Introduction
Hepatocellular carcinoma (HCC) is reported to be the
sixth most common malignancy worldwide, affecting 626,000
individuals annually. In terms of mortality rate, HCC is among the
malignancies with the poorest prognosis worldwide, coming third
after lung cancer and gastric cancer (1). HCC has a high rate of recurrence, which
shortens long-term survival, with extrahepatic metastasis known to
develop during the course of the disease (2,3). While
there has been no effective treatment established for advanced HCC
with extrahepatic metastasis (stage IVB), as of 2008, two
placebo-controlled randomized trials have been underway. These
trials have demonstrated the usefulness of the multikinase
inhibitor sorafenib in treating advanced HCC patients with
extrahepatic metastasis (4,5). This has led to the recommendation of the
use of sorafenib as a standard treatment for advanced HCC in Japan
(6,7).
However, while sorafenib prolongs survival, it is insufficient;
therefore, a new agent or combined treatment is required for the
treatment of patients with stage IVB HCC. It is important to
elucidate the clinical characteristics and prognostic factors of
such patients, in order to identify optimal treatment methods. The
usefulness of inflammatory markers, such as the systemic
inflammatory response (SIR), as prognostic factors of cancer has
been recently reported (8). The
usefulness of the neutrophil-to-lymphocyte ratio (NLR) as a
predictive factor following treatment for HCC [transplantation,
resection, radiofrequency ablation (RFA), and transcatheter
arterial chemoembolization (TACE)], has also been reported
(9–13). In general, cancer-related inflammatory
responses affect cellular proliferation, cell survival,
angiogenesis, tumor cell migration, invasion, metastasis and
inhibition of adaptive immunity, indicating that cancer and
inflammation are closely associated (14). Cancer may develop on a background of
inflammation, such as chronic hepatitis, chronic gastritis, chronic
pancreatitis and chronic inflammatory bowel disease. By contrast,
cancer may also activate transcription factors and lead to systemic
or localized inflammation mediated by the main inflammatory
cytokines. Cancer and the inflammatory response have a strong
involvement in their respective reciprocal development (15). An underlying cause of HCC is
continuous infection with the hepatitis virus, i.e., it is strongly
associated with inflammation. Therefore, the measurement of
inflammatory markers should be clinically useful. The aim of the
present study was to investigate the usefulness of the SIR as a
prognostic factor for stage IVB HCC.
Patients and methods
Patient characteristics
Between April, 1997 and March, 2013, a total of 434
patients diagnosed with stage IVB HCC at Kurume University Hospital
were enrolled in the present study. Hepatic functional reserve was
determined using the Child-Pugh classification system and tumor
staging was performed in accordance with the sixth edition of the
American Joint Committee on Cancer/Union for International Cancer
Control tumor-node-metastasis classification (16). The characteristics of the 434 patients
are presented in Table I.
 | Table I.Clinicobiochemical characteristics in
the 434 HCC patients with extrahepatic metastases (n=434). |
Table I.
Clinicobiochemical characteristics in
the 434 HCC patients with extrahepatic metastases (n=434).
| Characteristics | Values |
|---|
| Gender
(male/female) | 363/71 |
| Age, years | 67.0 (15.0–92.0) |
| Eiology
(HCV/HBV/others) | 303/75/56 |
| Child-Pugh class
(A/B/C) | 218/153/63 |
| Albumin, g/dl | 3.3 (2.0–4.8) |
| AST, U/l | 40.0 (7.0–338.0) |
| CRP, mg/dl | 0.50 (0.0–16.58) |
| WBC count,
×109/l | 4.6 (1.4–20.5) |
| Neutrophil
count/µl | 2,916
(522–10,413) |
| Lymphocyte
count/µl | 967 (98–3,749) |
| Platelet count,
×109/l | 111 (31–678) |
| AFP, ng/ml | 622.1
(1.5–3,311,794.0) |
| DCP, mAU/ml | 1285.0
(8.0–75,000.0) |
| Primary tumor
stagea (T0-2/T3/T4) | 60/190/181 |
| Site of extrahepatic
metastasis, n (%) |
|
|
Lungs | 234 (53.9) |
|
Bones | 169 (38.9) |
| Lymph
nodes | 93
(21.4) |
| Adrenal
glands | 44
(10.1) |
The sample comprised 363 male (83.6%) and 71 female
patients, with a median age of 67.0 years (range, 15–92 years). Of
the 434 patients, 303 (69.8%) were positive for hepatitis C virus
and 75 (17.3%) were positive for hepatitis B virus. A total of 218,
153 and 63 patients were Child-Pugh class A, B and C, respectively.
Following initial tumor staging, 60, 190 and 181 patients were
classified as T0-2, T3 and T4, respectively. The sites of
extrahepatic metastasis included the lungs in 234 patients (53.9%),
bone in 169 (38.9%), lymph nodes in 93 (21.4%), adrenal glands in
44 (10.1%), the peritoneum and/or pleura in 31 (7.1%), diaphragm in
21 (4.8%), brain in 1 (2.5%) and other sites in 69 patients
(15.9%). The treatment for stage IVB HCC patients (n=434) included
hepatectomy in 12 (2.8%), percutaneous ethanol injections and RFA
in 8 (1.8%), TACE in 114 (26.3%), hepatic arterial infusion
chemotherapy in 216 (49.8%), systemic chemotherapy in 69 (15.9%),
and radiation therapy in 127 patients (29.3%). A total of 50
patients (11.5%) did not fall under the aforementioned treatments
categories; for these patients, treatment was administered as a
combined multimodal approach, including systematic treatments that
each patient was able to receive continuously.
Blood parameters
Routine laboratory measurements of haemoglobin,
white cell count (WBC), albumin (Alb) and C-reactive protein (CRP)
concentration were performed. The coefficient of variation for
these methods over the range of measurement was <5%, as
established by routine quality control procedures.
NLR-PLR
The value measured on the day of diagnosis was used
for each measurement. The NLR was calculated as the absolute
neutrophil count/absolute lymphocyte count, whereas the PLR was
calculated as the absolute platelet count/absolute lymphocyte
count, and the median value of each was used for the respective
cut-off value. The patients were then divided into two groups and
the overall survival time for each factor was comparatively
examined using Cox proportional hazard analysis. The median values
for the NLR and PLR were 3.02 and 111.37, respectively. Analyses
were performed using the approximate cut-off values of 3 for NLR
and 111 for PLR.
Glasgow prognostic score (GPS)
Based on pretreatment CRP and Alb levels, GPS was
defined as 0 (CRP ≤1.0 mg/dl and Alb ≥3.5 mg/dl), 1 (CRP >1.0
mg/dl and Alb <3.5 g/dl) and 2 (CRP >1.0 mg/dl and Alb
<3.5 mg/dl). Each patient was scored between 0 and 2 and the
patients were divided into two groups, namely GPS 0–1 and 2. The
overall survival times were comparatively examined using the Cox
proportional hazard analysis.
HCC diagnosis and extrahepatic
lesions
HCC was diagnosed based on high signal intensity
images in the hepatic arterial-dominant phase and wash-out images
in the venous and delayed phases by either contrast-enhanced
computed tomography (CT) or magnetic resonance imaging (MRI), which
were then radiographically confirmed. We also measured the serum
concentrations of α-fetoprotein (AFP) and des-gamma-carboxy
prothrombin (DCP). The tumors were biopsied if the imaging findings
were inconsistent with characteristics specific to HCC, or if we
did not observe an elevation in tumor marker levels. Pulmonary
lesions were detected by X-ray or CT of the chest to assess
extrahepatic metastasis. These examinations were conducted
routinely on the first hospital visit and once every 3–6 months
during the follow-up period. Additional examinations, such as bone
scintigraphy and CT or MRI of the brain, were conducted in the
event of symptoms suspicious of extrahepatic metastasis. These
additional examinations were also performed if elevated serum
concentrations of AFP and/or DCP were detected, and the elevation
could not be explained by the status of the intrahepatic lesion.
Positron CT was also performed as a supplementary examination.
Follow-up and endpoints
Each patient was closely followed up, in terms of
monitoring intrahepatic lesions and investigating the presence of
extrahepatic metastasis following HCC diagnosis. Serum biochemical
tests were performed and AFP and DCP levels were measured.
Furthermore, ultrasound examinations were performed once every 1–2
months, contrast-enhanced CT and/or MRI were performed once every
2–6 months, and tests using other diagnostic imaging modalities
were performed as required. The endpoints used in the present study
were the date of death and the date of the final follow-up. The
present study was completed in September, 2013 and the median
follow-up period was 5.7 months (range, 0.2–111.9 months).
Statistical analysis
Continuous variables are expressed as median values
(range). Overall survival was determined by Kaplan-Meier analysis
and differences between subgroups were compared with log-rank
tests. A Cox proportional hazards stepwise model was used for
univariate and multivariate analysis to identify any independent
variables related to overall survival. Data from these models are
expressed as hazard ratios (HR) and 95% confidence intervals (95%
CI). All P-values were two-tailed and values <0.05 were
considered to indicate statistically significant differences.
Statistical analysis was performed by SPSS software, version 20
(IBM SPSS, Armonk, NY, USA).
Results
Overall survival
The overall median survival time (MST) was 7.3
months. The survival rates at 1, 2, 3 and 5 years were 31.8, 14.5,
7.7 and 0.7%, respectively.
Prognosis analysis results
The results of our prognosis analysis are presented
in Table II. As a result of the
univariate analysis, we observed that Child-Pugh class (B+C),
alanine aminotransferase (≥80 U/l), WBC count (≥6,000/l), NLR (≥3),
PLR (≥111), AFP (≥200 ng/ml) and tumor stage (T≥3) were significant
risk factors that were adversely associated with survival. The
multivariate analysis revealed that hepatic functional reserve
(Child-Pugh class B+C; HR=2.055; 95% CI: 1.592–2.651, P<0.001),
T stage (T≥3; HR=2.359; 95% CI: 1.648–3.376, P<0.001), AFP (≥200
ng/ml; HR=1.416; 95% CI: 1.125–1.783, P=0.003), NLR (≥3; HR=1.569;
95% CI: 1.253–1.963, P<0.001) and GPS (1+2; HR=1.410; 95% CI:
1.060–1.874, P=0.018) were independent predictive factors of
survival.
 | Table II.Univariate and multivariate analysis
of survival in all 434 HCC patients with extrahepatic
metastasis. |
Table II.
Univariate and multivariate analysis
of survival in all 434 HCC patients with extrahepatic
metastasis.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Variables | HR (95% CI) | P-value | HR (95% CI) | P-value |
|---|
| Gender (male) | 0.95 (0.71–1.27) | 0.741 |
|
|
| Age (≥65
years) | 1.06
(0.86–1.32) | 0.578 |
|
|
| Etiology (HCV
infection) | 0.97
(0.77–1.22) | 0.807 |
|
|
| Child-Pugh class
(B+C) | 2.76
(2.21–3.44) | <0.001 | 2.03
(1.58–2.60) | <0.001 |
| AST (≥80 U/l) | 1.18
(0.90–1.55) | 0.241 |
|
|
| WBC count
(≥6.0×109/l) | 1.78
(1.41–2.26) | <0.001 |
|
|
| NLR (≥3.0) | 1.96
(1.58–2.43) | <0.001 | 1.46
(1.16–1.85) | 0.002 |
| Platelet count
(≥120×109/l) | 0.94
(0.76–1.17) | 0.579 |
|
|
| PLR (≥111.0) | 1.38
(1.11–1.71) | 0.004 |
|
|
| GPS (≥1) | 2.61
(2.04–3.33) | <0.001 | 1.30
(1.10–1.54) | 0.003 |
| AFP (≥200
ng/ml) | 1.81
(1.45–2.26) | <0.001 | 1.39
(1.10–1.76) | 0.005 |
| DCP (≥200
mAU/ml) | 1.10
(0.99–1.23) | 0.066 |
|
|
| Primary tumor
stagea (≥T3) | 2.88
(2.03–4.10) | <0.001 | 2.25
(1.56–3.23) | <0.001 |
| Site of
extrahepatic metastasis |
|
|
|
|
|
Lungs | 0.92
(0.74–1.14) | 0.440 |
|
|
|
Bones | 1.22
(0.99–1.52) | 0.065 |
|
|
| Lymph
nodes | 0.96
(0.74–1.24) | 0.740 |
|
|
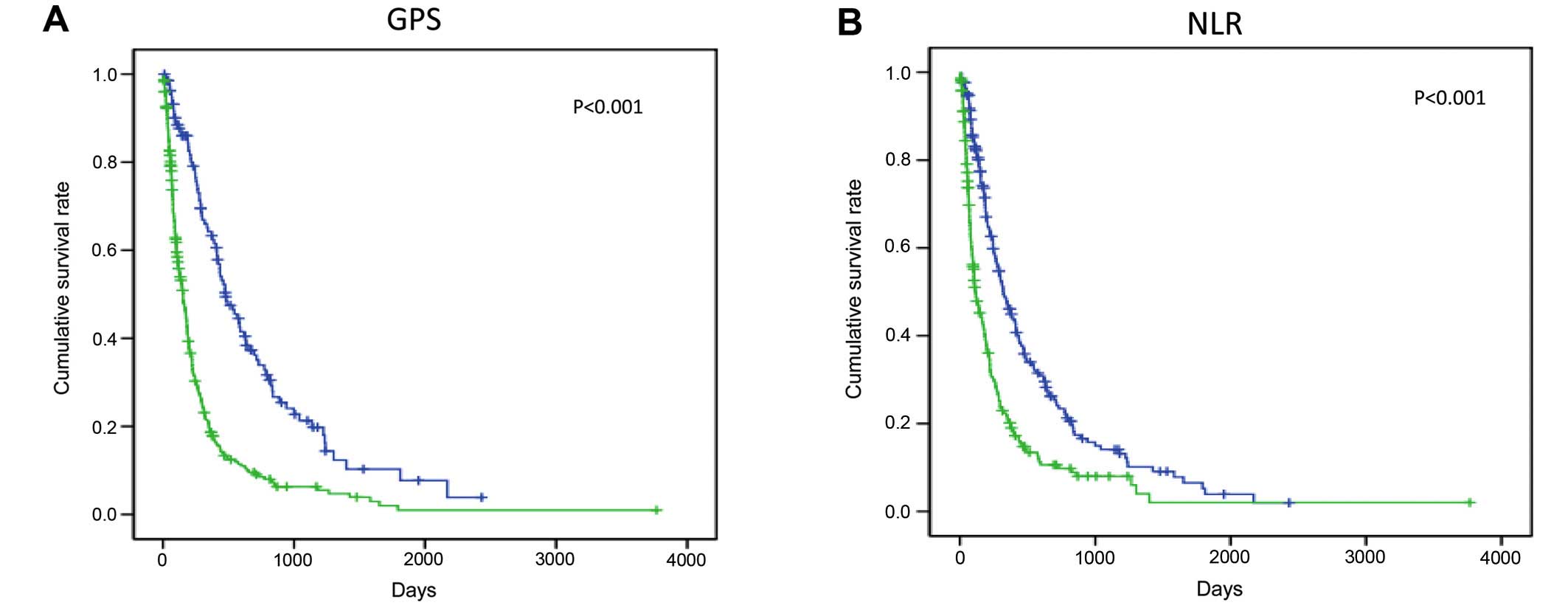
Correlation of GPS and NLR scores with
survival
The cumulative survival curves for GPS and NLR are
shown in Fig. 1. A total of 136
patients were included in the GPS 0 group, 169 in the GPS 1 group
and 129 in the GPS 2 group; the low together with the high NLR
groups included 217 patients. The MST was 480 days in the GPS 0
group, 154 days in the GPS 1 and 2 groups, 115 days in the high NLR
group and 321 days in the low NLR group; a significant difference
in survival was observed for the GPS and NLR groups.
Discussion
As regards clinical characteristics, including main
site of metastasis and survival, our results were similar to those
of previous reports (17–22). The analysis of prognosis revealed that
the degree of intrahepatic tumor progression (T stage), hepatic
functional reserve (Child-Pugh class) and tumor marker levels (AFP)
were all significant prognostic factors, as previously reported
(19,21,22). In
the present study, we observed that, of the SIR indices, GPS and
NLR were useful prognostic factors. It has been reported that
common sites of extrahepatic metastasis that are clinically
characteristic for this stage of HCC in patients aged >50 years
include the lungs (39.5–67.3%), followed by the lymph nodes
(27.9–45.0%) and bone (18.3–35.8%) (17–22). As
regards prognosis, the MST has been reported to be 4.9–8.1 months
(19,20,22)
whereas survival analyses indicate that the state of the
intrahepatic tumor, Child-Pugh class and tumor markers are
independent prognostic factors of survival (19,20,23). The
analysis of stage IVB HCC prognosis indicates that there are more
deaths from intrahepatic events rather than from extrahepatic
events, and the degree of intrahepatic tumor progression is a
significant risk factor (20).
Furthermore, it has been reported that AFP is a marker of tumor
progression (22), and that total
bilirubin, Alb and Child-Pugh class are indices of hepatic
functional reserve (19,22,24).
The present study demonstrated anew that NLR and GPS
are useful prognostic factors in patients with stage IVB HCC. It
has recently been reported that various markers used in the
detection of SIR, such as cytokines, CRP and absolute neutrophil
and lymphocyte counts and their ratios (including NLR), play a
useful prognostic role in cancer. Of those, NLR is one of the
simplest and most effective inflammatory markers, and is associated
with a poor prognosis in various types of cancer (25–27). A
meta-analysis of the usefulness of NLR as a prognostic factor in
HCC was recently published (28). The
results indicated that the NLR cut-off value varied according to
various treatments, such as transplantation, hepatectomy, RFA and
TACE. However, in terms of survival in all treatment groups, a high
NLR was strongly correlated with poor prognosis.
It remains unclear why a high NLR is associated with
poor prognosis. In general, cancer is considered to cause
abnormalities in the differential WBC count via cytokines. A high
NLR is observed when the absolute neutrophil count is high and the
absolute lymphocyte count is low. It has been reported that the
mechanism causing neutrophilia involves a systemic/localized
inflammatory response to a tumor or virus that leads to
microcirculatory changes favorable for cancer progression or
metastasis. It has also been suggested that a high NLR correlates
with the strong invasion and activation of tumor-related
macrophages (TAM) within the tumor, which promotes neutrophilia via
cytokines such as interleukin (IL)-6 and IL-8 (28). It has also been demonstrated that
neutrophils produce matrix metalloproteinase 9, which is involved
in angiogenesis, thus promoting the development of tumors and
chemokines, and vascular endothelial growth factor, thereby
promoting tumor development and metastasis (29–31). In
accordance, an increase in neutrophils leads to an increase in
angiogenic growth factors and precipitates circulatory changes
beneficial for the development of HCC; as a result, it increases
the likelihood of extrahepatic metastasis and decreases HCC patient
survival.
The mechanism underlying the decrease in the
lymphocyte count involves the activation of TAM, which leads to the
release of immunosuppressive cytokines (IL-10 and transforming
growth factor-β) and the decrease in cytotoxic T lymphocytes. The
relative lymphocyte count and T4/T8 ratio tend to decrease,
resulting in a weak inflammatory response via lymphocytes in
patients with a high NLR (32).
At present, a proposed hypothesis for the
aforementioned correlation between high NLR and poor prognosis in
stage IVB HCC patients is that inflammatory markers significantly
promote cytokines associated with the development of advance-staged
cancer. The mechanisms underlying metastasis also involve various
cytokines. It is hypothesized that cytokines are involved in the
progression of the underlying liver disease. Thus, inflammatory
markers, such as NLR, are considered to be useful for advanced
cancer with metastasis that develops on a background of chronic
liver disease.
McMillan (33)
proposed GPS as an index of nutritional status based on CRP and the
Alb-induced inflammatory response. In recent years, the
deterioration of nutritional status and chronic inflammatory
response have been found to be involved in the status and
progression of cancer. Several reports indicate that the GPS is
correlated with treatment outcomes and prognosis of various cancers
when scored on the basis of the Alb level, which is an indicator of
nutritional status, and the inflammatory CRP level (33). The GPS scores are classified in
relation to a CRP level of 1.0 mg/dl and an Alb level of 3.5 g/dl
as follows: CRP ≤1.0 mg/dl with Alb ≥3.5 g/dl is scored as 0 points
(normal); CRP ≤1.0 mg/dl with Alb <3.5 g/dl is scored as 1 point
(malnutrition); CRP >1.0 mg/dl with Alb ≥3.5 g/dl is scored as 1
point (pre-cancer cachexia); and CRP >1.0 mg/dl with Alb <3.5
g/dl is scored as 2 points (cancer cachexia). The higher the GPS
score, the stronger the correlation with poor treatment outcome and
prognosis. It has been reported that this score is strongly
correlated with treatment outcome and prognosis in HCC (33). Cachexia is reported in 20–80% of
cancer patients, and is significantly correlated with the patient's
quality of life and prognosis. This score is even more useful due
to the high incidence of cachexia in gastrointestinal cancer.
In conclusion, we consider the inflammatory markers
GPS and NLR to be useful prognostic factors in patients with stage
IVB HCC. However, while the inflammatory response described herein
may be very useful for simple, low-cost general screening, its
clinical application may be problematic. The inflammatory response
may be biased by infection and stress not asociated with cancer.
Therefore, the establishment of a useful cut-off value in clinical
practice remains a limitation that requires further
investigation.
References
|
1.
|
Parkin DM, Bray F, Ferlay J and Pisani P:
Global cancer statistics, 2002. CA Cancer J Clin. 55:74–108. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Portolani N, Coniglio A, Ghidoni S,
Giovanelli M, Benetti A, Tiberio GA and Giulini SM: Early and late
recurrence after liver resection for hepatocellular carcinoma:
Prognostic and therapeutic implications. Ann Surg. 243:229–235.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Yang Y, Nagano H, Ota H, Morimoto O,
Nakamura M, Wada H, Noda T, Damdinsuren B, Marubashi S, Miyamoto A,
et al: Patterns and clinicopathologic features of extrahepatic
recurrence of hepatocellular carcinoma after curative resection.
Surgery. 141:196–202. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Llovet JM, Ricci S, Mazzaferro V, Hilgard
P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A,
et al: Sorafenib in advanced hepatocellular carcinoma. N Engl J
Med. 359:378–390. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S,
Kim JS, Luo R, Feng J, Ye S, Yang TS, et al: Efficacy and safety of
sorafenib in patients in the Asia-Pacific region with advanced
hepatocellular carcinoma: A phase III randomised, double-blind,
placebo-controlled trial. Lancet Oncol. 10:25–34. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Bruix J and Sherman M: American
Association for the Study of Liver Diseases: Management of
hepatocellular carcinoma: An update. Hepatology. 53:1020–1022.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Kudo M, Izumi N, Kokudo N, Matsui O,
Sakamoto M, Nakashima O, Kojiro M and Makuuchi M: HCC Expert Panel
of Japan Society of Hepatology: Management of hepatocellular
carcinoma in Japan: Consensus-based clinical practice guidelines
proposed by the Japan Society of Hepatology (JSH) 2010 updated
version. Dig Dis. 29:339–364. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Forrest LM, McMillan DC, McArdle CS,
Angerson WJ and Dunlop DJ: Evaluation of cumulative prognostic
scores based on the systemic inflammatory response in patients with
inoperable non-small-cell lung cancer. Br J Cancer. 89:1028–1030.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Gomez D, Farid S, Malik HZ, Young AL,
Toogood GJ, Lodge JP and Prasad KR: Preoperative
neutrophil-to-lymphocyte ratio as a prognostic predictor after
curative resection for hepatocellular carcinoma. World J Surg.
32:1757–1762. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Huang ZL, Luo J, Chen MS, Li JQ and Shi M:
Blood neutrophil-to-lymphocyte ratio predicts survival in patients
with unresectable hepatocellular carcinoma undergoing transarterial
chemoembolization. J Vasc Interv Radiol. 22:702–709. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Halazun KJ, Hardy MA, Rana AA, Woodland DC
IV, Luyten EJ, Mahadev S, Witkowski P, Siegel AB, Brown RS Jr and
Emond JC: Negative impact of neutrophil-lymphocyte ratio on outcome
after liver transplantation for hepatocellular carcinoma. Ann Surg.
250:141–51. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Bertuzzo VR, Cescon M, Ravaioli M, Grazi
GL, Ercolani G, Del Gaudio M, Cucchetti A, D'Errico-Grigioni A,
Golfieri R and Pinna AD: Analysis of factors affecting recurrence
of hepatocellular carcinoma after liver transplantation with a
special focus on inflammation markers. Transplantation.
91:1279–1285. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Dan J, Zhang Y, Peng Z, Huang J, Gao H, Xu
L and Chen M: Postoperative neutrophil-to-lymphocyte ratio change
predicts survival of patients with small hepatocellular carcinoma
undergoing radiofrequency ablation. PLoS One. 8:e581842013.
View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Mantovani A, Allavena P, Sica A and
Balkwill F: Cancer-related inflammation. Nature. 454:436–444. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Trinchieri G: Cancer and inflammation: an
old intuition with rapidly evolving new concepts. Annu Rev Immunol.
30:677–706. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Pawlik TM, Esnaola NF and Vauthey JN:
Surgical treatment of hepatocellular carcinoma: Similar long-term
results despite geographic variations. Liver Transpl. 10(2 Suppl
1): S74–S80. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Yoo DJ, Kim KM, Jin YJ, Shim JH, Ko GY,
Yoon HK, Sung KB, Lee JL, Kang YK, Lim YS, et al: Clinical outcome
of 251 patients with extrahepatic metastasis at initial diagnosis
of HCC: Does transarterial chemoembolization improve survival in
these patients? J Gastroentel Hepatol. 26:145–154. 2011. View Article : Google Scholar
|
|
18.
|
Katyal S, Oliver JH III, Peterson MS,
Ferris JV, Carr BS and Baron RL: Extrahepatic metastases of
hepatocellular carcinoma. Radiology. 216:698–703. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Uka K, Aikata H, Takaki S, Shirakawa H,
Jeong SC, Yamashina K, Hiramatsu A, Kodama H, Takahashi S and
Chayama K: Clinical features and prognosis of patients with
extrahepatic metastases from hepatocellular carcinoma. World J
Gastroenterol. 13:414–420. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Uchino K, Tateishi R, Shiina S, Kanda M,
Masuzaki R, Kondo Y, Goto T, Omata M, Yoshida H and Koike K:
Hepatocellular carcinoma with extrahepatic metastasis: Clinical
features and prognostic factors. Cancer. 117:4475–4483. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Ishii H, Furuse J, Kinoshita T, Konishi M,
Nakagohri T, Takahashi S, Gotohda N, Nakachi K and Yoshino M:
Extrahepatic spread from HCC: Who are candidates for aggressive
anti-cancer treatment? Jpn J Clin Oncolol. 34:733–739. 2004.
View Article : Google Scholar
|
|
22.
|
Natsuizaka M, Omura T, Akaike T, Kuwata Y,
Yamazaki K, Sato T, Karino Y, Toyota J, Suga T and Asaka M:
Clinical features of hepatocellular carcinoma with extrahepatic
metastases. J Gastroenterol Hepatol. 20:1781–1787. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Yoo DJ, Kim KM, Jin YJ, Shim JH, Ko GY,
Yoon HK, Sung KB, Lee JL, Kang YK, Lim YS, et al: Clinical outcome
of 251 patients with extrahepatic metastasis at initial diagnosis
of hepatocellular carcinoma: Does transarterial chemoembolization
improve survival in these patients? J Gastroenterol Hepatol.
26:145–154. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Pawarode A, Voravud N, Sriuranpong V,
Kullavanijaya P and Patt YZ: Natural history of untreated primary
HCC: A retrospective study of 157 patients. Am J Clin Oncol.
21:386–391. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Ding PR, An X, Zhang RX, Fang YJ, Li LR,
Chen G, Wu XJ, Lu ZH, Lin JZ, Kong LH, et al: Elevated preoperative
neutrophil to lymphocyte ratio predicts risk of recurrence
following curative resection for stage IIA colon cancer. Int J
Colorectal Dis. 25:1427–1433. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Jung MR, Park YK, Jeong O, Seon JW, Ryu
SY, Kim DY and Kim YJ: Elevated preoperative neutrophil to
lymphocyte ratio predicts poor survival following resection in late
stage gastric cancer. J Surg Oncol. 104:504–510. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27.
|
Stotz M, Gerger A, Eisner F, Szkandera J,
Loibner H, Ress AL, Kornprat P, AlZoughbi W, Seggewies FS, Lackner
C, et al: Increased neutrophil-lymphocyte ratio is a poor
prognostic factor in patients with primary operable and inoperable
pancreatic cancer. Br J Cancer. 109:416–321. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28.
|
Xiao WK, Chen D, Li SQ, Fu SJ, Peng BG and
Liang LJ: Prognostic significance of neutrophil-lymphocyte ratio in
hepatocellular carcinoma: A meta-analysis. BMC Cancer. 14:1172014.
View Article : Google Scholar : PubMed/NCBI
|
|
29.
|
Coussens LM, Tinkle CL, Hanahan D and Werb
Z: MMP-9 supplied by bone marrow-derived cells contributes to skin
carcinogenesis. Cell. 103:481–490. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
30.
|
Strieter RM, Burdick MD, Mestas J,
Gomperts B, Keane MP and Belperio JA: Cancer CXC chemokine networks
and tumour angiogenesis. Eur J Cancer. 42:768–778. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
31.
|
Gong Y and Koh DR: Neutrophils promote
inflammatory angiogenesis via release of preformed VEGF in an in
vivo corneal model. Cell Tissue Res. 339:437–448. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
32.
|
Chew V, Tow C, Teo M, Wong HL, Chan J,
Gehring A, Loh M, Bolze A, Quek R, Lee VK, et al: Inflammatory
tumour microenvironment is associated with superior survival in
hepatocellular carcinoma patients. J Hepatol. 52:370–379. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
33.
|
McMillan DC: The systemic
inflammation-based Glasgow prognostic score: A decade of experience
in patients with cancer. Cancer Treat Rev. 39:534–540. 2013.
View Article : Google Scholar : PubMed/NCBI
|