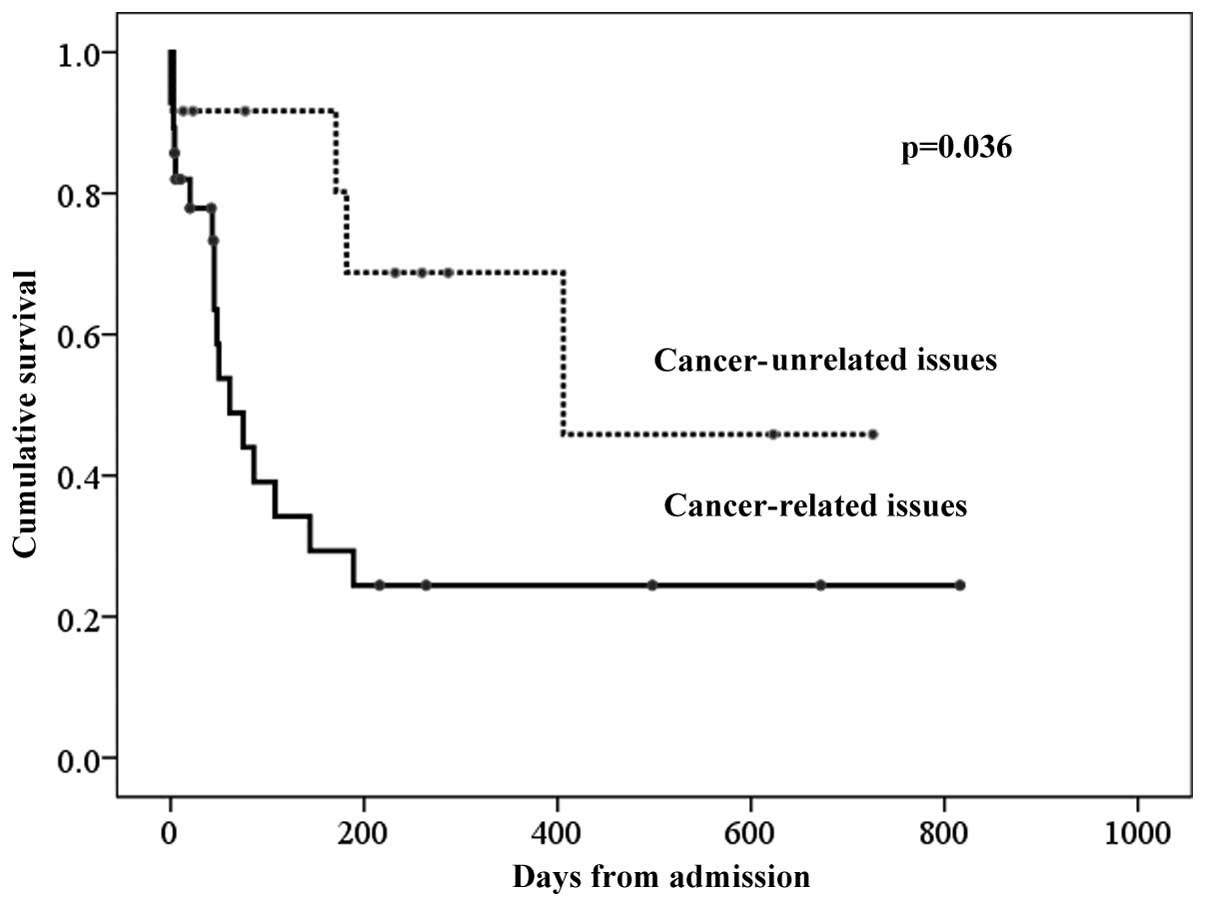
The overall median survival time (MST) of stage IV
patients from emergency admission was 144 days. The patients
admitted for cancer-related reasons exhibited a significantly
shorter MST compared to those admitted for cancer-unrelated disease
(61 vs. 406 days, respectively; P<0.05) (Fig. 3), indicating the validity of
distinguishing between cancer-related and -unrelated cases.
Discussion
This study demonstrated that outpatients with lung
cancer visited the ER at a similar frequency for cancer-related as
well as -unrelated reasons. We were unable to distinguish between
the two on the basis of their chief complaints; however, fever was
predominant among patients with cancer-unrelated problems.
Respiratory symptoms were common in patients with either
cancer-related or -unrelated issues. Cancer-related dyspnea was
predominant in advanced stages. Among the cancer-unrelated issues,
respiratory problems, such as respiratory tract infection and
chronic lung diseases, were commonly encountered. Fever was
frequently observed in patients visiting the ER for
cancer-unrelated issues for the same reason. Neutropenic fever
following chemotherapy was not often seen, which was consistent
with the findings of previous studies (3,6).
However, neutropenic fever should be diagnosed with caution due to
its significant morbidity and mortality (7).
Furthermore, in contrast to hospitalization for
stage IV lung cancer, the patients admitted for cancer-unrelated
issues had a relatively good prognosis. Thus, immediate diagnosis
at ER presentation is crucial for deciding on either intensive or
palliative care. End-of-life cancer care has become more aggressive
over the years (8). However, a
previous cohort study reported that 48% of the patients with
advanced NSCLC visited the ER within the month preceding death
(4). Another study reported that
only 32% of lung cancer patients admitted to the ICU survived and
only 11% of those requiring mechanical ventilation remained alive
after 6 months (5). Aggressive
end-of-life cancer care may thus be counterproductive in terms of
the patient’s quality of life and the utilization of medical
resources.
For the purpose of accurate diagnosis of treatable
cancer-related and -unrelated issues at presentation in the ER, we
recommend whole-body computed tomography to evaluate cancer
progression. Blood sampling may be useful for differential
diagnosis. Other possible tools for rapid diagnosis in the ER are
reportedly lung ultrasound (9) and
B-natriuretic peptide assay (10,11).
There were certain limitations to the present study.
First, the study was conducted at a single institution and the
results may not be representative of all lung cancer patients at
different centers. Second, there are differences in place of death
between Western countries and Japan. The majority of the patients
die in the hospital in Japan, whereas ~50% of lung cancer patients
die at home in the US (4). Third,
although we classified patients into those with cancer-related and
those with cancer-unrelated issues on the basis of reviewing their
medical records, it is possible that the two types coexisted in
some cases.
Visiting the ER for cancer-related issues may
reflect inadequate management during routine cancer care (12). The control of dyspnea is
particularly important, as was reflected by the fact that dyspnea
was the most frequent reason for visiting the ER (3), as well as for emergency admission;
dyspnea was also associated with poor prognosis (13–15).
In order to control dyspnea by regular routine care, opioids,
corticosteroids and home oxygen should be properly administered by
oncologists. Previous studies demonstrated that earlier and more
frequent palliative care consultations and greater family physician
continuity of care for terminal cancer patients resulted in a lower
incidence of ER visits (8,16). Another previous study revealed that
lung cancer patients who succumbed in an acute care hospital were
more likely to have presented with progressive thoracic symptoms
compared to those who died elsewhere (17). It was also reported that patients
preferred direct admission to the oncology ward compared to
admission through the ER (18).
Our study may contribute to the optimization of the
emergency care for lung cancer patients. However, further studies
should be conducted for each of the emergency issues associated
with lung cancer.
In conclusion, a similar fraction of outpatients
with lung cancer visited the ER due to cancer-related and
-unrelated events. Accurate differential diagnosis at presentation
in the ER is crucial for allotting appropriate emergency care to
patients with lung cancer.
Acknowledgements
We would like to thank NAI Inc. for the English
editing of our manuscript.
References
|
1
|
Barbera L, Taylor C and Dudgeon D: Why do
patients with cancer visit the emergency department near the end of
life? CMAJ. 182:563–568. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Leak A, Mayer DK, Wyss A, Travers D and
Waller A: Why do cancer patients die in the emergency department?
An analysis of 283 deaths in NC EDs. Am J Hosp Palliat Care.
30:178–182. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Mayer DK, Travers D, Wyss A, Leak A and
Waller A: Why do patients with cancer visit emergency departments?
Results of a 2008 population study in North Carolina. J Clin Oncol.
29:2683–2688. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Temel JS, McCannon J, Greer JA, et al:
Aggressiveness of care in a prospective cohort of patients with
advanced NSCLC. Cancer. 113:826–833. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Slatore CG, Cecere LM, Letourneau JL, et
al: Intensive care unit outcomes among patients with lung cancer in
the surveillance, epidemiology, and end results-medicare registry.
J Clin Oncol. 30:1686–1691. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
McKenzie H, Hayes L, White K, et al:
Chemotherapy outpatients’ unplanned presentations to hospital: a
retrospective study. Support Care Cancer. 19:963–969. 2011.
|
|
7
|
Cull LF and Nolan MB: Treating neutropenic
fever in the emergency department: delays may be deadly! J Emerg
Nurs. 35:36–39. 2009.PubMed/NCBI
|
|
8
|
Gonsalves WI, Tashi T, Krishnamurthy J, et
al: Effect of palliative care services on the aggressiveness of
end-of-life care in the Veteran’s Affairs cancer population. J
Palliat Med. 14:1231–1235. 2011.PubMed/NCBI
|
|
9
|
Volpicelli G and Frascisco M: Lung
ultrasound in the evaluation of patients with pleuritic pain in the
emergency department. J Emerg Med. 34:179–186. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Morrison LK, Harrison A, Krishnaswamy P,
Kazanegra R, Clopton P and Maisel A: Utility of a rapid
B-natriuretic peptide assay in differentiating congestive heart
failure from lung disease in patients presenting with dyspnea. J Am
Coll Cardiol. 39:202–209. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Schwam E: B-type natriuretic peptide for
diagnosis of heart failure in emergency department patients: a
critical appraisal. Acad Emerg Med. 11:686–691. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Barbera L, Paszat L and Chartier C:
Indicators of poor quality end-of-life cancer care in Ontario. J
Palliat Care. 22:12–17. 2006.PubMed/NCBI
|
|
13
|
Escalante CP, Martin CG, Elting LS, et al:
Dyspnea in cancer patients. Etiology, resource utilization, and
survival-implications in a managed care world. Cancer.
78:1314–1319. 1996.PubMed/NCBI
|
|
14
|
Escalante CP, Martin CG, Elting LS, et al:
Identifying risk factors for imminent death in cancer patients with
acute dyspnea. J Pain Symptom Manage. 20:318–325. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Geraci JM, Tsang W, Valdres RV and
Escalante CP: Progressive disease in patients with cancer
presenting to an emergency room with acute symptoms predicts
short-term mortality. Support Care Cancer. 14:1038–1045. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Burge F, Lawson B and Johnston G: Family
physician continuity of care and emergency department use in
end-of-life cancer care. Med Care. 41:992–1001. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Barbera L, Paszat L and Qiu F: End-of-life
care in lung cancer patients in Ontario: aggressiveness of care in
the population and a description of hospital admissions. J Pain
Symptom Manage. 35:267–274. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yates M and Barrett A: Oncological
emergency admissions to the Norfolk and Norwich University
Hospital: an audit of current arrangements and patient
satisfaction. Clin Oncol (R Coll Radiol). 21:226–233. 2009.
View Article : Google Scholar : PubMed/NCBI
|