Introduction
Malignant peripheral nerve sheath tumor (MPNST;
formerly, melanotic schwannoma) is a rare neoplasm of Schwann cell
origin capable of melanogenesis (1,2).
Clinicopathologically, it is considered a distinct entity from
conventional schwannoma due to genetic and clinical differences
(3). Immunophenotypic indicators for
schwannomas with melanotic differentiation include the presence of
epitheloid cells with variably sized nuclei, and a marked
accumulation of melanin (2), but
differential diagnosis typically requires further analysis through
ultrastructural and immunohistochemical testing. In terms of
clinical management, it is of paramount importance to distinguish
primary melanin-containing lesions from malignant melanoma in order
to plan an appropriate therapeutic approach.
Case report
A 14 year-old female initially presented with a
non-painful swelling of the right posterior mandible with right
facial weakness. A magnetic resonance imaging (MRI) scan of the
face and neck revealed a 5.3 cm mass of the right parotid gland,
and a chest computed tomography (CT) scan revealed several small,
non-specific opacities in the upper right lobe. A histopathological
examination performed by core needle biopsy revealed a malignant
melanotic spindle cell neoplasm, with atypical spindle cell
proliferation arranged in a fascicular pattern. The tumor was
histologically and immunophenotypically consistent with MPNST. The
patient underwent a right radical parotidectomy and a right
modified radical neck dissection with reconstructive surgery. Note
was made of the extension of the neoplasm into the soft tissues
around the parotid gland with perineural invasion.
Immunohistochemical analysis confirmed the diagnosis, with the
involvement of three out of eight tumorous lymph nodes staining
positive for laminin, homatropine methylbromide 45 (HMB-45), and
tyrosinase, and negative for melanoma-associated antigen recognized
by T cells (MART-1) and S-100 protein. In March 2007, the patient
started chemotherapy with temozolomide (75 mg/m2 given
orally, daily for 45 days), and in April 2007, sorafenib (40 mg by
mouth, twice daily), due to the increased sizes of nine lung
lesions. In spite of these treatments, however, a repeat positron
emission tomography (PET)/CT scan in June 2007 revealed diffuse
progression in the lungs, thighs, and left flank. The patient was
admitted for treatment with high-dose interleukin-2, but only
received 7 of 14 doses due to unacceptable toxicity and disease
progression. After three cycles of ifosfamide (1,800
mg/m2/day for 5 days) as continuous infusion with mesna,
and doxorubicin (37.5 mg/m2/day intravenously for 2
days), a repeat PET/CT scan revealed further tumor progression;
therefore, the chemotherapy was discontinued.
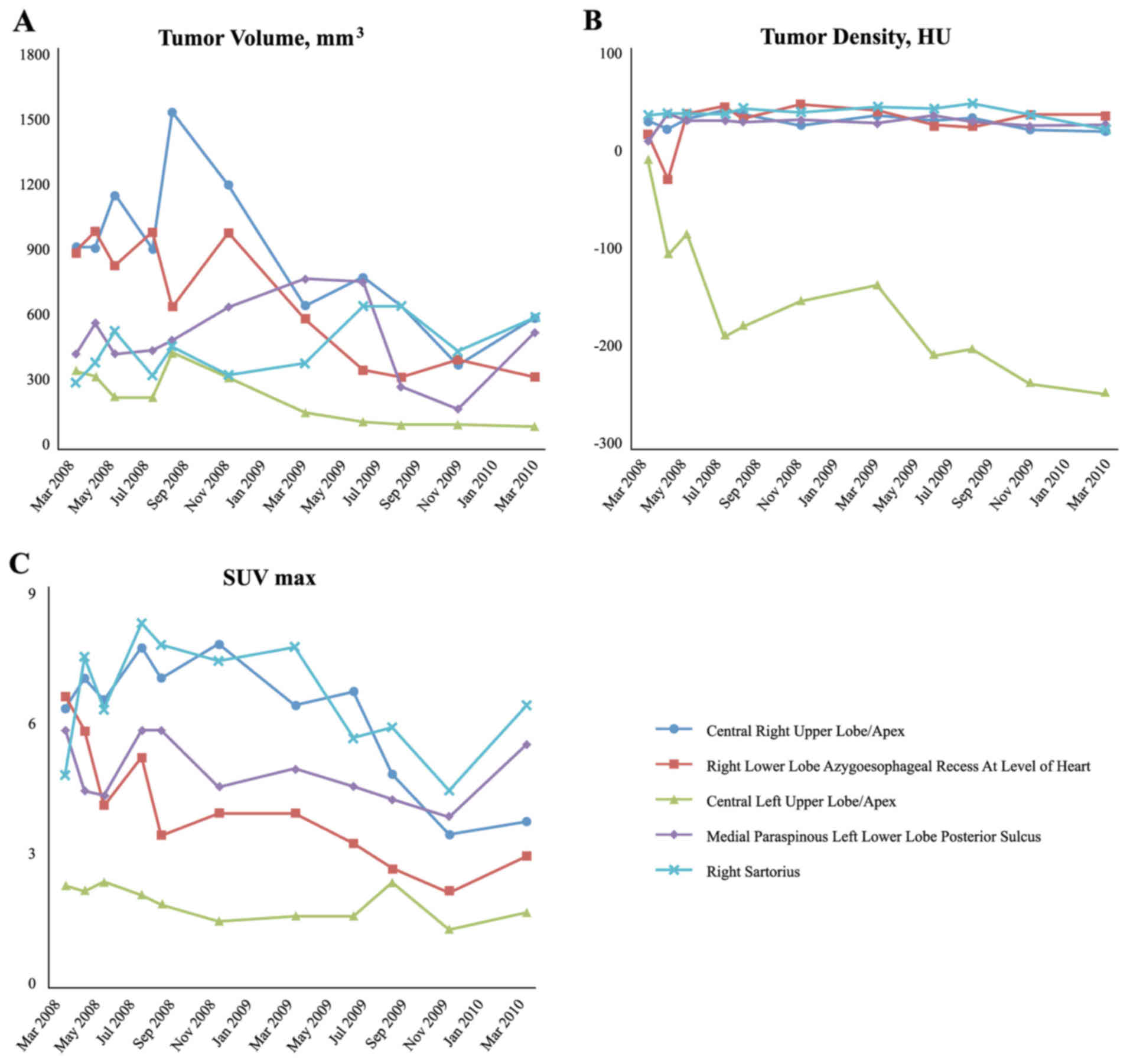
In March 2008, the patient participated in a Phase
1/2 clinical trial using intravenous Rexin-G® (developed
at the USC Keck School of Medicine, Los Angeles, CA, USA) for
advanced chemoresistant sarcoma (clinical trial protocol no.
NCT00505713; see Table I). The
patient received dose level 3 of Rexin-G®
[3×10e11 colony-forming units (cfu)] three times a week
as an outpatient. Objective tumor responses were evaluated by a
number of parameters, including Response Evaluation Criteria In
Solid Tumors (RECIST) v1 (4), tumor
volume, mm3 (length × width2 × 0.52), tumor
density in Hounsfeld units (HU) and the maximum standardized uptake
value (SUVmax) by fluorodeoxyglucose (18-FDG) PET-CT
(4,5). Based on the RECIST v1 and other
radiological parameters, the patient experienced sustained disease
control (Fig. 1). The patient's
clinical course was complicated by an episode of nephrotic
syndrome, which was attributed to the bi-weekly subcutaneous
granulocyte-macrophage colony-stimulating factor (GM-CSF)
injections, and therefore these were discontinued. The patient
received a total of 205 Rexin-G® vector infusions over a
2-year period with minimal toxicity and no serious adverse events.
Following the last infusion in June 2010, the patient underwent a
PET/CT scan, comparing the results with those images taken prior to
treatment. The radiology report stated that there was a marked
overall improvement in the patient's pulmonary metastases, with all
but one nodule being either markedly improved in size, or resolved.
It was also noted that the right pleural effusion and previous
significant ascites had been resolved. Currently, nine years after
commencing the Rexin-G® treatment, the patient is alive
and well, with no evidence of active neoplastic disease.
 | Table I.USA-based clinical trials using
tumor-targeted Rexin-G® for chemotherapy-resistant solid
malignancies. |
Table I.
USA-based clinical trials using
tumor-targeted Rexin-G® for chemotherapy-resistant solid
malignancies.
| Clinical trial
protocol number/dose levela | Clinical
site(s)/Phase | Clinical
indication | No. of patients | Outcome |
|---|
| NCT00121745; dose
level, minus 3-minus 1 | Rochester, MN, USA:
Phase 1 | Pancreas CA | 12 | 0% 1-year OS |
|
NCT00504998b; dose level, 1–3 | Santa Monica, CA,
USA/Manhattan, NY, USA/(Duke) Durham, NC, USA: Phase 1/2 | Pancreas CA | 20 | 26.7% 1-year OS 13.3%
2-year OS 1 alive in sustained remission, 9-year OS |
|
NCT00505713b; dose level, 1–4 | Santa Monica, CA,
USA: Phase 1/2 | Bone and soft tissue
sarcoma | 36 | 38.5% 1-year OS; 31%
2-year OS 1 alive with no active disease, 9-year OS |
| NCT00505271; dose
level, 1–4 | Santa Monica, CA,
USA/Manhattan, NY, USA: Phase 1/2 | Breast CA | 20 | 60% 1-year OS |
| NCT00572130; dose
level, 1–2 | Santa Monica, CA,
USA: Phase 2 | Osteosarcoma | 22 | 27.3% 1-year OS 22.7%
2-year OS 1 alive in sustained remission, 8 years |
Discussion
Peripheral nerve sheath tumor (PNST) is a rare
subset of soft tissue sarcomas displaying an immunophenotype
consistent with that of conventional schwannomas, along with
cytoplasmic melanin deposition characteristic of melanomas
(3,6,7). These
tumors occur most frequently at nerve roots, although other
locations along the peripheral nervous system have been described
(8). Tumors originating from the
bone, soft tissues, heart, mouth, esophagus, bronchus,
retroperitoneum, uterine cervix, orbit, parotid gland, as well as
the spinal cord, acoustic nerve, cerebellum, and sympathetic chain,
have been reported (1,9). Statistics have revealed a 1.1:1 male:
female ratio (9). The ages of those
afflicted vary between 10 and 84 years (7,9),
although the peak incidence occurs with patients in their fourth
decade (7). There have been fewer
than 200 cases of PNST reported since it was first described in
1932 (10,11), with approximately 40 reported
malignancies as of 2014 (12). To
date, there have been no published cases of MPNST originating from
the parotid gland. Therefore, this case is unique and worthy of
report, particularly with respect to the patient's impressive
response to an innovative tumor-targeted gene therapy vector,
designated Rexin-G®.
To make a differential diagnosis between MPNST and
spindle cell melanoma is very difficult, particularly in small
biopsy specimens, due to the diverse range of tumor derivations
from a Schwann cell lineage (13)
and similar histological features, including cell pleomorphisms
with prominent nucleoli (1). In the
present case study, immunohistochemical staining and
ultrastructural examinations proved to be useful in guiding the
diagnostic process. All reported cases of MPNST, including the
present patient's case, have revealed positive gene expression of
HMB-45 and tyrosinase, indicative of melanocytic differentiation,
but negative expression of MART-1 and S-100 protein, thereby
eliminating a diagnosis of melanoma (14). Further studies for the expression of
laminin, which was displayed intensely in two-thirds of the
reported cases (15), concluded that
the tumor represented a Schwannian differentiation, based on the
biphasic pattern (i.e. individual cell and nested) in the external
lamina.
The prognosis for PNST is unpredictable at best,
with 10% of all cases developing metastasis (8,10,14).
Although generally considered benign, the tumor is prone to
malignancy and recurrence, occurring in ~20% of patients (1,8,16). Surgery has been the primary treatment
option (9), followed by radiation
therapy or adjuvant chemotherapy. For the patient described in the
present case report, a right parotidectomy was performed, and
systemic chemotherapy was administered post-surgery to treat the
metastatic lung lesions, albeit without success.
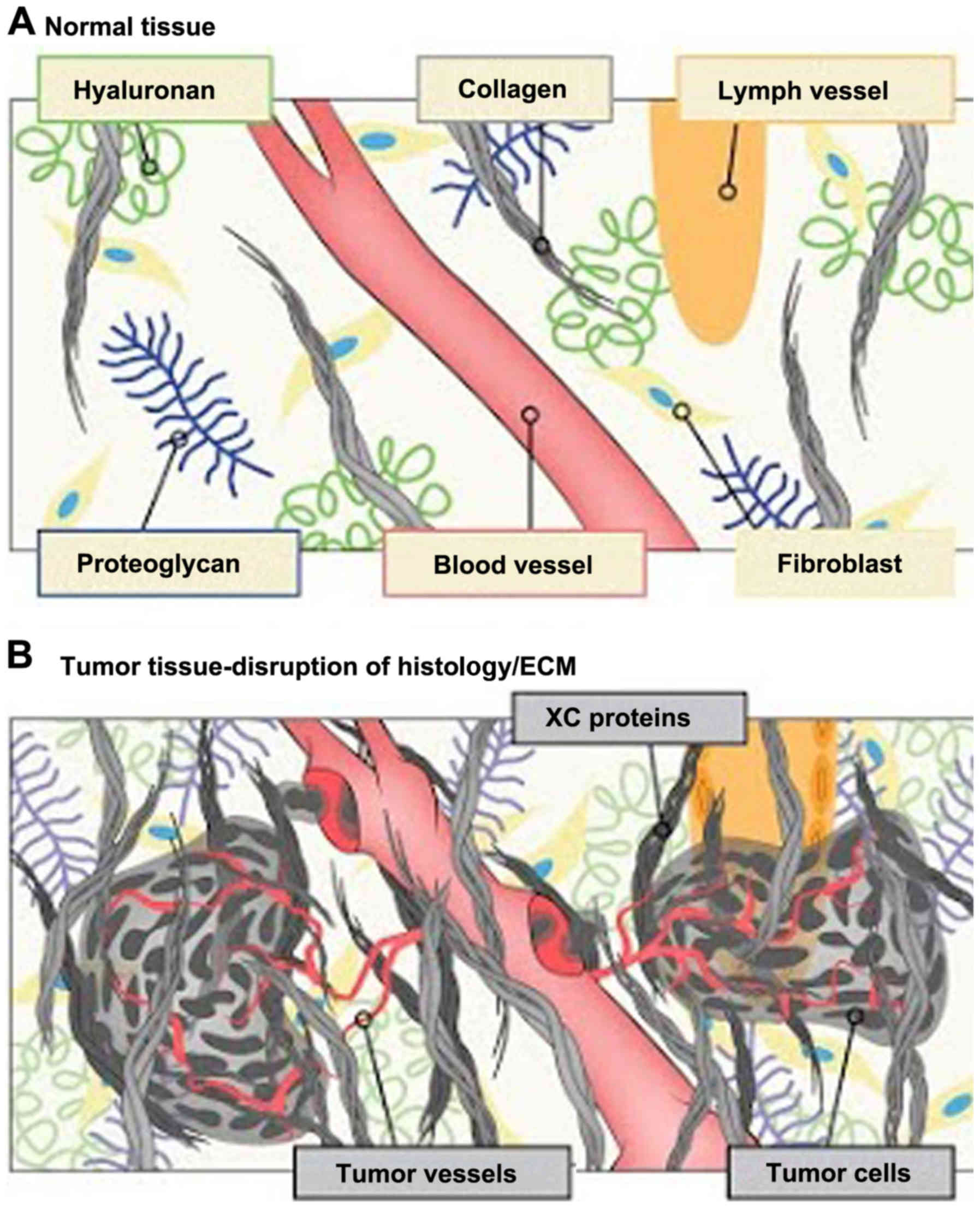
Rexin-G® is the first tumor-targeted gene
therapy vector that has been tested in the clinic (4). Injected intravenously, the targeted
retroviral particles operate within the vascular system via a
high-affinity collagen-binding motif derived from von Willebrand
coagulation factor (17). Atypical
amounts of exposed collagenous (XC) proteins are located in areas
of tumor invasion, neoangiogenesis and stroma formation, possibly
resulting from exposure to protease activity within the tumor
microenvironment (TME; Fig. 2).
Rexin-G® accumulates in these metastatic deposits by
seeking out the abnormal XC proteins, thereby increasing effective
vector concentration in the TME in close association with the
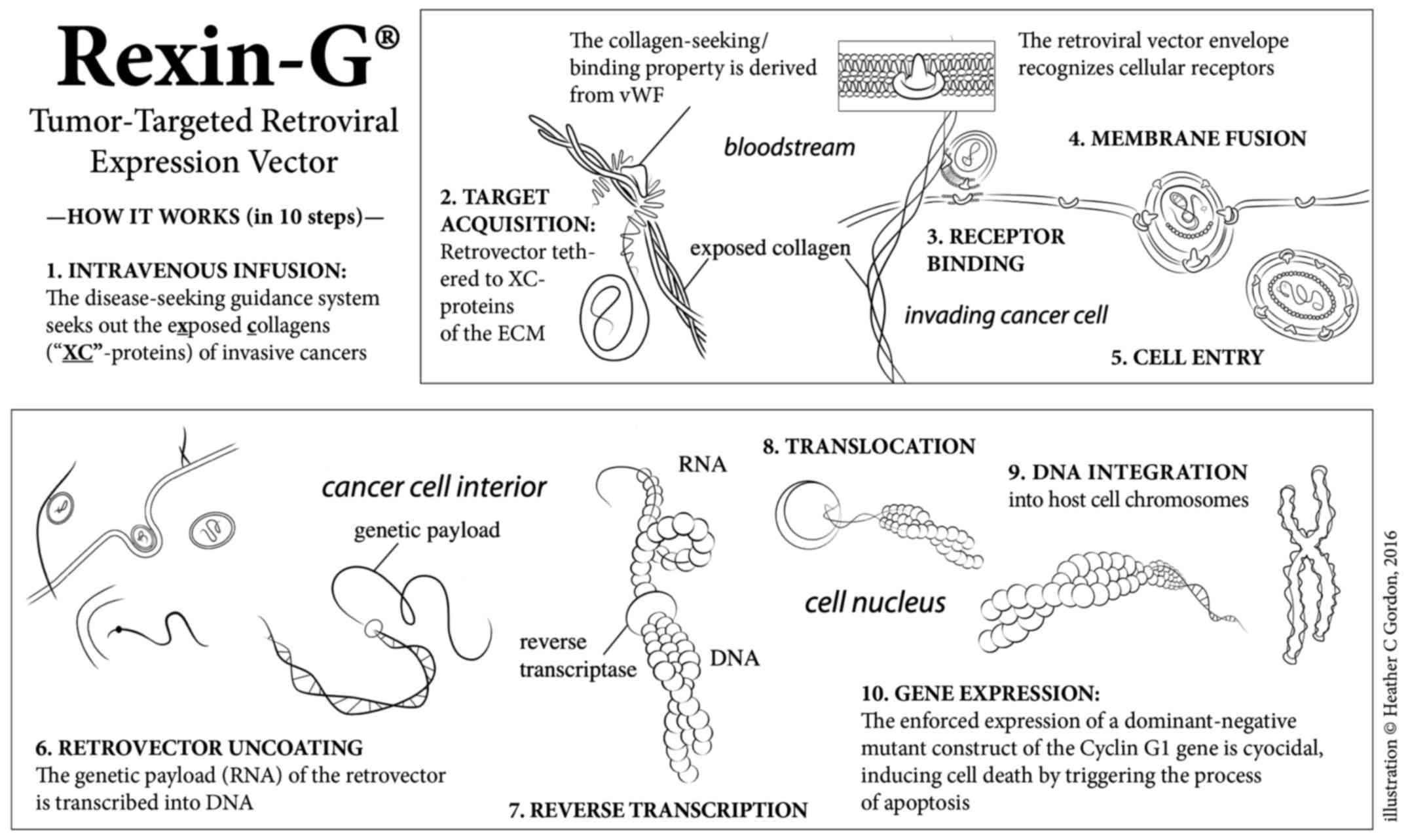
cancer cells. The function of the genetic payload (a dominant
negative cyclin G1 construct is encoded in Rexin-G®) is
to halt the G1 phase of the cell cycle, thus inducing cell death
via apoptosis-mediated pathways (Fig.
3) (17–20).
 | Figure 3.An illustration of the mechanism of
action of Rexin-G®. The Rexin-G® nanoparticle
displays an XC-targeting motif, derived from the coagulation
factor, vWF, on its surface amphotropic gp70 envelope protein. When
injected intravenously, Rexin-G® seeks out and
accumulates in cancerous lesions by binding to exposed collagenous
(XC) proteins. This chimeric retrovector has the innate property of
binding to a tumor's natural viral/cell receptor, fusing, entering,
uncoating, and integrating randomly into the chromosomes of only
actively dividing cells (i.e., cancer cells). This selective
property spares all terminally differentiated and/or
non-replicative cells of normal organs, including hepatocytes,
neuronal cells and myocardial cells. Rexin-G® carries a
cytocidal dominant negative cyclin G1 construct, which causes cell
death via apoptosis. vWF, von Willebrand factor; XC, exposed
collagenous. |
Based on a critical evaluation of its safety and
potential efficacy, as well as the unmet medical need,
Rexin-G® was granted Orphan Drug status for soft tissue
sarcoma and osteosarcoma by the US Food and Drug Administration
(FDA) in 2008 (21); and in 2010,
Phase 1 and Phase 2 clinical trials using Rexin-G® for
chemotherapy-resistant soft tissue sarcoma and osteosarcoma,
respectively, were successfully completed (5,21). The
results of these studies demonstrated the overall safety and, in
clinical trials for sarcoma and pancreatic cancer, the
dose-dependent efficacy in controlling tumor growth and improving
survival rates with the use of Rexin-G®, particularly at
the higher dose levels (Table I).
Accordingly, long-term survival follow-up (up to 15 years
post-treatment) is required by the US FDA for investigational gene
therapy products; to date, there have been no reports of delayed or
late adverse events associated with Rexin-G®
treatment.
In summary, in the present report, the unique case
of a 14 year-old patient with widely metastatic MPNST of the
parotid gland, who experienced a durable response and sustained
tumor control (and minimal toxicity) with an innovative therapy
treatment of Rexin-G®, an XC-/tumor-targeted retrovector
bearing a cytocidal gene construct, is described. On the basis of
these results, the continued development of Rexin-G® for
this rare type of mesenchymal cancer, and potentially other
chemoresistant sarcomas, is highly recommended.
Acknowledgements
The authors are grateful to Heather C. Gordon (Art
Consultant, Sarcoma Oncology Center, Santa Monica, CA, USA) for
graphic illustrations and editorial assistance in the writing of
this manuscript (see www.heathergordondrawings.com).
Glossary
Abbreviations
Abbreviations:
|
CT
|
computed tomography
|
|
MRI
|
magnetic resolution imaging
|
|
MPNST
|
malignant peripheral nerve sheath
tumor
|
|
PNST
|
peripheral nerve sheath tumor
|
|
PET
|
positron emission tomography
|
|
GM-CSF
|
granulocyte-macrophage
colony-stimulating factor
|
|
XC
|
exposed collagenous
|
|
TME
|
tumor microenvironment
|
References
|
1
|
Vallat-Decouvelaere AV, Wassef M, Lot G,
Catala M, Moussalam M, Caruel N and Mikol J: Spinal melanotic
schwannoma: A tumour with poor prognosis. Histopathology.
35:558–566. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rodriguez FJ, Folpe AL, Giannini C and
Perry A: Pathology of peripheral nerve sheath tumors: Diagnostic
overview and update on selected diagnostic problems. Acta
Neuropathol. 123:295–319. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Louis DN, Perry A, Reifenberger G, von
Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD,
Kleihues P and Ellison DW: The 2016 world health organization
classification of tumors of the central nervous system: A summary.
Acta Neuropathol. 131:803–820. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chawla SP, Chawla NS, Quon D, Chua-Alcala
V, Blackwelder WC, Hall FL and Gordon EM: An advanced phase 1/2
study using an XC-targeted gene therapy vector for chemotherapy
resistant sarcoma. Sarcoma Res Int. 3:10242016.
|
|
5
|
Gordon EM, Cornelio GH, Lorenzo CC III,
Levy JP, Reed RA, Liu L and Hall FL: First clinical experience
using a ‘pathotropic’ injectable retroviral vector (Rexin-G) as
intervention for stage IV pancreatic cancer. Int J Oncol.
24:177–185. 2004.PubMed/NCBI
|
|
6
|
Er U, Kazanci A, Eyriparmak T, Yigitkanli
K and Senveli E: Melanotic schwannoma. J Clin Neurosci. 14:676–678.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kurtkaya-Yapicier O, Scheithauer B and
Woodruff JM: The pathobiologic spectrum of Schwannomas. Histol
Histopathol. 18:925–934. 2003.PubMed/NCBI
|
|
8
|
Welling LC, Guirado VM, Tessari M, Felix
AR, Zanellato C, Figueiredo EG, Taricco MA and Teixeira MJ: Spinal
melanotic schwannomas. Arq Neuropsiquiatr. 70:156–157. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Faria MH, Dória-Netto RH, Osugue GJ, Lde S
Queiroz and Chaddad-Neto FE: Melanotic schwannoma of the cervical
spine progressing with pulmonary metastasis: Case report. Neurol
Med Chir (Tokyo). 53:712–716. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Pan SY, Cheng YC and Kao TH:
Intramedullary melanotic schwannoma: Case report and review of the
literature. Surg Neurol Int. 5 Suppl 4:S181–S184. 2014. View Article : Google Scholar
|
|
11
|
Khoo M, Pressney I, Hargunani R and
Tirabosco R: Melanotic schwannoma: An 11-year case series. Skeletal
Radiol. 45:29–34. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Torres-Mora J, Dry S, Li X, Binder S, Amin
M and Folpe AL: Malignant melanotic schwannian tumor: A
clinicopathologic, immunohistochemical, and gene expression
profiling study of 40 cases, with a proposal for the
reclassification of ‘melanotic schwannoma’. Am J Surg Pathol.
38:94–105. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Röhrich M, Koelsche C, Schrimpf D, Capper
D, Sahm F, Kratz A, Reuss J, Hovestadt V, Jones DT,
Bewerunge-Hudler M, et al: Methylation-based classification of
benign and malignant peripheral nerve sheath tumors. Acta
Neuropathol. 131:877–887. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Küsters-Vandevelde HV, van Engen-van
Grunsven IA, Küsters B, van Dijk MR, Groenen PJ, Wesseling P and
Blokx WA: Improved discrimination of melanotic schwannoma from
melanocytic lesions by combined morphological and GNAQ mutational
analysis. Acta Neuropathol. 120:755–764. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Huang HY, Park N, Erlandson RA and
Antonescu CR: Immunohistochemical and ultrastructural comparative
study of external lamina structure in 31 cases of cellular,
classical, and melanotic schwannomas. Appl Immunohistochem Mol
Morphol. 12:50–58. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Killeen RM, Davy CL and Bauserman SC:
Melanocytic schwannoma. Cancer. 62:174–183. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hall FL, Liu L, Zhu NL, Stapfer M,
Anderson WF, Beart RW and Gordon EM: Molecular engineering of
matrix-targeted retroviral vectors incorporating a surveillance
function inherent in von Willebrand factor. Hum Gene Ther.
11:983–993. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Chawla SP, Chua VS, Fernandez L, Quon D,
Blackwelder WC, Gordon EM and Hall FL: Advanced phase I/II studies
of targeted gene delivery in vivo: Intravenous Rexin-G for
gemcitabine-resistant metastatic pancreatic cancer. Mol Ther.
18:435–441. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gordon EM, Levy JP, Reed RA, Petchpud WN,
Liu L, Wendler CB and Hall FL: Targeting metastatic cancer from the
inside: A new generation of targeted gene delivery vectors enables
personalized cancer vaccination in situ. Int J Oncol. 33:665–675.
2008.PubMed/NCBI
|
|
20
|
Gordon EM, Lopez FF, Cornelio GH, Lorenzo
CC III, Levy JP, Reed RA, Liu L, Bruckner HW and Hall FL:
Pathotropic nanoparticles for cancer gene therapy Rexin-G IV:
Three-year clinical experience. Int J Oncol. 29:1053–1064.
2006.PubMed/NCBI
|
|
21
|
Gordon EM and Hall FL: Rexin-G, a targeted
genetic medicine for cancer. Expert Opin Biol Ther. 10:819–832.
2010. View Article : Google Scholar : PubMed/NCBI
|