Introduction
Medulloblastoma is the most common central nervous
system (CNS) malignancy in children; however, it is extremely
uncommon among adults, comprising only 0.4–1% of CNS neoplasms in
adults. Medulloblastoma is located in the cerebellar hemispheres
and exhibits a male predominance in the adult population. The
majority of affected adults (~63%) are aged 20–40 years, whereas
occurrence in individuals aged >50 years is exceedingly rare
(1). Several adult medulloblastoma
cases have already been reported in China. Lin and Gao (2) have recorded the oldest patient to be
aged 75 years, but lack clinical information regarding complaints,
physical signs, imaging and pathology. To the best of our
knowledge, the case presented herein appears to be the first
complete report on the oldest medulloblastoma case in China. The
aim of this study was to analyze the clinical characteristics,
imaging findings, operative method and pathology, and provide
specific information on adult medulloblastoma for clinicians.
Case report
A 72-year-old woman sought medical attention due to
progressive problems with dizziness over 1 year, particularly when
standing or walking, exhibiting a drunken gait. The severity of the
dizziness increased during the month preceding admission and it was
always present during daily activities. The patient reported
nausea, vomiting and diaphoresis, gradually relieved after resting.
The past medical history included hyperlipidemia. The physical
examination revealed level nystagmus, positive Romberg's sign, and
poor sense of vibration in the left arm compared with the right
when testing with a tuning fork. The remaining cranial nerve,
motor, and sensory examinations were normal. The preoperative
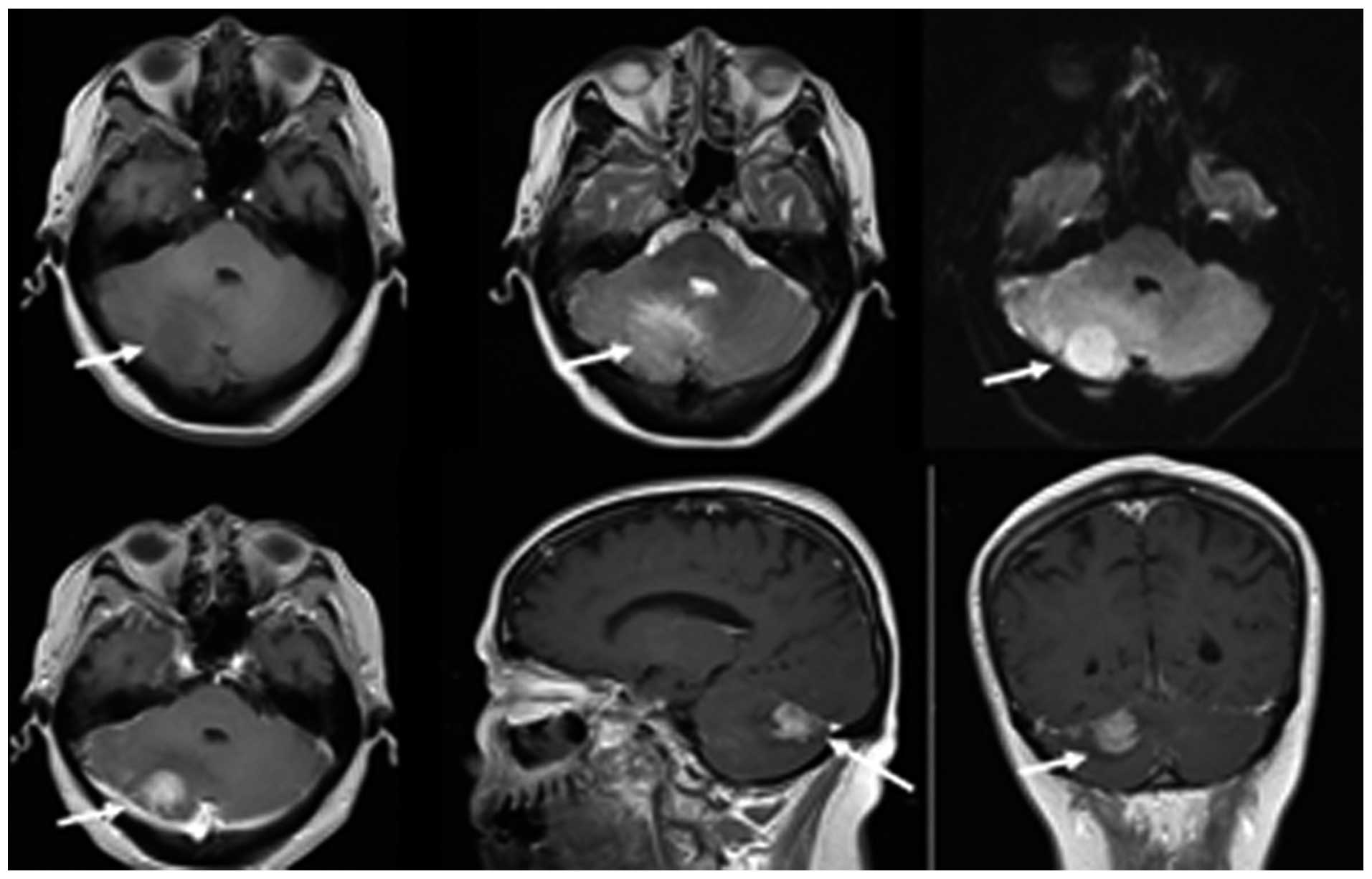
magnetic resonance imaging (MRI) is shown in Fig. 1.
Surgical treatment and outcome
The operation was performed using the suboccipital
midline approach, which included an inverted ‘L’-shaped incision in
the right occipital bone, removing a bone flap sized ~3×3 cm, from
the midline to the transverse sinus.
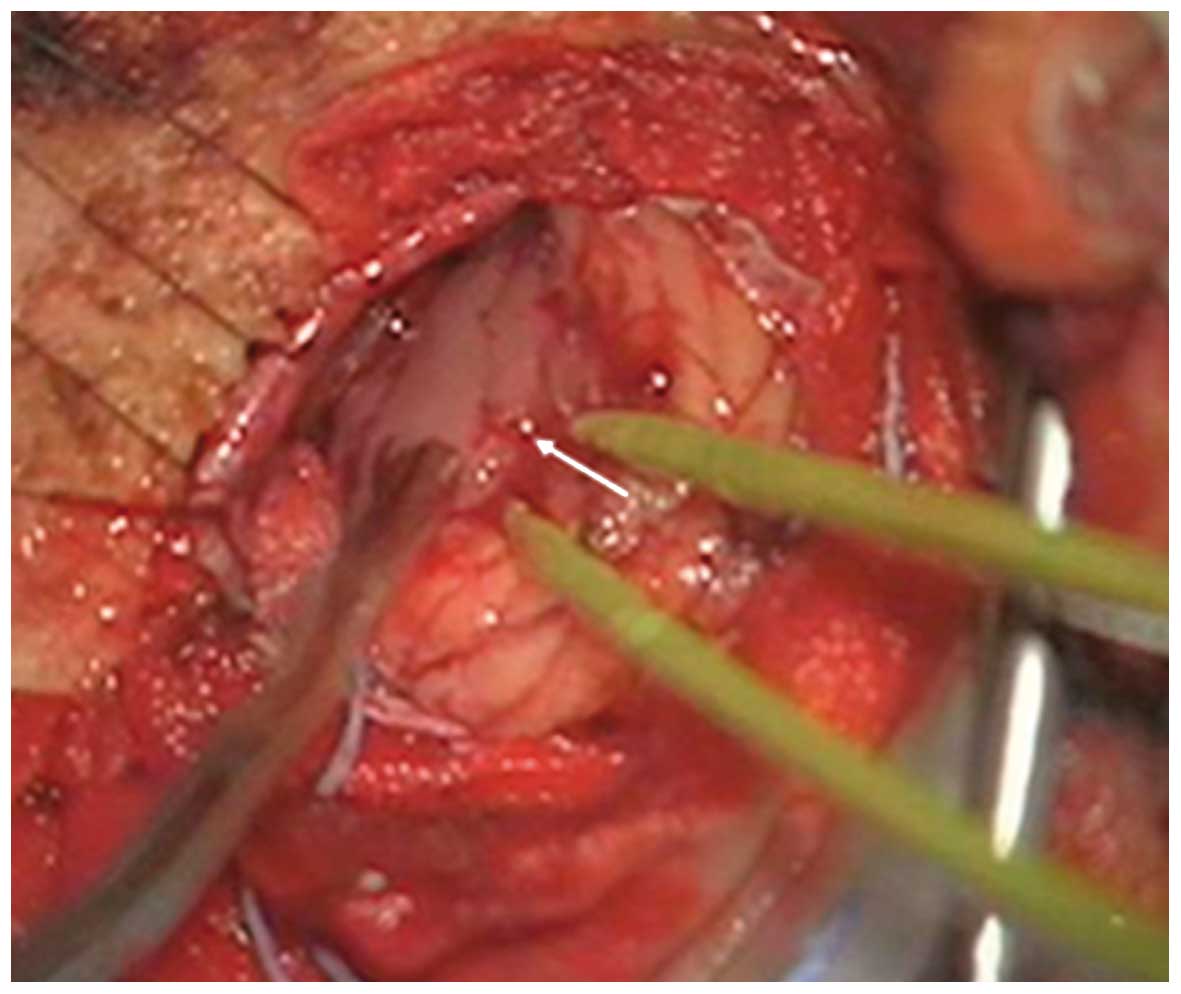
During the operation, the lesion was found to be
located in the inferior border of the tentorium of the cerebellum
and upper surface of the right cerebellar hemisphere (Fig. 2). The boundary between the tentorium
of the cerebellum and cerebellar tissue was clear. The lesion was
sized ~2.4×2.0×2.0 cm, had a soft texture, gray color, and a rich
blood supply.
The computed tomography (CT) scans before and after
the operation are shown in Figs. 3
and 4, respectively.
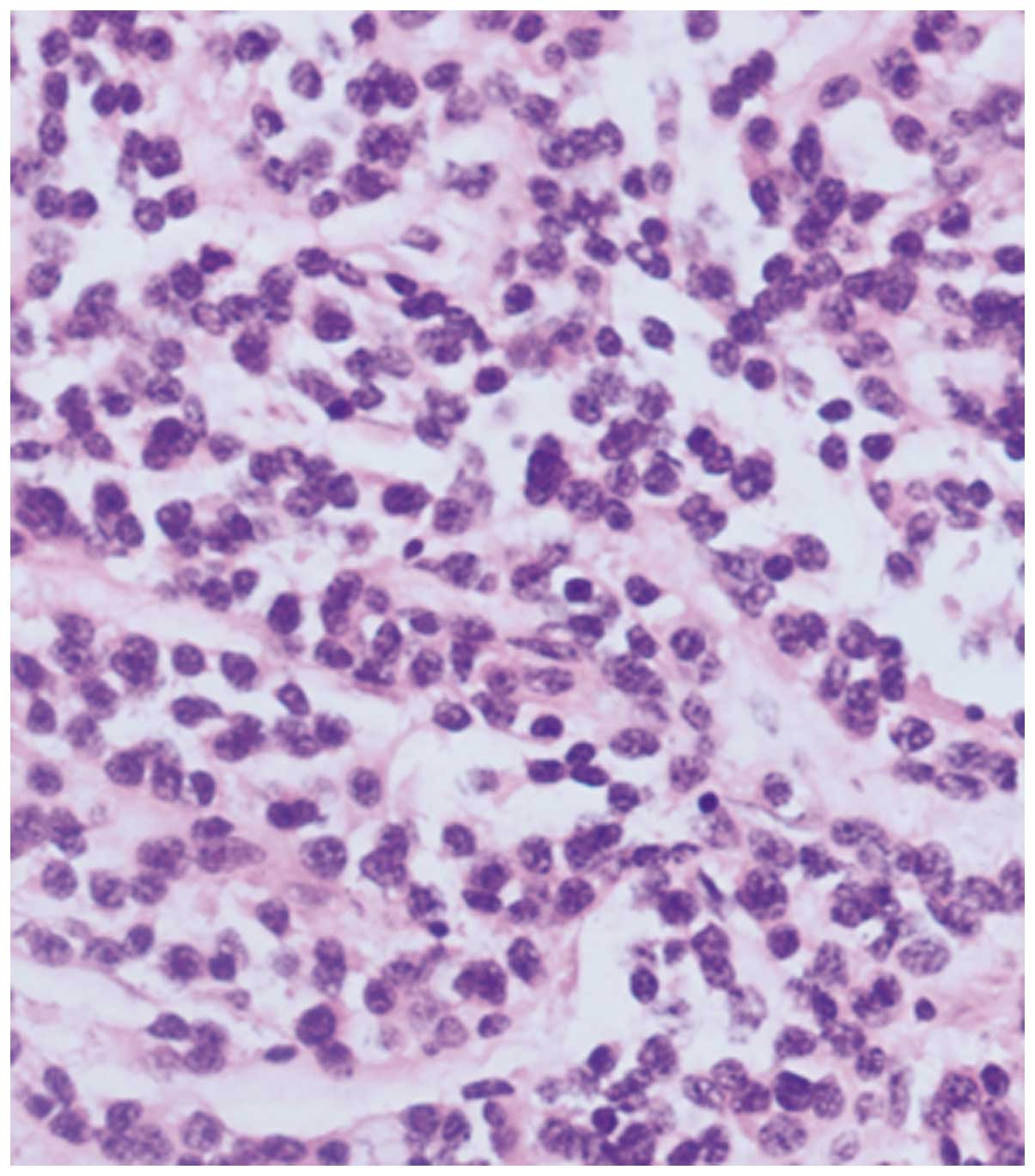
Histological examination
The results of the pathological examination
confirmed the tumor to be a medulloblastoma. The tumor cells were
the classic type, and the structure was nodular. The cell types of
medulloblastoma include 5 types: desmoplastic/nodular
medulloblastoma; medulloblastoma with extensive nodularity;
anaplastic medulloblastoma and large cell medulloblastoma (3).
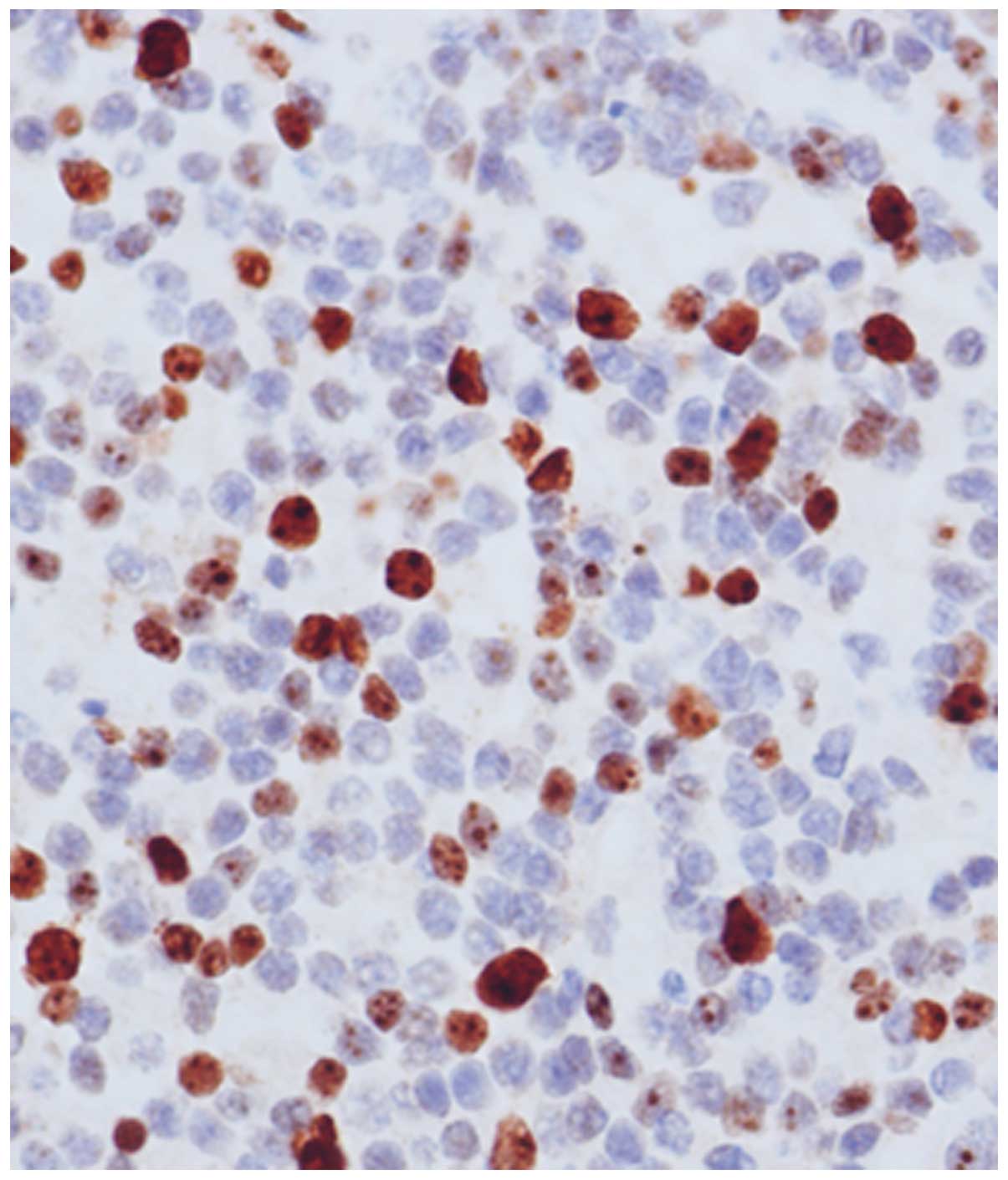
The immunohistochemistry results (Figs. 5 and 6)
were as follows: Cytokeratin (CK) (−), Neuronal Nuclei (+),
oligodendrocyte transcription factor 2 (−), nestin (−), thyroid
transcription factor-1 (−), neurofilament protein (NF) (−), B-cell
lymphoma (Bcl)-6 protein (−), CD20 (−), CD3 (−), CD34 (−), CD56
(+), CD99 (−), CKAE1/3 (−), chromogranin A (+/-), cyclin D1 (−),
glial fibrillary acidic protein (−/+), Ki-67 (+; >30%), multiple
myeloma oncogene 1 (−), neuron-specific enolase (+), S-100 (−),
synaptophysin (+), Bcl-2 (+), vimentin (−) and reticular fiber
antibody (−). Based on the microscopic findings, the
medulloblastoma was classified as grade IV according to the WHO
classification (3).
Therapeutic method
The patient's condition significantly improved after
the operation. The patient was treated with radiotherapy of the
posterior cranial fossa, the whole brain and the spinal cord (the
whole-brain and spinal cord dose was 26–36 Gy, whereas the dose to
the posterior cranial fossa without the brain stem was 50–60 Gy.
The patient is currently followed up by mail or telephonical
communication.
Discussion
Medulloblastoma is a CNS malignancy originating from
the neuroepidermal layer of the cerebellum, first presented by
Cushing and Bailey in 1925. This malignancy is the most common CNS
tumor in children, and is commonly located in the fourth ventricle,
cerebellum and vermis. However, only 9 cases of medulloblastoma in
adults (aged >65 years) have been reported outside China
(4), with an onset between 65 and 88
years (mean age, 77.8 years); 7 cases (77.8%) occurred in the
cerebellar hemisphere and 2 cases (22.2%) in the cerebellar vermis.
One case (11.1%) was located in the fourth ventricle, whereas the
cerebellar hemisphere was the most common location in elderly
patients. Our findings were similar to those of previous cases
regarding the onset and location of adult medulloblastoma. Koeller
and Rushing (1) described
undifferentiated cells in the posterior medullary vellum that are
close to the midline early in life, but exhbit lateral and superior
lateral migration with aging. Gupta et al (5) reported that adult medulloblastoma
originates in a primordium of the granule cell layer of the
cerebellum, which is located on the surface of submeningian
molecular layer, and its cells disappear gradually within 18 months
after birth. This theory of biological origin may explain the
predilection site at the dorsal surface of the cerebellar
hemisphere in adults. Thus, medulloblastoma should be taken into
account in parenchymatous tumors of the cerebellar hemispheres.
The main clinical manifestations of medulloblastoma
are increased intracranial pressure and cerebellar ataxia. If the
nuclei of the brain stem become damaged, the patients present with
gait disturbance, diplopia and anesthesia. If the tumor involves
the fourth ventricle, it may cause obstructive hydrocephalus. The
clinical symptoms were not severe in our patient, which was related
to the location of the tumor.
The imaging characteristics of adult cerebellar
medulloblastoma are closely associated with the tentorium of the
cerebellum or meninges. The CT images showed isodensity or
marginally high density, on a background of edema, with a clear
boundary. MRI imaging revealed mildly long T1 and T2, with a clear
boundary, which may be associated with the cellular composition of
the tumor (6). However, through
careful observation, particularly after enhancement, all levels and
various angles of observation revealed a difficulty in
differentiating between the tumor and the cerebellar parenchyma
(7). Due to the lack of knowledge of
non-cerebellar vermis medulloblastoma, the misdiagnosis rate is
high. Our patient was initially misdiagnosed with meningioma,
vascular tumor and metastasis.
The origin, pathological subtype, clinical treatment
and prognosis of adult medulloblastoma patients differ compared
with those in children; in adults, the postoperative 5-year
survival rate was ~64.9–81.0% and the postoperative 10-year
survival rate ~52.0–62.0%, with a median survival time of 8.1–17.7
years (8). Some studies report that
older medulloblastoma patients may have a better prognosis
(9). With the aging of the general
population, there may be more similar cases reported in the
future.
Acknowledgements
The present study is supported by the hospital
department of internal medicine research foundation (DTQH201403)
from Beijing Ditan Hospital, Capital Medical University.
References
|
1
|
Koeller KK and Rushing EJ: From the
archives of the AFIP: Medulloblastoma: A comprehensive review with
radiologic-pathologic correlation. Radiographics. 23:1631–1637.
2003. View Article : Google Scholar
|
|
2
|
Lin Y and Gao PY: CT and MR imaging of
medulloblastomas in adults. China JMI T. 16:96–98. 2000.
|
|
3
|
Louis DN, Ohgaki H, Wiestler OD, et al:
The 2007 WHO Classification of Tumours of the Central Nervous
System. Acta Neuropathol. 114:97–109. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Huppmann AR, Orenstein JM and Jones RV:
Cerebellar medulloblastoma in the elderly. Ann Diagn Pathol.
13:55–59. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gupta A and Kasliwal MK: Unusual MR
features of adult cerebellar medulloblastoma. J Neurooncol.
78:47–48. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rasalkar DD, Chu WC, Shing MK and Li CK:
Medulloblastoma with leptomeningeal metastases. Hong Kong Med J.
17:340–341. 2011.PubMed/NCBI
|
|
7
|
Qiong Wang, Peiyi Gao, Yan Lin and
Shengjun Sun: CT and MR imaging of characteristtics of
non-cerebellar-vermis medulloblastomas. Radiol Practice.
27:1058–1060. 2012.
|
|
8
|
Fu Zhao, Peiran Qu and Jing Zhang: The
analysis of clinical treatment and prognostic factors of adult
medulloblastoma. Chin J Neurol. 46:470–473. 2013.
|
|
9
|
Lu YC, Jia W, et al: Analysis of surgical
treatment and prognostic factors of adult medulloblastoma. Chin J
Neurosurg. 30:76–78. 2014.
|