Introduction
Bisphosphonate (BP) is used for bone metastasis or
hormonal agent-related bone loss in patients with breast cancer
(1–4). The mechanism of BP involves inhibiting
the synthesis and liberation of osteoclasts, which results in
promoting resistance against bone resorption (5,6).
Therefore, long-term use of BP easily causes osteoporotic fractures
(7). In 2003, osteonecrosis of the
jaw (ONJ) was reported as a serious complication of BP treatment
for the first time (8).
Odontogenic infection can spread from the
submandibular space to the retropharyngeal space, and lead to
descending necrotizing mediastinitis (DNM). DNM progresses rapidly,
without specific clinical findings, and requires invasive
procedures, including mediastinal drainage or open thoracic
surgery. Thus, it is associated with high mortality, even in this
antibiotic era. Once BP-induced ONJ causes mandibular
osteomyelitis, it may potentially lead to DNM. To the best of our
knowledge, however, DNM caused by BP-induced ONJ have never been
reported before. This is the first case in the English
literature.
Here, we present a rare case of DNM caused by
BP-induced ONJ in a patient with bone metastasis of breast cancer.
It is difficult to manage DNM in patients with terminal cancer
because of their impaired general condition and limited longevity.
Therefore, we should start prophylactic treatment and detect the
initial signs of DNM carefully.
Case report
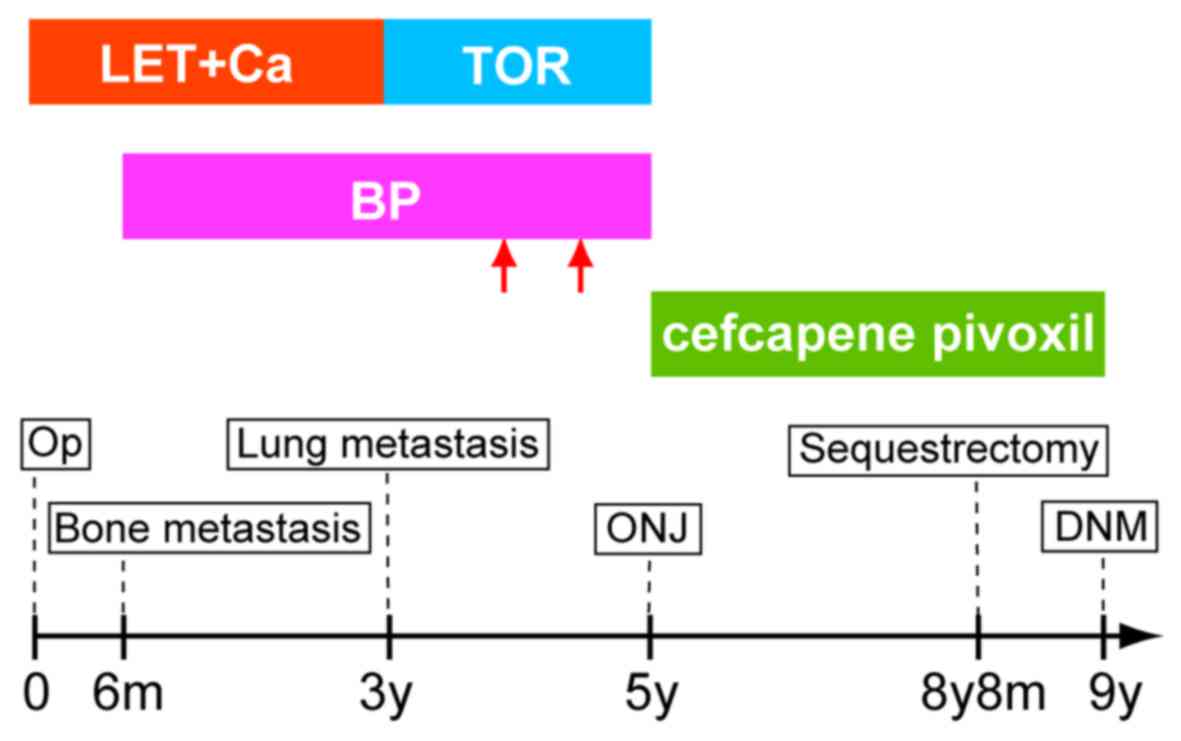
An 83-year-old woman was referred to our hospital
for a mass with skin distortion in her right breast 9 years ago. At
this time, the patient was diagnosed with estrogen
receptor-positive breast cancer and axillary lymph node metastasis,
and underwent right mastectomy and axillary lymphadenectomy. Of the
14 lymph nodes identified in the axillary tail, 8 were positive for
malignancy. Pathological examination revealed pT3N1M0. Bone
metastasis was found in the right costal bone 6 months after the
operation, despite treatment with letrozole concomitant with
irradiation postoperatively. Therefore, we added zoledronate. The
patient had no documented history of dental treatment before BP
treatment. In addition, serum tumor marker levels gradually
elevated. We changed the regimen to high-dose toremifene (12
mg/day) due to lung metastasis. However, the patient's condition
worsened despite modifying the regimen of these hormonal
agents.
Bone scintigraphy showed abnormal uptake in the
mandibular bone 5 years after the operation. We diagnosed ONJ and
treated the patient conservatively with oral administration of
cefcapene pivoxil for 3 years and 8 months. Four months prior to
the present referral, however, the patient underwent sequestrectomy
because the ONJ involved the mandibular canal and the patient
presented with uncontrollable pain. First, oral mucosa around the
exposed sequestrum was incised, and mucoperiosteal flap tissue was
dissected. Following exposure of the borderline between the normal
bone and sequestrum, the anterior portion was removed completely.
Next, the remaining posterior lesion was removed as much as
possible to avoid injury to arteries in the mandible because the
laboratory data showed anemia. At this time, cefazolin was
administered perioperatively. Additional sequestrectomy for the
residual lesion was planned after anemia improved. Four years and 6
months after the initiation of BP therapy, the patient developed
osteonecrosis of the jaw. Therefore, we stopped BP immediately and
did not resume administration. In addition, the patient underwent
no other dental procedures except for sequestrectomy while she had
treatment for cancer. BP was administered for 4 years and 6 months
in total, including 2 cessation periods at 2 and 5 months for
transient impairment of renal function.
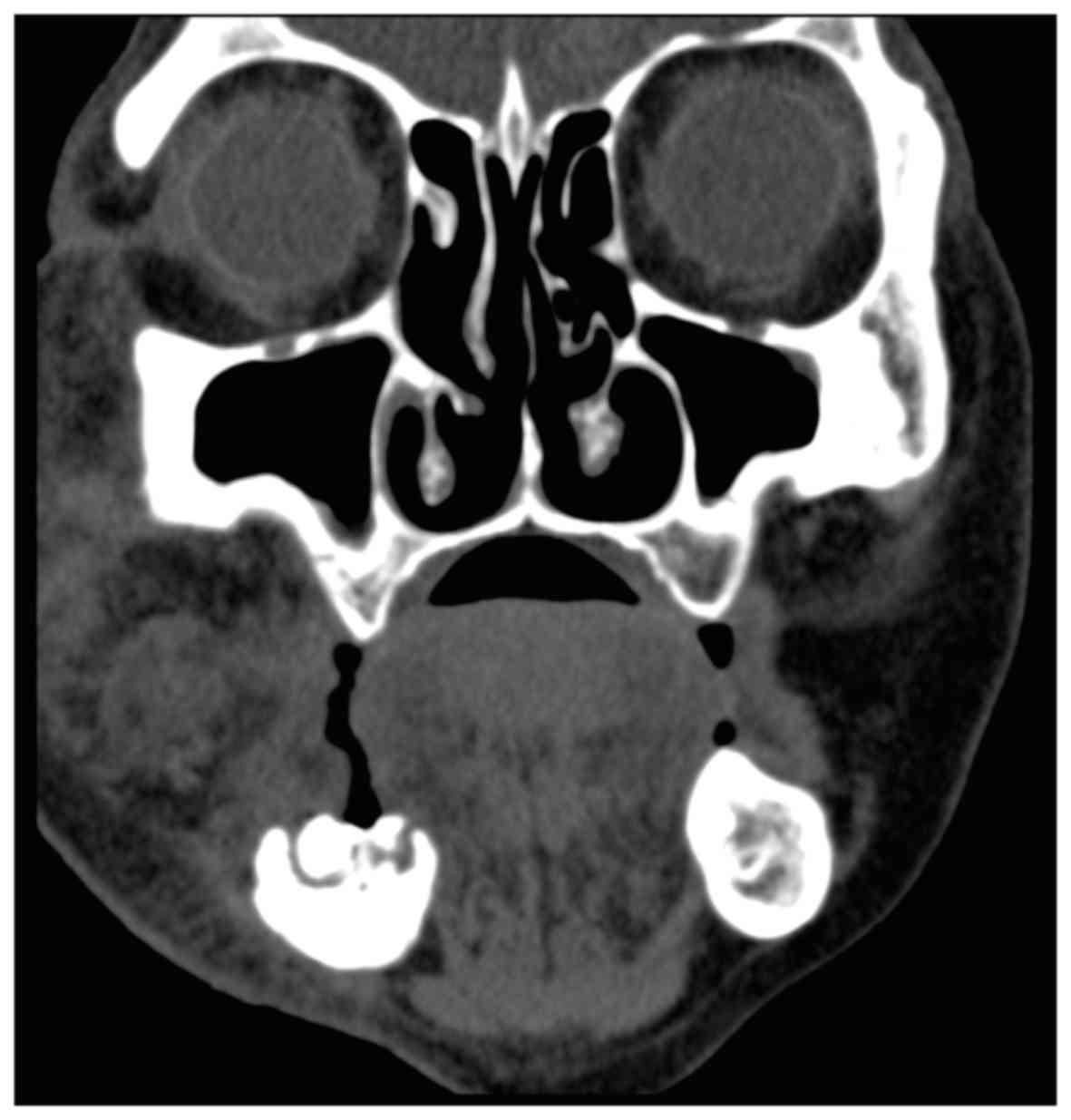
The patient presented to the emergency department
with a 1-week history of fever, dyspnea, and right facial swelling
with pain. Blood tests showed an elevated white blood cell count of
25,500/µl and C-reactive protein level of 14.05 mg/dl. Computed
tomography (CT) demonstrated inflammation in the right mandibular
subcutaneous tissue, but no gas formation or airway obstruction
(Fig. 1). The patient was diagnosed
with right mandibular cellulitis. The patient was admitted to our
hospital and we started intravenous infusion of ceftriaxone.
Inflammatory marker levels continued to rise despite antibiotic
therapy. The patient's general condition worsened rapidly, and she
fell into shock. We performed repeated neck and chest CT scans, and
found de novo gas formation extending to the cervical and
retropharyngeal spaces, down to the posterior mediastinum (Fig. 2A-C). Consequently, the patient was
diagnosed with DNM, and surgical drainage was considered. However,
we could not perform any further invasive procedures because of the
patient's impaired general condition and her family's wishes. The
patient died of septicemia on the third hospital day. Fig. 3 shows the entire clinical course for
the treatment of breast cancer.
Discussion
BP-induced ONJ is a rare, but serious complication,
that reduces quality of life considerably. Bamias et al
(9) reported that the incidence of
BP-induced ONJ in patients with breast cancer was 2.9% (2/70),
whereas that in all patients with BP treatment was 6.7% (17/252).
Periodontal disease and a history of tooth extraction, as well as
various cancer treatments, including hormone, radiation, and
chemotherapies, can increase the risk for ONJ (6,10). In
this case, a 4-year history of BP treatment and a 9-year history of
hormone therapy predisposed the patient to ONJ.
In general, BP-induced ONJ is treated with
antibiotic therapy and cessation of BP. Increased apoptosis of
keratinocytes impairs the oral mucosal barrier in patients with BP
treatment (6,10). Therefore, it is preferable to avoid
any surgical procedures as an initial treatment for either
diagnostic or therapeutic purposes (5,6,8). The present patient was closely followed
up after the diagnosis of ONJ. However, we performed sequestrectomy
to manage uncontrollable pain. This surgical intervention might
potentially be the cause of the osteomyelitis and subsequent
mediastinitis. There is no clear guideline that indicates
sequestrectomy for ONJ. As this case implied, however, we should
avoid sequestrectomy as long as possible, and perform careful
follow-up of elderly patients and those with poor general health
status if they receive long-term BP treatment.
In our institute, regardless of age, BP is
administered in patients with bone metastasis as long as renal
function does not worsen. In patients with a history of dental
procedures, we consult with the oral and maxillofacial surgeon as
to whether BP can be administered. We also consult the oral surgeon
to decide cessation of BP therapy when symptoms of osteonecrosis of
the jaw are observed. The more BP accumulates in the body, the
higher the risk of ONJ. The risk drastically increases when the
administration period exceeds 4 years in total (11). Some clinicians have reported that as
many as 50% of patients with a malignant tumor have inflammatory
dental disease including periodontal disease before the development
of BP-induced ONJ (12). It is also
thought that the direct predisposing factor is not the invasiveness
of the procedure itself, but the local inflammation that led to the
surgical procedure. Therefore, it is important to confirm that the
oral environment is healthy before starting BP therapy. Moreover,
patients with long-term BP therapy require regular follow-up of
serum calcium level and use of prophylactic antibiotics for dental
procedures.
The most common causes of mediastinitis are
esophageal perforation and surgery with sternotomy (13). DNM, which is a rare type of
mediastinitis, occurs as a complication of odontogenic or
cervicofascial infections spreading down the deep fascial planes
into the mediastinum (14). The
mortality rate reaches 50%, even in the current antibiotic era
(15). A recent review estimated the
mortality rate at 25% (16), and DNM
can thus be regarded as one of the most complicated infections.
Predisposing factors previously reported are age over 70 years,
alcoholism, and diabetes mellitus (14). In addition, the incidence of DNM is
much higher in patients who are in poor physical condition owing to
malnutrition, drug addiction, or immunosuppression (17).
Maxillofacial infection can spread into the
mediastinum through the following routes (13,14): i)
Pretracheal space: The infection descends into the frontal
mediastinum through the suprapleural membrane (Sibson's fascia).
ii) Retropharyngeal space: This route begins from the base of the
skull passing downwards into the posterior mediastinum, thereby
enabling direct access of the dental infection to the mediastinum.
iii) Perivascular space: This route is a vascular sheath for the
great cervical vessels-the carotid artery and internal jugular
vein.
According to Moncada et al (18), 71% of cervical infections spread
through retropharyngeal space, while 21% of cases descend through
perivascular space. In the present case, the focus of infection was
a necrotic lesion in the mandibular canal, which communicates with
the dental alveolus. Thus, we speculated that the infection
extended down the retropharyngeal space.
The gold standard for diagnosis of DNM is CT, which
can clearly detect inflammation, abscesses, and gas formation
(14,16). In the present case, CT on admission
revealed evidence of inflammation in subcutaneous tissue of the
right mandibular bone, but no gas formation. Therefore, the patient
was initially diagnosed with cellulitis. However, considerable gas
formation was seen from the mandibular bone to the posterior
mediastinum on CT 2 days later. This finding was compatible with
DNM. The mortality associated with DNM cannot be reduced
drastically, even with antibiotic therapy and drainage, while a
delay of diagnosis and incomplete drainage cause further increased
mortality (13,17). Most cases of DNM are caused by
odontogenic infection in the roots of the second and third lower
molars, because these teeth are directly communicated with the
submandibular space. Therefore, infection from these teeth descends
into the mediastinum more rapidly and diffusely. A conservative
surgical approach is insufficient to manage DNM, and it requires
more radical drainage, including open chest surgery (14,17). We
considered performing mediastinal drainage, in addition to
antibiotic therapy. However, it was impossible to perform surgical
intervention because the patient's general condition was severely
impaired by her progressive cancer.
In conclusion, once BP-induced ONJ in patients with
advanced cancer causes DNM, the mortality risk greatly increases
because clinicians cannot perform radical treatment due to the
impaired general condition and limited life expectancy. We should
perform CT and check the current condition while keeping the
possibility of DNM in mind when patients with BP-induced ONJ
present trismus, dysphagia, and maxillofacial edema. To prevent
progression, antibiotic therapy should be started empirically,
regardless of the presence of findings implying DNM. Subsequently,
aggressive surgical drainage should be performed as soon as abscess
formation is found. As this case showed, DNM advances by the hour.
Repeated CT scans are essential when antibiotic therapy does not
improve the patient's condition. Attention must be paid to detect
signs of DNM in such patients.
Acknowledgements
The authors would like to thank Dr Tomoki Sakata
(Department of Cardiovascular Surgery, Funabashi Municipal Medical
Center) for valuable advice on mediastinitis.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
TT made substantial contributions to conception and
design of the study and wrote the manuscript. TA, AM, and HM
participated in the treatment of this patient and provided
supervision of this manuscript editing and revised each draft
regarding ONJ (AM) and breast cancer (TA and HM). All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Patient consent for publication of data was
obtained.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kohno N, Aogi K, Minami H, Nakamura S,
Asaga T, Iino Y, Watanabe T, Goessl C, Ohashi Y and Takashima S:
Zoledronic acid significantly reduces skeletal complications
compared with placebo in Japanese women with bone metastases from
breast cancer: A randomized, placebo-controlled trial. J Clin
Oncol. 23:3314–3321. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Takahashi S, Iwase T, Kohno N, Ishikawa T,
Taguchi T, Takahashi M, Horiguchi J, Nakamura S, Hozumi Y, Fukunaga
M and Noguchi S: Efficacy of zoledronic acid in postmenopausal
Japanese women with early breast cancer receiving adjuvant
letrozole: 12-month results. Breast Cancer Res Treat. 133:685–693.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Mauri D, Valachis A, Polyzos IP, Polyzos
NP, Kamposioras K and Pesce LL: Osteonecrosis of the jaw and use of
bisphosphonates in adjuvant breast cancer treatment: A
meta-analysis. Breast Cancer Res Treat. 116:433–439. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Valachis A, Polyzos NP, Georgoulias V,
Mavroudis D and Mauri D: Lack of evidence for fracture prevention
in early breast cancer bisphosphonate trials: A meta-analysis.
Gynecol Oncol. 117:139–145. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Marx RE, Sawatari Y, Fortin M and Broumand
V: Bisphosphonate-induced exposed bone
(osteonecrosis/osteopetrosis) of the jaws: Risk factors,
recognition, prevention, and treatment. J Oral Maxillofac Surg.
63:1567–1575. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kyrgidis A, Vahtsevanos K, Koloutsos G,
Andreadis C, Boukovinas I, Teleioudis Z, Patrikidou A and Triaridis
S: Bisphosphonate-related osteonecrosis of the jaws: A case-control
study of risk factors in breast cancer patients. J Clin Oncol.
26:4634–4638. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kim YS and Park WC: Atypical
subtrochanteric femur fracture in patient with metastatic breast
cancer treated with zoledronic acid. J Breast Cancer. 15:261–264.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Marx RE: Pamidronate (Aredia) and
zoledronate (Zometa) induced avascular necrosis of the jaws: A
growing epidemic. J Oral Maxillofac Surg. 61:1115–1117. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bamias A, Kastritis E, Bamia C,
Moulopoulos LA, Melakopoulos I, Bozas G, Koutsoukou V, Gika D,
Anagnostopoulos A, Papadimitriou C, et al: Osteonecrosis of the jaw
in cancer after treatment with bisphosphonates: Incidence and risk
factors. J Clin Oncol. 23:8580–8587. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Vahtsevanos K, Kyrgidis A, Verrou E,
Katodritou E, Triaridis S, Andreadis CG, Boukovinas I, Koloutsos
GE, Teleioudis Z, Kitikidou K, et al: Longitudinal cohort study of
risk factors in cancer patients of bisphosphonate-related
osteonecrosis of the jaw. J Clin Oncol. 27:5356–5362. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ruggiero SL, Dodson TB, Assael LA,
Landesberg R, Marx RE and Mehrotra B: American Association of Oral
Maxillofacial Surgeons; American Association of Oral and
Maxillofacial Surgeons position paper on bisphosphonate-related
osteonecrosis of the jaws-2009 update. J Oral Maxillofac Surg. 67
Suppl 1:S2–S12. 2009. View Article : Google Scholar
|
|
12
|
Qi WX, Tang LN, He AN, Yao Y and Shen Z:
Risk of osteonecrosis of the jaw in cancer patients receiving
denosumab: A meta-analysis of seven randomized controlled trials.
Int J Clin Oncol. 19:403–410. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Papalia E, Rena O, Oliaro A, Cavallo A,
Giobbe R, Casadio C, Maggi G and Mancuso M: Descending necrotizing
mediastinitis: Surgical management. Eur J Cardiothorac Surg.
20:739–742. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Novakov IP, Safev GP and Peicheva SE:
Descending necrotizing mediastinitis of odontogenic origin-personal
experience and literature review. Folia Med (Plovdiv). 52:13–20.
2010.PubMed/NCBI
|
|
15
|
Sancho LM, Minamoto H, Fernandez A, Sennes
LU and Jatene FB: Descending necrotizing mediastinitis: A
retrospective surgical experience. Eur J Cardiothorac Surg.
16:200–205. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Furst IM, Ersil P and Caminiti M: A rare
complication of tooth abscess-Ludwig's angina and mediastinitis. J
Can Dent Assoc. 67:324–327. 2001.PubMed/NCBI
|
|
17
|
Chen KC, Chen JS, Kuo SW, Huang PM, Hsu
HH, Lee JM and Lee YC: Descending necrotizing mediastinitis: A
10-year surgical experience in a single institution. J Thorac
Cardiovasc Surg. 136:191–198. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Moncada R, Warpeha R, Pickleman J, Spak M,
Cardoso M, Berkow A and White H: Mediastinitis from odontogenic and
deep cervical infection. Anatomic pathways of propagation. Chest.
73:497–500. 1978.
|