Introduction
Lung cancer is the leading cause of cancer-related
mortality worldwide, accounting for 1.37 million deaths in 2008
(1). Lung cancer is generally
treated with surgical resection, chemotherapy, radiation therapy,
or combined modality approaches with curative intent. Among these
treatments, chemotherapy is the only applicable and recommended
treatment for patients with metastatic or relapsed lung cancer.
However the clinical efficacy of conventional cytotoxic
chemotherapy is insufficient, with a response rate (RR) of 20–40%
(2–4). Recently, ~80% of non-smoker Asian
adenocarcinoma lung cancer (AdLC) patients were found to have at
least one genetic abnormality in the epidermal growth factor
receptor (EGFR), v-Ki-ras2 Kirsten rat sarcoma viral oncogene
homolog (KRAS), echinoderm microtubule-associated protein-like
4-anaplastic lymphoma kinase (EML4-ALK), or human EGFR-related 2
genes (5). Treatment targeting the
aberrant proteins encoded by these genes has been the focus of
treatment for AdLC, which accounts for 45% of lung cancer cases. In
particular, patients harboring an EGFR mutation and an EML4-ALK
fusion respond remarkably to the EGFR tyrosine kinase inhibitors
(TKIs) erlotinib (RR, 70–83%) or gefitinib (RR, 62–73%) and the ALK
inhibitor crizotinib (RR, 57%), respectively (6). Thus, drugs targeting these aberrant
proteins have significantly improved the treatment outcome for lung
cancer patients. Similarly, an EGFR mutation is frequently
encountered among patients with adenosquamous carcinoma (ASC)
(7) and Iwanaga et al
(8) reported a case with ASC
harboring an EGFR mutation that responded significantly to EGFR-TKI
treatment. Conversely, in patients with pulmonary squamous cell
carcinoma (SCC), which accounts for 35% of lung cancer cases,
mutations in the EGFR or KRAS genes are extremely rare (9,10).
Marchetti et al (9) could
not find any mutations in the area encoding the tyrosine kinase
domain of EGFR in 454 SCC patients. Thus, in the treatment of SCC,
molecular-targeted therapy is not considered to be a suitable
approach and chemotherapy is limited to the use of conventional
cytotoxic antineoplastic drugs. Similarly, in other histological
subtypes, such as ASC, large-cell carcinoma (LCC), large-cell
neuroendocrine carcinoma (LCNEC) and small-cell lung carcinoma
(SCLC), the use of molecular-targeted drugs is not recommended, as
only a limited number of patients harbor targetable mutations
(11).
Recently, the concomitant administration of
dasatinib (a Src family protein TKI) and erlotinib reportedly
achieved a partial response in SCC patients (12). Additionally, patients who achieve
partial remission with dasatinib reportedly harbor mutations in the
gene encoding discoidin domain receptor 2 (DDR2) (13), a transmembrane receptor activated
by binding to extracellular collagen. In tumor cells, DDRs
interrupt normal cell-matrix communication and initiate
pro-migratory and pro-invasive cascades (14). Hammerman et al (13) recently reported that the
proliferation of SCC cell lines harboring DDR2 mutations was
inhibited by dasatinib in an in vitro study and that tumors
established from DDR2 mutant cell lines were highly responsive to
dasatinib in a xenograft model study. Those studies indicated the
possibility of dasatinib as a highly effective drug for SCC
patients harboring DDR2 mutations. In a study on European and North
American subjects, the frequency of mutations in DDR2 was reported
to be 3.2% in SCC (13), 0.5% in
AdLC (15) and 17% in LCC
(16), with no mutations
identified in SCLC and LCNEC patients. In addition, DDR2 mutations
were more often encountered in smokers compared to non-smokers
(17). Those studies indicated
that DDR2 may be a target molecule for the treatment of non-AdLC,
at least in European and North American subjects. However, ethnic
differences in the frequency of DDR2 mutations were not adequately
assessed, despite the presence of considerable ethnic genetic
variation, such as EGFR in AdLC, which has an exceptionally high
prevalence in East Asian populations (30–60%) and a low occurrence
in European and North American populations (10–20%) (18–21).
Thus, to select an appropriate therapeutic strategy, accurate data
on the frequencies of genetic mutations in non-AdLC (including SCC)
patients of different ethnic groups are required. In a recent
study, Sasaki et al (22)
failed to identify a DDR2 mutation in 166 Japanese SCC patients;
however, the authors only focused on mutations in the exons
encoding the receptor or transmembrane region. The available data
on the frequency of DDR2 mutations are not considered sufficient to
support the possible use of DDR2 mutations as a therapeutic target
for SCC patients, due to the lack of data in the region encoding
the kinase domain, which is considered to directly affect the
clinical efficacy of dasatinib. Thus, in the present study, we
investigated the frequency of mutations in DDR2 exons 5, 8 and
12–17; v-raf murine sarcoma viral oncogene homolog B1 (BRAF) V600E;
EGFR exons 19 and 21; and KRAS codons 12 and 13 in Japanese
non-AdLC patients to assess their potential use as therapeutic
biomarkers in the Japanese population.
Materials and methods
Patients and samples
We enrolled a total of 150 patients who had
undergone surgery for non-AdLC at the Gunma University Hospital
(Maebashi, Gunma, Japan) between December, 2003 and December, 2012,
including 87 SCC and 2 ASC patients who were previously reported by
Miyamae et al (23). This
study was approved by the Institutional Review Board for Clinical
Trials at the Gunma University Hospital and the Ethics Committee
for Human Genome Analysis of the Gunma University. Written consent
was obtained from all the participants after they had been informed
of the experimental procedure and the purpose of this study. The
resected tumor samples were immediately frozen and stored at −80°C
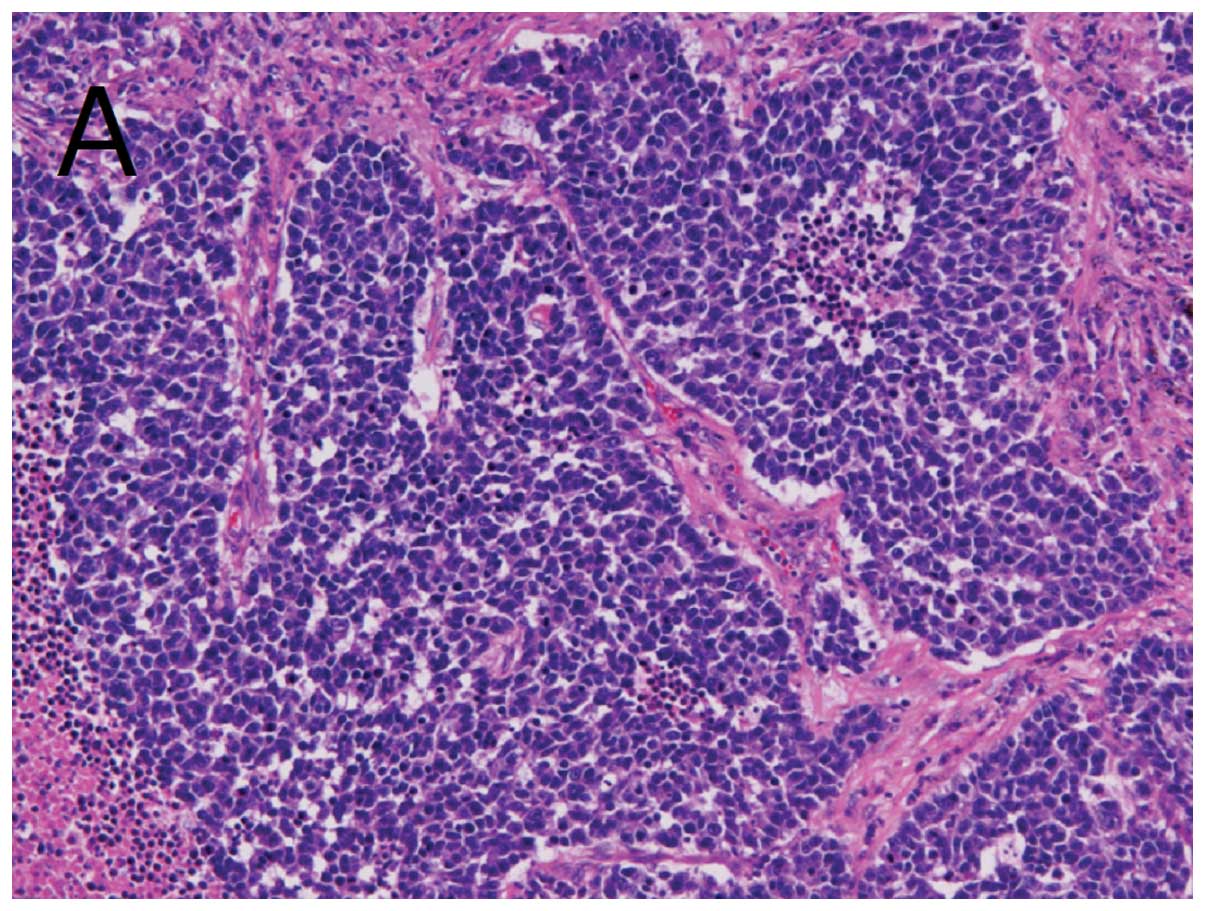
until DNA extraction. All the tumor tissue samples were diagnosed
as non-AdLC and the pathological subtype was determined by
hematoxylin and eosin staining. For the cases of poorly
differentiated and histologically atypical SCC or LCC and cases
harboring KRAS or EGFR mutations, additional immunostaining for p63
and thyroid transcription factor 1 was performed to confirm the
specific histological subtype. The cases diagnosed as SCLC or LCNEC
were confirmed to exhibit neuroendocrinological differentiation by
3 types of staining for neural cell adhesion molecule, chromogranin
A and synaptophysin.
Detection and characterization of
mutations
DNA samples were extracted from resected tumor
tissues using a QIAamp DNA mini kit (Qiagen, Hilden, Germany) and
were serially diluted to 50 ng/μl for use as DNA templates.
Mutations in EGFR exon 19 and KRAS codons 12 and 13 were detected
using the Sanger sequencing method according to previous studies
(24,25). Mutations in EGFR exon 21 were
detected by the Smart Amplification Process 2 assay, using an EGFR
mutation detection kit (K.K. DNAFORM, Kanagawa, Japan). BRAF V600E
mutations were detected using a LightMix kit for BRAF V600E (TIB
MolBiol, Berlin, Germany). Genetic variations in 8 exons of DDR2
(exons 5, 8 and 12–17), which reportedly affect the activity of the
protein or disease onset, were analyzed using the Sanger sequencing
method according to previous studies, with slight modifications
(13,26). Briefly, amplification was performed
using 0.5 U AmpliTaq Gold DNA polymerase (Applied Biosystems,
Foster City, CA, USA), 2.5 nmol of each dNTP, 1X polymerase chain
reaction buffer, 1.8 nmol MgCl2, 5 pmol of each forward
and reverse primer set and 25 ng of genomic DNA template in a
reaction volume of 12.5 μl. Polymerase chain reaction was performed
with an initial 5 min denaturation step at 95°C, followed by 35
cycles at 95°C for 30 sec, at 62°C for 35 sec and at 72°C for 45
sec, with a final elongation step at 72°C for 10 min. The annealing
temperature for exon 5 was set at 66°C to prevent non-specific
amplification.
Sequencing was performed with the Sanger dideoxy
method with fluorescent automated sequencing on an ABI 3130xl
Genetic Analyzer (Applied Biosystems) and the sequence data were
analyzed using Sequencing Analysis Software v5.4 (Applied
Biosystems).
In the patients whose cancer tissues were found to
harbor genetic mutations in EGFR, KRAS, BRAF or DDR2, genomic DNA
obtained from blood samples or peritumoral normal tissue was also
analyzed to confirm the mutations as somatic or germline.
Results
Patient characteristics and detection of
mutations
The characteristics of the patients are listed in
Table I. The patients’ age,
gender, smoking history and histological subtypes were comparable
to those of Japanese non-AdLC patients previously reported
(22). Among the 150 samples, a
previously unreported mutation in DDR2 (1:162748496) was identified
(Table II) in exon 17, near the
area encoding the tyrosine kinase domain and resulted in an amino
acid alteration (Phe804Ile). The same mutation was also detected in
the samples derived from the blood of each patient. Conversely, no
somatic mutation of DDR2 was detected in Japanese SCC, LCC, ASC,
LCNEC or SCLC patients (Table
III), whereas an unreported nonsense mutation (1:162746130) was
detected in 1 LCC patient (Table
II). Among the LCNEC and SCLC patients, 2 different non-coding
mutations, namely rs2271305 in exon 5 and rs3738807 in the upstream
region of exon 13, were detected in DDR2 (Table II).
 | Table ICharacteristics of the 150
non-adenocarcinoma patients used in this study. |
Table I
Characteristics of the 150
non-adenocarcinoma patients used in this study.
| Characteristics | No. (n=150) | % |
|---|
| Age, years (mean ±
SD) | 70.9±7.4 | |
| Gender |
| Male | 129 | 86.0 |
| Female | 21 | 14.0 |
| Histological
subtype |
| SCC | 116 | 77.33 |
| LCC | 3 | 2.00 |
| LCNEC | 11 | 7.33 |
| SCLC | 15 | 10.00 |
| ASC | 5 | 3.33 |
| Smoking history |
| Smoker | 144 | 96.0 |
| Never smoked | 6 | 4.0 |
| Brinkman index (mean
± SD) | 1,175±605 | |
| Pathological
stage |
| IA–IB | 102 | 68.0 |
| IIA–IIB | 28 | 18.7 |
| IIIA–IV | 20 | 13.3 |
 | Table IIFrequencies of DDR2 germline mutations
in each histological subtype. |
Table II
Frequencies of DDR2 germline mutations
in each histological subtype.
| | Minor allele
frequency (%) |
|---|
| |
|
|---|
| Histological
subtype | No. | rs2271305 | rs3738807 | 1:162748496 | 1:162746130 |
|---|
| SCC | 116 | C: 5.2 | C: 21.6 | A: 0.4 | T: 0.0 |
| LCC | 3 | C: 0.0 | C: 16.7 | A: 0.0 | T: 16.7 |
| LCNEC | 11 | C: 0.0 | C: 22.7 | A: 0.0 | T: 0.0 |
| SCLC | 15 | C: 10.0 | C: 20.0 | A: 0.0 | T: 0.0 |
| ASC | 5 | C: 10.0 | C: 40.0 | A: 0.0 | T: 0.0 |
| All patients | 150 | C: 4.9 | C: 20.4 | A: 0.3 | T: 0.3 |
 | Table IIIFrequencies of somatic mutations in
each histological subtype. |
Table III
Frequencies of somatic mutations in
each histological subtype.
| Histological
subtype | No. | Mutation |
|---|
|
|---|
| EGFR | KRAS | DDR2 | BRAF |
|---|
| SCC | 116 | 3 | 3 | 0 | 0 |
| LCC | 3 | 0 | 0 | 0 | 0 |
| LCNEC | 11 | 0 | 1 | 0 | 0 |
| SCLC | 15 | 0 | 0 | 0 | 0 |
| ASC | 5 | 3 | 0 | 0 | 0 |
| All patients | 150 | 6 | 4 | 0 | 0 |
Genetic mutations of EGFR exon 19 were detected in 3
SCC and 3 ASC patients and a mutation of KRAS codon 12 in 3 SCC
patients (including the cases that were previously reported by
Miyamae et al) and 1 LCNEC patient (Fig. 1 and Table III) (23). The EGFR and KRAS mutations were
mutually exclusive and their frequencies did not differ between
central and peripheral SCCs (Table
IV). BRAF V600E was not found in any of the patients (Table III).
 | Table IVCharacteristics of central and
peripheral squamous cell carcinoma. |
Table IV
Characteristics of central and
peripheral squamous cell carcinoma.
| Central type
(n=25) | Peripheral type
(n=91) |
|---|
|
|
|
|---|
| Mutations | No. (%) | No. (%) |
|---|
| Brinkman index
(mean ± SD) | 1,357±792 | 1,134±575 |
| EGFR mutation | 1 (4.0) | 2 (2.2) |
| KRAS mutation | 1 (4.0) | 2 (2.2) |
| DDR2 mutation | 0 (0.0) | 0 (0.0) |
| BRAF mutation | 0 (0.0) | 0 (0.0) |
Discussion
In a previous study on North American subjects,
somatic mutations of DDR2 were detected in 3.2% of SCC patients
(13). Similar to EGFR and KRAS
mutations, DDR2 mutations, particularly in the area encoding the
tyrosine kinase domain, are considered to affect the intracellular
downstream signaling pathways and lead to aberrant cell
proliferation. In the present study, we analyzed exons 5, 8 and
12–17 of DDR2, in which somatic mutations were identified in the
previous study on North American subjects; however, we did not
identify a somatic mutation in our Japanese patients. Moreover,
Sasaki et al (22) assessed
the genetic diversity of exons 3–7 and 9–12 of DDR2 in Japanese
patients and found no mutations. According to our results and those
of Sasaki et al, we concluded that, although DDR2 is
considered to be a candidate as a therapeutic target in European or
North American non-AdLC patients, DDR2 mutations may only rarely be
used as therapeutic targets in Japanese SCC patients, due to their
extremely low frequency. Moreover, if the previously reported DDR2
mutations found in North American subjects were defined as driver
mutations, our results suggested the possibility of racial
differences in the oncogenic mechanism underlying SCC, since there
is a racial difference in the frequency of these mutations. Similar
to SCC, we were unable to identify any DDR2 mutations in other
non-AdLC subtypes; however, a larger study is required to determine
the frequency of DDR2 mutations in LCC, SCLC, LCNEC and ASC
patients, as the sample size of our study was quite limited.
We identified an unreported germline mutation in
DDR2. Although this mutation cannot be a driver mutation, since it
is congenital, it may change the clinical efficacy of dasatinib
through altering the affinity of dasatinib to DDR2, as this
mutation is located in the area encoding the dasatinib-binding
site. Thus, a more detailed study is required to elucidate the
effect of this mutation on the clinical efficacy of dasatinib.
Conversely, we identified 6 somatic mutations in
EGFR and KRAS in Japanese SCC patients, despite the reportedly rare
frequency of such mutations in European and North American SCC
patients. Additionally, we detected EGFR mutations in 3 ASC
patients and KRAS mutations in 1 LCNEC patient. To the best of our
knowledge, this is first study including a LCNEC patient harboring
a KRAS mutation (27). These
mutations have been considered to be driver mutations and our
results indicated that EGFR or KRAS inhibitors may be effective for
a subset of SCC, LCNEC and ASC patients, at least in the Japanese
population. Indeed, the superior clinical effect of EGFR-TKIs in
Asian non-AdLC patients harboring an EGFR mutation was reported in
several studies (8,28,29)
and molecular-targeted therapy against the downstream effectors of
activated KRAS was reportedly more effective in patients harboring
a KRAS mutation (30,31). In certain studies, detection
sensitivity was discussed in depth, since highly sensitive methods
were required to detect somatic mutations in AdLC containing a
subpopulation of mutant cells mixed within an excess of normal
tissue. However, as we focused on non-AdLCs with a high cellularity
of tumoral tissue and a lower percentage of normal cells compared
to AdLC, we hypothesized that detection sensitivity did not affect
the data.
In the present study, the frequencies of EGFR and
KRAS mutations in peripheral SCCs, which are mainly encountered in
the Japanese population, were not different from those in central
SCCs, which are mainly encountered in European and North American
populations (32). These data
indicate that the difference in mutation frequency may be caused by
a difference in the cancer or oncogenic pathway between Japanese
and European and North American subjects, rather than by a
difference in the affected site.
As candidate therapeutic targets for non-AdLCs other
than DDR2, certain genetic aberrations have been reported,
including fibroblast growth factor receptor 1 amplification,
phosphatidylinositol-4,5-bisphosphate 3-kinase, catalytic subunit α
mutations, v-akt murine thymoma viral oncogene homolog 1 mutations
and phosphatase and tensin homolog mutations (33). Since our results suggested that
carcinogenic genes in non-AdLCs exhibit ethnic differences, a more
detailed evaluation of these candidate genes in different
ethnicities is required to make more appropriate suggestions for
personalized drug therapy. Furthermore, since dasatinib inhibits a
number of tyrosine kinases, including DDR2 (34), the association between the
expression level or mutations of tyrosine kinases and the efficacy
of dasatinib requires more detailed assessment.
In conclusion, this study suggests that DDR2
mutations and the BRAF V600E mutation may only rarely be used as
therapeutic targets, at least in Japanese non-AdLC patients;
however, EGFR and KRAS mutations may represent candidate
therapeutic targets in Japanese non-AdLC patients. The detection of
EGFR and KRAS mutations may be used to select the optimal treatment
for Japanese non-AdLC patients. Other genetic aberrations that may
be used as therapeutic targets should be assessed in detail among
different ethnic groups.
Acknowledgements
We would like to thank Ms. Aiko Matsumoto for the
secretarial assistance.
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar
|
|
2
|
Scagliotti GV, Parikh P, von Pawel J, et
al: Phase III study comparing cisplatin plus gemcitabine with
cisplatin plus pemetrexed in chemotherapy-naive patients with
advanced-stage non-small-cell lung cancer. J Clin Oncol.
26:3543–3551. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Schiller JH, Harrington D, Belani CP, et
al: Comparison of four chemotherapy regimens for advanced
non-small-cell lung cancer. N Engl J Med. 346:92–98. 2002.
View Article : Google Scholar
|
|
4
|
Sandler A, Gray R, Perry MC, et al:
Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell
lung cancer. N Engl J Med. 355:2542–2550. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sun Y, Ren Y, Fang Z, et al: Lung
adenocarcinoma from East Asian never-smokers is a disease largely
defined by targetable oncogenic mutant kinases. J Clin Oncol.
28:4616–4620. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gaughan EM and Costa DB: Genotype-driven
therapies for non-small cell lung cancer: focus on EGFR, KRAS and
ALK gene abnormalities. Ther Adv Med Oncol. 3:113–125. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Toyooka S, Yatabe Y, Tokumo M, et al:
Mutations of epidermal growth factor receptor and K-ras genes in
adenosquamous carcinoma of the lung. Int J Cancer. 118:1588–1590.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Iwanaga K, Sueoka-Aragane N, Nakamura T,
Mori D and Kimura S: The long-term survival of a patient with
adenosquamous lung carcinoma harboring EGFR-activating mutations
who was treated with gefitinib. Intern Med. 51:2771–2774. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Marchetti A, Martella C, Felicioni L, et
al: EGFR mutations in non-small-cell lung cancer: analysis of a
large series of cases and development of a rapid and sensitive
method for diagnostic screening with potential implications on
pharmacologic treatment. J Clin Oncol. 23:857–865. 2005. View Article : Google Scholar
|
|
10
|
Rekhtman N, Paik PK, Arcila ME, et al:
Clarifying the spectrum of driver oncogene mutations in
biomarker-verified squamous carcinoma of lung: lack of EGFR/KRAS
and presence of PIK3CA/AKT1 mutations. Clin Cancer Res.
18:1167–1176. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lindeman NI, Cagle PT, Beasley MB, et al:
Molecular testing guideline for selection of lung cancer patients
for EGFR and ALK tyrosine kinase inhibitors: guideline from the
College of American Pathologists, International Association for the
Study of Lung Cancer, and Association for Molecular Pathology. Arch
Pathol Lab Med. 137:828–860. 2013.
|
|
12
|
Haura EB, Tanvetyanon T, Chiappori A, et
al: Phase I/II study of the Src inhibitor dasatinib in combination
with erlotinib in advanced non-small-cell lung cancer. J Clin
Oncol. 28:1387–1394. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hammerman PS, Sos ML, Ramos AH, et al:
Mutations in the DDR2 kinase gene identify a novel therapeutic
target in squamous cell lung cancer. Cancer Discov. 1:78–89. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Valiathan RR, Marco M, Leitinger B, Kleer
CG and Fridman R: Discoidin domain receptor tyrosine kinases: new
players in cancer progression. Cancer Metastasis Rev. 31:295–321.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ding L, Getz G, Wheeler DA, et al: Somatic
mutations affect key pathways in lung adenocarcinoma. Nature.
455:1069–1075. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Davies H, Hunter C, Smith R, et al:
Somatic mutations of the protein kinase gene family in human lung
cancer. Cancer Res. 65:7591–7595. 2005.PubMed/NCBI
|
|
17
|
An SJ, Chen ZH, Su J, et al:
Identification of enriched driver gene alterations in subgroups of
non-small cell lung cancer patients based on histology and smoking
status. PLoS One. 7:e401092012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lynch TJ, Bell DW, Sordella R, et al:
Activating mutations in the epidermal growth factor receptor
underlying responsiveness of non-small-cell lung cancer to
gefitinib. N Engl J Med. 350:2129–2139. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Paez JG, Jänne PA, Lee JC, et al: EGFR
mutations in lung cancer: correlation with clinical response to
gefitinib therapy. Science. 304:1497–1500. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Pao W, Miller V, Zakowski M, et al: EGF
receptor gene mutations are common in lung cancers from ‘never
smokers’ and are associated with sensitivity of tumors to gefitinib
and erlotinib. Proc Natl Acad Sci USA. 101:13306–13311. 2004.
|
|
21
|
Calvo E and Baselga J: Ethnic differences
in response to epidermal growth factor receptor tyrosine kinase
inhibitors. J Clin Oncol. 24:2158–2163. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Sasaki H, Shitara M, Yokota K, et al: DDR2
polymorphisms and mRNA expression in lung cancers of Japanese
patients. Oncol Lett. 4:33–37. 2012.PubMed/NCBI
|
|
23
|
Miyamae Y, Shimizu K, Hirato J, et al:
Significance of epidermal growth factor receptor gene mutations in
squamous cell lung carcinoma. Oncol Rep. 25:921–928.
2011.PubMed/NCBI
|
|
24
|
Araki T, Shimizu K, Nakamura T, et al:
Clinical screening assay for EGFR exon 19 mutations using PNA-clamp
smart amplification process version 2 in lung adenocarcinoma. Oncol
Rep. 26:1213–1219. 2011.PubMed/NCBI
|
|
25
|
Araki T, Shimizu K, Nakamura K, et al:
Usefulness of peptide nucleic acid (PNA)-clamp smart amplification
process version 2 (SmartAmp2) for clinical diagnosis of KRAS codon
12 mutations in lung adenocarcinoma: comparison of PNA-clamp
SmartAmp2 and PCR-related methods. J Mol Diagn. 12:118–124. 2010.
View Article : Google Scholar
|
|
26
|
Ali BR, Xu H, Akawi NA, et al: Trafficking
defects and loss of ligand binding are the underlying causes of all
reported DDR2 missense mutations found in SMED-SL patients. Hum Mol
Genet. 19:2239–2250. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Iyoda A, Travis WD, Sarkaria IS, et al:
Expression profiling and identification of potential molecular
targets for therapy in pulmonary large-cell neuroendocrine
carcinoma. Exp Ther Med. 2:1041–1045. 2011.PubMed/NCBI
|
|
28
|
Tanaka K, Hata A, Kida Y, et al: Gefitinib
for a poor performance status patient with squamous cell carcinoma
of the lung harboring EGFR mutation. Intern Med. 51:659–661. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zhou C, Wu YL, Chen G, et al: Erlotinib
versus chemotherapy as first-line treatment for patients with
advanced EGFR mutation-positive non-small-cell lung cancer
(OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase
3 study. Lancet Oncol. 12:735–742. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Jänne PA, Shaw AT, Pereira JR, et al:
Selumetinib plus docetaxel for KRAS-mutant advanced non-small-cell
lung cancer: a randomised, multicentre, placebo-controlled, phase 2
study. Lancet Oncol. 14:38–47. 2013.PubMed/NCBI
|
|
31
|
Sequist LV, von Pawel J, Garmey EG, et al:
Randomized phase II study of erlotinib plus tivantinib versus
erlotinib plus placebo in previously treated non-small-cell lung
cancer. J Clin Oncol. 29:3307–3315. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Sakurai H, Asamura H, Watanabe S, Suzuki K
and Tsuchiya R: Clinicopathologic features of peripheral squamous
cell carcinoma of the lung. Ann Thorac Surg. 78:222–227. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Drilon A, Rekhtman N, Ladanyi M and Paik
P: Squamous-cell carcinomas of the lung: emerging biology,
controversies, and the promise of targeted therapy. Lancet Oncol.
13:e418–e426. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Montero JC, Seoane S, Ocaña A and
Pandiella A: Inhibition of SRC family kinases and receptor tyrosine
kinases by dasatinib: possible combinations in solid tumors. Clin
Cancer Res. 17:5546–5552. 2011. View Article : Google Scholar : PubMed/NCBI
|