Introduction
Squamous cell carcinoma is a type of metaplastic
carcinoma; metaplastic carcinoma is characterized as carcinoma of
the breast ductal tissue and stratified squamous epithelial tissue
followed by their consequent differentiation into bone, cartilage
and osteocartilaginous tissue. It has been reported that
metaplastic breast carcinoma accounts for <1% of all breast
carcinomas, and it is characterized by large size, low incidence of
lymphatic metastasis and high incidence of triple-negative
phenotype (1–3). While chemotherapy for metaplastic
carcinoma is commonly similar to that of invasive ductal carcinoma,
a number of studies in the literature report a poor response to
conventional chemotherapy (1,4,5). We herein report our experience with
eribulin administration in a case of recurrent squamous cell
carcinoma of the breast and discuss the relevant literature.
Case report
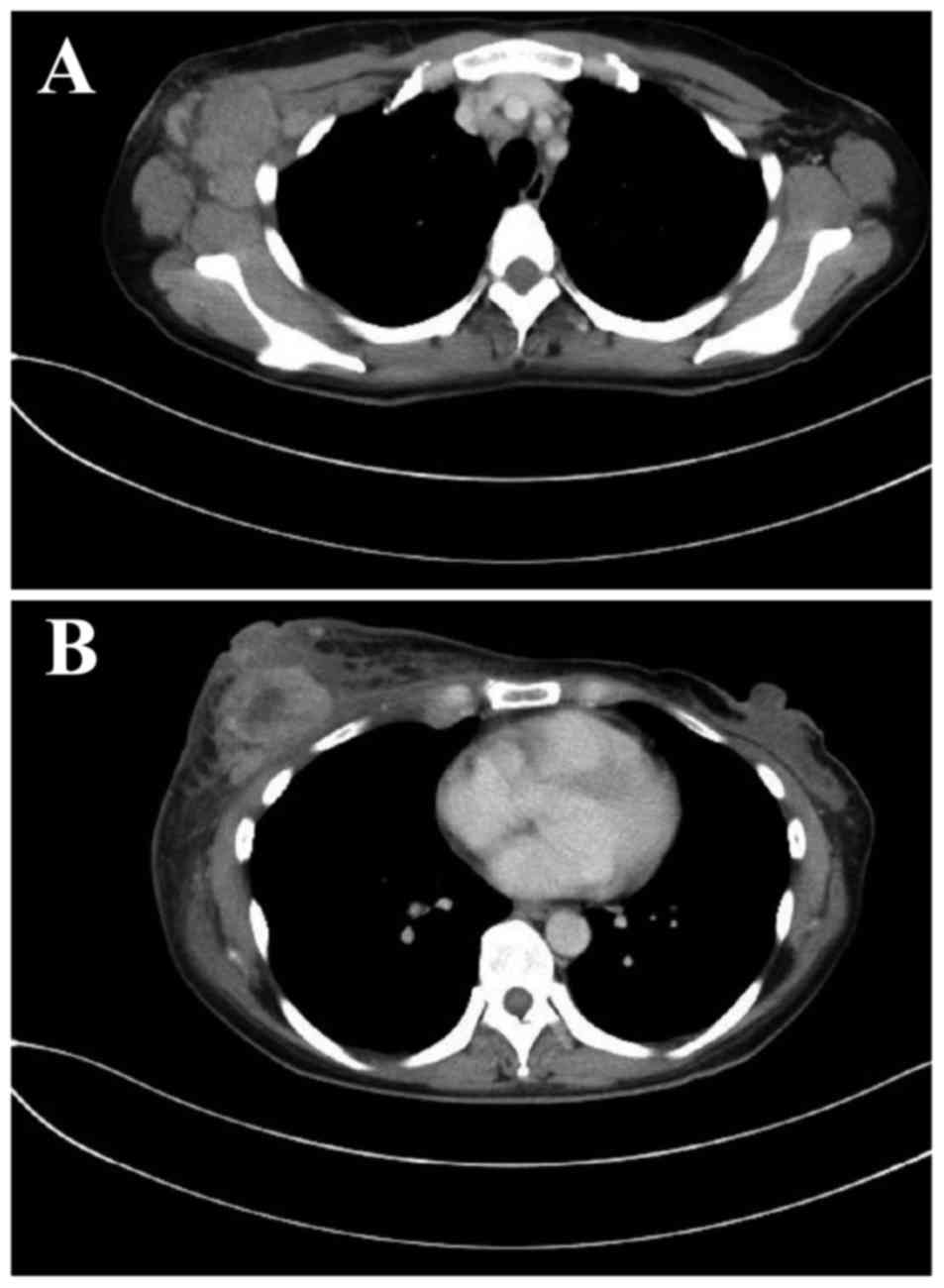
A 42-year-old woman with carcinoma of the right
breast (T4N3aM0, stage IIIC) underwent mastectomy and level III
axillary lymph node dissection (Fig.
1).
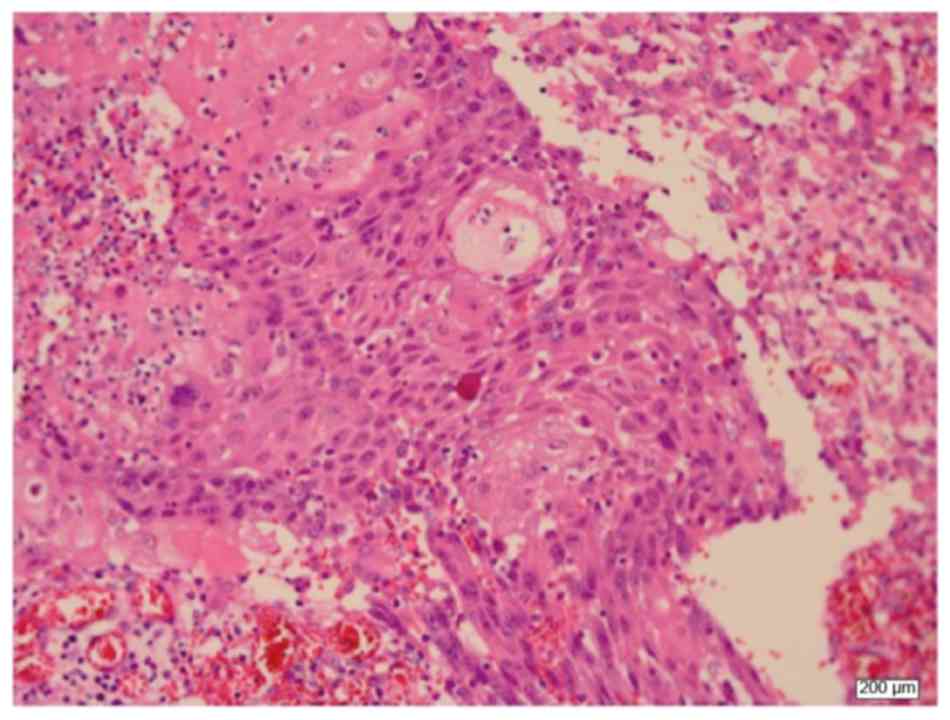
Pathological examination revealed squamous cell
carcinoma negative for estrogen receptor, progesterone receptor and
human epidermal growth factor receptor 2 (Fig. 2). Six cycles of postoperative
adjuvant chemotherapy with cyclophosphamide 500 mg/m2,
epirubicin 75 mg/m2 and fluorouracil 500
mg/m2 (CEF regimen) were administered, following which
an increase in the size of the ipsilateral sternal lymph nodes was
observed. No other metastatic lesions were found on computed
tomography (CT) scans, and the patient was subjected to
lymphadenectomy with pleural drainage. Pathological examination of
the resected nodes demonstrated metastatic squamous cell carcinoma.
Docetaxel (75 mg/m2) was administered as adjuvant
therapy; however, allergic symptoms developed, including
respiratory distress and palpitations, and docetaxel was
discontinued. Radiotherapy to the right thoracic wall and the right
supraclavicular lymph node (60 Gy) was next administered. However,
enlargement of the ipsilateral supraclavicular lymph node was
observed 3 months after radiotherapy. Lymphadenopathy (lymph node
enlarged to 2 cm in diameter) was identified on ultrasound
examination, and fine-needle aspiration cytology confirmed the
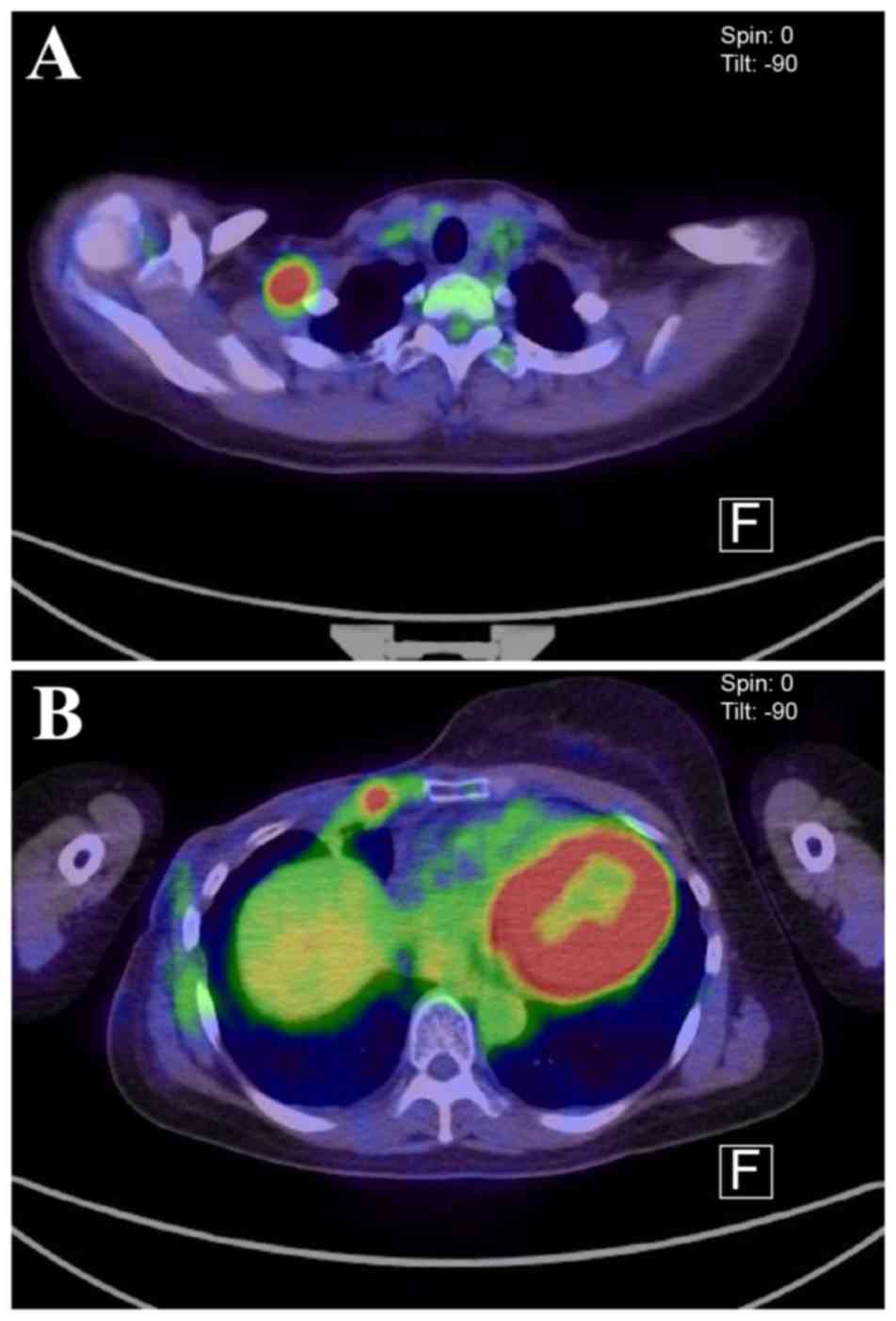
presence of metastatic squamous cell carcinoma. Fluorodeoxyglucose
positron emission tomography (FDG-PET)-CT revealed accumulation in
the anterior thoracic wall close to the previous surgical site
(Fig. 3). Consequently, eribulin
(1.4 mg/m2) was administered as initial therapy. The
lymph node was not palpable at 1 month after therapy initiation,
and at 3 months after chemotherapy the enlargement had completely
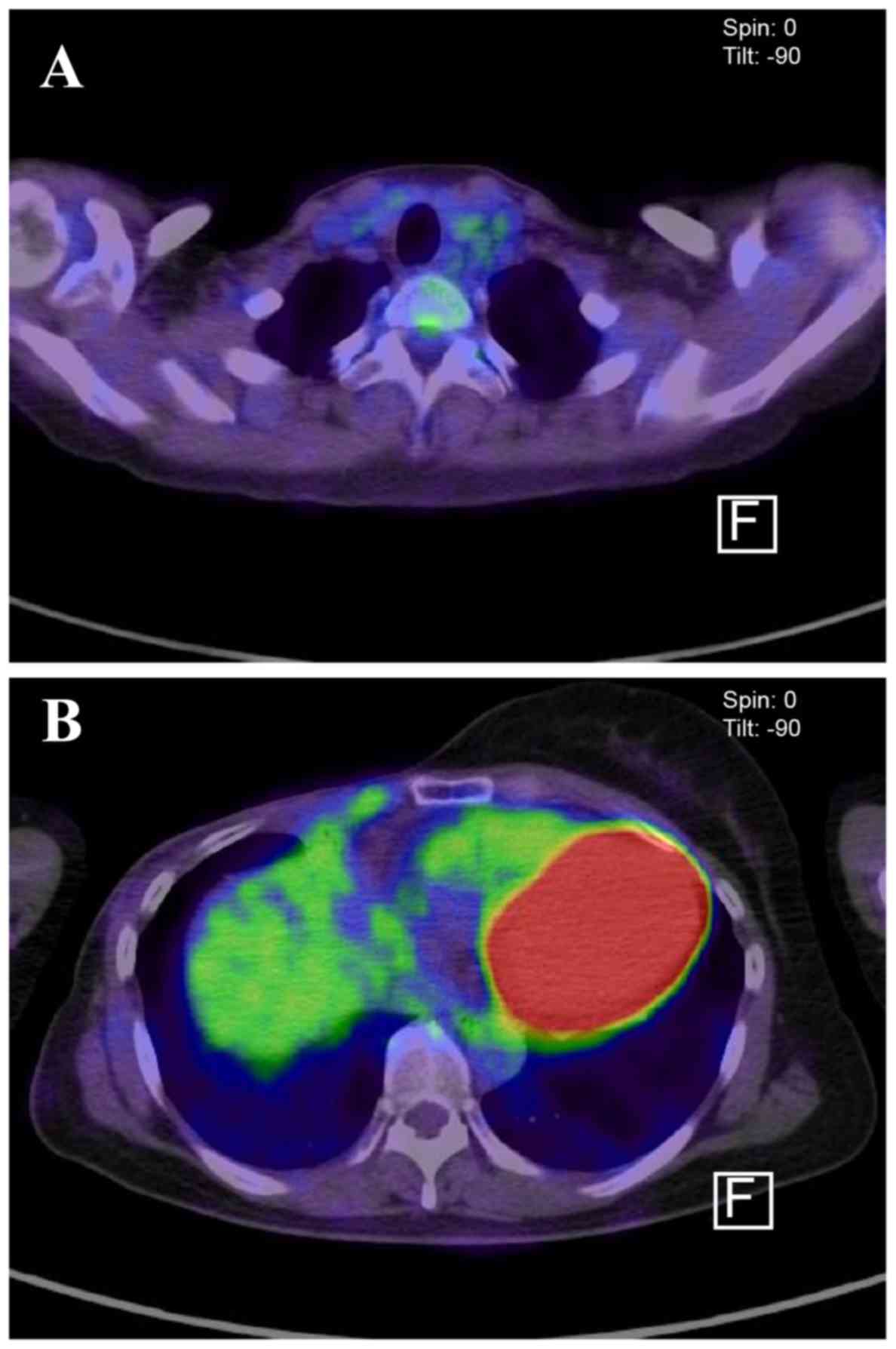
disappeared, as demonstrated on a CT examination. No metastatic
lymph node or thoracic wall FDG accumulation was observed on PET-CT
11 months after treatment initiation (Fig. 4). After 17 months of treatment, the
patient remained metastasis-free. During those 17 months, no major
side effects were observed although peripheral neuropathy not
affecting daily life grade 1 peripheral neurotoxicity occurred.
Discussion
It is generally recommended that the protocols for
the treatment of invasive ductal carcinoma of breast cancer are
applied for the treatment of squamous cell carcinoma. However, poor
efficacy of chemotherapy in recurrent carcinomas, including
squamous cell carcinoma, has been reported to date. While previous
studies have reported the use of anthracyclines and taxanes, to the
best of our knowledge, there are yet no published reports on the
efficacy of eribulin. We herein discuss the possible reasons for
the observed effectiveness of eribulin in the treatment of
metaplastic breast carcinoma.
In addition to its effectiveness against the
epithelial component, it is possible that eribulin is also
effective against the mesenchymal component of the carcinoma. Drug
regimens including adriamycin, which is also indicated for soft
tissue tumors with a mesenchymal component, have been reported to
significantly prolong progression-free survival in metaplastic
carcinomas compared with other regimens. Reduced incidence of
hepatic metastasis has also been reported with the use of
ifosfamide and etoposide, which are used for treating soft tissue
tumors (6). In Study 309, eribulin
was found to be effective against liposarcoma or leiomyosarcoma
(7). Eribulin promotes DNA repair,
the inhibition of which is characteristic of metaplastic
carcinomas, and is thus considered a more effective therapeutic
agent compared with adriamycin, of which the primary mechanism of
action involves the inhibition of DNA synthesis.
Furthermore, in metaplastic carcinomas, tumors
including squamous epithelial and sarcomatous components exhibit
increased expression of TWIST and SNAIL 2 transcription factors,
suggesting an association with epithelial-to-mesenchymal transition
(EMT) (8,9). Reports indicate that the occurrence of
EMT in cancer cells coincides with the development of resistance to
various anticancer agents. Several anticancer agents have been
reported to induce EMT and are considered to be involved in drug
resistance. Albeit in an in vitro study, eribulin has been
shown to inhibit Smad 2 and Smad 3 phosphorylation via transforming
growth factor-β induction or MET inhibition. These characteristic
mechanisms of action of eribulin are considered to contribute to
the effectiveness of the therapy in the present case.
Acknowledgements
The authors would like to thank Shiro Sugihara for
the pathological examinations and interpretations.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
YG designed the study and wrote the initial draft of
the manuscript. TY contributed to the analysis and interpretation
of data and assisted in the preparation of the manuscript. MK
critically reviewed the manuscript. All authors have read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
The study was conducted in accordance with the
principles of the Declaration of Helsinki.
Patient consent for publication
This patient and her family were informed that the
data from her case would be submitted for publication and provided
written informed consent.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
CEF
|
cyclophosphamide-epirubicin-fluorouracil
|
|
FDG-PET/CT
|
fluorodeoxyglucose positron emission
tomography-computed tomography
|
|
EMT
|
epithelial-to-mesenchymal
transition
|
|
TGF-β
|
transforming growth factor-β
|
References
|
1
|
Rayson D, Adjei AA, Suman VJ, Wold LE and
Ingle JN: Metaplastic breast cancer: prognosis and response to
systemic therapy. Ann Oncol. 10:413–419. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pezzi CM, Patel-Parekh L, Cole K, Franko
J, Klimberg VS and Bland K: Characteristics and treatment of
metaplastic breast cancer: analysis of 892 cases from the National
Cancer Data Base. Ann Surg Oncol. 14:166–173. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lee H, Jung SY, Ro JY, Kwon Y, Sohn JH,
Park IH, Lee KS, Lee S, Kim SW, et al: Metaplastic breast cancer:
clinicopathological features and its prognosis. J Clin Pathol.
65:441–446. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chen IC, Lin CH, Huang CS, Lien HC, Hsu C,
Kuo WH, Lu YS, Cheng AL, et al: Lack of efficacy to systemic
chemotherapy for treatment of metaplastic carcinoma of the breast
in the modern era. Breast Cancer Res Treat. 130:345–351. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Abouharb S and Moulder S: Metaplastic
breast cancer: clinical overview and molecular aberrations for
potential targeted therapy. Curr Oncol Rep. 17:4312015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Brown-Glaberman U, Graham A and Stopeck A:
A case of metaplastic carcinoma of the breast responsive to
chemotherapy with Ifosfamide and Etoposide: improved antitumor
response by targeting sarcomatous features. Breast J J. 16:663–665.
2010. View Article : Google Scholar
|
|
7
|
Schoffski P, Chawla S, Maki RG, Italiano
A, Gelderblom H, Choy E, Grignani G, Camargo V, Bauer S, et al:
Eribulin versus dacarbazine in previously treated patients with
advanced liposarcoma or leiomyosarcoma: a randomised, open-label,
multicentre, phase 3 trial. Lancet. 387:1629–1637. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Karreth F and Tuveson DA: Twist induces an
epithelial-mesenchymal transition to facilitate tumor metastasis.
Cancer Biol Ther. 3:1058–1059. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Valsesia-Wittmann S, Magdeleine M,
Dupasquier S, Garin E, Jallas AC, Combaret V, Krause A, Leissner P
and Puisieux A: Oncogenic cooperation between H-Twist and N-Myc
overrides failsafe programs in cancer cells. Cancer Cell.
6:625–630. 2004. View Article : Google Scholar : PubMed/NCBI
|