Introduction
ENKTL has several unusual characteristics, including
being predominantly involved in the nasal cavity and nasopharynx,
and closely associated with Epstein-Barr virus (EBV) infection.
Primary extranasal sites of involvement are mainly the skin, soft
tissue, gastrointestinal tract and testis (1). There are no differences in ethnicity,
gender, age or immunophenotypic profile between the nasal and
extranasal cases; however, the latter exhibit a more aggressive
clinical outcome (2). In cases of
extranasal ENKTL, the lung is a relatively rare site of
involvement. To the best of our knowledge, there is no large-scale
investigation referring to primary pulmonary ENKTL.
Case report
A 34-year-old female was admitted to the respiratory
intensive care unit of The First Affiliated Hospital of Zhengzhou
University (Zhengzhou, Henan, China) on 8 November, 2016 with chief
complaints of fever for one month and progressive dyspnea for 6
days. At first, the patient had an intermittent fever ≤39°C. She
was subsequently admitted to a local hospital and initially
received empirical antibiotic treatment (cefoxitin) for more than a
week, but her clinical condition deteriorated. As the patient
showed no response to empirical antibiotic therapy, a computed
tomography (CT) of the chest was performed for proper diagnosis.
The chest CT showed multiple massive infiltrates in both lungs with
cervical, mediastinal and axillary lymphadenopathy. The patient was
therefore referred to The First Affiliated Hospital of Zhengzhou
University for further study. She was a farmer and non-smoker.
There was no relevant personal or familial medical history. The
patient was immunocompetent and human immunodeficiency
virus-negative.
Physical examination
On admission, the patient's vital signs included
blood pressure, 137/97 mmHg; pulse rate, 100 beats/min; respiratory
rate, 25 breaths/min; and body temperature, 38.4°C. Her face had an
acutely ill-looking appearance. On chest auscultation, bilateral
moist rales were found in both lung fields. Physical examination
confirmed cervical and axillary lymph node enlargement.
Laboratory assessments
Laboratory assessments were conducted and revealed
in Table I.
 | Table I.Laboratory assessments. |
Table I.
Laboratory assessments.
| Variables | Results | Reference range |
|---|
| White blood cell
count | 3.0×109/l | 4-10×109/l |
| Absolute neutrophil
count | 1.8×109/l | 2-7.7×109/l |
| Hemoglobin | 115 g/l | 110–160 g/l |
| Platelet count | 214×109/l | 100-300×109/l |
| Alanine
aminotransferase | 63 U/l | 0–40 U/l |
| Aspartate
aminotransferase | 130 U/l | 0–40 U/l |
| Albumin | 26 g/l | 35–55 g/l |
| Globulin | 28.6 g/l | 20–35 g/l |
| Serum total
bilirubin | 5.77 µmol/l | 0–25 µmol/l |
| Direct bilirubin | 2.15 µmol/l | 0–10 µmol/l |
| Indirect
bilirubin | 3.6 µmol/l | 0–14 µmol/l |
| Lactate
dehydrogenase | 1184 IU/l | 75–240 IU/l |
| β2-microglobulin | 5.38 mg/l | 0.9–2.3 mg/l |
| Urea nitrogen | 2.85 mmol/l | 1.8–7.5 mmol/l |
| Serum creatinine | 42 µmol/l | 30–110 μmol/l |
| C-reactive
protein | 10.44 mg/l | 0–10 mg/l |
| Erythrocyte
sedimentation rate | 3.7 mm/h | 0–20 mm/h |
| Procalcitonin | 0.095 ng/ml | 0-0.1 ng/ml |
| pH | 7.46 | 7.35–7.45 |
| PCO2 | 32.8 mmHg | 35–45 mmHg |
| PO2 | 61.3 mmHg | 80–100 mmHg |
| HCO3
concentration | 21.1 mmol/l | 22–26 mmol/l |
| SaO2
concentration | 92.6% | 91.9–99% |
| CEA | 1.86 ng/ml | 0–5 ng/ml |
| AFP | 2.29 ng/ml | 0–10 ng/ml |
| CA125 | 36.25 U/ml | 0–35 U/ml |
| CA19-9 | 105 U/ml | 0–35 U/ml |
| CA15-3 | 21.78 U/ml | 0–35 U/ml |
| Cyfra21-1 | 6.48 ng/ml | 0-3.3 ng/ml |
| CA72-4 | 0.67 U/ml | 0–10 U/ml |
| NSE | 30.39 ng/ml | 0–20 ng/ml |
| G test | Negative | Negative |
| GM test | Negative | Negative |
| T-SPOT | Negative | Negative |
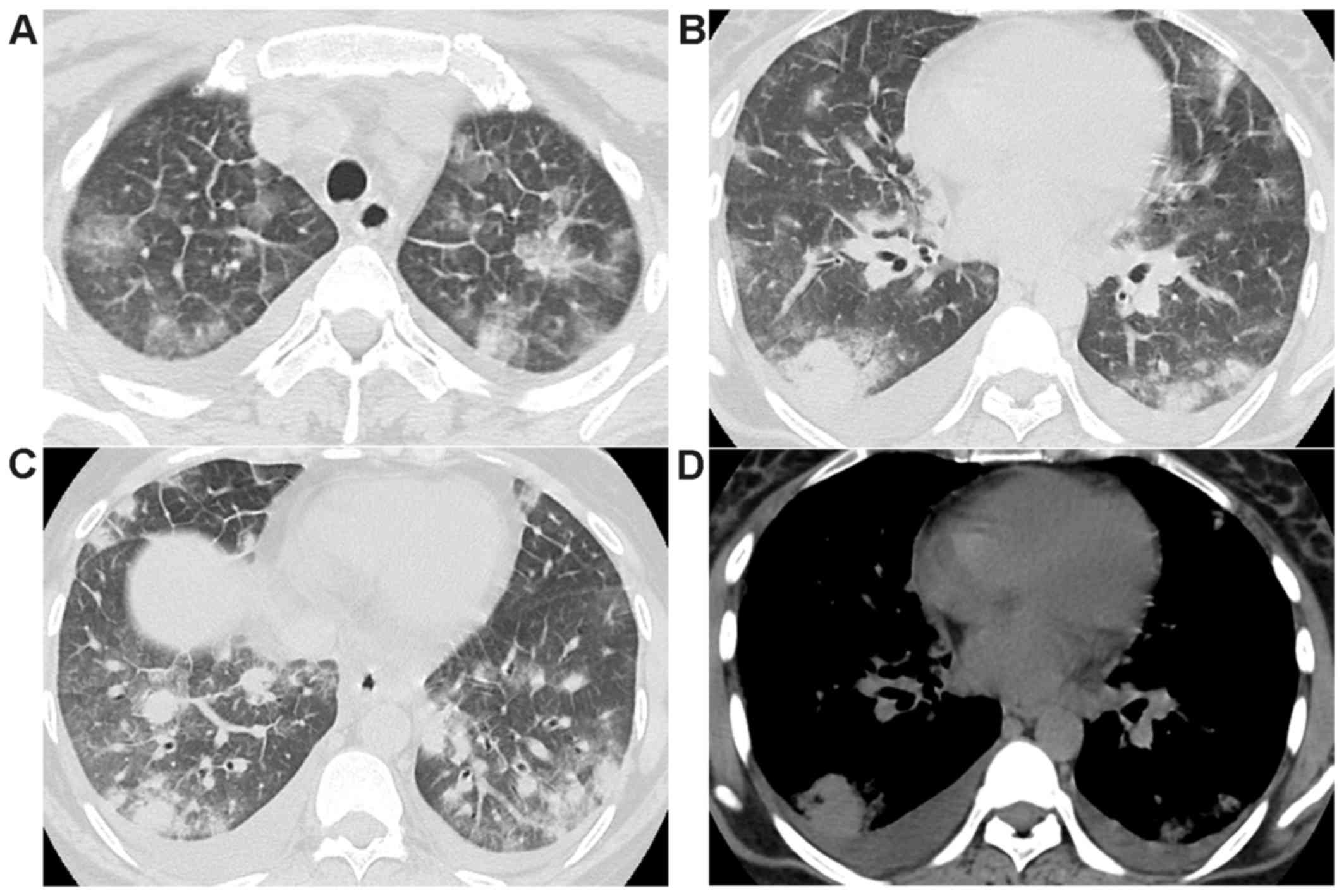
On admission, a repeat chest CT revealed progressive
multiple nodules in both lungs with ground-glass opacities,
measuring ≤27×22.5 mm in diameter, as shown in Fig. 1. CT also revealed bilateral pleural
effusion and cervical, mediastinal and axillary lymphadenopathy.
These findings suggested an advanced lung cancer or severe
pneumonia. The patient was then treated with broad-spectrum
antibiotic therapy (imipenem, moxifloxacin and voriconazole) for 6
days. Despite enhanced antibiotic therapy, the patient showed
aggravated dyspnea and her clinical condition continued to
deteriorate. A CT-guided transthoracic needle biopsy of the right
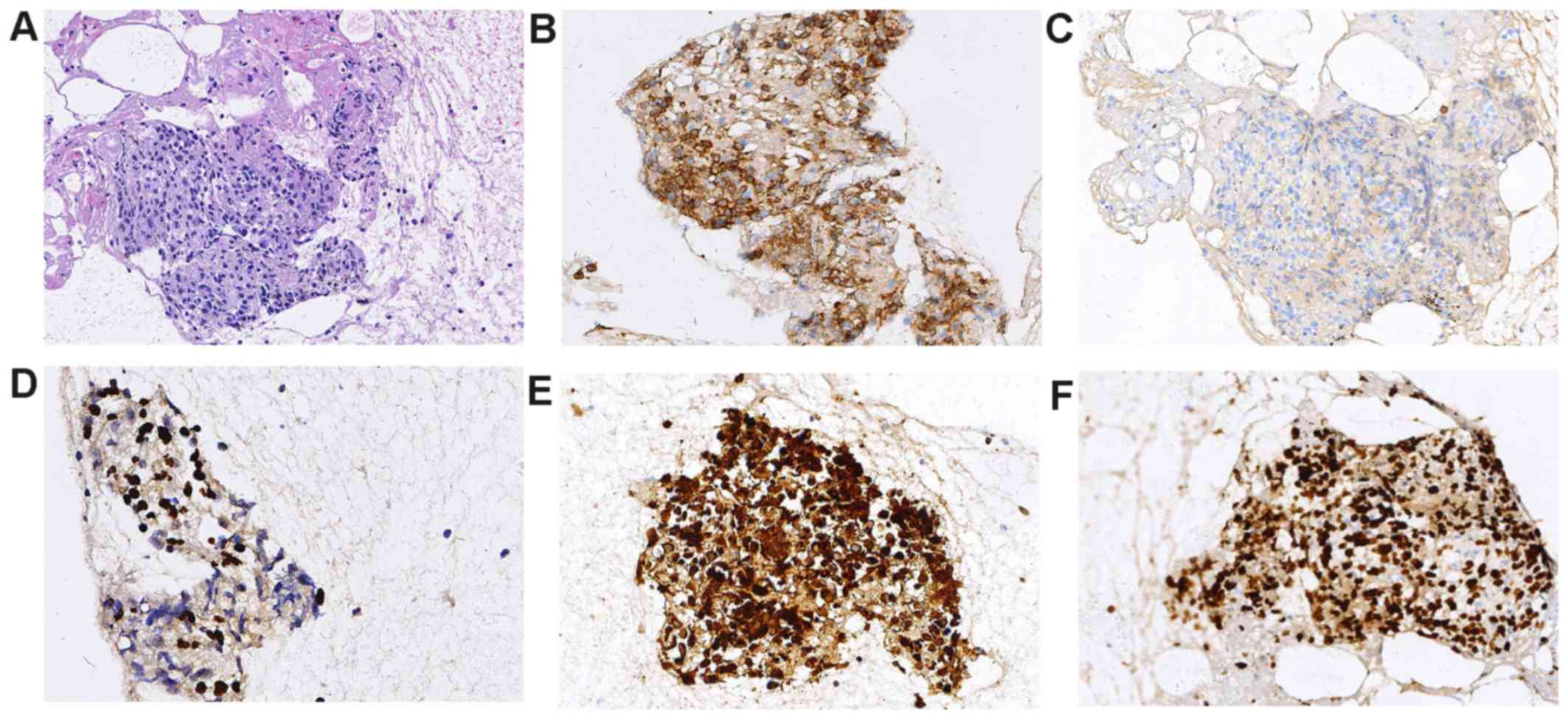
lung was therefore undertaken. The surgical specimen was fixed in
4% formalin, embedded in paraffin and stained with hematoxylin and
eosin. Histologically, the small to medium-sized cells presented
angiodestructive growth patterns with an inflammatory response and
necrosis. Immunohistochemical (IHC) staining was positive for CD43,
CD3, TIA-1, GranzymeB, CD30 and 70%Ki-67; and negative for CD20,
CD79α, thyroid transcription factor 1, CD56, SYN and cytokeratin
(AE1/AE3). The antibodies of IHC were purchased from
ZSGB-BIO(Beijing, China). The IHC staining was performed according
to the manufacturer's instructions. The cells were labeled for
EBV-encoded RNA (EBER) in situ hybridization, as shown in
Fig. 2. These findings were
consistent with NK/T-cell lymphoma, although there was no previous
ENKTL history and no evidence of lymphoma involvement in the
extrapulmonary site. Thus, the patient was diagnosed with primary
pulmonary ENKTL. Unfortunately, the patient refused to undergo
chemotherapy and showed rapid deterioration. She died three days
after hospital discharge as a result of disease progression with
respiratory failure. This study was approved by the ethics
committee of the First Affiliated Hospital of Zhengzhou University,
and written informed consent was obtained from this patient.
Discussion
There are few studies in the literature on the
clinicopathological characteristics, therapy and prognostic factors
of primary pulmonary ENKTL. The similar cases of pulmonary ENKTL in
the latest literature have been listed here (3–14). Due
to the rarity of this disease, nonspecific clinical symptoms and
limited availability of biopsy tissues, the diagnosis of primary
pulmonary ENKTL is notably difficult. Patients are frequently
presumed to present with pneumonia and initially treated with
empirical antibiotics. Therefore, CT-guided needle biopsy or
bronchoscopic examination should be considered when clinical
symptoms show deterioration in spite of adequate antibiotic
therapy. It should also be differentiated from tuberculosis,
pneumomycosis and lung cancer. A delay in diagnosis may result in a
fatal outcome, so an early correct diagnosis is crucial to
determine prognosis. In the previous reports, the patients most
presented with fever (90%), cough (70%), and dyspnea (45%). Fever
was the most common initial clinical symptom. It was different from
primary pulmonary MALT lymphoma, which most frequently presented
with dry cough (41%) and dyspnoea (35%). We presumed that the
possible reason was EBV infection and aggressive nature of
ENKTL.
ENKTL is an aggressive disease with poor prognosis.
Primary pulmonary ENKTL is associated with shorter survival rate
and poorer therapy response irrespective of the stage, compared
with nasal disease. The aggressive clinical behavior of primary
extranasal disease is similar to that of advanced stage nasal
disease (2). Furthermore, survival
does not differ between primary pulmonary ENKTL and any other
subset of primary pulmonary lymphoma (15). There is still no consensus on the
optimal therapy for primary pulmonary ENKTL (16,17).
Cyclophosphamide, hydroxydaunorubicin, oncovin and prednisone
(CHOP/CHOP-like) chemotherapy has generally been used for the
treatment of primary pulmonary ENKTL, but with unsatisfactory
results; p-glycoprotein may be responsible for the multiple drug
resistance. However, chemotherapy remains the main treatment for
primary extranasal ENKTL; more effective treatment strategies are
therefore required for this disease. Recent large-scale studies
demonstrated that the outcome of ENKTL was noticeably improved with
the advent of asparaginase/gemcitabine-based regimens including
SMILE (dexamethasone, methotrexate, ifosfamide, L-asparaginase and
etoposide) and DDGP(dexamethasone, cisplatin, gemcitabline and
pegaspargase) (18,19). It has been identified that
asparaginase/gemcitabine-based regimens are superior to
CHOP/CHOP-like chemotherapy in ENKTL patients and
asparaginase/gemcitabine-based regimens have been recommended for
patients with advanced-stage or relapsed/refractory ENKTL (20). In the previous reports, the patients
who received asparagine/gemcitabine-based chemotherapy survived for
24 and 3 months, respectively (11,13).
Therefore, we propose that asparaginase-basedchemotherapy may be
the optimal treatment strategy for primary pulmonary ENKTL.
However, there remains no prognostic model for primary pulmonary
ENKTL. In the published lieratures, we identified only one risk
factor(female) out of various clinical parameters that was
prognostic for overall survival by univariate analysis.
There were also limitations in this study: i)
EBV-DNA level is very important to ENKTL, but we did not test the
plasma EBV-DNA level; ii) given the patient found the ineffective
treatment and supposed to suffer from the potential lymphoma in
other hospital, we did not conduct a needle biopsy for confirmation
as early as possible. It may result in a delay in diagnosis and
unfavourable prognosis. An earlier needle biopsy and
asparaginase-basedchemotherapy would have been better for the
patient.
In conclusion, primary pulmonary ENKTL is extremely
rare with dismal survival, the diagnosis should be considered when
patients present with fever, lung mass and non-responsive to
antibiotics. Correct diagnosis with early effective treatment may
have benefit for prognosis. Further prospective multicenter studies
should be conducted to define the best therapeutic strategies and
prognostic factors.
Acknowledgements
Not applicable.
Funding
Not applicable.
Authors' contributions
YQ made contributions to the conception and design
of the study, and wrote the manuscript. JH and DH performed data
collection. DZ performed histological examination. The final
version of the manuscript has been read and approved by all
authors.
Ethics approval and consent to
participate
This study was approved by the ethics committee of
the First Affiliated Hospital of Zhengzhou University, and written
informed consent was obtained from the patient.
Consent for publication
Written informed consent was obtained from the
patient for publication of this case report and any accompanying
images.
Competing of interests
Authors declare no competing of interest.
References
|
1
|
Chan JK, Sin VC, Wong KF, Ng CS, Tsang WY,
Chan CH, Cheung MM and Lau WH: Nonnasal lymphoma expressing the
natural killer cell marker CD56: A clinicopathologic study of 49
cases of an uncommon aggressive neoplasm. Blood. 89:4501–4513.
1997.PubMed/NCBI
|
|
2
|
Au WY, Weisenburger DD, Intragumtornchai
T, Nakamura S, Kim WS, Sng I, Vose J, Armitage JO and Liang R:
International Peripheral T-Cell Lymphoma Project: Clinical
differences between nasal and extranasal natural killer/T-cell
lymphoma: A study of 136 cases from the International Peripheral
T-Cell Lymphoma Project. Blood. 113:3931–3937. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lee S, Shin B, Yoon H, Lee JY and Chon GR:
A case of primary pulmonary NK/T cell lymphoma presenting as
pneumonia. Respir Med Case Rep. 17:1–4. 2015.PubMed/NCBI
|
|
4
|
Lee BH, Kim SY, Kim MY, Hwang YJ, Han YH,
Seo JW, Kim YH, Cha SJ and Hur G: CT of nasal-type T/NK cell
lymphoma in the lung. J Thorac Imaging. 21:37–39. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gong L, Wei LX, Huang GS, Zhang WD, Wang
L, Zhu SJ, Han XJ, Yao L, Lan M, Li YH, et al: Identification of
genuine primary pulmonary NK cell lymphoma via clinicopathologic
observation and clonality assay. Diagn Pathol. 8:1402013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Laohaburanakit P and Hardin KA: NK/T cell
lymphoma of the lung: A case report and review of literature.
Thorax. 61:267–270. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chien CC, Lee HS, Lin MH and Hsieh PP:
Primary extranodal natural killer/T-cell lymphoma of bronchus and
lung: A case report and review of literature. Thorac Cancer.
7:140–144. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liu CH, Wang HH, Perng CL, Peng CK, Chian
CF and Shen CH: Primary extranodal NK/T-cell lymphoma of the lung:
Mimicking bronchogenic carcinoma. Thorac Cancer. 5:93–96. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yang L, Feng W, Chen C, Zhang X, Zhu Y,
Lei W and Huang JA: Primary pulmonary T-cell lymphoma mimicking
pneumonia: A case report and literature review. Exp Ther Med.
12:365–368. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Fei W, Xiaohong W, Hong Z and Bei H:
Pulmonary Extranodal Natural Killer/T-Cell Lymphoma (Nasal Type): A
Case Report and Radiological Image Review. Medicine (Baltimore).
94:e15272015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gui W, Yang B, Shen Q, Bai M, Wang J, Guan
T, Zhao J, Wang J and Su L: Successful treatment with
L-asparaginase-based regimen for primary pulmonary NK/T cell
lymphoma: A case report and review of the literature. Clin Respir
J. 9:493–496. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cao MS, Cai HR, Yin HL, Zhang DP, Xiao YL,
Cao M, Dai LJ and Hou J: Primary natural killer/T cell lymphoma of
the lung: Two cases report and clinical analysis. Zhonghua Jie He
He Hu Xi Za Zhi. 31:120–124. 2008.(in Chinese). PubMed/NCBI
|
|
13
|
Ding W, Wang J, Zhao S, Yang Q, Sun H, Yan
J, Gao L, Yao W, Zhang W and Liu W: Clinicopathological study of
pulmonary extranodal nature killer/T-cell lymphoma, nasal type and
literature review. Pathol Res Pract. 211:544–549. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Oshima K, Tanino Y, Sato S, Inokoshi Y,
Saito J, Ishida T, Fukuda T, Watanabe K and Munakata M: Primary
pulmonary extranodal natural killer/T-cell lymphoma: Nasal type
with multiple nodules. Eur Respir J. 40:795–798. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Borie R, Wislez M, Thabut G, Antoine M,
Rabbat A, Couderc LJ, Monnet I, Nunes H, Blanc FX, Mal H, et al:
Clinical characteristics and prognostic factors of pulmonary MALT
lymphoma. Eur Respir J. 34:1408–1416. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ferraro P, Trastek VF, Adlakha H,
Deschamps C, Allen MS and Pairolero PC: Primary non-Hodgkin's
lymphoma of the lung. Ann Thorac Surg. 69:993–997. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cadranel J, Wislez M and Antoine M:
Primary pulmonary lymphoma. Eur Respir J. 20:750–762. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kwong YL, Kim WS, Lim ST, Kim SJ, Tang T,
Tse E, Leung AY and Chim CS: SMILE for natural killer/T-cell
lymphoma: Analysis of safety and efficacy from the Asia Lymphoma
Study Group. Blood. 120:2973–2980. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhang L, Jia S, Ma Y, Li L, Li X, Wang X,
Fu X, Ma W, Qin Y, Li W, et al: Efficacy and safety of cisplatin,
dexamethasone, gemcitabine and pegaspargase (DDGP) regimen in newly
diagnosed, advanced-stage extranodal natural killer/T-cell
lymphoma: Interim analysis of a phase 4 study NCT01501149.
Oncotarget. 7:55721–55731. 2016.PubMed/NCBI
|
|
20
|
Jaccard A, Gachard N, Marin B, Rogez S,
Audrain M, Suarez F, Tilly H, Morschhauser F, Thieblemont C,
Ysebaert L, et al: GELA and GOELAMS Intergroup: Efficacy of
L-asparaginase with methotrexate and dexamethasone (AspaMetDex
regimen) in patients with refractory or relapsing extranodal
NK/T-cell lymphoma, a phase 2 study. Blood. 117:1834–1839. 2011.
View Article : Google Scholar : PubMed/NCBI
|