Introduction
While meningioma is the most common pathological
form of intracranial tumor in the elderly (1), such patients often present with multiple
complications and have a poor prognosis (2,3). Seizures
are the most clinically significant complication (4,5) with early
postoperative seizures being defined as those appearing within the
first week after surgery (6). Brain
edema reaches a maximum level during the first week following
surgery, and during this time early postoperative seizures may
aggravate brain edema and intracranial hematomas, leading to poor
patient prognosis. Therefore, it is important to predict the
likelihood of postoperative seizures and subsequently select an
optimal prophylactic therapy.
Previous studies have revealed that seizures
following meningioma resection are associated with multiple
factors. Preoperative seizures, imageable peritumoral brain edema
(PTBE) and preoperative dyskinesia are all recognized risk factors
for early seizures following meningioma resection, while pre- and
postoperative prophylactic antiepileptic drugs appear to protect
against such early postoperative seizures. Tumors located in the
cortex, near the cortex and near functional areas are more
frequently complicated with early postoperative seizures (7,8). However,
previous studies have not examined whether these various
correlation factors influence each other, whether elderly
meningioma patients have distinct pathophysiological backgrounds
(2,3)
or whether the correlation factors for early postoperative seizures
are highly specific. A multifactorial logistic regression analysis
was performed of the clinical data obtained from 209 elderly
patients who had undergone a meningioma resection for the purpose
of further investigating the associations between the occurrence of
early seizures following meningioma resection and various clinical
correlation factors. An equation was subsequently developed, which
used these correlation factors to predict the likelihood of an
early post-operative seizure.
Patients and methods
General information
The clinical data obtained from 209 elderly patients
(mean age, 67.5 years; range, 65–76 years) who had been
hospitalized and undergone a meningioma resection in the First
Hospital of Jilin University (Changchun, China) between December
2000 and December 2010 were reviewed. Of these patients, 35 (17
males and 18 females) had experienced an early postoperative
seizure, while 174 patients (58 males and 116 females) had not. All
the patients had no history of seizures prior to surgery.
Clinical data collection
The medical records of all the patients were checked
for any history of preoperative seizures, aphesis or dyskinesia.
All the patients had been diagnosed by head magnetic resonance
imaging and/or computed tomography scans, and the gross tumor
volume, tumor site and any peritumoral brain edema (PTBE) were
preliminarily determined. Phenobarbital sodium (0.1 g
intramuscularly) was administered to all 209 patients 30 min prior
to the surgery, and Dilantin (5 mg/kg/day, oral) or sodium
valproate (15 mg/kg/day, oral) was administered to certain patients
as a pre- and/or postoperative prophylactic drug. Craniotomy for
meningioma resection was performed microscopically for all 209
patients. Tumor adhesion to peritumoral tissues, circumscription
between the tumor and normal tissues, blood supply and the original
site of the tumor were determined during surgery.
Statistical methods
A logistic regression analysis was performed using
SPSS for Windows, Version 15.0 (SPSS, Inc., Chicago, IL, USA).
Correlations of all the variables with early postoperative seizures
were determined by multifactorial logistic regression analysis.
Variables were selected by stepwise regression analysis. The
influence of each factor on early postoperative seizures was
analyzed by fitting a logistic regression equation and a
multifactorial logistic regression equation was established.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Main factors possibly associated with
early postoperative seizures
A total of 14 factors (gender, tumor site,
dyskinesia, PTBE, tumor diameter, pre- and postoperative
prophylaxes, surgery time, tumor adhesion, circumscription, blood
supply, intraoperative transfusion, original site of the tumor and
dysphasia) were grouped for analysis. The tumor site groups were
further divided into three subgroups: i) Superficial supratentorial
subgroup: Frontal, frontotemporal, frontoparietal, temporal,
temporoparietal, temporo-occipital, parietal, parietooccipital and
occipital regions; ii) deep supratentorial subgroup: Sphenoid
ridge, middle and anterior cranial fossae and saddle area; and iii)
subtentorial subgroups, including cerebellar hemispheres,
petroclival and cerebellopontine angle. The tumor diameter, surgery
time and blood supply groups were each individually divided into
three subgroups: Tumor diameter 1 (<3 cm), 2 (3–5 cm) and 3
(>5 cm); surgery time subgroups 1 (<2 h), 2 (2–4 h) and 3
(>4 h); and blood supply subgroups 1 (rich), 2 (medium) and 3
(poor). Original tumor site groups were subdivided into five
subgroups: i) Supratentorial convexity; ii) falx: Cerebral falx and
sagittal sinus; iii) deep basicranial and intracranial: Middle
cranial fossa, optic nerve, brainstem, petroclivas, sphenoid ridge,
anterior cranial fossa, choroid plexus, tuberculum sellae and
olfactory sulcus; iv) tentorium cerebelli: Tentorium cerebelli; and
v) subtentorial convexity. The remaining factors were established
as binary variables.
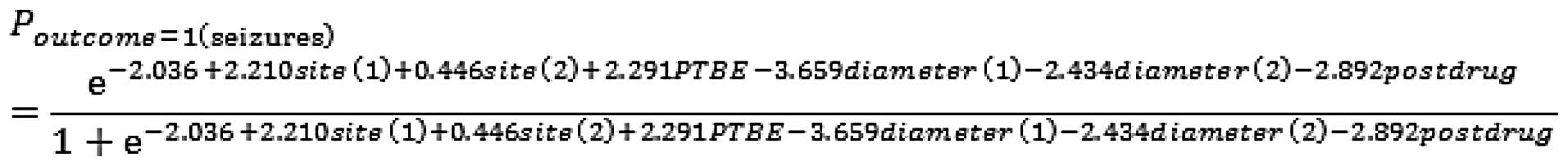
The logistic regression model was fitted using the
regrouped factors, and model variables were selected by stepwise
regression analysis. The four correlation factors: Tumor diameter
(Diameter), postoperative prophylactic antiepileptic drug
administration (Postdrug), PTBE and tumor site (Site), were entered
into the logistic regression model, and the other factors were
excluded. The odds ratio (OR) of the tumor diameter was >1,
making it a risk factor, while the OR of PPAD (postdrug) was <1,
making it a protective factor (P<0.05) (Table I). Two independent variables (‘Site’
and ‘Diameter’) were dummy-coded (Table
II).
 | Table I.Correlation analysis of early
postoperative seizures in elderly patients following meningioma
resection (1). |
Table I.
Correlation analysis of early
postoperative seizures in elderly patients following meningioma
resection (1).
| B | χ2 | df | P-value | OR | 95% CI of OR |
|---|
| Site (1) | 2.210 | 2.919 | 1 | 0.088 | 9.116 | (0.722,115.062) |
| Site (2) | 0.446 | 0.099 | 1 | 0.753 | 1.562 | (0.097, 25.053) |
| PTBE | 2.291 | 15.860 | 1 | <0.001 | 9.887 | (3.201, 30.534) |
| Diameter (1) | -3.659 | 20.629 | 1 | <0.001 | 0.026 | (0.005, 0.125) |
| Diameter (2) | -2.434 | 16.476 | 1 | <0.001 | 0.088 | (0.027, 0.284) |
| Postdrug | -2.892 | 14.719 | 1 | <0.001 | 0.055 | (0.013, 0.243) |
| Constant | -2.036 | 2.548 | 1 | 0.110 | 0.131 | |
 | Table II.Correlation analysis of early
postoperative seizures in elderly patients following meningioma
resection (2). |
Table II.
Correlation analysis of early
postoperative seizures in elderly patients following meningioma
resection (2).
|
|
|
| Parameter coding |
|---|
|
|
|
|
|
|---|
| Group | Team | Frequency | (1) | (2) | (3) | (4) |
|---|
| Diameter | 1.00 | 71 | 1.000 | 0.000 |
|
|
| 2.00 | 95 | 0.000 | 1.000 | | |
| 3.00 | 43 | 0.000 | 0.000 | |
| Site | 1.00 | 136 | 1.000 | 0.000 | | |
| 2.00 | 51 | 0.000 | 1.000 | | |
| 3.00 | 22 | 0.000 | 0.000 | | |
Statistical analysis
Statistical calculations indicated that four factors
(Diameter, Postdrug, PTBE and Site) were significantly correlated
with early postoperative seizures in the elderly patients
(P<0.05) (Tables I and II).
Based on these results, the possible occurrence of
an early postoperative seizure could be represented by the
following logistic regression equation:
(χ2 goodness of fit test for the logistic
regression test: P=0.713, sensitivity=74.3%,
specificity=91.4%).
The χ2 goodness of fit test was
statistically significant as the P-value was >0.05. Application
of this regression equation to data from each patient produced a
number ranging from zero to one. A value of 1 or close to 1
indicated a high probability of an early postoperative seizure,
while a value close to zero indicated a low probability of an early
postoperative seizure.
Discussion
Meningioma is the most common pathological form of
intracranial tumor in the elderly (1). Multiple factors lead to an unfavorable
prognosis and markedly higher incidence of complications in elderly
patients following surgery for intracranial meningioma (9–11). Elderly
patients may have various degrees of compromised physical function
and complications with comorbidities in other systems. In addition,
meningiomas in the elderly are characterized by their growth and
produce only slightly increased intracranial pressure and
incidences of atypical clinical manifestations due to brain
atrophy. Additionally, meningioma tumors are usually located in
areas of the brain not associated with physical functions (12,13).
Seizures following intracranial meningioma resection
represent a serious complication, and the molecular and cellular
mechanisms of tumor-induced seizures are not fully understood.
However, previously suggested mechanisms for seizure include focal
cortical hypoxia, a direct mass effect, PTBE, peripheral cortical
damage and changes in levels of excitatory amino acids. Seizures
tend to be the first symptom of an intracranial tumor and may
further aggravate brain damage and increase the risk of an
unfavorable prognosis based on the underlying disease (4,14). In
particular, early postoperative seizures occur within one week
following surgery and often aggravate the pathological damage to
brain tissue and biochemical changes in nerves caused by underlying
disease (15). Information gained
from a study of clinical factors correlated with early
postoperative seizures in elderly patients following meningioma
resection may significantly help to improve patient prognosis.
Previous studies have reported that seizures following meningioma
resection are associated with multiple clinical factors (4,5,7,8), such as a
history of preoperative seizures, imageable PTBE and preoperative
dyskinesia. Tumors located in the cortex, near cortex and near
functional areas are more likely to be associated with
postoperative seizures, while pre- and postoperative prophylactic
antiepileptic drugs have been shown to reduce the incidence of
seizures. However, no previous study has investigated the clinical
factors associated with early postoperative seizures in elderly
patients following meningioma resection. The present study used
multiple regression analysis to examine the correlation of early
postoperative seizures with several clinical factors (gender, tumor
site, dyskinesia, PTBE, tumor diameter, pre- and postoperative
prophylaxes, surgery time, tumor adhesion, circumscription, blood
supply, intraoperative transfusion, original site of the tumor and
dysphasia) in a cohort of 209 elderly patients who had undergone a
meningioma resection.
Meningiomas are usually slow growing tumors, and
their induced seizures are often a result of mechanical
compression. Compression of peritumoral brain tissue may destroy
the neural network structure; however, neuronal shortcuts leading
to a histological basis for interictal epileptiform discharges may
appear following pathological reconstruction of the network
(16,17). Intracalvarial invasion by a meningioma
produces mechanical compression and localized damage to the brain,
and the incidence of seizures increases with the volume occupied.
In addition, slow growing tumors may cause edema and ischemia in
surrounding brain tissues, secondary brain parenchymal atrophy and
gliosis, neuronal metabolic disturbance and abnormal depolarization
of cell membranes. Such changes lead to epileptic seizures evoked
by abnormal neuronal discharges during tumor growth (14,18). The
majority of the elderly patients in the present study cohort showed
signs of pathological underlying brain parenchymal atrophy and
cerebral ischemia. The slow growth of their meningiomas and
subsequent development of clinical manifestations may have resulted
in chronically and mechanically compressed peritumoral brain
tissues and damaged neural network structures, which provided a
histological basis for seizures. In the study, a multifactorial
logistic regression analysis was performed of the clinical data
obtained from 209 elderly patients who had undergone a meningioma
resection. The results showed that the OR was maximal in tumor
diameter group 3 (1.000) and minimal in tumor diameter group 1
(0.026), suggesting that the odds of an early postoperative seizure
increased with increasing tumor diameter.
Results of a retrospective study by Kawugachi et
al (19) indicated that PTBE was
a significant epileptogenic factor. Tumor-evoked compression or
stimulation of brain tissue results in gliosis, which later causes
PTBE, tumidness, insufficient blood supply, anoxia, gradual brain
atrophy, cerebral sclerosis, proliferation of glial cells and
fibers, loss of partial ganglion cells and the formation of fine
insular phagocyte-like lesions. The membranes of these altered
pathological nerve cells can stimulate allergic reactions and cause
clinical seizures by sudden and transient neuronal discharges
induced by endogenous or exogenous stimuli (16). According to Lieu and Howng (5), clinically significant seizures can be
caused by supratentorial or convexity meningiomas complicated with
severe PTBE. The present study concluded that the OR of PTBE was
9.887, suggesting that the odds of an early postoperative seizure
occurring in an elderly patient with meningioma complicated with
definite PTBE were almost 10-fold greater than those in a patient
without PTBE. This result is in accordance with the above-mentioned
study. Previous studies (20–22) have demonstrated that perioperative
administration of prophylactic antiepileptic drugs can prevent
partial seizures from evolving into persistent ones, and markedly
reduce or avoid seizure-induced brain damage. Other studies
(23–25) have indicated that prophylactic
Dilantin and sodium valproate can reduce the incidence of
postoperative seizures, and that no significant difference was
noted between the results achieved with the two drugs. Therefore,
the present study did not distinguish between these two
prophylactic antiepileptic drugs when they were used in patient
treatment. The results showed a significant difference in the
incidence of postoperative seizures in elderly patients who did and
did not receive a prophylactic antiepileptic drug. However, use of
preoperative prophylactic antiepileptic drugs was not included in
the multifactorial stepwise logistic regression; therefore, no
statistical evidence is available to indicate that the results were
different from those reported in previous studies conducted with
patients of all ages (15). In this
study, phenobarbital sodium, a temporary prophylactic antiepileptic
drug, was administered intramuscularly to all patients 30 min
before surgery, and this factor may have impacted the correlation
between preoperative administration of prophylactic antiepileptic
drugs and early postoperative seizures. However, the elderly
patients in the present study were relatively sensitive to
antiepileptic drugs, and any impact should have been evident.
Furthermore, empiric therapy may have also influenced the present
results, thus results of the χ2 test were not
significantly correlated with early seizures prior to meningioma
resection. Further confirmation of the effects of antiepileptic
drugs is also required as the plasma concentrations of these agents
were not determined following pre- and postoperative administration
in the study. However, it is reasonable to assume that
administration of an antiepileptic drug during the perioperative
period may significantly reduce morbidity from early postoperative
seizures.
The site of a meningioma may be a decisive factor
affecting its likelihood to induce epileptic seizures. Previous
studies (6,26) suggested that supratentorial and
cerebellar convexity meningiomas are significant causes of
seizures. Tumors in areas of the brain associated with reasoning,
emotions and motor activities are known to more easily cause
epileptic seizures, and tumors in or near the cortex are associated
with a higher incidence of seizures compared to tumors in other
locations. Pathological changes of deep tissue occur less
frequently. Regardless of patient history of preoperative seizures,
parasagittal meningiomas located in the front third of the superior
sagittal sinus are associated with a high incidence of
postoperative seizures due to their close proximity to the central
region of the brain. Penfield et al (27) reported that the incidence of seizures
caused by intracranial tumors in the supratentorial, saddle and
subtentorial areas were 50.0, 5.7 and 2.5%, respectively. These
findings may be associated with whether a balance between
excitation and inhibition is more easily destroyed in different
areas of the brain. The results of the present study support the
above findings. Compared to the subtentorial group, the ORs of the
superficial and deep supratentorial groups were 9.116 and 1.562,
respectively. Therefore, the superficial and deep supratentorial
tumor groups were at a higher risk for seizure compared to the
subtentorial group, and the superficial supratentorial group was at
the highest risk for early postoperative seizures.
In summary, a multifactorial stepwise logistic
regression analysis of 14 clinical factors that may be correlated
to early postoperative seizures in elderly patients who had
undergone resection for meningioma was performed. Following
exclusion of the interference factors, four clinical factors (tumor
diameter, administration of a postoperative prophylactic
antiepileptic drug, PTBE and tumor site) were entered into a
regression model as independent factors correlated with seizures.
Furthermore, a stepwise logistic regression equation with a
statistically significant goodness of fit test (P>0.05) was
obtained. This equation can be used to objectively predict disease
prognosis and provide guidance for postsurgical treatment, while
laying a foundation for further systematic studies.
References
|
1
|
Kuratsu J and Ushio Y: Epidemiological
study of primary intracranial tumours in elderly people. J Neurol
Neurosurg Psychiatry. 63:116–118. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Patil CG, Veeravagu A, Lad SP and Boakye
M: Craniotomy for resection of meningioma in the elderly: a
multicentre, prospective analysis from the national surgical
quality improvement program. J Neurol Neurosurg Psychiatry.
81:502–505. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Poon MT, Fung LH, Pu JK and Leung GK:
Outcome comparison between younger and older patients undergoing
intracranial meningioma resections. J Neurooncol. 114:219–227.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
González-Martínez JA and Najm IM:
Meningiomas and epilepsy meningiomas. Springer; pp. 243–246. 2009,
View Article : Google Scholar
|
|
5
|
Lieu AS and Howng SL: Intracranial
meningiomas and epilepsy: incidence, prognosis and influencing
factors. Epilepsy Res. 38:45–52. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mauro AM, Bomprezzi C, Morresi S, et al:
Prevention of early postoperative seizures in patients with primary
brain tumors: preliminary experience with oxcarbazepine. J
Neurooncol. 81:279–285. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Marosi C, Hassler M, Roessler K, et al:
Meningioma. Crit Rev Oncol Hematol. 67:153–171. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chow SY, Hsi MS, Tang LM and Fong VH:
Epilepsy and intracranial meningiomas. Zhonghua Yi Xue Za Zhi
(Taipei). 55:1511995.PubMed/NCBI
|
|
9
|
Markides KS, Black SA, Ostir GV, Angel RJ,
Guralnik JM and Lichtenstein M: Lower body function and mortality
in Mexican American elderly people. J Biol Sci Med Sci.
56:M243–M247. 2001.
|
|
10
|
Bernstein M: Brain tumour surgery in the
elderly: a brief reappraisal. Can J Surg. 39:147–150.
1996.PubMed/NCBI
|
|
11
|
Caroli M, Locatelli M, Prada F, et al:
Surgery for intracranial meningiomas in the elderly: a
clinical-radiological grading system as a predictor of outcome. J
Neurosurg. 102:290–294. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fang C, Tan Y, Cui Z, Shi Y, Wang J and Di
H: Clinical and pathological features in 49 elderly patients with
meningiomas. Neural Regen Res. 2:574–576. 2007. View Article : Google Scholar
|
|
13
|
Wofford JL, Moran WP, Wilson TA and Velez
R: Clinical presentation of meningioma in the elderly. J Am Geriatr
Soc. 41:1221993. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wyllie E, Comair YG, Kotagal P, Bulacio J,
Bingaman W and Ruggieri P: Seizure outcome after epilepsy surgery
in children and adolescents. Ann Neurol. 44:740–748. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhang B, Zhao G, Yang HF, Wang D, Yu JL
and Huang HY: Assessment of risk factors for early seizures
following surgery for meningiomas using logistic regression
analysis. J Int Med Res. 39:1728–1735. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Beaumont A and Whittle IR: The
pathogenesis of tumour associated epilepsy. Acta Neurochirurgica
(Wien). 142:1–15. 2000. View Article : Google Scholar
|
|
17
|
Shamji MF, Fric-Shamji EC and Benoit BG:
Brain tumors and epilepsy: pathophysiology of peritumoral changes.
Neurosurg Rev. 32:275–284. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
van Breemen MS, Wilms EB and Vecht CJ:
Epilepsy in patients with brain tumours: epidemiology, mechanisms
and management. Lancet Neurol. 6:421–430. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kawaguchi T, Kameyama S and Tanaka R:
Peritumoral edema and seizure in patients with cerebral convexity
and parasagittal meningiomas. Neurol Med Chir (Tokyo). 36:568–574.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
De Santis A, Villani R, Sinisi M,
Stocchetti N and Perucca E: Add-on phenytoin fails to prevent early
seizures after surgery for supratentorial brain tumors: a
randomized controlled study. Epilepsia. 43:175–182. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Lee ST, Lui TN, Chang CN, et al:
Prophylactic anticonvulsants for prevention of immediate and early
postcraniotomy seizures. Surg Neurol. 31:361–364. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zachenhofer I, Donat M, Oberndorfer S and
Roessler K: Perioperative levetiracetam for prevention of seizures
in supratentorial brain tumor surgery. J Neurooncol. 101:101–106.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Foy PM, Chadwick DW, Rajgopalan N, Johnson
AL and Shaw MD: Do prophylactic anticonvulsant drugs alter the
pattern of seizures after craniotomy? J Neurol Neurosurg
Psychiatry. 55:753–757. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Franceschetti S, Binelli S, Casazza M, et
al: Influence of surgery and antiepileptic drugs on seizures
symptomatic of cerebral tumours. Acta Neurochir (Wien). 103:47–51.
1990. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Temkin NR: Antiepileptogenesis and seizure
prevention trials with antiepileptic drugs: meta. analysis of
controlled trials. Epilepsia. 42:515–524. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
O'Connell J: Parasagittal and falx
meningiomas. Proc Royal Soc Med. 64:5841971.
|
|
27
|
Penfield W, Erickson T and Tarlov I:
Relation of intracranial tumors and symptomatic epilepsy. Arch
Neurol Psychiatry. 44:3001940. View Article : Google Scholar
|