Introduction
In recent years, laparoscopic surgery has been
widely performed for colorectal cancer (CRC) in a number of
institutions. It has been reported that the efficacy of
laparoscopic surgery is due to the reduced blood loss, shorter
hospital stay, decreased postoperative pain, earlier postoperative
recovery and improved quality of life, with oncological outcomes
comparable to those with open surgery (1–3).
Conventional multiport laparoscopic surgery for CRC is mainly
performed using five trocars, namely one for the laparoscopist, two
for the operator and two for the assistant. Recently, efforts have
been made to reduce the number of trocars and perform a shorter
skin incision, in order to reduce wound pain and provide a better
cosmetic outcome; therefore, single-incision laparoscopic surgery
(SILS) and reduced-port surgery (RPS) have been applied in
colectomies (3–7). In SILS and RPS, an umbilical incision is
used for multi-trocar access, to remove the specimen and perform
the anastomosis; thus, the length of the umbilical skin incision
depends on these procedures. A shorter umbilical skin incision may
reduce postoperative pain and provide a better cosmetic outcome. A
Z-shaped skin incision has been used in orthopedics and plastic
surgery (8). The Z-shaped skin
incision is used for the relaxation of scar contractures and it may
provide an incision that is longer compared with a straight line
(9). We attempted to perform a
shorter umbilical incision using this method and we herein report
the usefulness of the Z skin incision in RPS for CRC.
Patients and methods
Patients
A total of 33 patients underwent RPS for CRC at the
Osaka Medical Center for Cancer and Cardiovascular Diseases (Osaka,
Japan) between July, 2013 and May, 2014. From December, 2013
onwards, we determined that the best method for achieving a shorter
umbilical incision was using the Z method. We separated patients
into two groups, namely the conventional skin incision group (July,
2013-November, 2013) and the Z skin incision group (December,
2013-May, 2014). A total of 4 patients who had received different
types of incisions in November and December, 2013 were excluded. In
total, 15 patients underwent RPS with the conventional incision
(conventional incision group) and 14 with the Z incision (Z
incision group). In all cases, the umbilical incision was used for
the first access to the abdominal cavity and as the main port with
multiple trocars.
This study was approved by our Institutional Review
Board and written informed consent regarding these surgical
procedures were obtained from all the participants according to the
ethical guidelines of the Osaka Medical Center for Cancer and
Cardiovascular Diseases.
Procedure
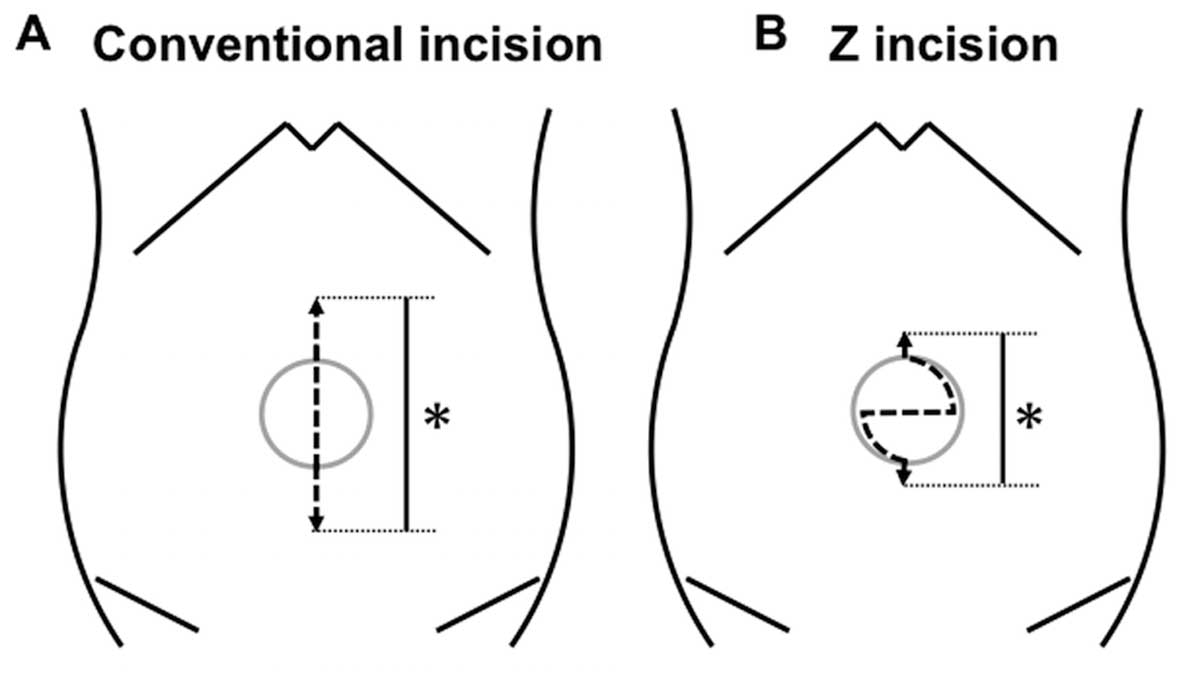
The Z or midline skin incision was marked in the
umbilical region with a sharp knife and the subcutaneous tissue was
incised (Fig. 1). A Lap Protector
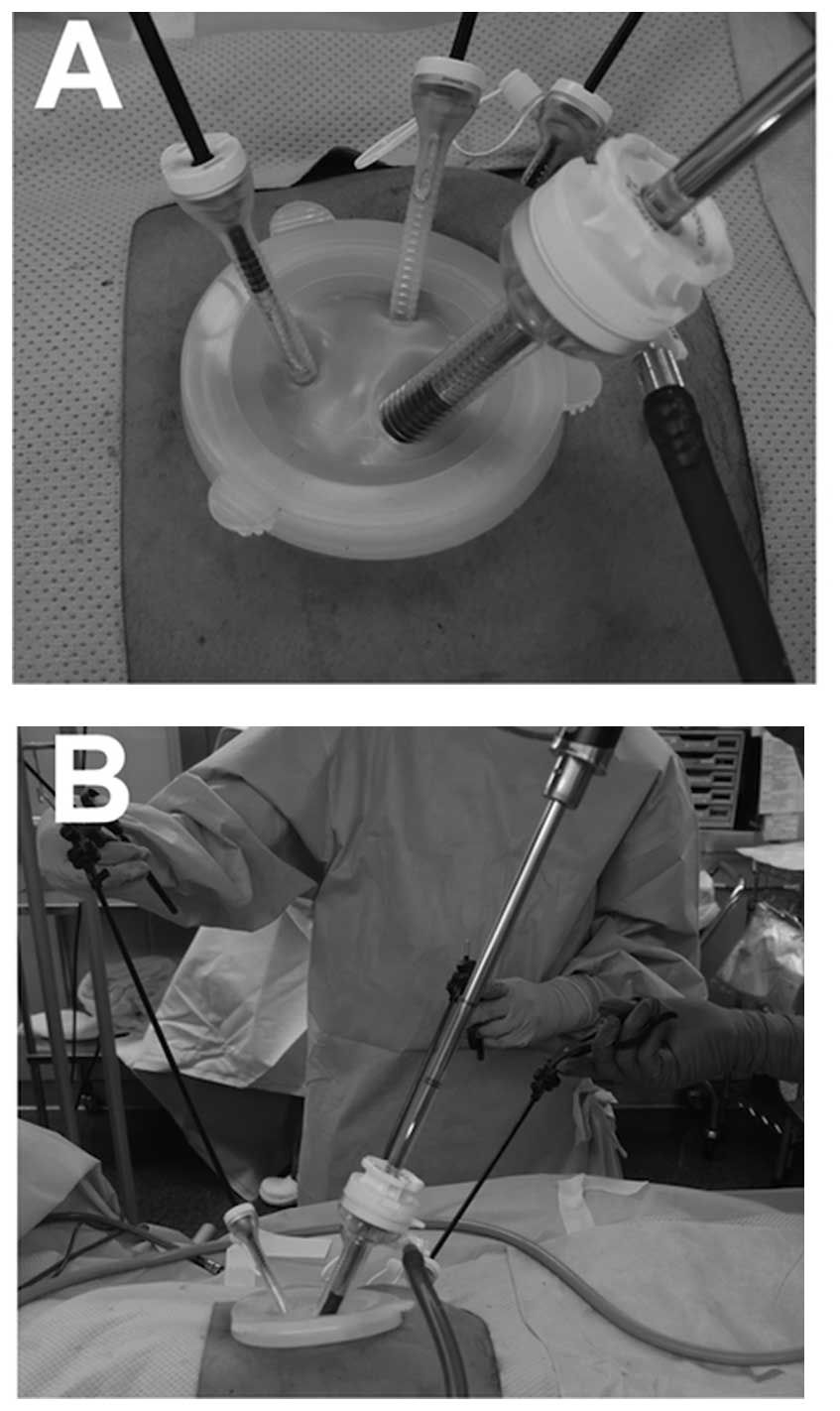
(Hakko Co., Ltd., Nagano, Japan) was folded and the bottom half was
inserted into the abdomen through the umbilical incision. EZ Access
(Hakko Co., Ltd.) was adjusted and two or three devices were
introduced through it: A flexible laparoscope (Olympus, Tokyo,
Japan) and one or two operating forceps (Fig. 2). Depending on the surgical procedure,
one or two ports were added to the lateral abdomen. An operator
used two trocars and an assistant used another two trocars,
including the laparoscope. The pneumoperitoneum was set at 10 mmHg.
In all the cases, laparoscopic intestinal mobilization and lymph
node dissection were performed. The intestinal specimen was
extracted through the umbilical incision. Functional end-to-end
anastomosis (FEEA) or the double-stapling technique (DST).FEEA was
performed outside the body after extracting the proximal and distal
parts of the intestine through the incision If the specimen could
not be extracted, the skin incision was extended along the midline
(Fig. 1). Finally, a drainage tube
was placed in the pouch of Douglas through the lateral abdominal
port site. The fascia was closed with 1 Vicryl sutures (Johnson
& Johnson, New Brunswick, NJ, USA) and, after washing with warm
saline (500 ml), the skin was closed with 4–0 polydioxanone sutures
(Johnson & Johnson). The clinical and operative factors and
postoperative outcomes between the conventional and the Z incision
groups were analyzed. Clinical stage was determined according to
Japanese Clinical Guidelines, Japanese Classification of Colorectal
Carcinoma (10).
Statistical analysis
For continuous variables, data are expressed as
median (range). The clinical and surgical factors between the
conventional and Z incision groups were analyzed using the Wilcoxon
rank-sum and Pearson's Chi-square tests. All the data were analyzed
using JMP software, version 11.0 (SAS Institute Inc., Cary, NC,
USA). Differences with P-values <0.05 were considered
statistically significant.
Results
Comparison of patient characteristics
between the conventional and Z incision groups
Gender, age, body mass index, clinical stage, tumor
site, operative procedure and lymph node dissection did not differ
significantly between the two groups (Table I). The surgical and perioperative
factors, apart from the length of the skin incision, did not differ
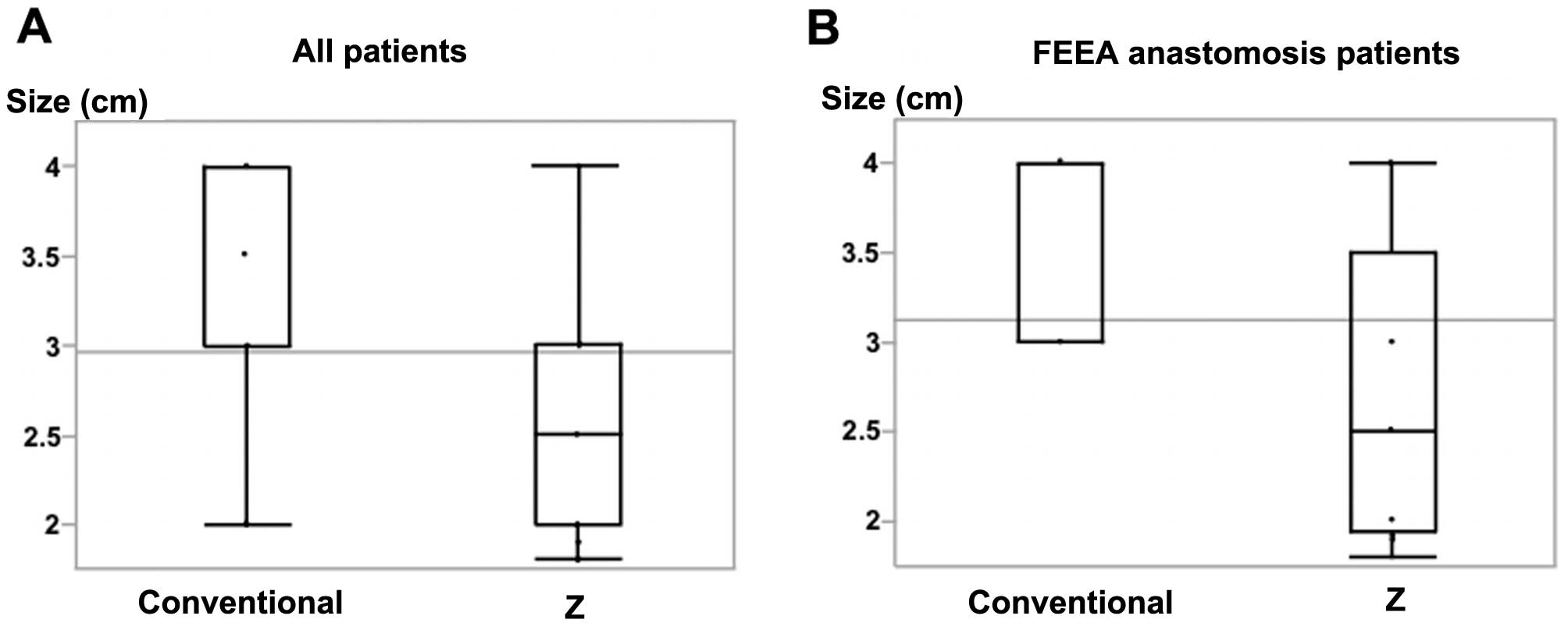
significantly between the two groups (Table II). The median length of the skin
incision was shorter in the Z incision group [2.5 cm (range,
1.8–4.0 cm)] compared with that in the conventional incision group
[3.0 cm (range, 2.0–4.0 cm)] (P=0.004) (Fig. 3). The median operative time was 283
min (range, 175–424 min) and 246 min (range, 169–471 min) in the
conventional and Z incision groups, respectively, whereas the blood
loss was 25 ml (range, 0–130 ml) and 35 ml (range, 5–300 ml),
respectively. In the conventional incision group, 3 patients
developed postoperative complications: 1 patient developed surgical
site infection in the umbilical wound, 1 suffered from
postoperative ileus, and 1 presented with anastomotic bleeding. All
the complications were grade I according to the Clavien-Dindo
classification (http://www.surgicalcomplication.info/index-2.html).
 | Table I.Clinical characteristics of the 29
patients. |
Table I.
Clinical characteristics of the 29
patients.
| Characteristics | Conventional incision
(n=15) | Z incision
(n=14) | P-value |
|---|
| Age, years
(range) | 62 (41–85) | 63 (38–81) | 0.861 |
| Gender
(male/female) | 10/5 | 8/6 | 0.597 |
| Body mass index,
kg/m2 (range) | 21 (18–28) | 22 (16–24) | 0.947 |
| Clinical stage
(0/I/II/III/IV) | 1/13/1/0/0 | 1/12/0/1/0 |
|
| Tumor site
(C/A/T/D/S/RS/Ra/Rb) | 2/5/0/1/1/4/1/1 | 1/2/3/3/1/1/1/2 |
|
 | Table II.Surgical factors and postoperative
outcome of the 29 patients. |
Table II.
Surgical factors and postoperative
outcome of the 29 patients.
| Variables | Conventional incision
(n=15) | Z incision
(n=14) | P-value |
|---|
| Operative procedure
(ICR/R/T/L/S/AR/LAR) | 3/4/0/2/0/4/2 | 1/3/2/3/1/1/3 |
|
| Lymph node
dissectiona
(D1/D2/D3) | 15/2/0 | 12/2/0 |
|
| Tumor size, mm
(range) | 30 (10–90) | 20 (10–50) |
0.128 |
| Length of umbilical
incision, cm (range) | 3.0 (2.0–4.0) | 2.5 (1.8–4.0) |
0.004 |
| Length of umbilical
incision (≤2.5 cm/2.5 cm<) | 1/14 | 10/4 | <0.001 |
| Number of ports
(range) | 3 (2–4) | 3 (2–4) |
1.000 |
| Operative time, min
(range) | 283 (175–424) | 246 (163–471) |
0.382 |
| Blood loss, ml
(range) | 25 (0–130) | 35 (5–300) |
0.417 |
| Open conversion | 0 | 0 |
|
| Anastomosis
(FEEA/DST) | 9/6 | 9/5 |
0.812 |
| SSI of umbilical
incision | 1 | 0 |
|
| Complications
(without SSI) | 2 | 0 |
|
| Postoperative
hospital stay, days (range) | 12 (5–83) | 11 (9–19) |
0.310 |
| Mortality | 0 | 0 |
|
| MFT Reccurence
(months) | 1 (25) | 0 (19) |
|
Comparison of patient characteristics
between the conventional and Z incision groups in patients
undergoing FEEA
We next examined cases in which FEEA was performed,
as this anastomosis procedure generally requires an extended
incision. The patients' characteristics did not differ
significantly between the two groups (Table III). The surgical and perioperative
factors, apart from the length of the skin incision, did not differ
significantly between the two groups (Table IV). The median length of the skin
incision was 4.0 cm (range, 3.0–4.0 cm) in the conventional and 2.5
cm (range, 1.8–4.0 cm) in the Z incision group (P=0.018),
suggesting that we may achieve shorter incisions using the Z
technique in FEEA. Using the Z technique, we performed RPS with a
shorter skin incision, without any effect on surgical or
perioperative factors.
 | Table III.Clinical characteristics of 18
patients with FEEA. |
Table III.
Clinical characteristics of 18
patients with FEEA.
| Characteristics | Conventional incision
(n=9) | Z incision (n=9) | P-value |
|---|
| Age, years
(range) | 62 (41–85) | 66 (38–77) | 0.894 |
| Gender
(male/female) | 8/1 | 6/3 | 0.256 |
| Body mass index,
kg/m2(range) | 20 (18–24) | 21 (16–24) | 0.857 |
| Clinical stage
(0/I/II/III/IV) | 0/8/1/0/0 | 1/7/0/1/0 |
|
| Tumor site
(C/A/T/D/S) | 2/5/0/1/1 | 1/2/3/3/0 |
|
 | Table IV.Surgical factors and postoperative
outcomes of 18 patients with FEEA. |
Table IV.
Surgical factors and postoperative
outcomes of 18 patients with FEEA.
| Variables | Conventional incision
(n=9) | Z incision (n=9) | P-value |
|---|
| Operative procedure
(ICR/R/T/L) | 3/4/0/2 | 1/3/2/3 |
|
| Lymph node
dissectiona
(D1/D2/D3) | 0/7/2 | 0/8/1 |
|
| Tumor size, mm
(range) | 30 (10–55) | 20 (10–50) | 0.264 |
| Length of umbilical
incision, cm (range) | 4.0 (3.0–4.0) | 2.5 (1.8–4.0) | 0.018 |
| Number of ports
(range) | 3 (2–4) | 3 (2–4) | 1.000 |
| Operative time, min
(range) | 262 (175–370) | 231 (163–430) | 0.627 |
| Blood loss, ml
(range) | 40 (0–130) | 40 (5–300) | 0.929 |
| Open conversion | 0 | 0 |
|
| SSI of umbilical
incision | 1 | 0 |
|
| Complication (without
SSI) | 2 | 0 |
|
| Postoperative
hospital stay, days (range) | 13 (5–17) | 11 (9–13) | 0.052 |
| Mortality | 0 | 0 |
|
| MFT Recurrence
(months) | 1 (25) | 0 (19) |
|
Discussion
The evolution of laparoscopic surgery has recently
led to the introduction of SILS and RPS, despite the limited
laparoscopic handling space. Certain studies previously compared
single-incision laparoscopic colectomy to conventional multiport
laparoscopic colectomy for CRC in terms of operative procedure and
outcome (11–13). There were no differences in operative
time, open conversion, number of harvested lymph nodes, length of
stay, postoperative complications and mortality.
In our study, we also hypothesized that the shorter
length of the umbilical incision may present with certain
difficulties in the operative technique of RPS for CRC. However,
there was no difference in those factors between the conventional
and the Z skin incision groups. Therefore, the shorter length of
the umbilical incision does not increase the difficulty of RPS in
terms of laparoscopic handling. Fujii et al (13) reported that the median length of the
skin incision was 3.3 cm in SILS for CRC, and Hachisuka et
al (14) reported on the zigzag
skin incision in RPS for CRC. An incision was required from above
to below the umbilical ring. Using the Z skin incision, we were
able to shorten the length of the umbilical incision and, in some
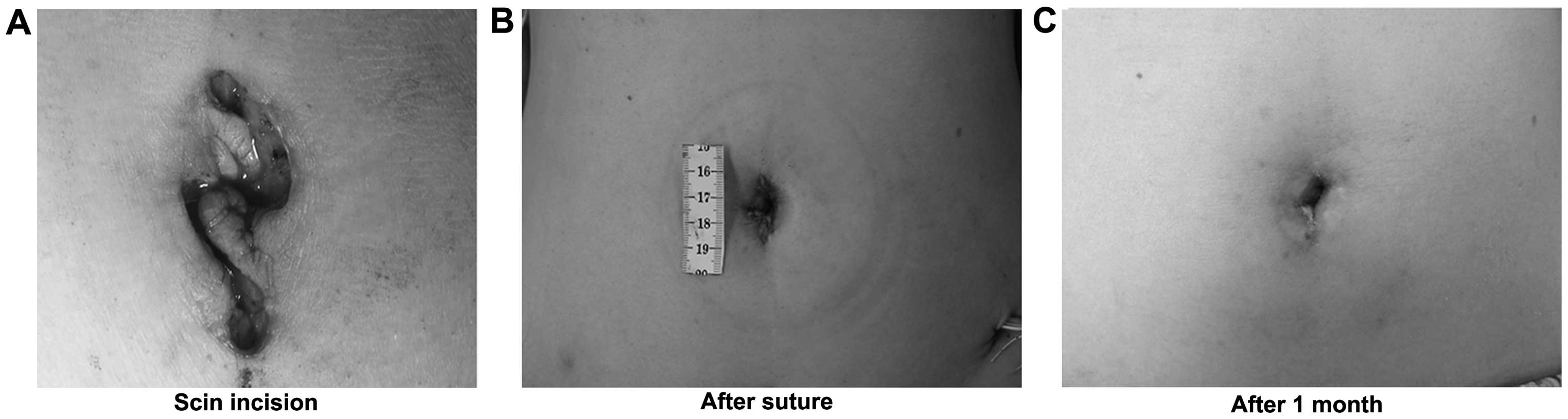
cases, the incisions were limited within the umbilical ring. With
an umbilical incision of <2.5 cm within the umbilical ring, the
patient appeared scar-free 1 month after surgery (Fig. 4). The length of the umbilical incision
was significantly <2.5 cm in the Z incision group (P=0.0003).
Performing and closing the Z incision is somewhat complicated
compared with the conventional incision. It generally requires 9
min to open and 15 min to close; however, there were no differences
in the total operative time between the conventional and Z skin
incision groups. There was no difference in surgical and
perioperative factors. Therefore, the Z incision is a useful
technique, particularly in SILS and RPS that use the umbilicus for
multi-trocar access.
In conclusion, we developed an umbilical Z skin
incision technique to perform an abdominal laparoscopic colectomy
with an umbilical skin incision of a shorter length. This appears
to be a useful technique in RPS for CRC.
Acknowledgements
We would like to thank Dr T. Fukata, Dr T. Umeda, Dr
K. Sasaki, Dr Y. Wada, Dr Y. Shishido, Dr T. Hara and Dr K. Hayashi
for surgical assistance and fruitful discussion. We would also like
to thank Ms. Y. Katayama for technical assistance.
Glossary
Abbreviations
Abbreviations:
|
RPS
|
reduced-port surgery
|
|
CRC
|
colorectal cancer
|
|
SILS
|
single-incision laparoscopic
surgery
|
References
|
1
|
Yamamoto S, Inomata M, Katayama H,
Mizusawa J, Etoh T, Konishi F, Sugihara K, Watanabe M, Moriya Y and
Kitano S: Japan Clinical Oncology Group Colorectal Cancer Study
Group: Short-term surgical outcomes from a randomized controlled
trial to evaluate laparoscopic and open D3 dissection for stage
II/III colon cancer: Japan Clinical Oncology Group Study JCOG 0404.
Ann Surg. 260:23–30. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Braga M, Frasson M, Zuliani W, Vignali A,
Pecorelli N and Di Carlo V: Randomized clinical trial of
laparoscopic versus open left colonic resection. Br J Surg.
97:1180–1186. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yang TX and Chua TC: Single-incision
laparoscopic colectomy versus conventional multiport laparoscopic
colectomy: A meta-analysis of comparative studies. Int J Colorectal
Dis. 28:89–101. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Makino T, Milsom JW and Lee SW:
Single-incision laparoscopic surgeries for colorectal diseases:
Early experiences of a novel surgical method. Minim Invasive Surg.
2012:7830742012.PubMed/NCBI
|
|
5
|
Makino T, Milsom JW and Lee SW:
Feasibility and safety of single-incision laparoscopic colectomy: A
systematic review. Ann Surg. 255:667–676. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Champagne BJ, Papaconstantinou HT, Parmar
SS, Nagle DA, Young-Fadok TM, Lee EC and Delaney CP:
Single-incision versus standard multiport laparoscopic colectomy: A
multicenter, case-controlled comparison. Ann Surg. 255:66–69. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Vestweber B, Galetin T, Lammerting K, Paul
C, Giehl J, Straub E, Kaldowski B, Alfes A and Vestweber KH:
Single-incision laparoscopic surgery: Outcomes from 224 colonic
resections performed at a single center using SILS. Surg Endosc.
27:434–442. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Davis JS: The relaxation of scar
contractures by means of the Z-, or reversed Z-type incision:
Stressing the use of scar infiltrated tissues. Ann Surg.
94:871–884. 1931. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tan O, Atik B and Ergen D: A new method in
the treatment of postburn scar contractures: Double opposing V-Y-Z
plasty. Burns. 32:499–503. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Watanabe T, Itabashi M, Shimada Y, Tanaka
S, Ito Y, Ajioka Y, Hamaguchi T, Hyodo I, Igarashi M, Ishida H, et
al: Japanese Society for Cancer of the Colon and Rectum: Japanese
Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2010
for the treatment of colorectal cancer. Int J Clin Oncol. 17:1–29.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Huscher CG, Mingoli A, Sgarzini G, Mereu
A, Binda B, Brachini G and Trombetta S: Standard laparoscopic
versus single-incision laparoscopic colectomy for cancer: Early
results of a randomized prospective study. Am J Surg. 204:115–120.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kim SJ, Ryu GO, Choi BJ, Kim JG, Lee KJ,
Lee SC and Oh ST: The short-term outcomes of conventional and
single-port laparoscopic surgery for colorectal cancer. Ann Surg.
254:933–940. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fujii S, Watanabe K, Ota M, Watanabe J,
Ichikawa Y, Yamagishi S, Tatsumi K, Suwa H, Kunisaki C, Taguri M,
et al: Single-incision laparoscopic surgery using colon-lifting
technique for colorectal cancer: A matched case-control comparison
with standard multiport laparoscopic surgery in terms of short-term
results and access instrument cost. Surg Endosc. 26:1403–1411.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hachisuka T, Kinoshita T, Yamakawa T,
Kurata N, Tsutsuyama M, Umeda S, Tokunaga S, Yarita A, Shibata M,
Shimizu D, et al: Transumbilical laparoscopic surgery using GelPort
through an umbilical zigzag skin incision. Asian J Endosc Surg.
5:50–52. 2012. View Article : Google Scholar : PubMed/NCBI
|