Introduction
Computer tomography (CT)-guided automated cutting
needle biopsy (ACNB) is a minimally invasive technique, which is an
accepted and widely used tool in the diagnosis of pulmonary lesions
(1–3).
Although considered to be a safe technique, several complications
have been associated with the procedure, including the occurrence
of pneumothorax, hemorrhaging, air embolism and tumor seeding
(4–6).
In the present study, a very rare case of non-traumatic acute
paraplegia resulting from an ACNB in a patient with silicosis is
reported. Although the symptoms of the patient in the present case
study were substantially relieved following aggressive treatment,
the patient still presented with a poor neurological recovery and
permanent deficit. To the best of our knowledge, no previous case
report has described paraplegia due to CT-guided ACNB of the
lungs.
Case report
A 45-year-old man was admitted to the Zhongnan
Hospital of Wuhan University with a history of productive coughing,
which had lasted for a duration of 1 year. Multiple nodules and
masses were revealed on performing chest radiography and CT. In
order to make a pathological diagnosis, a CT-guided biopsy using an
automatic cutting needle (18-gauge; Bard® Maxcore®, Bard Biopsy
Systems, Tempe, AZ, USA) was required. The largest accessible lung
mass was selected to be the targeted area for biopsy, also
considering the needle puncture pathway and the direction of the
targeted mass. The transthoracic distance to the lung mass was
selected to be the shortest, without any evident emphysematous
changes or bulla in the pathway of the needle entrance.
Subsequently, the patient was placed into the prone position.
Limited CT (Somatom Sensation 16; Siemens Healthcare, Erlangen,
Germany) scanning was performed to localize the lesion and to
document the needle progression to the depth of the target. The
puncture point on the skin was labeled. The distance between the
targeted mass and the pleura was 20 mm, and the distance between
the puncture point and the spine tube was 70 mm (Fig. 1). Subsequently, the biopsy was
performed under aseptic conditions and local anesthesia. A total of
three tissue samples were obtained. The tumor tissues were immersed
in 10% formalin, and processed for conventional pathological
examination. Immediately following the procedure, the patient
coughed up approximately one tablespoon's volume of bloody sputa. A
CT scan was performed again to assess the complications of the
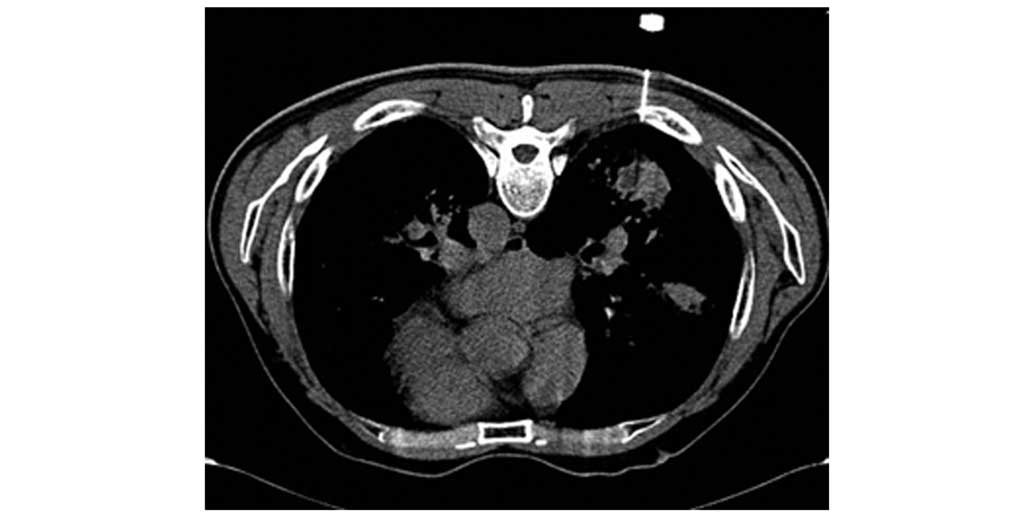
biopsy. No pneumothorax or bleeding was identified (Fig. 2). The patient exited the CT room by
himself. However, 10 min later, the patient suddenly felt weakness
in his lower limbs and fell to the ground with clear consciousness.
The patient was immediately sent to the emergency department close
to the CT room. Supplemental 100% oxygen was administered, and
general symptomatic support was provided. A neurological
examination revealed a flaccid paraplegia. Hyperesthesia at the
level below the T8 dermatome was observed. The anal reflex was
absent, and the patient experienced urinary and fecal incontinence.
Subsequent spine magnetic resonance imaging (MRI) demonstrated no
abnormal findings in the spinal cord (Fig. 3). An MRI was performed on the
subsequent day, which revealed swelling of the thoracic spinal
cord; in addition, a high-signal-intensity lesion at the level of
T7, T8 and T9 was identified in T2-weighted images (Fig. 4). The patient subsequently received
hyperbaric oxygen therapy for a few days, and rehabilitative
treatment over a period of a few weeks. The patient made a gradual
recovery over 4 months. At 6 months following the biopsy, the
patient remained unable to walk, although the patient could stand
for 10 min and defecate independently. At present, the patient
remains active in daily life, in spite of confinement to a
wheelchair.
Discussion
The present case report highlights that patients
undergoing CT-guided ACNB are susceptible to spinal cord ischemia,
which, to the best of our knowledge, has not been previously
reported. The mechanism underlying spinal cord ischemia remains to
be fully elucidated, although it is considered to be
multifactorial, involving air embolism. A plausible hypothesis is
that concurrent coughing during the procedure is able to displace
the biopsy needle into the large vessel adjacent to the pulmonary
lesion, and continuous high intrathoracic pressure may have pushed
a large quantity of air into the pulmonary vein, leading to
systemic air embolism.
CT-guided lung biopsy is a frequently performed
procedure, and is important in the evaluation of solitary and
multiple pulmonary nodules. Minor complications commonly (30–60%)
associated with the procedure include pneumothorax of low abundance
(17–60%) and alveolar bleeding (5–30%) (7). In general, these complications are
asymptomatic, and regress spontaneously. Serious complications
requiring a specific treatment, including drained pneumothorax,
hemopericardium, hemothorax, hemoptysis, intense pain and air
embolism (1–8), rarely occur. Air embolism is the most
severe complication, although it is among those that occur the
least frequently. In a study of 9,783 biopsies, air embolism
occurred in six patients, resulting in an incidence rate of 0.06%
(1), which also revealed no major
difference from the previously reported complication rate.
The present case study has been reported to raise
the awareness of the possibility of such a complication arising in
CT-guided ACNB of the lungs. Although very rare in occurrence,
however, this kind of complication may occur in a patient with
interstitial lung disease and emphysema (9), such as in the present case. Although air
embolism occurs only very rarely as a complication of percutaneous
needle biopsy, physicians should be aware of its occurrence and
significance. Air embolism may lead to myocardial infarction,
arrhythmia, stroke and mortality. The operators must check their
practice, and calculate the risk of complications. The risks should
be clearly explained to the patients in order that they may give
their informed consent prior to the procedure. Once an air embolism
is suspected, the patient should be placed into either the left
lateral decubitus or the Trendelenberg position to prevent residual
air in the left atrium from entering the cerebral circulation.
Supplemental 100% oxygen should be administered, and general
symptomatic support should be provided (10).
References
|
1
|
Tomiyama N, Yasuhara Y, Nakajima Y, Adachi
S, Arai Y, Kusumoto M, Eguchi K, Kuriyama K, Sakai F, Noguchi M, et
al: CT-guided needle biopsy of lung lesions: A survey of severe
complication based on 9783 biopsies in Japan. Eur J Radiol.
59:60–64. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Khan MF, Straub R, Moghaddam SR, Maataoui
A, Gurung J, Wagner TO, Ackermann H, Thalhammer A, Vogl TJ and
Jacobi V: Variables affecting the risk of pneumothorax and
intrapulmonal hemorrhage in CT-guided transthoracic biopsy. Eur
Radiol. 18:1356–1363. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wu CC, Maher MM and Shepard JA:
Complications of CT-guided percutaneous needle biopsy of the chest,
Prevention and management. AJR Am J Roentgenol. 196:W678–W682.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Nour-Eldin NE, Alsubhi M, Naguib NN,
Lehnert T, Emam A, Beeres M, Bodelle B, Koitka K, Vogl TJ and
Jacobi V: Risk factor analysis of pulmonary hemorrhage complicating
CT-guided lung biopsy in coaxial and non-coaxial core biopsy
techniques in 650 patients. Eur J Radiol. 83:1945–1952. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhuang YP, Wang HY, Zhang J, Feng Y and
Zhang L: Diagnostic accuracy and safety of CT-guided fine needle
aspiration biopsy in cavitary pulmonary lesions. Eur J Radiol.
82:182–186. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
O'Neill AC, McCarthy C, Ridge CA, Mitchell
P, Hanrahan E, Butler M, Keane MP and Dodd JD: Rapid needle-out
patient-rollover time after percutaneous CT-guided transtho-racic
biopsy of lung nodules, Effect on pneumothorax rate. Radiology.
262:314–319. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Prosch H, Stadler A, Schilling M, Bürklin
S, Eisenhuber E, Schober E and Mostbeck G: CT fluoroscopy-guided
vs. multislice CT biopsy mode-guided lung biopsies, Accuracy,
complications and radiation dose. Eur J Radiol. 81:1029–1033. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Cheung YC, Chang JW, Hsieh JJ, Lin G and
Tsai YH: Adequacy and complications of computed tomography-guided
core needle biopsy on non-small cell lung cancers for epidermal
growth factor receptor mutations demonstration. 18-gauge or
20-gauge biopsy needle. Lung Cancer. 67:166–169. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Heyer CM, Reichelt S, Peters SA, Walther
JW, Müller KM and Nicolas V: Computed tomography-navigated
transthoracic core biopsy of pulmonary lesions, Which factors
affect diagnostic yield and complication rates? Acad Radio.
15:1017–1026. 2008. View Article : Google Scholar
|
|
10
|
Klein JS and Zarka MA: Transthoracic
needle biopsy. Radiol Clin North Am. 38:235–266. 2000. View Article : Google Scholar : PubMed/NCBI
|