Introduction
Pelvic lymph node dissection (PLND) represents the
most accurate and reliable staging procedure for the detection of
lymph node invasion in prostate cancer (1). For PLND in radical prostatectomy (RP),
its adaptation, significance and dissection range have been
previously discussed (2). The
European Association of Urology (EAU) and National Comprehensive
Cancer Network (NCCN) guidelines recommend determining the
adaptation of PLND using nomograms to predict the risk of
preoperative lymph node metastases when performing PLND, and
extended PLND is considered desirable if cases are evaluated as an
adaptation of PLND (1,3). However, to date, no consensus has been
reached. Therefore, to assess the association between the range of
PLND and prostate specific antigen (PSA) failure, a retrospective
investigation was conducted using the clinicopathological data of
patients who underwent RP, but had not received preoperative
treatment.
Materials and methods
Patient characteristics and risk-group
classification
Between August 1998 and May 2013, 638 consecutive
patients with clinically localized prostate cancer underwent RP at
the National Kyushu Cancer Center (Fukuoka, Japan) and were
reviewed. RP was performed in an open retropubic manner in all
cases. In total, 171 patients were excluded from this study,
including 151 patients due to a past history of receiving hormone
therapy, 14 patients due to no PLND being performed and 6 patients
due to unclear biopsy or prostatectomy specimen findings. The
patients were classified into three risk groups according to the
D'Amico criteria (4). Two
pathologists evaluated the degree of malignancy in the biopsy and
prostatectomy specimens according to the 2005 International Society
of Urological Pathology Consensus Conference on Gleason grading
system and determined the pathological stage based on the 2009
Tumor-Node-Metastasis classification (5,6).
PLND technique
All patients underwent standard PLND as a minimum,
which was performed along the lower edge of the external iliac
vein, the caudal limit being the deep circumflex iliac vein and
femoral canal, preserving the lymphatics overlying the external
iliac artery. The proximal border was bifurcation of the common
iliac artery, and all tissue in the angle between the external and
internal iliac arteries and obturator nerve was removed. All fatty,
connective and lymphatic tissue of the obturator fossa along the
obturator muscle was removed, leaving the obturator nerve and
vessels bare. Subsequently, the internal iliac artery and, as far
as possible, the internal iliac vein were skeletonized up to the
obturator arteriovenous branch section. The patients were
subdivided into two subgroups according to the lymph node
dissection technique: Standard PLND and expanded (extended + more
extended) PLND. The technique for extended PLND included the
technique for standard PLND as well as the lymphatics overlying the
external iliac artery and vein, until reaching the genitofemoral
nerve laterally. More extended PLND included the technique of
extended PLND as well as the lymphatics overlying the common iliac
artery up to the ureteric crossing cranially.
Tissue processing and PSA level
determination
The RP specimens were fixed in 15% neutral buffered
formalin (Wako Pure Chemical Industries, Ltd., Osaka, Japan) for
48–96 h at room temperature, and whole organ prostate specimens
were serially sectioned perpendicular to the rectal surface at 5 mm
intervals. Sections that were predominantly caudal and cephalic
were cut in the sagittal plane at 5 mm intervals in order to assess
the bladder neck and apical margins. The specimens were
subsequently embedded in paraffin, cut into 5 µm sections and
stained with hematoxylin and eosin. Extraprostatic extension was
defined as the extension of the tumor from the prostate to the
periprostatic soft tissue. The presence of tumor cells at the
stained resection margin was defined as a positive resection
margin. The follow-up schedule after RP involved a PSA assay
performed every 3 months for the first 2 years, followed by every 4
months for the next 3 years and every 6 months thereafter. Disease
recurrence or PSA failure was determined as the time point when the
serum PSA level was >0.2 ng/ml, and RP was performed if the PSA
level did not decrease below 0.2 ng/ml following surgery. A number
of patients who underwent RP were subsequently treated with
radiation and/or hormone therapy prior to the serum PSA level
exceeding 0.2 ng/ml. Therefore, in these patients, the time point
of adjuvant therapy was defined as the date of disease recurrence.
All patients provided their written informed consent to participate
in this study, and the study protocol was approved by the Ethics
Committee of the National Kyushu Cancer Center (Fukuoka,
Japan).
Statistical analysis
Statistical analyses were performed using the
JMP® Pro, version 11.0.0 software package (SAS
Institute, Inc., Cary, NC, USA). The PSA failure-free rate was
determined according to the Kaplan-Meier method, and the
significance of clinicopathological parameters associated with PSA
failure was assessed using the Cox proportional hazards regression
model. The χ2 test and Mann-Whitney U test was used to assess the
differences between standard PLND and expanded PLND. P<0.05 was
considered to indicate a statistically significant difference.
Results
Clinicopathological
characteristics
The clinicopathological characteristics according to
the PLND technique used are presented in Table I. All patients were Japanese (median
age, 66 years; range, 47–77), and the PSA levels ranged between
0.623 and 39.413 ng/ml (median, 7.486 ng/ml; normal range <4.0
ng/ml). The median follow-up period after surgery was 53.8 months.
According to the PLND technique used, the standard PLND group and
the expanded group contained 301 (64.5%) and 166 (35.5%) patients,
respectively. No differences were observed in the preoperative
characteristics, including age, preoperative PSA, clinical tumor
stage and biopsy Gleason score, between the groups (Table I). There were also no differences in
postoperative characteristics, such as pathological tumor stage,
final Gleason score, extraprostatic extension, resection margin,
seminal vesicle invasion and lymph node metastasis between the
groups. In addition, there was no significant difference in PSA
recurrence between the two groups. Furthermore, lymph node
metastasis was not observed in any patient in the low-risk group,
but was detected in 5 patients in the intermediate-risk group and 8
patients in the high-risk group.
 | Table I.Clinicopathological characteristics of
patients. |
Table I.
Clinicopathological characteristics of
patients.
|
| Extent of PLND |
|---|
|
|
|
|---|
|
|
|
|
| Expanded |
|---|
|
|
|
|
|
|
|---|
| Characteristic | Standarda,n (%) | Expandedb,n (%) | P-value | Extended(standard +
external iliac) | More
extended(standard + external and common iliac) |
|---|
| Total no. of
patients | 301 (64.5) | 166 (35.5) |
| 125 | 41 |
| Age, years |
|
|
|
|
|
|
<70 | 210 (69.8) | 112 (67.5) | 0.6082 | 90 (72.0) | 22 (53.7) |
| ≥70 | 91 (30.2) | 54 (32.5) |
| 35 (28.0) | 19 (46.3) |
| Preoperative PSA,
ng/ml |
|
|
|
|
|
| ≤10 | 222 (73.8) | 111 (66.9) | 0.1157 | 84 (67.2) | 27 (65.9) |
|
>10 | 79 (26.2) | 55 (33.1) |
| 41 (32.8) | 14 (34.1) |
| Clinical T stage |
|
|
|
|
|
| cT1c | 195 (64.8) | 121 (72.9) | 0.0708 | 92 (73.6) | 29 (70.7) |
|
≥cT2a | 106 (35.2) | 45 (27.1) |
| 33 (26.4) | 12 (29.3) |
| Biopsy Gleason
score |
|
|
|
|
|
| ≤7 | 222 (73.8) | 131 (78.9) | 0.2146 | 98 (78.4) | 33 (80.5) |
|
>8 | 79 (26.2) | 35 (21.1) |
| 27 (21.6) | 8 (19.5) |
| Pathological T
stage |
|
|
|
|
|
| ≤pT2 | 186 (61.8) | 107 (64.5) | 0.5682 | 77 (61.6) | 30 (73.2) |
| ≥pT3 | 115 (38.2) | 59 (35.5) |
| 48 (38.4) | 11 (26.8) |
| Final Gleason
score |
|
|
|
|
|
| ≤7 | 239 (79.4) | 125 (72.3) | 0.3068 | 95 (76.0) | 30 (73.2) |
|
>8 | 62 (20.6) | 41 (27.7) |
| 30 (24.0) | 11 (26.8) |
| Extraprostatic
extension |
|
|
|
|
|
|
Negative | 208 (69.1) | 116 (69.9) | 0.8622 | 86 (68.8) | 30 (73.2) |
|
Positive | 93 (30.9) | 50 (30.1) |
| 39 (31.2) | 11 (26.8) |
| Resection margin |
|
|
|
|
|
|
Negative | 239 (79.4) | 140 (84.3) | 0.1868 | 103 (82.4) | 37 (90.2) |
|
Positive | 62 (20.6) | 26 (15.7) |
| 22 (17.6) | 4 (9.8) |
| Seminal vesicle
invasion |
|
|
|
|
|
|
Negative | 281 (93.4) | 159 (95.8) | 0.2707 | 118 (94.4) | 41 (100) |
|
Positive | 20 (6.6) | 7 (4.2) |
| 7 (5.6) | 0 |
| Lymph node
metastasis |
|
|
|
|
|
|
Negative | 294 (97.7) | 160 (96.4) | 0.4257 | 120 (96.0) | 40 (97.6) |
|
Positive | 7 (2.3) | 6 (3.6) |
| 5 (4.0) | 1 (2.4) |
| PSA
recurrence | 46 (15.3) | 22 (13.3) | 0.5526 | 18 (14.4) | 4 (9.8) |
Association between the lymph node
dissection number and lymph node metastasis for each PLND
technique
In total, 301 patients (64.5%) underwent standard
PLND and 166 patients (35.5%) underwent expanded PLND (Table II). The median number of dissected
lymph nodes was 13 and 19, respectively, and there was a
significant difference between the standard PLND and expanded PLND
groups (P<0.0001; Table II).
Lymph node metastasis was observed in 7 patients (2.3%) in the
standard PLND group and 6 patients (3.6%) in the expanded PLND
group. With regard to the number of lymph node metastases and the
rate of lymph node metastasis, no significant difference was
observed between the standard PLND and expanded PLND groups
(P=0.4219 and P=0.4257, respectively).
 | Table II.The association between the lymph
node dissection number and lymph node metastasis in the each
technique of PLND. |
Table II.
The association between the lymph
node dissection number and lymph node metastasis in the each
technique of PLND.
|
| Extent of PLND |
|---|
|
|
|
|---|
|
|
|
|
| Expanded |
|---|
|
|
|
|
|
|
|---|
| Characteristic |
Standarda |
Expandedb | P-value | Extended(standard +
external iliac) | More
extended(standard + external and common iliac) |
|---|
| Total no. of
patients, n (%) | 301 (64.5) | 166 (35.5) | – | 125 | 41 |
| Lymph node
metastasis, n (%) |
|
| 0.4257 |
|
Negative | 294 (97.7) | 160 (96.4) |
| 120 (96.0) | 40 (97.6) |
|
Positive | 7 (2.3) | 6 (3.6) |
| 5 (4.0) | 1 (2.4) |
| Total no. of
dissected nodes, | 13 (0–31) | 19 (5–40) | <0.0001 | 19 (5–40) | 19 (12–35) |
| median (range) |
| Upper
obturator | 11 (0–29) | 8 (2–22) | – | 9 (2–22) | 8 (2–18) |
| Lower
obturator + internal iliac | 3 (0–14) | 2 (0–16) |
| 2 (0–11) | 1 (0–16) |
|
External iliac | – | 7 (0–21) |
| 7 (0–21) | 8 (0–16) |
| Common
iliac | – | 0 (0–8) |
| – | 2 (0–8) |
| Total no. of
positive nodes, | 0 (0–5) | 0 (0–5) | 0.4219 | 0 (0–5) | 0 (0–1) |
| median (range) |
| Upper
obturator | 0 (0–4) | 0 (0–1) | – | 0 (0–1) | 0 |
| Lower
obturator + internal iliac | 0 (0–1) | 0 (0–2) |
| 0 (0–2) | 0 |
|
External iliac | – | 0 (0–2) |
| 0 (0–2) | 0 (0–1) |
| Common
iliac | – | 0 (0) |
| – | 0 |
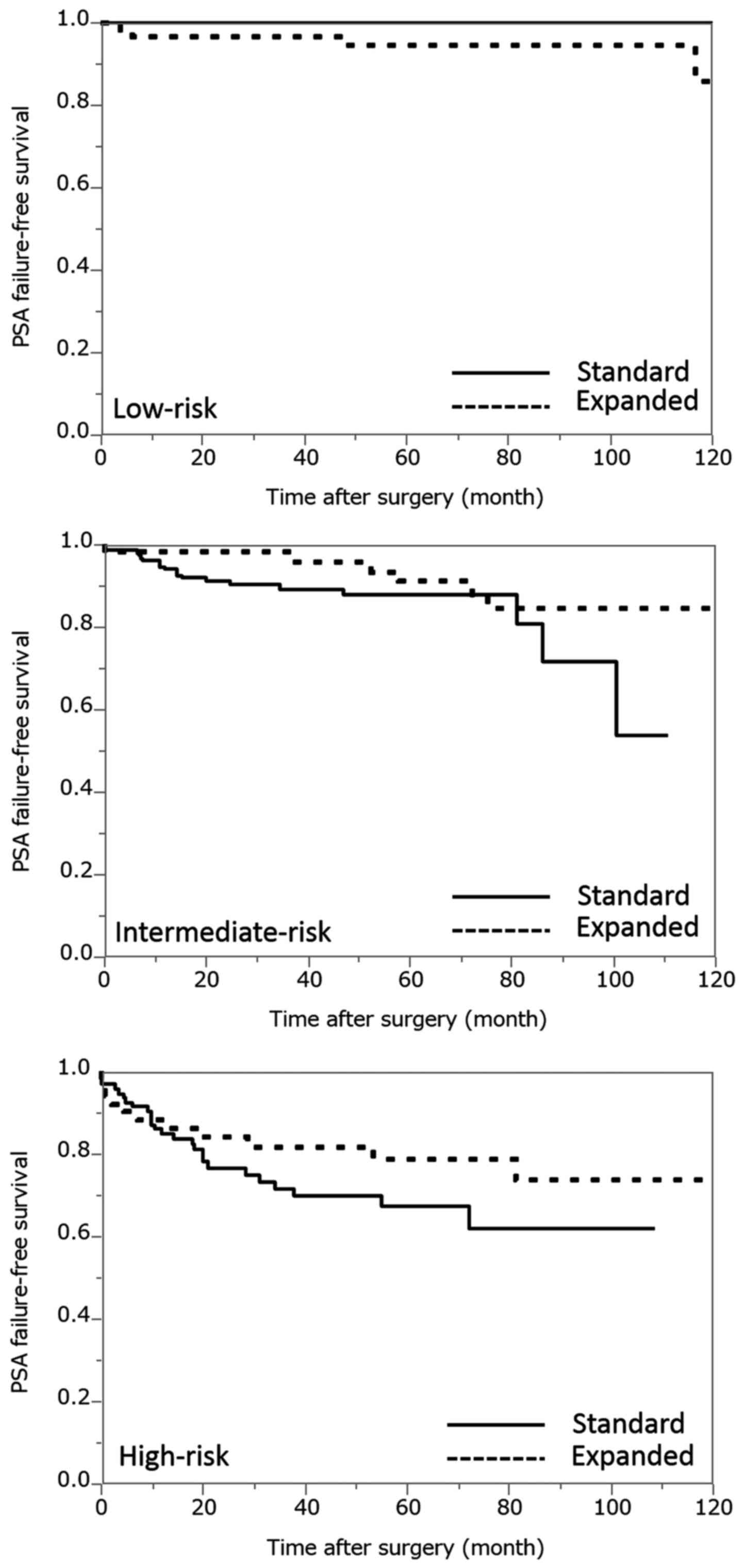
PSA failure-free survival rate of each
dissection template according to risk group classification
According to the D'Amico criteria, 47 (15.6%), 157
(52.2%) and 97 (32.2%) of the patients in the standard PLND group,
and 58 (34.9%), 56 (33.7) and 52 (31.4) patients in the expanded
PLND group were classified into the low-, intermediate- and
high-risk groups, respectively. In the low-risk groups, the 5-year
PSA failure-free rates in the standard and expanded PLND groups
were 100 and 94.4%, respectively (Fig.
1). In the intermediate-risk groups, the 5-year PSA
failure-free rates in the standard and expanded PLND groups were
88.1 and 91.1%, respectively (Fig.
1). In the high-risk groups, the 5-year PSA failure-free rates
in the standard and expanded PLND groups were 67.6 and 78.9%,
respectively (Fig. 1). There was no
significant difference in the frequency of patients in the low-,
intermediate- and high-risk groups between the standard and
expanded PLND categories (P=0.1456, P=0.1581 and P=0.2125,
respectively).
Association between patient
characteristics and PSA failure
According to the Cox proportional hazards analysis,
all characteristics without a preoperative variable, such as age,
were significant predictors based on the univariate analysis
(Table III). In the multivariate
analysis, significant differences were identified in the
preoperative characteristics, including preoperative PSA, biopsy
Gleason score and clinical tumor stage, and in the postoperative
characteristics, such as pathological tumor stage, resection margin
positive and lymph node metastasis, between the patients with and
without PSA failure (Table III). A
significant difference in PSA failure between the PLND techniques
was only observed in the univariate analysis (P=0.0312); no
significant differences were detected in the multivariate analysis
(P=0.0655).
 | Table III.Association between patient
characteristics and PSA failure. |
Table III.
Association between patient
characteristics and PSA failure.
|
Characteristics | Hazard ratio | 95% confidence
interval | P-value |
|---|
| Univariate
analysis |
|
|
|
| Age
<70 vs. ≥70 years | 1.261 | 0.759–2.759 | 0.3624 |
|
Preoperative PSA ≤10 vs.
>10 | 3.134 | 1.936–5.936 | <0.0001 |
|
Clinical T stage, cT1c vs.
≥T2a | 3.270 | 2.023–5.023 | <0.0001 |
| Biopsy
Gleason score ≤7 vs. >8 | 3.658 | 2.257–5.257 | <0.0001 |
|
Pathological T stage, ≤ pT2
vs. ≥pT3 | 5.944 | 3.516–10.516 | <0.0001 |
| Final
Gleason score ≤7 vs. >8 | 3.621 | 2.242–5.242 | <0.0001 |
|
Extraprostatic extension | 3.822 | 2.361–6.361 | <0.0001 |
|
Resection margin | 3.159 | 1.908–5.908 | <0.0001 |
| Seminal
vesicle invasion | 5.179 | 2.636–9.636 | <0.0001 |
| Lymph
node metastasis | 5.792 | 1.995–13.995 | 0.0029 |
| Range
of PLND, standard vs. expanded | 0.563 | 0.323–0.323 | 0.0312 |
| Multivariate
analysis |
|
|
|
|
Preoperative PSA ≤10 vs.
>10 | 1.874 | 1.124–3.124 | 0.0162 |
|
Clinical T stage, cT1c vs.
≥cT2a | 2.780 | 1.686–4.686 | <0.0001 |
| Biopsy
Gleason score ≤7 vs. >8 | 2.399 | 1.454–3.454 | 0.0007 |
|
Pathological T stage, ≤pT2 vs.
≥pT3 | 3.038 | 1.648–5.648 | 0.0003 |
|
Resection margin | 1.877 | 1.068–3.068 | 0.0289 |
| Lymph
node metastasis | 3.547 | 1.202–8.202 | 0.0247 |
Discussion
In patients undergoing RP for prostate cancer, PLND
is the most accurate and reliable lymph node staging procedure, as
imaging techniques have be demonstrated to be insufficient
(7–9). However, to date, no consensus has been
reached regarding the extent of PLND required to achieve optimal
lymph node staging. Previous studies have argued that the extent of
PLND may be directly correlated with a higher rate of pN1 stage
cases (10,11). Conversely, another study reported no
difference in the rate of pN1 stage cases between patients who
received limited and extended PLND (12). Thus, the extent of PLND has varied by
era, institution and individual urologist due to the lack of
consensus regarding its anatomical extension. In recent years,
standard PLND, which is similar (but not identical) to extended
PLND in the NCCN guidelines, has been performed at the National
Kyushu Cancer Center. When RP was initially performed at this
institution, all cases underwent more extended PLND, which includes
the common iliac, external, obturator and internal lymph nodes, as
there was no consensus among the urologic surgeons with regard to
the extent of PLND, and performing PLND with an increased range may
allow for the surgical resection of microscopic lymph node
metastases. However, even including cases receiving preoperative
hormone therapy, the proportion of lymph node metastasis and PSA
recurrence rate following RP at the National Kyushu Cancer Center
institution were lower compared with previous studies (13,14).
Therefore, the range of lymph node dissection was gradually reduced
to extended PLND, and finally standard PLND, regardless of the
D'Amico risk classification, as more RP procedures were performed.
A survival advantage with more extensive lymphadenectomy has been
suggested by several studies, potentially due to the elimination of
microscopic metastases (15–18). The purpose of the current study was
to evaluate the adequate PLND technique for prostate cancer in RP.
Compared with a multicenter study, the advantage of this single
institutional study is that all of the operations were performed by
or under the supervision of urological surgeons who performed
standardized surgery, resulting in negligible differences in the
dissection of area and methods.
As presented in Table
I, the patients were classified into two groups according to
the range of PLND: Standard PLND (obturator + internal iliac) and
expanded PLND (standard + additional nodes) groups, accounting for
64.5 (301/467) and 35.5% (166/467) of the patients, respectively.
No differences were observed in the preoperative and postoperative
characteristics. In addition, there was no difference in PSA
recurrence between the two groups. The range of extended PLND
differs according to the guidelines used. According to the NCCN
guidelines, extended PLND includes the removal of all node-bearing
tissue from the area bounded by the external iliac vein
anteriority, the pelvic side wall laterally, the bladder wall
medially, the floor of the pelvic posteriorly, Cooper's ligament
distally and the internal iliac artery proximally (3). On the other hand, according to the EAU
guidelines, extended PLND includes the removal of the nodes
overlying the external iliac artery and vein, the nodes within the
obturator fossa located cranially and caudally to the obturator
nerve and the nodes medial and lateral to the internal iliac artery
(1). The major difference between
these guidelines is the range of extended PLND, that is, whether
the nodes overlying the external iliac artery were resected. At the
National Kyushu Cancer Center, the standard PLND range is similar
(but not identical) to the extended PLND range in the NCCN
guidelines, as it was performed along the lower edge of the
external iliac vein, so that the nodes overlying the external iliac
vein were not resected. The correlation between the lymph node
dissection number and lymph node metastasis number was examined for
each technique of PLND (Table II).
By decreasing the dissected area from expanded PLND to standard
PLND, the number of dissected lymph nodes decreased significantly
(P<0.0001). However, with regard to the number of lymph node
metastases and the rate of patients with lymph node metastasis, no
significant difference was observed between the standard PLND and
expanded PLND groups (P=0.4219 and P=0.4257, respectively). A
greater number of lymph nodes are able to be dissected when the
dissection extent is increased; however, the expansion of the
dissection range was not associated with the number or rate of
positive lymph nodes detected. According to these results, the
present study hypothesizes that there is no need to expand the
dissection range further than the standard technique of PLND at the
National Kyushu Cancer Center.
The present study subsequently examined the PSA
failure-free survival rates of each dissection technique according
to each risk group classification (Fig.
1). In the intermediate- and high-risk groups, the 5-year PSA
failure-free rates for standard PLND were lower than that of
expanded PLND. The risk of lymph node metastasis among the patients
in the low-risk group was minimal (1,19). Thus,
the therapeutic role of PLND remains unclear and these guidelines
indicate that extended PLND may only be recommended for
intermediate-, high-risk or highly suspicious patients. However,
the results of the present study revealed that there was no
significant difference in the outcomes after standard and expanded
PLND, not only in the low-risk group but also in the intermediate-
and high-risk groups (P=0.1456, P=0.1581, P=0.2125, respectively).
According to these results, the current study speculates that it is
not necessary to expand the dissection range further than the
standard technique of PLND at the National Kyushu Cancer Center,
even in intermediate- and high-risk patients.
The correlation between patient characteristics and
PSA failure were next examined in the RP cases (Table III). First, all factors excluding
age were determined to affect PSA recurrence in the univariate
analysis. Ultimately, PSA, cT and biopsy Gleason score were factors
used in risk classification, and pT, resection margin and lymph
node metastasis were factors affecting PSA recurrence in the
multivariate analysis. Lymph node metastasis was a significant
factor, however, the dissection range was not according to the
multivariate analysis (P=0.0655).
In the current study, it was possible to dissect a
greater number of lymph nodes by widening the range of lymph node
dissection. However, widening the range of lymph node dissection
was not linked to an increase in lymph node metastasis, thus it may
not affect PSA failure after RP. According to these results, the
National Kyushu Cancer Center's standard dissection range for
prostate cancer is considered to be reasonable; however, there is a
small difference between this standard dissection range and the
extended dissection range around the femoral vein between the NCCN
and EAU guidelines.
RP has been applied as one of the local radical
therapy modalities for prostate cancer cases which have no
metastases, including to the lymph nodes, in preoperative image
evaluations. Therefore, it is very rare for surgeons to perform
PLND while recognizing hard and swollen lymph nodes, which are
suspected of lymph node metastasis during surgery. Namely,
lymphadenectomy in prostate cancer occurs when surgeons determine
the dissection area according to the anatomical index, and dissect
the connective tissue, including the lymph nodes, as much as
possible. Then, the presence or absence of pathologic lymph node
metastasis is determined by observing lymph nodes from the excised
connective tissue. In some series, the number of nodes removed
during lymphadenectomy has been significantly correlated with time
to disease progression (13). In one
population-based study with a 10-year follow-up, patients
undergoing excision of at least 10 nodes (node-negative patients)
had a lower risk of prostate cancer-specific mortality at 10 years
than those who did not undergo lymphadenectomy (15). However, the number of dissected lymph
nodes is considered to be a secondary result, as the number of
dissected lymph nodes is also affected by pathological examinations
(20), and the secure removal of
connective tissue including the lymph nodes in the dissection area
is likely to be more important than the number of dissected lymph
nodes. An expansion of the pelvic cavity is required by urologists
so that larger quantities of connective tissue, including lymph
nodes, are able to be removed, and the dissection of connective
tissues must be performed to the greatest extent possible, in order
to eliminate localized microscopic metastases surgically. Though it
was not shown in the table of this article, there were no patients
with lymph node metastasis in the low-risk group. In addition, the
rates of patients with lymph node metastasis were low (2.3 and 3.6%
in the standard and expanded group, respectively), but this does
not indicate whether PLND may surgically eliminate microscopic
lymph node metastases that are not able not be pathologically
diagnosed as lymph node metastases. Therefore, PLND may be
necessary in the RP cases with intermediate- and high-risk, but not
for patients with low-risk disease. The NCCN and EAU guidelines
also indicate that extended PLND must only be recommended for
intermediate- and high-risk patients, consistent with the
hypothesis of the present study.
In conclusion, at the National Kyushu Cancer Center,
the reduced the range of PLND has been gradually reduced over time,
and standard PLND is routinely performed. Although a greater number
of lymph nodes are able to be dissected when the dissection extent
is greater, the expansion of the dissection range was not
associated with the number or rate of positive lymph nodes.
Therefore, the current dissection range is considered to be
appropriate for Japanese males undergoing radical
prostatectomy.
References
|
1
|
European Association of Urology:
Guidelines on prostate cancer. http://uroweb.org/guideline/prostate-cancer/Accessed.
October 1–2015.
|
|
2
|
Cookson MS: Should pelvic lymph node
dissection be performed with radical prostatectomy? J Urol.
183:1284–1285. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
National Comprehensive Cancer Network:
Guidelines on prostate cancer. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp#prostate/Accessed.
October 1–2015.
|
|
4
|
D'Amico AV, Whittington R, Malkowicz SB,
Schultz D, Blank K, Broderick GA, Tomaszewski JE, Renshaw AA,
Kaplan I, Beard CJ and Wein A: Biochemical outcome after radical
prostatectomy, external beam radiation therapy, or interstitial
radiation therapy for clinically localized prostate cancer. JAMA.
280:969–974. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Epstein JI, Allsbrook WC Jr, Amin MB and
Egevad LL: ISUP Grading Committee: The 2005 International Society
of Urological Pathology (ISUP) consensus conference on gleason
grading of prostatic carcinoma. Am J Surg Pathol. 29:1228–1242.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sobin LH, Gospodarowicz MK and Wittekind
Ch: TNM Classification of Malignant Tumors. 7th. Wiley Blackwell;
Oxford: 2009
|
|
7
|
Katz S and Rosen M: MR imaging and MR
spectroscopy in prostate cancer management. Radiol Clin North Am.
44:723–734. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tempany CM and McNeil BJ: Advances in
biomedical imaging. JAMA. 285:562–567. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Briganti A, Blute ML, Eastham JH, Graefen
M, Heidenreich A, Karnes JR, Montorsi F and Studer UE: Pelvic lymph
node dissection in prostate cancer. Eur Urol. 55:1251–1265. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Briganti A, Chun FK, Salonia A, Gallina A,
Zanni G, Scattoni V, Valiquette L, Rigatti P, Montorsi F and
Karakiewicz PI: Critical assessment of ideal nodal yield at pelvic
lymphadenectomy to accurately diagnose prostate cancer nodal
metastasis in patients undergoing radical retropubic prostatectomy.
Urology. 69:147–151. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Heidenreich A, Varga Z and Von Knobloch R:
Extended pelvic lymphadenectomy in patients undergoing radical
prostatectomy: High incidence of lymph node metastasis. J Urol.
167:1681–1686. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Clark T, Parekh DJ, Cookson MS, Chang SS,
Smith ER Jr, Wells N and Smith J Jr: Randomized prospective
evaluation of extended versus limited lymph node dissection in
patients with clinically localized prostate cancer. J Urol.
169:145–148. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bader P, Burkhard FC, Markwalder R and
Studer UE: Is a limited lymph node dissection an adequate staging
procedure for prostate cancer? J Urol. 168:514–518. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Burkhard FC and Studer UE: The role of
lymphadenectomy in prostate cancer. Urol Oncol. 22:198–204. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Joslyn SA and Konety BR: Impact of extent
of lymphadenectomy on survival after radical prostatectomy for
prostate cancer. Urology. 68:121–125. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bader P, Burkhard FC, Markwalder R and
Studer UE: Disease progression and survival of patients with
positive lymph nodes after radical prostatectomy. Is there a chance
of cure? J Urol. 169:849–854. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Daneshmand S, Quek ML, Stein JP,
Lieskovsky G, Cai J, Pinski J, Skinner EC and Skinner DG: Prognosis
of patients with lymph node positive prostate cancer following
radical prostatectomy: long-term results. J Urol. 172:2252–2255.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wagner M, Sokoloff M and Daneshmand S: The
role of pelvic lymphadenectomy for prostate cancer-therapeutic? J
Urol. 179:408–413. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Mitsuzuka K, Koie T, Narita S, Kaiho Y,
Yoneyama T, Kawamura S, Tochigi T, Ohyama C, Habuchi T and Arai Y:
Is pelvic lymph node dissection required at radical prostatectomy
fo low-risk prostate cancer? Int J Urol. 20:1092–1096. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Perry-Keene J, Ferguson P, Samaratunga H,
Nacey JN and Delahunt B: Total submission of pelvic lymphadenectomy
tissues removed during radical prostatectomy for prostate cancer
increases lymph node yield and detection of micrometastases.
Histopathology. 64:399–404. 2014. View Article : Google Scholar : PubMed/NCBI
|