Introduction
Lung cancer is one of the most common types of
cancer worldwide, it is highly aggressive and has a high rate of
distant metastasis (1). Subcutaneous
metastasis from lung cancer has been well described (2); however, reports of subcutaneous
metastasis of lung cancer after three surgeries for recurrent brain
metastasis are scarce. We herein report a rare case of subcutaneous
metastasis from pulmonary adenocarcinoma and provide a brief review
of the relevant literature.
Case report
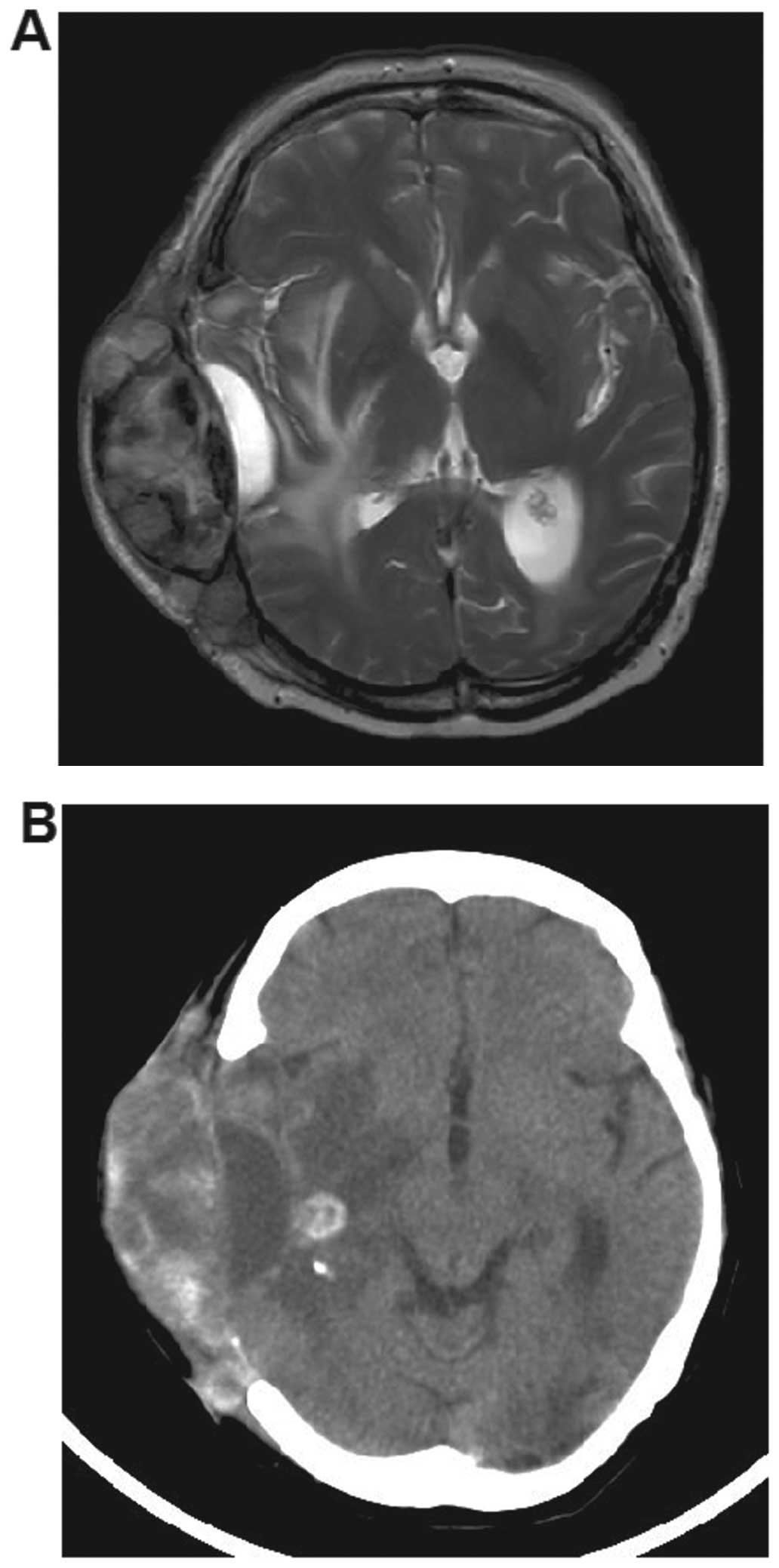
A 49-year-old female patient was admitted to our
hospital due to a fast-growing mass in the left temporal scalp at a
craniotomy site (Fig. 1). The mass
was round and adhered firmly to the scalp tissues. The patient was
aware of the swelling as it caused her pain. A routine magnetic
resonance imaging (MRI) revealed recurrent lesions in the left
temporal and parietal lobes and a separate large nodular mass in
the subcutaneous tissue coinciding with the site of the previous
craniotomy (Fig. 2). In 2011, a lung
computed tomography (CT) scan at another hospital revealed a 2.4-cm
mass in the upper lobe of the left lung. Fine-needle aspiration
cytology revealed pulmonary adenocarcinoma. The patient did not
undergo surgery due to enlarged mediastinal lymph nodes, but was
treated with radiosurgery (5 years) and chemotherapy (2 years). The
subsequent CT scan demonstrated no residual or recurrent
adenocarcinoma in the lung.
In March, 2013, a routine MRI scan at another
hospital revealed brain metastases in the left temporal and
parietal lobes. The patient underwent subtotal resection of the
tumors and decompressive craniectomy at the First Hospital of Jilin
University (Changchun, China). In May, 2014 and August, 2015 the
patient suffered recurrent brain metastases in the left temporal
lobe, which were resected. The pathological diagnosis was
adenocarcinoma.
In November, 2015, the patient was admitted to our
hospital due to a fast-growing mass in the left temporal scalp at
the craniotomy site.
The patient's medical history was unremarkable,
apart from her father having been a heavy smoker for 30 years. The
physical and neurological examinations were normal. There were no
other metastases. The laboratory test results for tumor markers
were as follows: Carcinoembryonic antigen, 191.6 ng/ml (normal,
<3.4 ng/ml) and carbohydrate antigen 15–3, 38.03 U/ml (normal,
<25.0 U/ml). Peripheral blood cell counts, liver and renal
function tests and hormonal levels were within the normal
range.
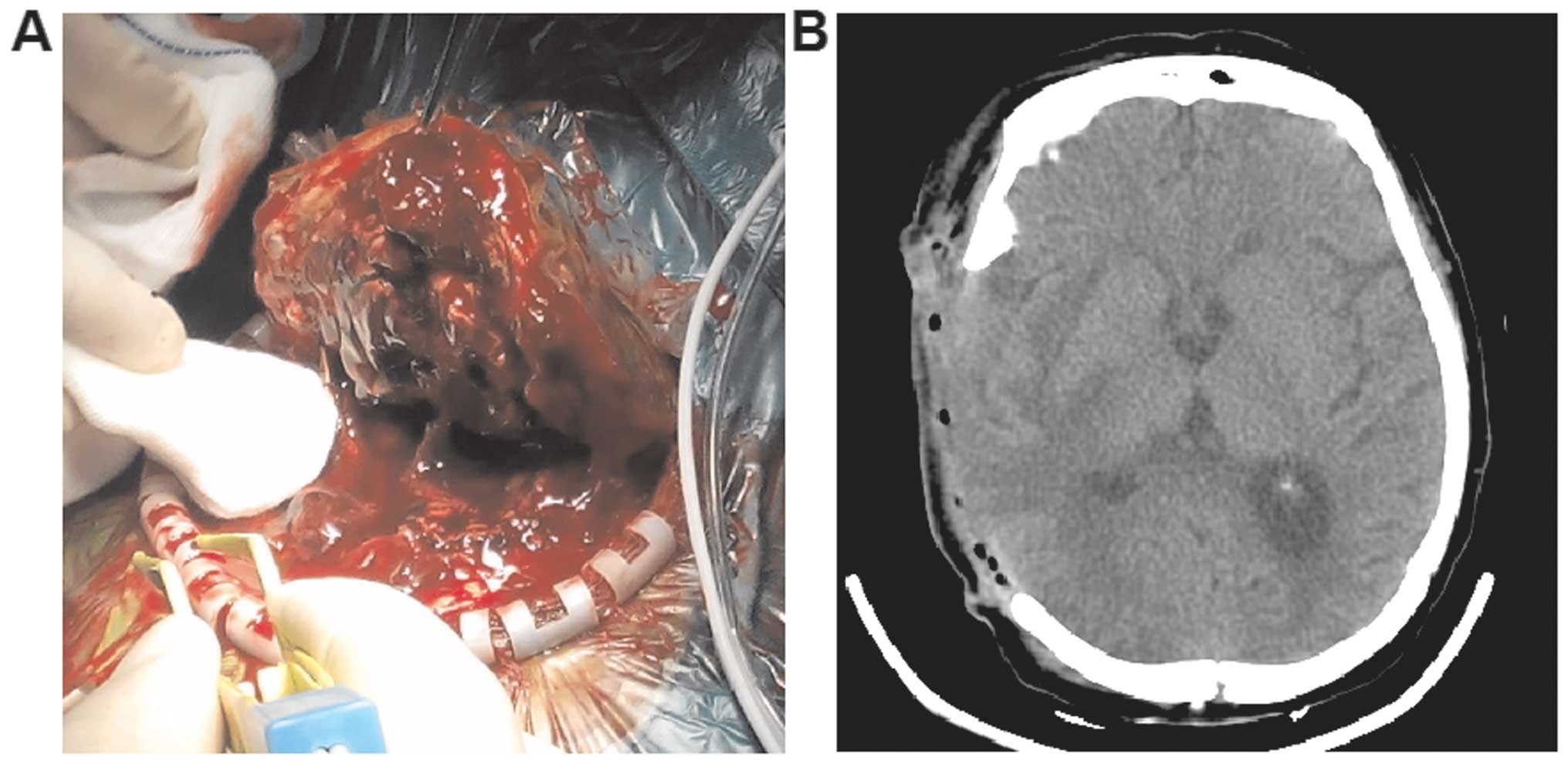
As the location of the mass corresponded to the site
of the craniotomy, seeding was considered. Surgical resection of
the subcutaneous nodule was performed. During surgery, the mass was
found to be infiltrating the subcutaneous tissue and dura mater.
There was no distinct boundary between the tumor and normal skin.
The nodule contained numerous vessels (Fig. 3A). Total excision of the lesions in
the left temporal and parietal lobes and the mass in the
subcutaneous tissue was performed (Fig.
3B).
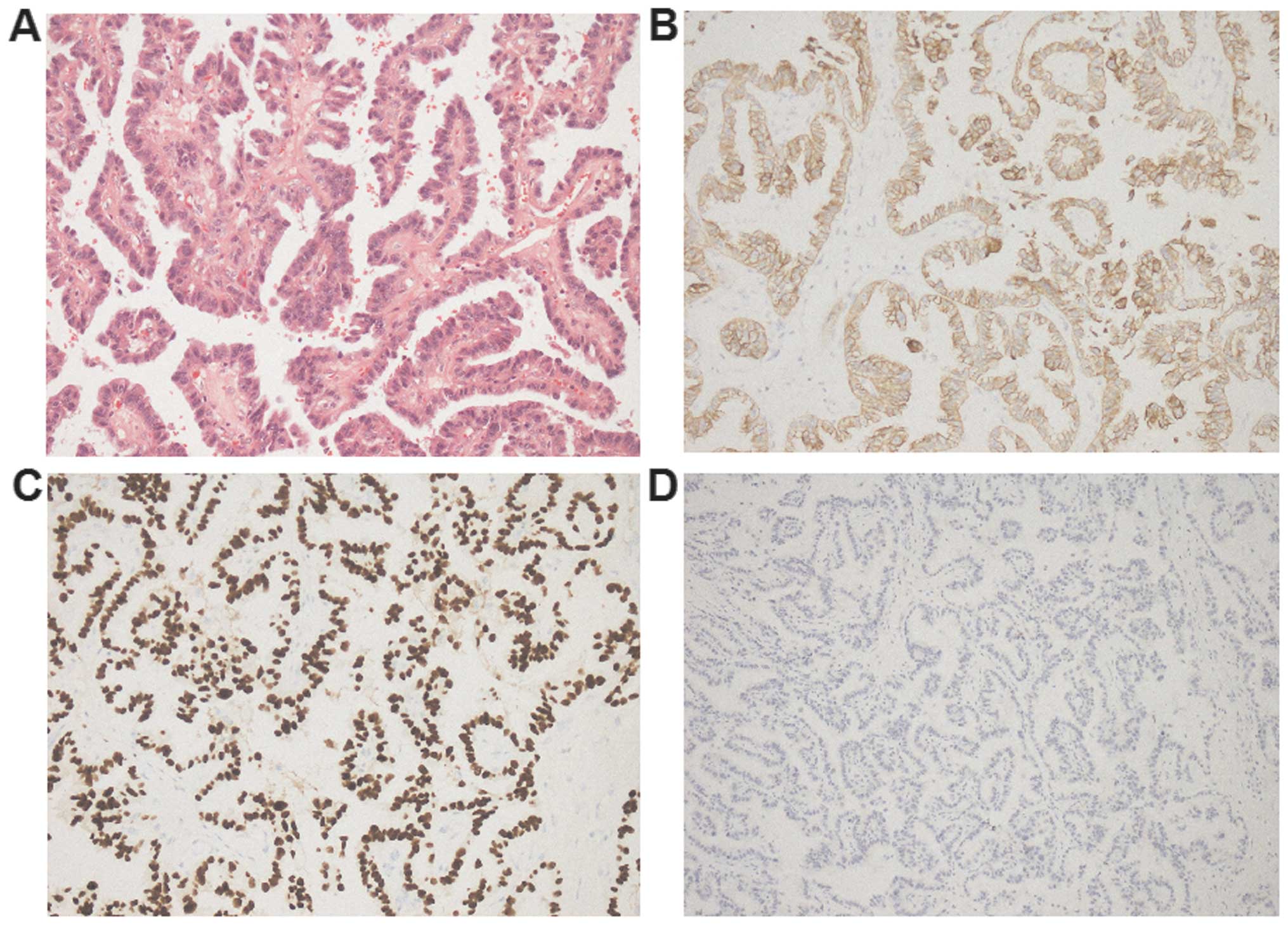
On immunohistochemistry (Fig. 4), the masses diffusely expressed
thyroid transcription factor-1 (TTF-1) and cytokeratin (CK)7, the
Ki-67 index was 25%, whereas villin, CK20 and Wilms tumor-1 were
negative. The patient continued her treatment and was followed up
at another hospital.
Discussion
Cutaneous metastasis is caused by primary
cancer-derived cells that grow in the skin (3). According to the published literature,
the overall incidence of cutaneous metastasis is 2.9–5.3% (4), and 1–12% in lung cancer (2,5–8). Cutaneous metastasis usually presents as
solitary or multiple nodules sized 5 mm-10 cm that are firm,
immobile and covered with normal skin. In the present case, the
nodule was firm, relatively immobile, and of normal yellow
color.
In the present case, the differential diagnosis was
primary skin malignancy. When the primary tumor is an
adenocarcinoma, other diagnoses such as melanoma and hematopoietic
malignancies should be considered (9). The patient in the present study had
undergone multiple surgeries with subsequent complications
associated with the surgical wounds, which may have contributed to
the scalp metastasis. Therefore, the initial diagnosis was
subcutaneous metastasis of lung cancer. Certain cases of
subcutaneous metastasis of lung cancer may manifest as purple or
bright red masses that are ulcerated or cauliflower-like,
accompanied by bleeding (3,10). The patient in the present case did
not experience bleeding, as the mass was discovered early.
The scalp accounts for 4–6.9% of all cutaneous
metastases and it is a relatively frequent metastatic site,
possibly due to the abundant blood supply and immobility (4). Skin metastases from internal
malignancies tend to occur at a site near the primary tumor
(11,12) through various routes, including
lymphatic spread, hematogenous spread and direct implanting. The
patient underwent three surgeries for brain metastasis and the mass
was located at the surgical site. Therefore, the mass was
considered to be an implantation metastasis from the previous brain
metastases.
The treatment options for scalp metastasis include
surgery, chemotherapy and radiotherapy. Our patient reported
swelling and pain; therefore, she underwent surgical resection in
an attempt to provide local palliation (13). During surgery, the mass was found to
be infiltrating the subcutaneous tissue and dura mater. Surgical
seeding of tumor cells is a known complication of lung cancer
surgery (14). We considered that
subcutaneous spreading of the intracranial tumor may have occurred,
rather than metastasis from the lung. The localization of a
metastasis along a surgical incision site indicates tumor seeding
as the likely mechanism, particularly when a metastasis is apparent
on imaging soon after surgery, as in this case. We consider that
scalp metastases due to intraoperative seeding may occur in all
histopathological grades of lung cancer.
The patient in the present case was at high risk for
extracranial spreading of intracranial tumors, as she had undergone
multiple surgeries. Surgical bone defects may compromise the
natural barriers to dissemination of intracranial tumors, providing
access to the lymphatic system, blood vessels and connective
tissues. Vascular invasion of the extracranial tissues, migration
of neoplastic cells and further growth may potentiate extracranial
metastases. However, differentiation between implantation of tumor
cells and metastasis from the lung may be difficult. Prevention of
extracranial spreading of intracranial tumors following resection
may be achieved by appropriate closure of the dura mater, changing
surgical instruments and gloves for wound closure after the
intracranial phase of the surgery, and copious saline irrigation of
the wound prior to closure.
In our patient, diagnosis was made by
histopathological examination of the cutaneous nodule following
surgical excision. Histological study of the nodule revealed
adenocarcinoma. The histology of cutaneous metastasis from lung
cancer most commonly reveals adenocarcinoma, followed by
squamous/small-cell carcinoma, and large-cell carcinoma (8). Immunohistochemistry, particularly
CK7⁄CK20 (15) and TTF-1 is useful
for identification of adenocarcinoma. In the present case,
immunohistochemistry for CK7/CK20 was CK7-positive and for
CK20-negative. TTF-1, a tissue-specific transcription factor
expressed in epithelial cells of the thyroid gland and lung
(16), confirmed that the primary
origin of the adenocarcinoma was the lung.
Following three surgeries for brain metastases and
one surgery for cutaneous metastasis, the patient recovered well
and was able to care for herself. The presence of cutaneous
metastases in lung cancer is associated with a poor prognosis, as
this is an indication that the primary cancer is advanced. The
median survival is ~4 months. The patient in the present case was
followed up for >4 months and continues to show good
recovery.
The present study was approved by the Ethics
Committee of the First Hospital of Jilin University. Informed
patient consent was obtained regarding the publication of the case
details and accompanying images.
Acknowledgements
The present study has been edited and proofread by
Medjaden Bioscience Limited.
Glossary
Abbreviations
Abbreviations:
|
MRI
|
magnetic resonance imaging
|
|
CT
|
computed tomography
|
|
TTF-1
|
thyroid transcription factor-1
|
|
CK
|
cytokeratin
|
References
|
1
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Salemis NS, Veloudis G, Spiliopoulos K,
Nakos G, Vrizidis N and Gourgiotis S: Scalp metastasis as the first
sign of small-cell lung cancer: Management and literature review.
Int Surg. 99:325–329. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Riahi RR and Cohen PR: Clinical
manifestations of cutaneous metastases: A review with special
emphasis on cutaneous metastases mimicking keratoacanthoma. Am J
Clin Dermatol. 13:103–112. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Krathen RA, Orengo IF and Rosen T:
Cutaneous metastasis: A meta-analysis of data. South Med J.
96:164–167. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
McGrath RB, Flood SP and Casey R:
Cutaneous metastases in non-small cell lung cancer. BMJ Case Rep.
2014:2014.http://dx.doi.org/10.1136/bcr-2014-205752PubMed/NCBI
|
|
6
|
Perisano C, Spinelli MS, Graci C,
Scaramuzzo L, Marzetti E, Barone C, Fabbriciani C and Maccauro G:
Soft tissue metastases in lung cancer: A review of the literature.
Eur Rev Med Pharmacol Sci. 16:1908–1914. 2012.PubMed/NCBI
|
|
7
|
Kamble R, Kumar L, Kochupillai V, Sharma
A, Sandhoo MS and Mohanti BK: Cutaneous metastases of lung cancer.
Postgrad Med J. 71:741–743. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Song Z, Lin B, Shao L and Zhang Y:
Cutaneous metastasis as a initial presentation in advanced
non-small cell lung cancer and its poor survival prognosis. J
Cancer Res Clin Oncol. 138:1613–1617. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Spitz DJ, Reddy V, Selvaggi SM, Kluskens
L, Green L and Gattuso P: Fine-needle aspiration of scalp lesions.
Diagn Cytopathol. 23:35–38. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Vadnal K Triller, Triller N, Pozek I,
Kecelj P and Kosnik M: Skin metastases of lung cancer. Acta
Dermatovenerol Alp Pannonica Adriat. 17:125–128. 2008.PubMed/NCBI
|
|
11
|
Lookingbill DP, Spangler N and Helm KF:
Cutaneous metastases in patients with metastatic carcinoma: A
retrospective study of 4020 patients. J Am Acad Dermatol.
29:228–236. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Mollet TW, Garcia CA and Koester G: Skin
metastases from lung cancer. Dermatol Online J. 15:12009.PubMed/NCBI
|
|
13
|
Saeed S, Keehn CA and Morgan MB: Cutaneous
metastasis: A clinical, pathological, and immunohistochemical
appraisal. J Cutan Pathol. 31:419–430. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Scotti V, Di Cataldo V, Falchini M,
Meattini I, Livi L, Ugolini D, Comin CE, Mazza E, Franzese C and
Biti G: Isolated chest wall implantation of non-small cell lung
cancer after fine-needle aspiration: A case report and review of
the literature. Tumori. 98:126e–129e. 2012.PubMed/NCBI
|
|
15
|
Rubin BP, Skarin AT, Pisick E, Rizk M and
Salgia R: Use of cytokeratins 7 and 20 in determining the origin of
metastatic carcinoma of unknown primary, with special emphasis on
lung cancer. Eur J Cancer Prev. 10:77–82. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Azoulay S, Adem C, Pelletier FL, Barete S,
Francès C and Capron F: Skin metastases from unknown origin: Role
of immunohistochemistry in the evaluation of cutaneous metastases
of carcinoma of unknown origin. J Cutan Pathol. 32:561–566. 2005.
View Article : Google Scholar : PubMed/NCBI
|