Introduction
Pulmonary sulcus tumors are a rare type of in lung
cancer (1). As the disease is often
unresectable, adequate palliative management is crucial. Concurrent
chemoradiotherapy for locally advanced non-small-cell lung cancer
(NSCLC) patients with a good overall condition has long been a
matter for discussion (2). However,
to the best of our knowledge, palliative therapy for patients with
such tumors who are in a poor overall condition has not been
reported to date. In order to increase the awareness of the
approach to palliative care of locally advanced NSCLC patients with
poor performance status (PS), we herein present the case of a
patient with symptomatic sulcus NSCLC, who was treated with
sequential chemoradiotherapy in the palliative setting.
Case report
A 54-year-old woman was referred to the Mito Medical
Center (Mito, Japan) due to complaints suspicious for lung cancer.
The patient presented with paralysis in the right upper extremity
and severe pain, which required oxycodone administration at 60 mg
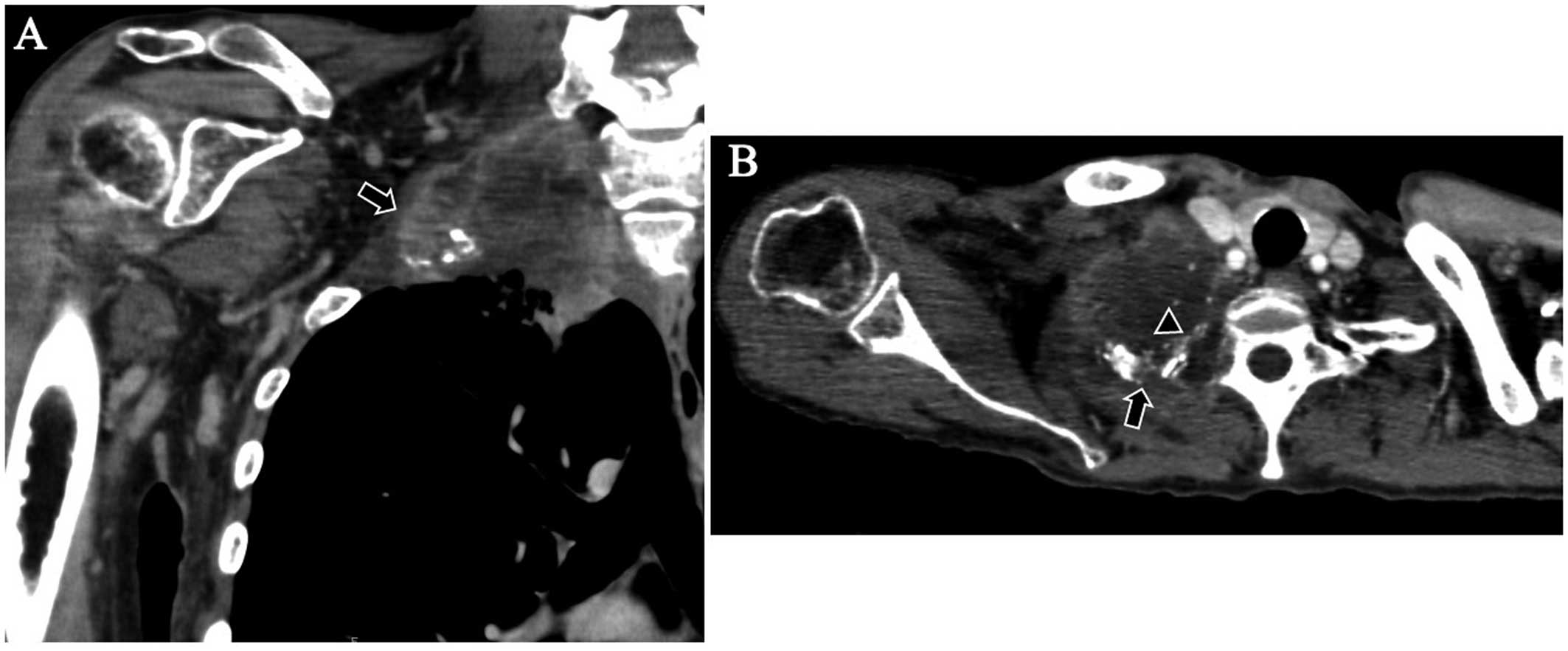
per day. A computed tomography (CT) scan revealed a pulmonary
sulcus tumor in the right lung, with direct invasion of the
brachial neural plexus and the thoracic spinal canal, with erosive
changes in the thoracic spine and ribs (Fig. 1). The CT scan also showed enlarged
ipsilateral mediastinal lymph nodes, an ipsilateral pleural fluid
collection, and an enlarged right adrenal gland. Transbronchial
biopsy specimens, which were obtained from the tumor through
fiberoptic bronchoscopy, revealed lung adenocarcinoma. Genetic
analysis of the tumor did not show epidermal growth factor receptor
or anaplastic lymphoma kinase mutations. On pretreatment
evaluation, the tumor was classified as cT4N2M1b lung
adenocarcinoma. The patient had a poor PS (PS 3), poor nutritional
status (serum albumin: 3.9 mg/dl), and presented with excessive
weight loss (body weight, 38.8 kg). At first, supportive care was
recommended due to the patient's poor clinical condition. However,
the patient insisted on multidisciplinary therapy. Therefore,
sequential chemoradiotherapy with a palliative intent was selected.
The patient received palliative irradiation for the primary lesion
(45 Gy in 4.5 weeks), without severe adverse events (AEs) or
deterioration of her clinical condition. Two weeks after the
palliative irradiation, taking the patient's clinical condition
into consideration, palliative chemotherapy with 6 courses of
pemetrexed (500 mg/m2 on day 1, q28) was performed. The
treatment was successful and uncomplicated. Although the paralysis
in right arm did not improve, the pain was effectively controlled
without increasing the morphine dose. There was no local recurrence
until the time of death from cancer progression, 8 months after the
initiation of therapy.
Discussion
Concurrent chemoradiotherapy is currently considered
as the standard therapy for locally advanced NSCLC (3–5) but, due
to the severe associated AEs, it is only indicated for NSCLC
patients in a good overall condition (3–5).
However, studies considering palliative sequential
chemoradiotherapy for locally advanced NSCLC have not been reported
to date. For patients with metastatic disease, chemotherapy and
supportive care are currently considered the standard of care.
Palliative radiotherapy for pain control may be effective in some
patients. Although only in a limited number of cases, a palliative
benefit with thoracic radiotherapy in patients with stage IV NSCLC
who have a good PS has rarely been reported (6,7), but
chemoradiotherapy for stage IV NSCLC patients has never been shown
to provide a survival benefit. As regards chemotherapy for stage IV
NSCLC patients with a poor PS, single-agent treatment with
docetaxel or pemetrexed may be considered (8). To the best of our knowledge, there have
been no reported cases with palliative chemoradiothrapy for stage
IV NSCLC patients with a poor PS. Due to the short life expectancy
of patients on palliative care, whenever possible,
chemoradiotherapy should be non-distressing, effective and
short-course. Irradiation may cause dermatitis and/or esophagitis,
and chemotherapy may be associated with general fatigue, appetite
loss and myelosuppression, whereas hospitalization during the
treatment period severely compromises the patient's quality of
life.
In addition, the cornerstone of the management for
NSCLC with a specific genetic etiology, such as epidermal growth
factor receptor mutations, is molecular-targeted therapy (9–11);
however, no such specific genetic etiology was identified in the
present case. In our patient, standard chemoradiotherapy, either
concurrent or sequential, was not indicated, as she had metastatic
disease and a poor PS, but the patient requested multidisciplinary
treatment. However, any standard concurrent chemoradiotherapy was
considered to be intolerable due to her poor condition, as
chemotherapy-induced AEs would increase the patient's discomfort.
Therefore, palliative sequential chemoradiotherapy was selected and
radiotherapy alone was first delivered. As severe AEs did not
develop, additional chemotherapy with pemetrexed alone was planned.
Pemetrexed was selected as the chemotherapeutic agent, as it is
associated with fewer hematological and non-hematological AEs
(8); if any severe AEs had developed
with this agent, another course of the chemotherapy would not have
been indicated.
The patient selection criteria for palliative
sequential chemoradiotherapy have not been specifically outlined
and must be considered on a case-by-case basis. When considering
palliative outcomes in general, poor PS, poor nutritional status
and excessive weight loss are associated with a poor outcome.
Although chemoradiotherapy is not generally considered in
metastatic NSCLC, local control and a survival benefit may be
achieved in selected patients. Palliative sequential
chemoradiotherapy for pulmonary sulcus NSCLC may be considered as
an option, and this treatment would be considered in selected
patients. Either chemotherapy or radiotherapy should be
administered first and, if there is no apparent deterioration of
the patient's general condition, the next treatment modality should
be administered.
References
|
1
|
Glassman LR and Hyman K: Pancoast tumor: A
modern perspective on an old problem. Curr Opin Pulm Med.
19:340–343. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Peedell C, Dunning J and Bapusamy A: Is
there a standard of care for the radical management of non-small
cell lung cancer involving the apical chest wall (Pancoast
tumours)? Clin Oncol (R Coll Radiol). 22:334–346. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Laine AM, Westover KD and Choy H:
Radiation therapy as a backbone of treatment of locally advanced
non-small cell lung cancer. Semin Oncol. 41:57–68. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Antoni D and Mornex F: Chemoradiotherapy
of locally advanced nonsmall cell lung cancer: State of the art and
perspectives. Curr Opin Oncol. 28:104–109. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Xu P and Le Pechoux C: Chemoradiotherapy
for stage III non-small cell lung cancer: Have we reached the
limit? Chin Clin Oncol. 4:452015.PubMed/NCBI
|
|
6
|
Topkan E, Yildirim BA, Guler OC, Parlak C,
Pehlivan B and Selek U: Safety and palliative efficacy of
single-dose 8-Gy reirradiation for painful local failure in
patients with stage IV non-small cell lung cancer previously
treated with radical chemoradiation therapy. Int J Radiat Oncol
Biol Phys. 91:774–780. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dandekar VK, Young J, Kiel K, Bonomi P,
Fidler MJ, Batus M and Sher DJ: Efficacy and tolerability of
palliative split-course thoracic chemoradiotherapy for symptomatic
Non-small cell lung cancer. Am J Clin Oncol. 38:605–609. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sculier JP and Moro-Sibilot D: First- and
second-line therapy for advanced nonsmall cell lung cancer. Eur
Respir J. 33:915–930. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bareschino MA, Schettino C, Rossi A,
Maione P, Sacco PC, Zeppa R and Gridelli C: Treatment of advanced
non small cell lung cancer. J Thorac Dis. 3:122–133.
2011.PubMed/NCBI
|
|
10
|
Thomas A, Liu SV, Subramaniam DS and
Giaccone G: Refining the treatment of NSCLC according to
histological and molecular subtypes. Nat Rev Clin Oncol.
12:511–526. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gerber DE, Gandhi L and Costa DB:
Management and future directions in non-small cell lung cancer with
known activating mutations. Am Soc Clin Oncol Educ Book. e353–e365.
2014. View Article : Google Scholar : PubMed/NCBI
|