Introduction
Pancreatic exocrine tumours are fatal in the
majority of the patients, due to late diagnosis and poor response
to combined treatment. Patients with locally advanced unresectable
or metastatic pancreatic cancer represent a clear majority among
all patients with pancreatic cancer (1–4).
Pancreatic cancer is the fourth leading cause of
cancer-related mortality, with a 5-year overall survival (OS) rate
of 6% (3–7). Cancers that are detected incidentally
are likely to be treated surgically, with or without adjuvant
therapy. However, the median survival time is limited to 11–23
months and the 5-year survival rate is <20% (2,4–6).
The majority of the patients present with incurable
disease and several experience rapid clinical deterioration,
without any improvement over several decades (7,8).
Determining whether a tumour is resectable is not
well reflected by TNM system staging, as demonstrated by the wide
range of survival figures reported for each stage.
To be determined as resectable, tumours must show no
evidence of extrapancreatic disease or direct tumour extension to
the celiac axis and superior mesenteric artery. However, the
evidence of non-obstructive superior mesenteric-portal vein
confluence does not always preclude tumour resection.
Complete surgical resection is the only potentially
curative treatment available.
For ~35–40% of the patients who have locally
advanced disease at the time of diagnosis, chemoradiation (CRT) is
one of the most common treatments (9). CRT is an effective palliative treatment,
although it has notable limitations. Studies have shown improved
median survival times in patients treated with CRT compared with
either chemotherapy (6) or RT alone.
Patients with locally advanced disease may present with major local
symptoms.
Optimal symptomatic treatment may play a key role in
the management of metastatic disease. This may require stenting or
bypass surgery for obstructive jaundice or gastric outlet
obstruction. The most common symptom from local extension is pain,
which may significantly affect the patient's quality of life. RT is
used to control these symptoms, as was reported in locally advanced
gastric cancer (10,11).
Patients and methods
Patient population
The candidate subjects for this retrospective study
were 31 patients with histologically proven unresectable pancreatic
cancer registered at the Center of Oncology, Maria Sklodowska-Curie
Memorial Institute (Gliwice, Poland) from November, 2000 to
November, 2007. We included patients with stage III pancreatic
cancer at the time of diagnosis, based on the 6th American Joint
Committee on Cancer staging guidelines (12). The median age of the patients was 57
years (range, 35–77 years) and the median Eastern Cooperative
Oncology Group performance status score was 2 (range, 0–3). The
patients in the study included 18 men (58%) and 13 women (42%). The
characteristics of the patients and tumours are summarised in
Table I. The initial palliative
treatment option for all the patients was chemotherapy based on
5-fluorouracil (5-FU) alone, or 5-FU with gemcitabine for the 5
patients with metastasis. Among the patients treated with
chemotherapy for palliation, single-agent 5-FU was the most common
treatment.
 | Table I.Patient and tumour characteristics in
31 patients. |
Table I.
Patient and tumour characteristics in
31 patients.
| Characteristics | Patient no. (%) |
|---|
| Gender |
|
| Male | 18 (58) |
|
Female | 13 (42) |
| Age, years |
|
| Median
(range) | 57 (35–77) |
|
70–79 | 8 (26) |
|
60–69 | 8 (26) |
|
<60 | 15 (48) |
| ECOG performance
status |
|
| 0 | 3 (10) |
| 1 | 10 (32) |
| 2 | 13 (42) |
| 3 | 5 (16) |
| Tumour location |
|
| Head | 22 (71) |
|
Body-tail | 9 (29) |
| Maximum tumour
diameter, cm |
|
| Median
(range) | 5.12 (2.2–11) |
| Metastases |
|
| M0 | 26 (84) |
| M1 | 5 (16) |
| Histological
diagnosis |
|
|
Adenocarcinoma | 29 (94) |
|
Others | 2 (6) |
| Differentiation |
|
| High | 14 (45) |
|
Moderate | 3 (10) |
| Poor | 2 (6) |
| Not
defined | 12 (39) |
| Percent weight
loss |
|
|
<10% | 21(68) |
| No
loss | 10 (32) |
| Presenting symptoms
prior to RTa |
|
|
Jaundice | 2 (6) |
| Abdominal
pain | 21 (68) |
|
Fatigue | 7 (23) |
|
Diarrhoea | 10 (32) |
| Back
pain | 10 (32) |
The primary endpoints of the study were OS,
treatment-related toxicity and an estimated intensity of pain
correlated with pancreatic cancer.
RT
Three-dimensional computer planning was used in all
the cases. All the patients underwent CT scans (X-vision, Somatom;
Siemens Inc., Munich, Germany) and the Eclipse system (Varian
Medical Systems, Palo Alto, CA, USA) was used for RT treatment
planning. The clinical target volume (CTV) included the primary
tumour - whole pancreatic body, as detected by CT scans. The
planning target volume was defined as the CTV plus 10-mm margins in
all directions. The two- (anterior and posterior) or three-field
techniques (anterior, posterior and oblique lateral field) were
used. RT was delivered with 20-MV X-rays. A total dose of 6–30 Gy
was delivered in 1–10 fractions over a period of 1 day-2 weeks.
One patient (3%) received 6 Gy in a single dose as
hypofractionated treatment, 1 patient (3%) received 11 Gy in 5
fractions, 3 patients (10%) received 18 Gy in 6 fractions, 7
patients (23%) received 20 Gy in 5 fractions and 19 patients (61%)
received 30 Gy in 10 fractions. We used two opposite fields in 22
patients (71%) and three oblique fields in 9 patients (29%). The
V50% of the liver was limited to 30 Gy and the V30% of both kidneys
was limited to 20 Gy.
Toxicity criteria and tumour
response
The treatment-related toxicities were classified
according to the Common Terminology Criteria for Adverse Events,
version 3.0 (13). Nausea, vomiting,
diarrhoea, leukopaenia, granulocytopaenia, lymphocytopaenia and
thrombocytopaenia were assessed weekly.
The pain intensity was assessed after 4 weeks of RT
using a visual analogue scale. The tumour response was assessed
based on the CT scans.
Statistical analysis
The OS was calculated from the first day of RT.
The survival curves were constructed using the
Kaplan-Meier method. Statistical analyses of categorical variables
were performed using the arithmetic mean coefficient of dominance.
The association between survival and one or more covariates was
examined using the Cox proportional hazards regression model. The
risk of early death was estimated using the hazard ratio (HR).
Two-sided P-values of <0.05 were considered
significant. All analyses were performed using the R 2.11.1
programme for Windows XP (www.r-project.org).
Results
Tolerance and response to
treatment
We observed an absence of RT interruptions, lack of
hospitalisation due to toxic reactions and an absence of severe
toxicity in patients undergoing palliative RT. Palliative RT was
well-tolerated, with only 9 patients (29%) requiring treatment for
toxicity, which primarily included nausea and vomiting in patients
with grade 2 (G2) events. The predominant G1 adverse events were
abdominal pain and fatigue (Table
II).
 | Table II.Treatment-related adverse events in 31
patients. |
Table II.
Treatment-related adverse events in 31
patients.
| Grade of adverse
events | Patient no. (%) |
|---|
| Nausea |
|
| G1 | 4
(13) |
| G2 | 6
(19) |
| G3–5 | 0 (0) |
| Vomiting |
|
| G1 |
2 (6.5) |
| G2 | 3
(10) |
|
G3–5 | 0 (0) |
| Diarrhoea |
|
| G1 | 3
(10) |
| G2 | 0 (0) |
|
G3–5 | 0 (0) |
| Fatigue |
|
| G1 | 7
(23) |
| G2 | 0 (0) |
|
G3–5 | 0 (0) |
| Abdominal pain |
|
| G1 |
17 (55) |
| G2 |
12 (39) |
| G3, 4,
5 | 0 (0) |
The pain intensity was evaluated prior to initiation
and 1 month after RT, and the analgesic drug therapy was adjusted
until a 0–3 pain score was reached (WHO).
A total of 17 patients (55%) achieved good pain
control (G1) without pharmacological therapy, 12 patients (39%)
reduced their use of analgesics (G2), and in the remaining 2
patients (6%) there was no change in analgesic use (G3).
Survival and pattern of failure
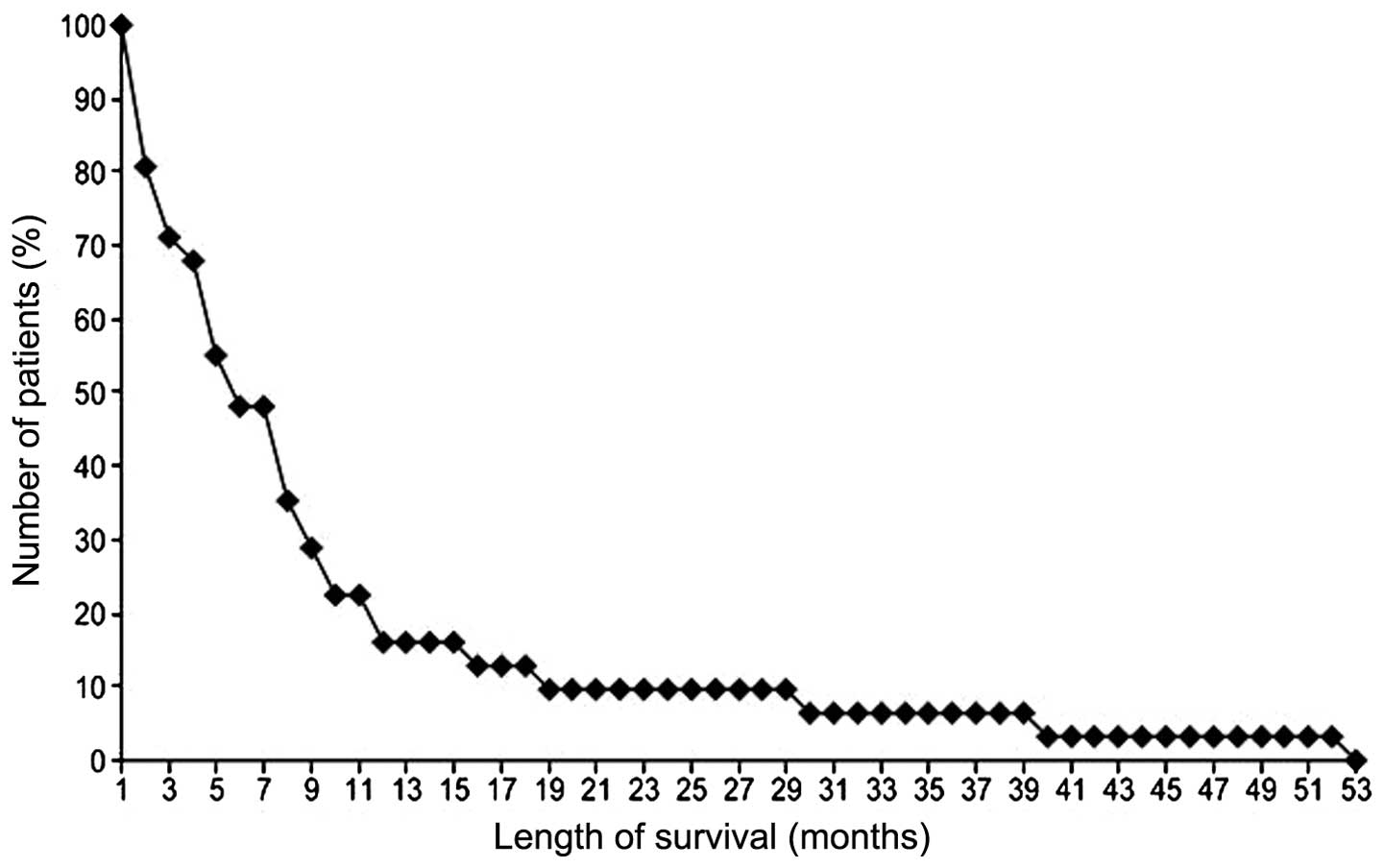
The median survival time for all 31 patients was 5
months (range, 1–53 months). The 1-year OS rate was 16.13%
(Fig. 1). An important positive
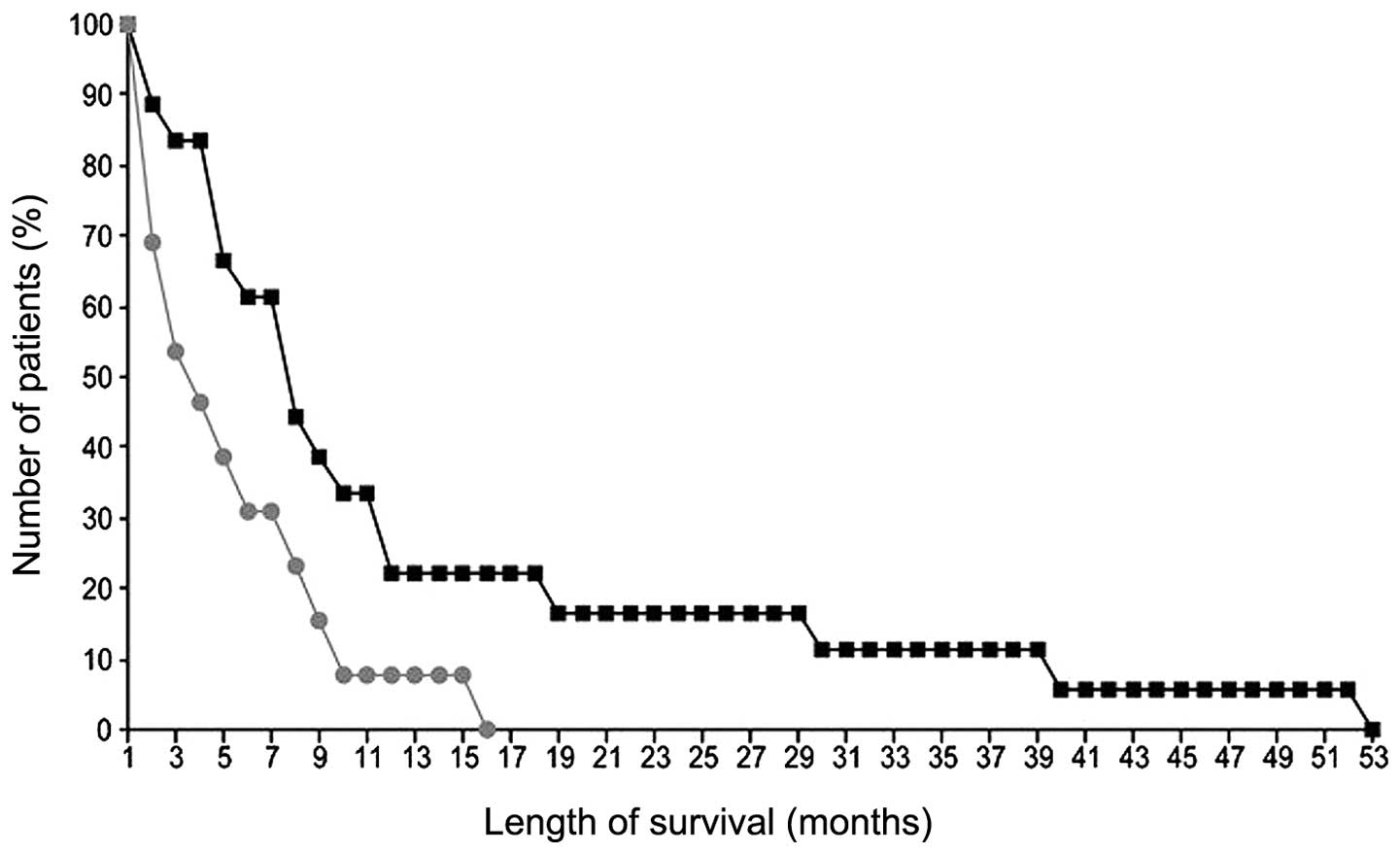
predictor of survival in single- and multiparameter analyses was
age (P=0.02). However, in the single-parameter analysis, the
positive predictors of survival were male gender (P=0.03) (Fig. 2), location of the tumour in the
pancreatic head (P=0.03), a lack of weight loss (P=0.03) and a lack
of metastases (P=0.02) (Tables III
and IV). Tumour diameter and total
dose were not found to be prognostically significant. The mean
total dose was 22.7 Gy [1 patient (3%) received 11 Gy in 5
fractions, 3 patients (10%) received 18 Gy in 6 fractions, 7
patients (23%) received 20 Gy in 5 fractions and 19 patients (61%)
received 30 Gy in 10 fractions. A single patient received 6 Gy in 1
fraction].
 | Table III.Multiparameter analysis of prognostic
factors affecting 1-year and overall survival rates. |
Table III.
Multiparameter analysis of prognostic
factors affecting 1-year and overall survival rates.
|
|
| P-value |
|---|
|
|
|
|
|---|
| Prognostic
factors | Patient no. | 12-month | All-month |
|---|
| Gender |
| 0.65 | 0.49 |
|
Male | 18 |
|
|
|
Female | 13 |
|
|
| Age |
| 0.02 | 0.02 |
| Location of
tumour |
|
|
|
|
Head | 22 | 0.13 | 0.14 |
|
Body-tail | 9 | 0.94 | 0.89 |
| Tumour
diameter |
| 0.15 | 0.14 |
| Weight loss |
|
|
|
|
>10% | 21 |
|
|
| No
loss | 10 | 0.32 | 0.41 |
| Metastases |
|
|
|
| M0 | 26 | 0.91 | 0.87 |
| M1 | 5 | 0.26 | 0.15 |
| Total dose
(TD) |
|
|
|
| Mean,
22.7 Gy |
|
|
|
| Range,
6–30 Gy |
|
|
|
 | Table IV.Single-parameter analysis of
prognostic factors affecting overall survival rate. |
Table IV.
Single-parameter analysis of
prognostic factors affecting overall survival rate.
| Prognostic
factors | Patient no. | OS P-value |
|---|
| Gender |
|
|
|
Male | 18 | 0.03 |
|
Female | 13 |
|
| Age |
| 0.02 |
| Location of
tumour |
|
|
|
Head | 22 | 0.03 |
|
Body-tail | 9 |
| Tumour
diameter |
| 0.14 |
| Weight loss |
|
|
|
>10% | 21 | 0.03 |
| No
loss | 10 |
|
| Metastases |
|
|
| M0 | 26 | 0.02 |
| M1 | 5 |
|
| Total dose
(TD) |
| 0.15 |
| Mean,
22.7 Gy |
|
|
| Range,
6–30 Gy |
|
|
The risk of premature death decreased by ~5% with
every increasing dose of RT (HR=0.947; 95% CI: 0.0208–0.0548;
P=0.0083).
Discussion
Most clinicians are cautious when recommending an
active treatment modality for pancreatic cancer in their clinical
practice, due to the poor prognosis of this disease, the wishes of
the patients or advanced age, although patients may be in a
reasonably good medical condition. Based on the results of
Krzyżanowska et al (14) in a
cohort study on locally advanced pancreatic cancer, 44% of the
patients received some form of cancer-directed therapy [24%
received concurrent CRT therapy (CCRT), 13% received RT alone and
7% received chemotherapy alone].
According to that study, any type of active
treatment was found to prolong survival.
Park et al (15), in a subgroup analysis of 340 patients
with unresectable, locally advanced, or metastatic pancreatic
cancer, found that stage III patients treated with either CCRT
(median OS, 10.4 months) or chemotherapy alone (median OS, 11.3
months) exhibited a survival benefit over supportive care (median
OS, 6.4 months), whereas stage IV patients treated with
chemotherapy alone (median OS, 6.4 months) showed a survival
benefit over supportive care (median OS, 3.1 months). The majority
of patients who have pancreatic cancer in their initial evaluation
have a combination of factors, such as advanced age, poor
performance status, medical comorbidity or tumour-related
conditions, such as anorexia; thus, they are poor candidates for
aggressive therapy, such as CRT. It is important to perform a
stratification of patients into treatment groups on the basis of
prognostic factors (16,17).
Morganti et al (18) evaluated 12 patients to observe whether
a short RT treatment (30 Gy, 3.0 Gy/fraction) exhibited analgesic
efficacy in patients with unresectable pancreatic carcinoma. They
concluded that, in patients excluded from standard concomitant CRT,
hypofractionated RT is feasible and results in pain relief in the
majority of the patients. Our observations also included a reduced
need for analgesics.
Pain due to pancreatic cancer is a manifestation of
neural invasion and obstructive ductal physiological pain in nearly
all patients. Intervention in the form of celiac neurolysis with
chemical agents decreases pain (19)
and may actually improve survival. Celiac neurolysis may be
performed intraoperatively, percutaneously, or endoscopically under
ultrasound guidance (20,21).
Other methods for reducing pain are advanced RT
techniques, such as stereotactic body RT, which are associated with
low rates of adverse effects and good local control in patients
with locally advanced pancreatic cancer (22,23).
However, not all patients are good candidates for this type of
sophisticated treatment.
This study indicates that more active treatments
should be attempted, even in cases of locally advanced unresectable
pancreatic cancer. Palliative RT is a last resort to improve local
pain control in patients with unresectable pancreatic cancer
(24). A total of 30 Gy in 10
fractions is one of the most commonly used dose-fractionation
regiments of palliative RT in cases with brain metastasis, bone
metastasis and bleeding from advanced gastric cancer (25). Wong et al (26) compared the scheme of 30 Gy in 10
fractions and the scheme of >30 Gy with concurrent infusions of
5-FU, and the median survival times were similar with both schemes.
Considering the median survival time (5 months) following RT, this
regimen appears to be adequate for patients with poor
prognosis.
The classical endpoints of palliative treatment are
survival, tumour response and quality of life. Patients who were
treated with palliative RT gained clinical benefits. Undoubtedly,
these treatments have reinforced the role of analgesic drugs.
Palliative treatment is often the only remaining
option in the management of pancreatic carcinoma, but its efficacy
is poor due to low tumour sensitivity and inadequate treatment
protocols. There are several options for palliative treatment, with
either an antitumor effect as immunotherapy (27,28) or as
supportive care. The present study demonstrated that patients with
locally advanced pancreatic cancer who receive palliative RT have
better survival rates compared with those who receive supportive
care alone. RT, when used as a palliative treatment, was
well-tolerated and was associated with a good median OS rate.
Hence, palliative RT remains a non-invasive treatment option for
improving pain control in patients with locally advanced or
metastatic pancreatic cancer.
References
|
1
|
Heinemann V: Present and future treatment
of pancreatic cancer. Semin Oncol. 29(Suppl 9): 23–31. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Goggins M: Molecular markers of early
pancreatic cancer. J Clin Oncol. 23:4524–4531. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chua YJ and Cunningham D: Adjuvant
treatment for resectable pancreatic cancer. J Clin Oncol.
23:4532–4537. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Real FX: A ‘catastrophic hypothesis’ for
pancreas cancer progression. Gastroenterology. 124:1958–1964. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nitecki SS, Sarr MG, Colby TV and van
Heerden JA: Long-term survival after resection for ductal
adenocarcinoma of the pancreas. Is it really improving? Ann Surg.
221:59–66. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sohn TA, Yeo CJ, Cameron JL, Koniaris L,
Kaushal S, Abrams RA, Sauter PK, Coleman J, Hruban RH and Lillemoe
KD: Resected adenocarcinoma of the pancreas-616 patients: Results,
outcomes, and prognostic indicators. J Gastrointest Surg.
4:567–579. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bilimoria KY, Bentrem DJ, Ko CY, Tomlinson
JS, Stewart AK, Winchester DP and Talamonti MS: Multimodality
therapy for pancreatic cancer in the U.S.: Utilization, outcomes,
and the effect of hospital volume. Cancer. 110:1227–1234. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sener SF, Fremgen A, Menck HR and
Winchester DP: Pancreatic cancer: A report of treatment and
survival trends for 100,313 patients diagnosed from 1985–1995,
using the National Cancer Database. J Am Coll Surg. 189:1–7. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Crane CH, Evans DB, Wolff RA, Abbruzzese
JL, Pisters PWT and Janjan NA: The pancreas. Radiation oncology:
rationale, technique, results (8th). Cox J and Ang KK: (Mosby, St
Louis, MO). 456–480. 2003.
|
|
10
|
Mantell BS: Radiotherapy for dysphagia due
to gastric carcinoma. Br J Surg. 69:69–70. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Myint AS: The role of radiotherapy in the
palliative treatment of gastrointestinal cancer. Eur J
Gastroenterol Hepatol. 12:381–390. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Greene FL, Page DL, Fleming ID, Fritz AG,
Balch CM, Haller DG and Morrow M: Digestive system. AJCC Cancer
Staging Manual (6th). (Chicago, IL). Springer. 151–157. 2002.
|
|
13
|
Cancer Therapy Evaluation Program: Common
Terminology Criteria for Adverse Events. version 3.0. DCTD, NCI,
NIH, DHHS. http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdfAccessed.
August 09–2006
|
|
14
|
Krzyzanowska MK, Weeks JC and Earle CC:
Treatment of locally advanced pancreatic cancer in the real word:
population-based practices and effectiveness. J Clin Oncol.
21:3409–3414. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Park JK, Yoon YB, Kim YT, Ryu JK, Yoon WJ
and Lee SH: Survival and prognostic factors of unresectable
pancreatic cancer. J Clin Gastroenterol. 42:86–91. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Rudra S, Narang AK, Pawlik TM, Wang H,
Jaffee EM, Zheng L, Le DT, Cosgrove D, Hruban RH, Fishman EK, et
al: Evaluation of predictive variables in locally advanced
pancreatic adenocarcinoma patients receiving definitive
chemoradiation. Pract Radiat Oncol. 2:77–85. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wild AT, Ye X, Ellsworth SG, et al: The
association between chemoradiation-related lymphopenia and clinical
outcomes in patients with locally advanced pancreatic
adenocarcinoma. Am J Clin Oncol. 38:259–265. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Morganti AG, Trodella L, Valentini V,
Barbi S, Macchia G, Mantini G, Turriziani A and Cellini N: Pain
relief with short-term irradiation in locally advanced carcinoma of
the pancreas. J Palliat Care. 19:258–262. 2003.PubMed/NCBI
|
|
19
|
Lillemoe KD, Cameron JL, Kaufman HS, Yeo
CJ, Pitt HA and Sauter PK: Chemical splanchnicectomy in patients
with unresectable pancreatic cancer. A prospective randomized
trial. Ann Surg. 217:447–457. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wong GY, Schroeder DR, Carns PE, Wilson
JL, Martin DP, Kinney MO, Mantilla CB and Warner DO: Effect of
neurolytic celiac plexus block on pain relief, quality of life, and
survival in patients with unresectable pancreatic cancer: A
randomized controlled trial. JAMA. 291:1092–1099. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Levy MJ and Wiersema MJ: EUS-guided celiac
plexus neurolysis and celiac plexus block. Gastrointest Endosc.
57:923–930. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Huguet F, Goodman KA, Azria D, Racadot S
and Abrams RA: Radiotherapy technical considerations in the
management of locally advanced pancreatic cancer: American-French
consensus recommendations. Int J Radiat Oncol Biol Phys.
83:1355–1364. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Goyal K, Einstein D, Ibarra RA, Yao M,
Kunos C, Ellis R, Brindle J, Singh D, Hardacre J, Zhang Y, et al:
Stereotactic body radiation therapy for nonresectable tumors of the
pancreas. J Surg Res. 174:319–325. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Cascinu S, Falconi M, Valentini V and
Jelic S: ESMO Guidelines Working Group: Pancreatic cancer: ESMO
Clinical Practice Guidelines for diagnosis, treatment and
follow-up. Ann Oncol. 21(Suppl 5): v55–v58. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Asakura H, Hashimoto T, Harada H, Mizumoto
M, Furutani K, Hasuike N, Matsuoka M, Ono H, Boku N and Nishimura
T: Palliative radiotherapy for bleeding from advanced gastric
cancer: Is a schedule of 30 Gy in 10 fractions adequate? J Cancer
Res Clin Oncol. 137:125–130. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wong AA, Delclos ME, Wolff RA, Evans DB,
Abbruzzese JL, Tamm EP, Xiong HQ, Ho L and Crane CH: Pancreatic
Tumor Study Group: Radiation dose considerations in the palliative
treatment of locally advanced adenocarcinoma of the pancreas. Am J
Clin Oncol. 28:227–233. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Royal RE, Levy C, Turner K, Mathur A,
Hughes M, Kammula US, Sherry RM, Topalian SL, Yang JC, Lowy I, et
al: Phase 2 trial of single agent ipilimumab (anti-CTLA-4) for
locally advanced or metastatic pancreatic adenocarcinoma. J
Immunother. 33:828–833. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Le DT, Lutz E, Uram JN, Sugar EA, Onners
B, Solt S, Zheng L, Diaz LA Jr, Donehower RC, Jaffee EM, et al:
Evaluation of ipilimumab in combination with allogeneic pancreatic
tumor cells transfected with a GM-CSF gene in previously treated
pancreatic cancer. J Immunother. 36:382–389. 2013. View Article : Google Scholar : PubMed/NCBI
|