Introduction
Pheochromocytoma is a neoplasm of the chromaffin
tissues, which mostly develops within the adrenal medulla. Only
~15% of pheochromocytomas develop from extra-adrenal chromaffin
tissues. Pheochromocytoma of the urinary bladder is rare, and it
originates from the chromaffin tissues of the sympathetic nervous
system in the urinary bladder wall (1,2). The
typical signs are hematuria, hypertension during micturition,
together with generalized symptoms due to the increased
catecholamine levels, including headache, blurred vision, heart
palpitations, profuse perspiration and flushing (1,3). The
standard treatment for localized or locally advanced
pheochromocytomas is surgery, while metastatic or recurrent tumors
are treated with palliative therapy (4–6).
We herein describe a case of primary urinary bladder
pheochromocytoma with invasion of the prostate, without distant
metastasis. The patient refused surgery and opted to receive
radiotherapy.
Case report
A 23-year-old male patient presented with gross
hematuria for 2 months, accompanied by hypertension for 20 days.
The patient had no family history of hypertension and presented
with no other symptoms. On admission, the blood pressure and pulse
rate were 160/100 mmHg and 76 beats/min, respectively. During
micturition, the blood pressure increased to 185/110 mmHg. The
physical examination was otherwise unremarkable and the
electrocardiography findings were normal.
Blood testing revealed high levels of norepinephrine
(26.81 nmol/l; normal range, 0.31–2.82 nmol/l) and epinephrine
(3.26 nmol/l; normal range, 0.03–0.98 nmol/l). A urinalysis
revealed hematuria and elevated levels of vanillylmandelic acid
(VMA) (121.9 µmol/24 h; normal range, 15.66–88.58 µmol/24 h). The
blood creatinine level was higher than normal (165 µmol/l; normal
range, 71–115 µmol/24 h). Computed tomography (CT) revealed
irregular thickening of the bladder wall, with an unclear boundary
of the bladder and prostate gland. There was an effusion in the
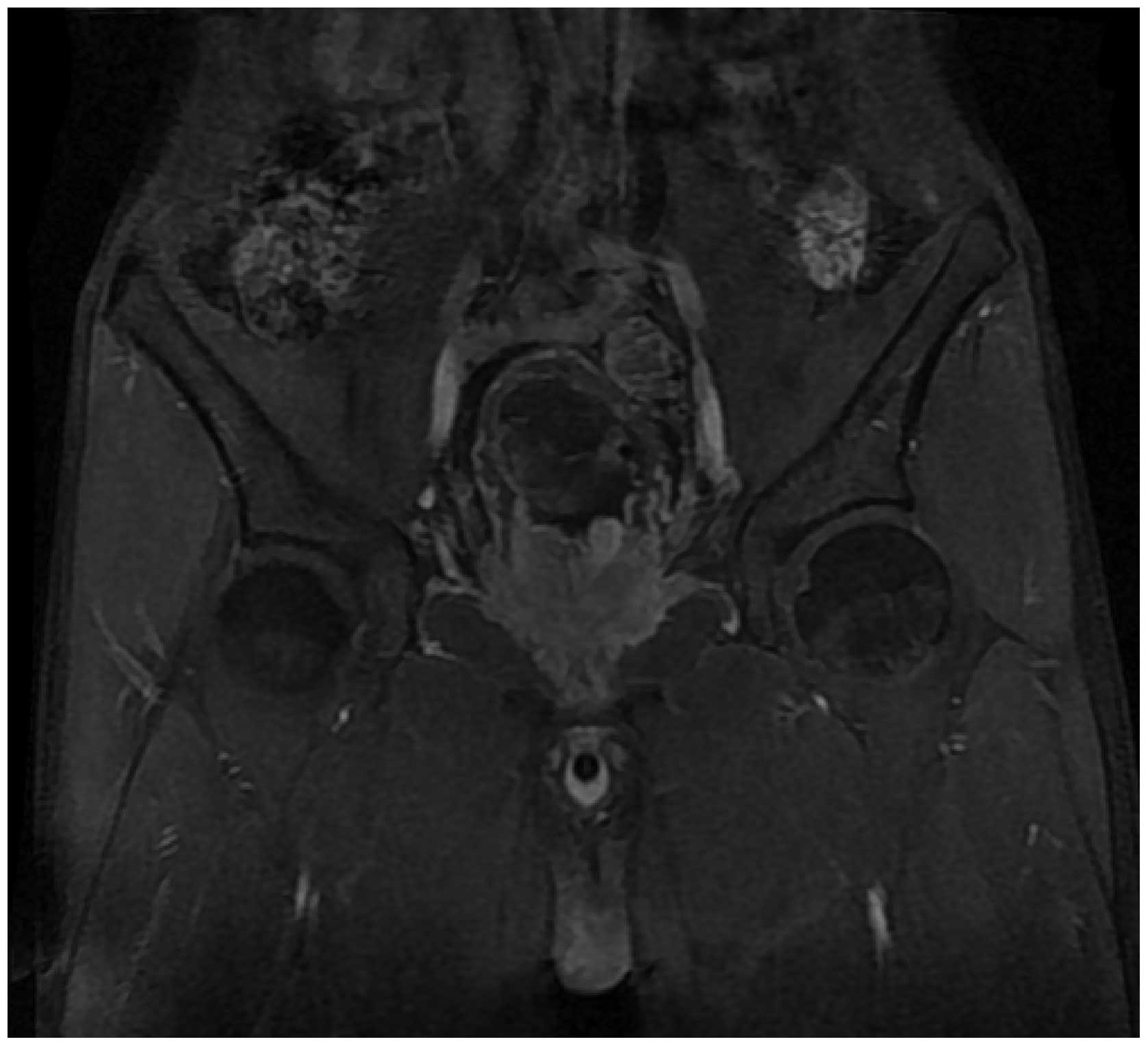
left renal pelvis, calyces and ureter. Magnetic resonance imaging
(MRI) revealed a heterogeneous mass located in the urinary bladder
and prostate (Fig. 1). The
histopathological report confirmed the diagnosis of bladder
pheochromocytoma with invasion of the prostate.
Although cystectomy and prostatectomy was considered
to be the preferred treatment in this case, the patient refused
surgery and opted to undergo radiotherapy; he received a total of
6,600 cGy, using 6-MV photon beams. The treatment was delivered in
30 fractions, 2.2 Gy/fraction, over 6 weeks. The patient completed
the treatment course without severe complications or side
effects.
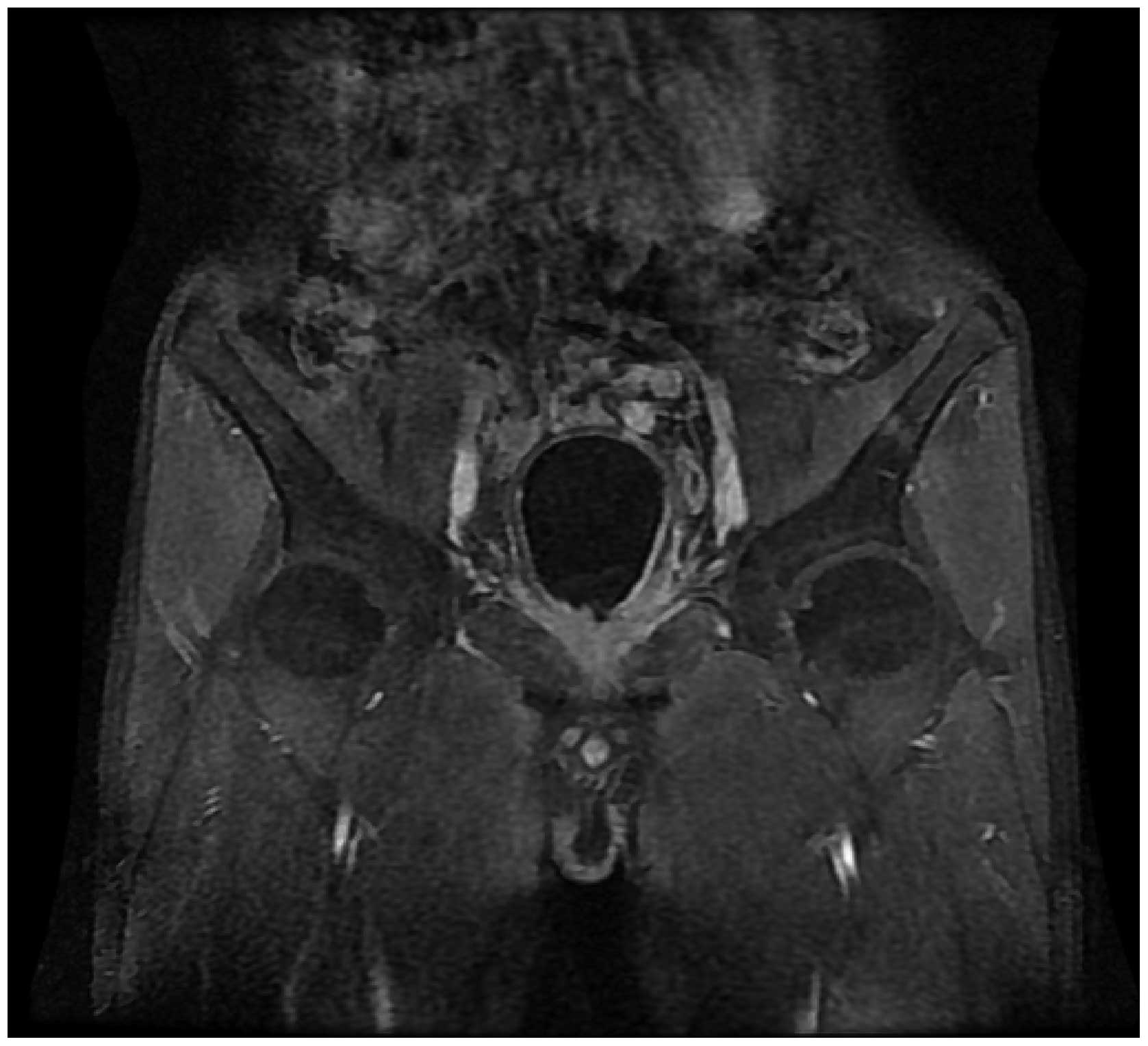
An MRI conducted one year after radiotherapy
revealed that the size of the tumor was clearly reduced (Fig. 2). The blood pressure remained within
normal limits after discontinuing the antihypertensive medication,
such as nifedipine controlled release tablets; serum
norepinephrine, epinephrine and urinary VMA levels were also
reduced and remained normal during the 1.5-year follow-up. However,
the creatinine level increased significantly to 704 µmol/l shortly
after radiotherapy. An ultrasound examination revealed that the
left hydronephrosis was exacerbated and right hydronephrosis
appeared following radiotherapy. A percutaneous nephrostomy
drainage was performed and the creatinine decreased to nearly
normal levels 1 month later; the drainage tube was then removed. A
mild bilateral hydronephrosis persisted persisted for one year and
the creatinine level was 120 µmol/l 1.5 years later.
Discussion
Pheochromocytoma is a rare catecholamine-producing
tumor, which commonly develops in the adrenal gland or paraaortic
ganglia (7,8). Approximately 3–13% of all
pheochromocytomas are malignant, and extra-adrenal
pheochromocytomas are more commonly malignant compared with
intra-adrenal tumors. No reliable histological characteristics
identify a pheochromocytoma as malignant, apart from the presence
of distant metastases, such as to the locoregional lymph nodes.
Metastasis is defined as appearance of chromaffin tissues at
non-chromaffin sites distant from the primary tumor (9,10).
Pheochromocytoma of the bladder is rare and it arises from
paraganglionic cells within the bladder wall; it often originates
in the bladder trigone, and rarely in the anterior or lateral wall,
which was the case in our patient (1,2). The most
common symptoms of bladder pheochromocytoma include hypertension,
hematuria and other symptoms associated with raised catecholamine
levels. However, certain patients may be asymptomatic (1,3). Our
patient only presented with hematuria and high blood pressure.
The biochemical diagnosis of pheochromocytoma is
confirmed through measurement of the catecholamines or their
metabolites in the plasma and urine (11). The blood norepinephrine and
epinephrine and urinary VMA levels were increased in our patient,
which supported the diagnosis of pheochromocytoma. The imaging
methods used for diagnosis include ultrasonography, CT, MRI and
meta-iodobenzylguanidine (MIBG) scintigraphy. CT may demonstrate
the association between the mass and the surrounding tissues;
however, it exhibits a high sensitivity for adrenal, but a lower
sensitivity for extra-adrenal pheochromocytomas. MRI may also
detect primary tumors and metastases, despite their small size, and
it is also more sensitive compared with CT in the evaluation of the
extra-adrenal pheochromocytomas (12–14). MIBG
scintigraphy exhibits a high sensitivity and specificity and serves
as a complementary diagnostic method (15,16). Our
patient was definitely diagnosed with pheochromocytoma by means of
biochemical examinations, CT and MRI. Therefore, we did not
consider a MIBG scan to be necessary. The histopathological report
confirmed the diagnosis of bladder pheochromocytoma with invasion
of the prostate, indicating that the tumor was malignant.
There is currently no effective treatment for
malignant pheochromocytoma. Although complete eradication of the
lesions may not be feasible, cytoreductive surgery is recommended
to reduce tumor burden and the symptoms of catecholamine excess. In
patients with advanced disease, for whom surgical resection is not
an option, systemic chemotherapy, radiotherapy and treatment with
131I-MIBG may be used to achieve symptomatic relief
(4–6).
However, the evidence on the effectiveness of these treatments is
limited for the majority of the cases. A limited number of case
reports, although not large patient samples or controlled trials,
have been published on the effectiveness of radiotherapy for
malignant pheochromocytoma. Previous studies considered that
radiotherapy was ineffective as a primary therapy and did not
prevent local recurrence. However, radiotherapy achieved control of
lymph node and bone metastases (17–19).
Cystectomy and prostatectomy was considered to be the preferred
treatment in the present case. However, the patient refused to
undergo surgery. The tumor in the bladder trigone caused
hydronephrosis and hydroureter, which resulted in postrenal renal
failure. In order to relieve the hydroureter and hydronephrosis
caused by the bladder pheochromocytoma, radiotherapy was selected.
Our study demonstrated that radiotherapy led to tumor necrosis and
caused the tumor to shrink gradually. Furthermore, the blood
pressure was decreased and antihypertensive drugs were
discontinued. In addition, the levels of catecholamines and their
metabolites decreased to within the normal range.
Extra-adrenal pheochromocytomas are more likely to
recur and metastasize; thus, long-term follow-up is required to
detect any recurrence or metastasis (20,21).
Although the size of the lesion did not increase and the blood
pressure remained normal 1.5 years later in the present case,
lifelong follow-up is warranted.
The patient had left hydronephrosis prior to
treatment and his creatinine level was marginally higher than the
normal range. However, the left hydronephrosis was exacerbated and
he developed right hydronephrosis shortly after radiotherapy. In
addition, the creatinine level increased significantly. These
changes may be attributed to the aggravation of the distal ureteral
obstruction caused by edema of the ureteral orifice and the bladder
trigone following radiotherapy. The hydronephrosis subsided and the
creatinine level decreased following percutaneous nephrostomy
drainage. The remission of hydronephrosis and decrease in
creatinine levels following radiotherapy may be due to the relief
of the ureteral obstruction caused by tumor shrinkage.
This case was reported due to the rarity of
pheochromocytomas of the bladder with invasion of the prostate, and
the current lack of effective treatment. The patient presented only
with hematuria and high blood pressure, without any other typical
symptoms of pheochromocytoma, despite increased levels of
catecholamines and their metabolic products. Although malignant
pheochromocytoma is considered to be resistant to radiation, and
radiotherapy is not considered a primary treatment modality, in our
case radiotherapy was effective for the treatment of malignant
pheochromocytoma to a certain extent; therefore, radiotherapy may
be selected when surgery is not feasible.
In conclusion, although malignant pheochromocytoma
of the bladder is a rare occurrence, its diagnosis should be
suspected in the presence of a bladder tumor accompanied by high
blood pressure. There are currently no large-scale clinical studies
comparing different therapeutic modalities in a randomized and
controlled manner, due to the scarcity of cases with this type of
tumor. Although malignant pheochromocytoma is generally considered
to be unresponsive to radiotherapy, our case demonstrated that
radiotherapy was effective to a certain extent and, therefore it
may be selected when surgery is not an option.
References
|
1
|
Doran F, Varinli S, Bayazit Y, Bal N and
Ozdemir S: Pheochromocytoma of the urinary bladder. APMIS.
110:733–736. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Onishi T, Sakata Y, Yonemura S and
Sugimura Y: Pheochromocytoma of the urinary bladder without typical
symptoms. Int J Urol. 10:398–400. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Naqiyah I, Rohaizak M, Meah FA, Nazri MJ,
Sundram M and Amram AR: Phaeochromocytoma of the urinary bladder.
Singapore Med J. 46:344–346. 2005.PubMed/NCBI
|
|
4
|
Nazario J and Gupta S: Transarterial
liver-directed therapies of neuroendocrine hepatic metastases.
Semin Oncol. 37:118–126. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Pacak K, Eisenhofer G, Ahlman H, Bornstein
SR, Gimenez-Roqueplo AP, Grossman AB, Kimura N, Mannelli M, McNicol
AM and Tischler AS: International Symposium on Pheochromocytoma:
Pheochromocytoma: Recommendations for clinical practice from the
first international symposium. October 2005. Nat Clin Pract
Endocrinol Metab. 3:92–102. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Vogl TJ, Naguib NN, Zangos S, Eichler K,
Hedayati A and Nour-Eldin NE: Liver metastases of neuroendocrine
carcinomas: Interventional treatment via transarterial
embolization, chemoembolization and thermal ablation. Eur J Radiol.
72:517–528. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bravo EL and Tagle R: Pheochromocytoma:
State-of-the-art and future prospects. Endocr Rev. 24:539–553.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Neumann HP, Bausch B, McWhinney SR, Bender
BU, Gimm O, Franke G, Schipper J, Klisch J, Altehoefer C, Zerres K,
et al: Germ-line mutations in nonsyndromic pheochromocytoma. N Engl
J Med. 346:1459–1466. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Eisenhofer G, Bornstein SR, Brouwers FM,
Cheung NK, Dahia PL, de Krijger RR, Giordano TJ, Greene LA,
Goldstein DS, Lehnert H, et al: Malignant pheochromocytoma: Current
status and initiatives for future progress. Endocr Relat Cancer.
11:423–436. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Scholz T, Schulz C, Klose S and Lehnert H:
Diagnostic management of benign and malignant pheochromocytoma. Exp
Clin Endocrinol Diabetes. 115:155–159. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kvetnansky R, Sabban EL and Palkovits M:
Catecholaminergic systems in stress: Structural and molecular
genetic approaches. Physiol Rev. 89:535–606. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Vyas S, Kalra N, Singh SK, Agarwal MM,
Mandal AK and Khandelwal N: Pheochromocytoma of urinary bladder.
Indian J Nephrol. 21:198–200. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang H, Ye H, Guo A, Wei Z, Zhang X, Zhong
Y, Fan Z, Wang Y and Wang D: Bladder paraganglioma in adults: MR
appearance in four patients. Eur J Radiol. 80:e217–e220. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Whalen RK, Althausen AF and Daniels GH:
Extra-adrenal pheochromocytoma. J Urol. 147:1–10. 1992.PubMed/NCBI
|
|
15
|
Berglund AS, Hulthén UL, Manhem P,
Thorsson O, Wollmer P and Törnquist C: Metaiodobenzylguanidine
(MIBG) scintigraphy and computed tomography (CT) in clinical
practice. Primary and secondary evaluation for localization of
phaeochromocytomas. J Intern Med. 249:247–251. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Nakatani T, Hayama T, Uchida J, Nakamura
K, Takemoto Y and Sugimura K: Diagnostic localization of
extra-adrenal pheochromocytoma: Comparison of 123I-MIBG
imaging and 131I-MIBG imaging. Oncol Rep. 9:1225–1227.
2002.PubMed/NCBI
|
|
17
|
Naguib M, Caceres M, Thomas CR Jr, Herman
TS and Eng TY: Radiation treatment of recurrent pheochromocytoma of
the bladder: Case report and review of literature. Am J Clin Oncol.
25:42–44. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tato A, Orte L, Diz P, Quereda C and
Ortuno J: Malignant pheochromocytoma, still a therapeutic
challenge. Am J Hypertens. 10:479–481. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yu L, Fleckman AM, Chadha M, Sacks E,
Levetan C and Vikram B: Radiation therapy of metastatic
pheochromocytoma: Case report and review of the literature. Am J
Clin Oncol. 19:389–393. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Guller U, Turek J, Eubanks S, Delong ER,
Oertli D and Feldman JM: Detecting pheochromocytoma: Defining the
most sensitive test. Ann Surg. 243:102–107. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zeitlin I, Dessau H, Lorberboym M and
Beigel Y: Malignant pheochromocytoma of the urinary bladder:
Challenges in diagnosis and management. Isr Med Assoc J.
13:311–313. 2011.PubMed/NCBI
|