Introduction
More than 50% of all cases of pancreatic ductal
adenocarcinoma (PDAC) are initially considered unresectable (UR)
(1), and the standard treatment for
locally advanced unresectable (UR-LA) PDAC is chemo-radiotherapy
(2). Even if an effective regimen,
such as combination therapy with gemcitabine and nab-paclitaxel
(GnP), is administered, the median overall survival (OS) is only
8.5 months (3). Recent case reports
and retrospective studies of chemo-radiotherapy prior to surgery,
i.e., conversion surgery, for UR PDAC have been published (4,5), and the
significance of conversion surgery is now being evaluated. This
report describes a case of successful conversion surgery after GnP
therapy for UR-LA PDAC.
Case report
A 43-year-old woman was referred to the Department
of General Surgery, Chiba University Hospital (Chiba, Japan) from a
local hospital with the complaint of back pain. Initial laboratory
findings showed a high level of cancer antigen 19-9 (CA 19-9), at
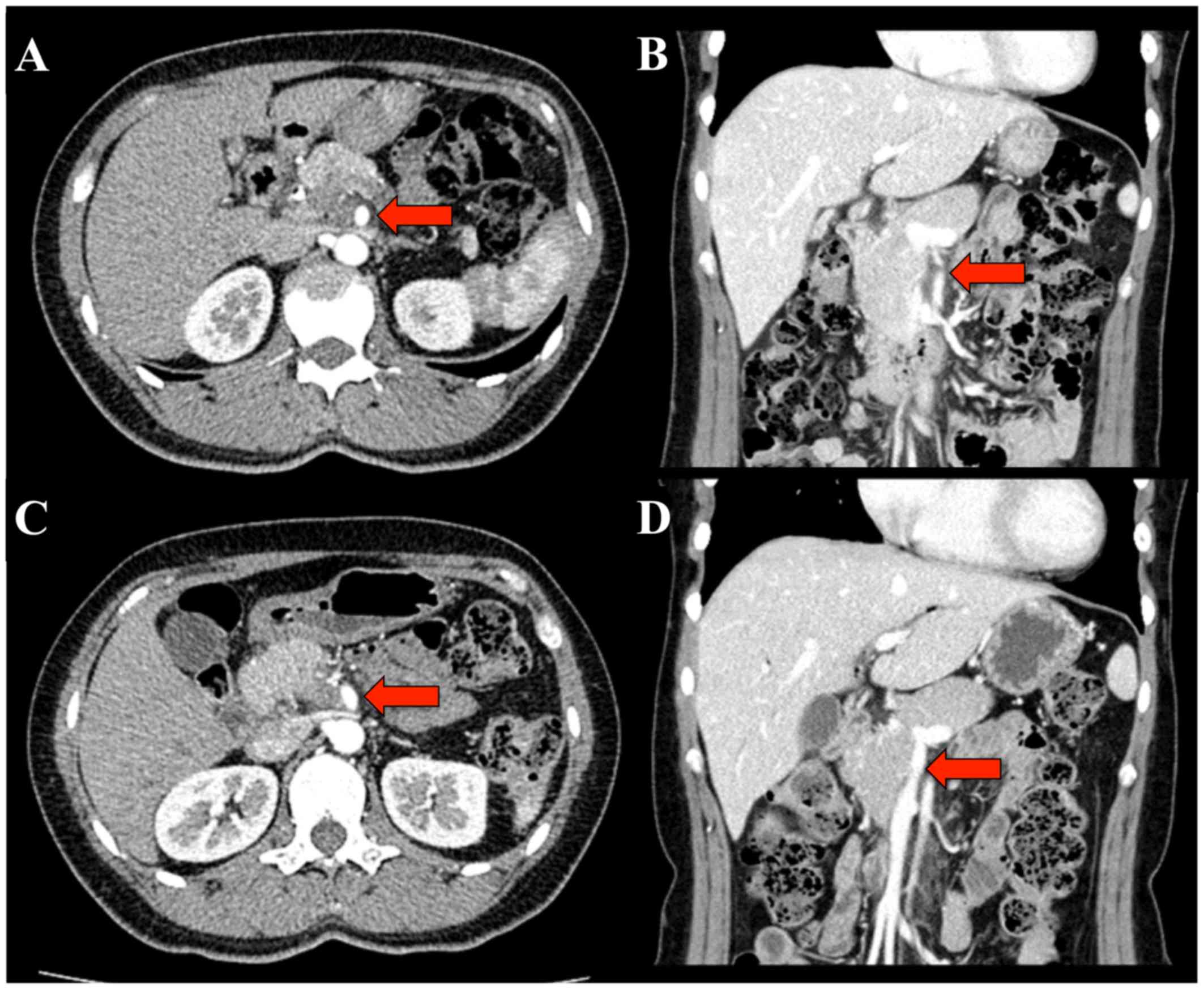
205.7 U/ml. Abdominal computed tomography (CT) revealed a
hypovascular tumor measuring 24 mm in the head of the pancreas. The
tumor was in contact with more than 270 degrees of the superior
mesenteric artery (SMA) perimeter, with invasion extending from the
superior mesenteric vein (SMV) to the portal vein (PV) (the
longitudinal axis was 30 mm) (Fig. 1A
and B). Endoscopic ultrasonography (EUS) indicated that the
tumor was in contact with >180 degrees of the SMA perimeter, and
the histological finding of fine needle aspiration biopsy was
adenocarcinoma. Both positron emission tomography (PET) and
ethoxybenzyl-magnetic resonance imaging (MRI) showed no evidence of
distant metastasis.
On the basis of these clinical findings, the patient
was diagnosed with UR-LA PDAC, and subsequently treated with a
combined chemotherapy regimen of gemcitabine (GEM, 1,000
mg/m2) and nab-paclitaxel (125 mg/m2), aimed
at conversion surgery. This combination chemotherapy was
intravenously administered on days 1 and 8 and repeated every 3
weeks. After 12 courses of combination chemotherapy for 9 months,
CT and EUS imaging demonstrated an effective response to
chemotherapy. The tumor size decreased to 20 mm and the contact
with the SMA was reduced to 90 degrees (Fig. 1C). The length of tumor invasion to
the SMV decreased from 30 to 15 mm in the longitudinal axis
(Fig. 1D). EUS examination also
showed that the extent of tumor invasion to the SMA and SMV had
decreased. Preoperative stage was T4N2M0 stage III according to the
8th edition of the UICC (International Union Against Cancer)-TNM
classification (6). Furthermore, the
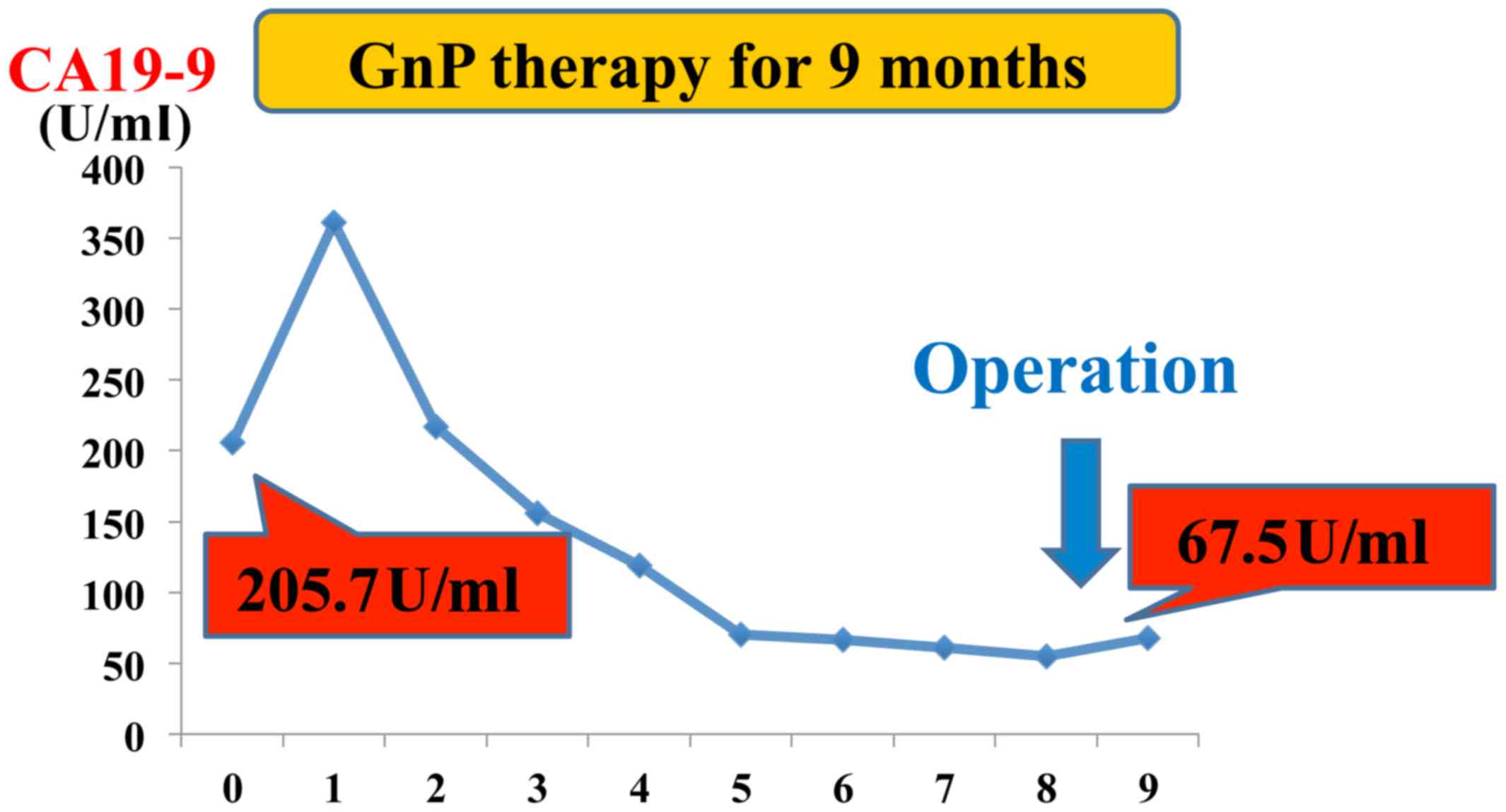
level of CA 19-9 decreased from 205.7 to 67.5 U/ml (Fig. 2). The radiological efficacy of
chemotherapy was stable disease (SD) on the Response Evaluation
Criteria in Solid Tumors (RECIST) (7). After discussion with the patient and
her family, conversion surgery was planned.
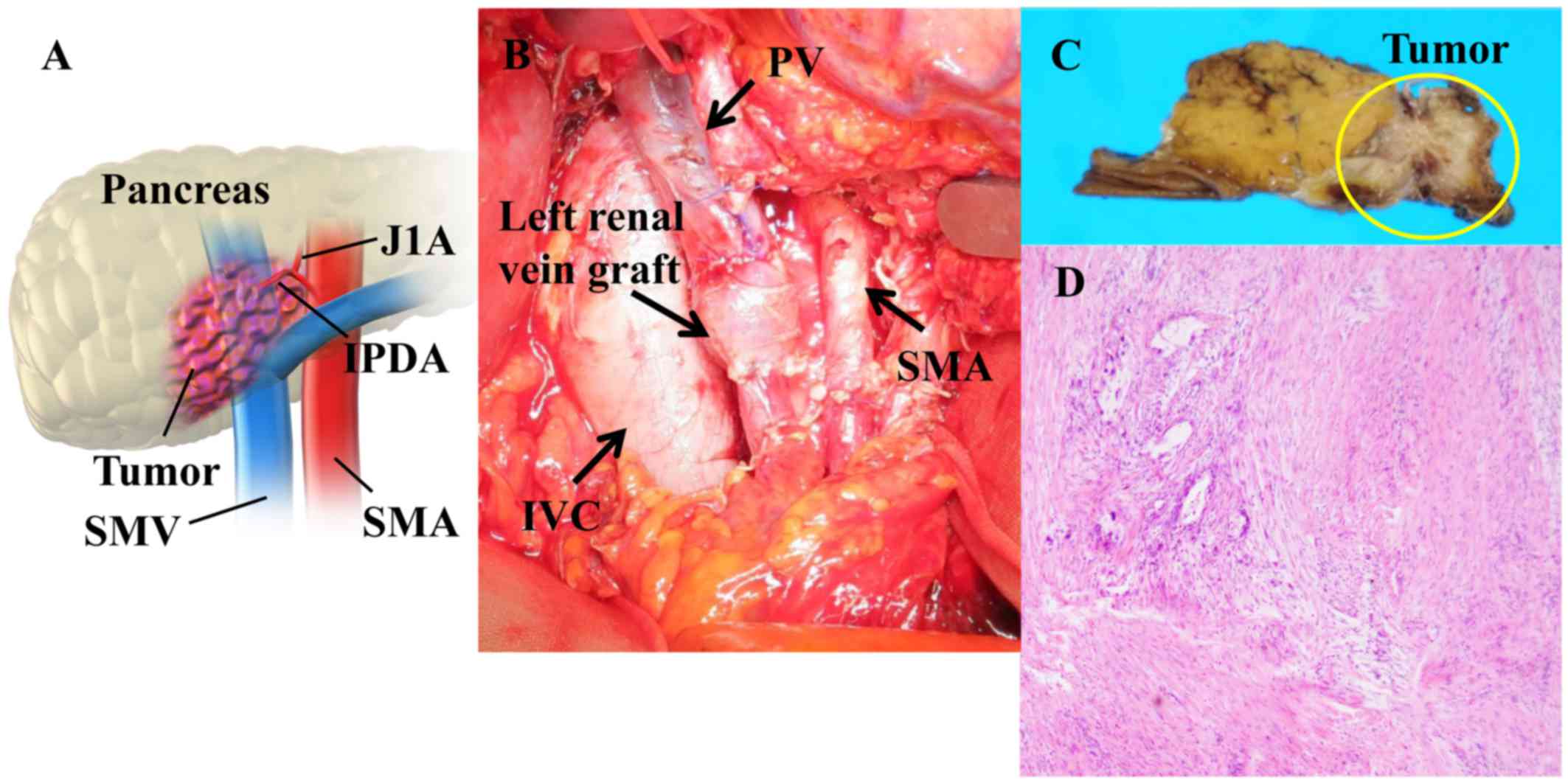
Pancreaticoduodenectomy with portal vein resection
and reconstruction using a left renal vein graft were performed
(8) (Fig.
3A and B). The margins of the bile duct and stump of the
pancreas were negative for cancer on intraoperative pathological
diagnosis of a frozen section. Microscopic pathological examination
showed R0 (no residual tumor) resection, and 10–50% of the tumor
cells were replaced with fibrosis (Evans' criteria IIa) (9). Based on the pathological findings
(moderately differentiated tubular adenocarcinoma, pT2 (24 mm), pN2
(4/32), pM0), the tumor was defined as stage III (Fig. 3C). After surgery, the patient showed
bleeding from the ligated inferior pancreatic duodenal artery due
to a pancreatic fistula (grade C) (10). Embolization with coiling and
reoperation (remnant pancreatectomy) were performed to stop
bleeding. The patient made a satisfactory recovery and was
discharged on postoperative day 53. The patient is alive at 19
months after initial treatment (9 months after surgery), but with
local tumor recurrence.
Discussion
Chemotherapy for PDAC has advanced since gemcitabine
was introduced (11). The MPACT
trial demonstrated the effectiveness of GnP therapy for UR PDAC
(3). Ueno et al reported that
GnP therapy (response rate: 69.2%) shows better efficacy compared
to gemcitabine or gemcitabine plus S-1 therapy (response rate: 30%)
for patients with UR PDAC (12,13). To
utilize these chemotherapies before surgery, it is possible to
exclude the cases showing aggressive growth or having distant
metastasis afterward. The selection of patients with a good
response to chemotherapy is important for successful conversion
surgery in UR PDAC. Satoi et al demonstrated that the median
OS of patients with UR PDAC treated with conversion surgery after
gemcitabine or S-1 therapy was significantly improved compared to
that with chemotherapy alone (39.7 vs. 20.8 months, respectively;
P<0.001) (14). Furthermore,
Ielpo et al reported that OS of patients treated with
conversion surgery with GnP therapy for resectable or borderline
resectable (BR) PDAC was significantly improved compared to that
with chemotherapy alone (21 vs. 12.5 months, respectively;
P<0.0002) (15). Taken together,
these results suggest that GnP therapy is one of the most useful
options for the treatment of UR-LA PDAC and is expected to improve
prognosis when followed by conversion surgery.
Recent cases of conversion surgery with GnP therapy
for UR-LA PDAC have been reported. Saito et al demonstrated
that the median OS of patients with UR-LA PDAC treated with
conversion surgery after GnP therapy was 13.3 months in a
retrospective study (5). FOLFIRINOX
(5-fluorouracil/leucovorin combined with irinotecan and
oxaliplatin) is another effective chemotherapeutic regimen to UR
PDAC (16). Suker et al
demonstrated that the median OS of patients with UR-LA PDAC treated
with conversion surgery after FOLFIRINOX therapy was 24.2 months in
a systematic review (17). Based on
the efficacy of chemotherapy, the use of conversion surgery for
UR-LA PDAC will likely increase. However, it is important to
determine whether the soft tissue around major vessels such as the
SMA is truly involved with tumor invasion. Therefore, it is
difficult to make a decision to convert treatment from chemotherapy
to surgery solely on the basis of radiological examination. A
retrospective cohort study reported that a >50% decrease in
pretreatment CA 19-9 levels after chemotherapy resulted in improved
OS, compared to that with a ≤50% decrease (28.0 vs. 11.1 months;
P<0.0001) (18). Thus, the CA
19-9 level should be taken into account in the evaluation of
chemotherapy efficacy.
We performed GnP therapy in 10 consecutive cases of
UR-LA PDAC between March 2015 and February 2016 in the Department
of General Surgery, Chiba University Hospital. Although there is
still no definite surgical indication for conversion surgery during
multidisciplinary treatment in patients with initially UR PDAC, the
following points were considered; i) tumor shrinkage from UR to
resectable or BR PDAC on radiological examinations, ii) serum CA
19-9 level is clearly decreased, and iii) good performance status.
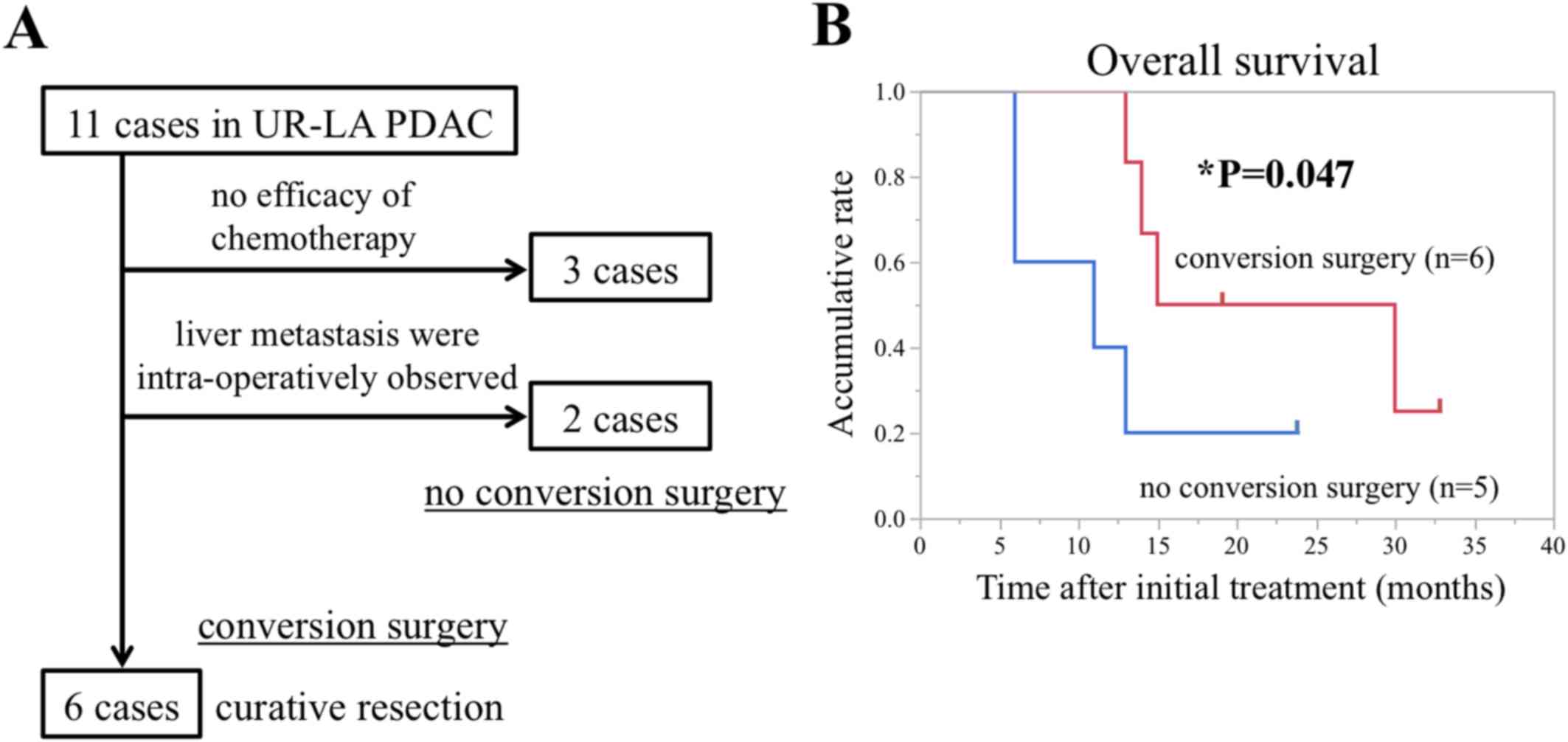
Adding the present case to these 10 cases, 3 of the 11 cases (27%)
were not converted to resection because chemotherapy was
ineffective, while 6 of 11 cases (55%) excluding 2 cases which
intra-operatively showed liver metastases in successfully underwent
conversion surgery with curative resection (Fig. 4A). In this retrospective cohort
study, the Kaplan-Meier analysis showed that patients treated with
conversion surgery presented significantly longer overall survival
(OS) than those treated with no conversion surgery (the median OS:
22.5 vs. 11 months, P=0.047, Wilcoxon test; Fig. 4B). The average duration of
chemotherapy before conversion surgery was 4.3 months and the
minimum reduction rate of CA 19-9 was 67% among 6 curative
resection cases (Table I). The rate
of R0 resection was 83% (Table II).
Based on these clinical data, a significant decrease in CA 19-9
levels might be useful in determining the time of changeover from
medicine to surgery in patients with UR-LA PDAC in whom conversion
surgery is being considered.
 | Table I.Preoperative characteristics of
locally advanced unresectable pancreatic ductal adenocarcinoma
patients preparing for conversion surgery with GnP therapy. |
Table I.
Preoperative characteristics of
locally advanced unresectable pancreatic ductal adenocarcinoma
patients preparing for conversion surgery with GnP therapy.
| No. | Age/gender | Location | Factors determining
unresectability | Period of Tx
(months) | CA19-9 (before Tx)
(U/ml) | CA19-9 (after Tx)
(U/ml) | Reduction rate of
CA19-9 (%) | RECIST |
|---|
| 1 | 61/M | Head | Contact with SMA
360° | 5 | 0.8 | 0.1 | 87.5 | PR |
| 2 | 56/F | Head | Contact with CHA with
extension to hepatic artery bifurcation | 3.9 | 150.4 | 35.2 | 76.6 | PR |
| 3 | 45/M | Body | Contact with CEA | 2.4 | 2909 | 884 | 69.6 | SD |
| 4 | 71/M | Body | Contact with SMA and
CEA | 1.4 | 165.7 | 35.4 | 78.0 | SD |
| 5 | 77/M | Head | Contact with SMA
>270° | 3.8 | 726.0 | 51.3 | 92.8 | PR |
| Present case | 43/M | Head | Contact with SMA
>270° | 9 | 205.7 | 67.5 | 67.1 | SD |
 | Table II.Clinical characteristics and outcomes
of locally advanced unresectable pancreatic ductal adenocarcinoma
in patients who underwent conversion surgery following gemcitabine
plus nab-paclitaxel therapy. |
Table II.
Clinical characteristics and outcomes
of locally advanced unresectable pancreatic ductal adenocarcinoma
in patients who underwent conversion surgery following gemcitabine
plus nab-paclitaxel therapy.
| No. | Operation method | Curability | Evans' criteria | OS from initial
treatment (months) | Survival |
|---|
| 1 | PD | R0 | IIa | 14 | No |
| 2 | PD-CAR, PVR | R0 | I | 33 | Yes |
| 3 | DP-CAR, PVR | R0 | IIa | 30 | No |
| 4 | DP-CAR | R0 | IIa | 15 | No |
| 5 | PD, PVR | R1 | IIa | 16 | No |
| Present case | PD, PVR | R0 | IIa | 19 | Yes |
In conclusions, we described a case of successful
conversion surgery with gemcitabine plus nab-paclitaxel for UR-LA
PDAC. GnP therapy decreased the level of CA 19-9, enabling surgical
resection. Conversion surgery after GnP therapy is a useful
treatment option for UR-LA PDAC. Further evidence and prospective
cohort studies are required to establish the optimal strategy for
treatment of UR-LA PDAC.
Acknowledgements
The authors would like to thank Dr Sugiura
(Department of Pathology, Chiba University Hospital) for their
assistance and the pathological information provided regarding the
chemotherapeutic effects.
Funding
This study was supported by the Grant-in-Aid for
Scientific Research, the Challenge Exploratory Research (grant no.
16K15607) and KIBAN B (grant no. 17H04287).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
RO gathered the patient's data and wrote the
manuscript. ST treated the patient with preoperative and adjuvant
chemotherapy. ST, TY, and MM performed the surgery. TM and MO were
responsible for the pathological diagnosis of the case. ST, TY, HY,
KF, TT, SaK, DS, NS, ShK, HN, MM and MO discussed and analyzed the
data with RO and assisted in writing the manuscript. All authors
approved the final manuscript.
Ethics approval and consent to
participate
The Ethics Committees of Chiba University approved
the content of this manuscript (approval no. 2732) and written
informed consent was obtained from each patient prior to
surgery.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of this case report and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
BR
|
borderline resectable
|
|
CA19-9
|
cancer antigen 19-9
|
|
CT
|
computed tomography
|
|
EUS
|
endoscopic ultrasonography
|
|
GnP
|
gemcitabine plus nab-paclitaxel
|
|
MST
|
median survival time
|
|
OS
|
overall survival
|
|
PET
|
positron emission tomography
|
|
PDAC
|
pancreatic ductal adenocarcinoma
|
|
PV
|
portal vein
|
|
SMA
|
superior mesenteric artery
|
|
SMV
|
superior mesenteric vein
|
|
UR-LA
|
locally advanced unresectable
|
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2017. CA Cancer J Clin. 67:7–30. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tempero MA, Malafa MP, Al-Hawary M, Asbun
H, Bain A, Behrman SW, Betnson AB III, Binder E, Cardin DB, Cha C,
et al: Pancreatic adenocarcinoma, version 2. 2017. NCCN clinical
practice guidelines in oncology. J Natl Compr Canc Netw.
15:1028–1061. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Von Hoff DD, Ervin T, Arena FP, Chiorean
EG, Infante J, Moore M, Seay T, Tjulandin SA, Ma WW, Saleh MN, et
al: Increased survival in pancreatic cancer with nab-paclitaxel
plus gemcitabine. N Engl J Med. 369:1691–1703. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hiyoshi M, Nanashima A, Wada T,
Tsuchimochi Y, Hamada T, Yano K, Imamura N and Fujii Y: A
successful case of locally advanced pancreatic cancer undergoing
curative distal pancreatectomy with en bloc celiac axis resection
after combination chemotherapy of nab-paclitaxel with gemcitabine.
Clin J Gastroenterol. 10:551–557. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Saito T, Ishido K, Kudo N, Kimura N,
Wakiya T, Nakayama Y and Hakamada K: Combination therapy with
gemcitabine and nab-paclitaxel for locally advanced unresectable
pancreatic cancer. Mol Clin Oncol. 6:963–967. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Brierley JD, Gospodarowicz MK and
Wittekind C: TNM Classification of Malignant Tumors (8th edition).
Wiley-Blackwell; New York: 2017
|
|
7
|
Eisenhauer EA, Therasse P, Bogaerts J,
Schwartz LH, Sargent D, Ford R, Dancy J, Arbuck S, Gwyther S,
Mooney M, et al: New response evaluation criteria in solid tumors:
Revised RECIST guideline (version 1.1). Eur J Cancer. 45:228–247.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Miyazaki M, Itoh H, Kaiho T, Ambiru S,
Togawa A, Sasada K, Shiobara M, Shimizu Y, Yoshioka S, Yoshitome H,
et al: Portal vein reconstruction at the hepatic hilus using a left
renal vein graft. J Am Coll Surg. 180:497–498. 1995.PubMed/NCBI
|
|
9
|
Evans DB, Rich TA, Byrd DR, Cleary KR,
Connelly JH, Levin B, Charnsangavej C, Fenoglio CJ and Ames FC:
Preoperative chemoradiation and pancreaticoduodenectomy for
adenocarcinoma of the pancreas. Arch Surg. 127:1335–1339. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bassi C, Marchegiani G, Dervenis C, Sarr
M, Hilal Abu M, Adham M, Allen P, Andersson R, Asbun HJ, Besselink
MG, et al: The 2016 update of the International Study Group (ISGPS)
definition and grading of postoperative pancreatic fistula: 11
years after. Surgery. 161:584–591. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Burris HA III, Moore MJ, Andersen J, Green
MR, Rothenberg ML, Modiano MR, Cripps MC, Portenoy RK, Storniolo
AM, Tarassoff P, et al: Improvements in survival and clinical
benefit with gemcitabine as first-line therapy for patients with
advanced pancreas cancer: A randomized trial. J Clin Oncol.
15:2403–2413. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ueno H, Ikeda M, Ueno M, Mizuno N, Ioka T,
Nakajima TE and Furuse J: Phase I/II study of nab-paclitaxel plus
gemcitabine for chemotherapy-naive Japanese patients with
metastatic pancreatic cancer. Cancer Chemother Pharmacol.
77:595–603. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ueno H, Ioka T, Ikeda M, Ohkawa S,
Yanagimoto H, Boku N, Fukutomi A, Sugimori K, Baba H, Yamao K, et
al: Randomized phase III study of gemcitabine plus S-1, S-1 alone,
or gemcitabine alone in patients with locally advanced and
metastatic pancreatic cancer in Japan and Taiwan: GEST study. J
Clin Oncol. 31:1640–1648. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Satoi S, Yamaue H, Kato K, Takahashi S,
Hirono S, Takeda S, Eguchi H, Sho M, Wada K, Shinchi H, et al: Role
of adjuvant surgery for patients with initially unresectable
pancreatic cancer with a long-term favorable response to
non-surgical anti-cancer treatments: Results of a project study for
pancreatic surgery by the Japanese Society of
Hepato-Biliary-Pancreatic Surgery. J Hepatobiliary Pancreat Sci.
20:590–600. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ielpo B, Duran H, Diaz E, Fabra I, Caruso
R, Ferri V, Malavé L, Hidalgo M, Alvarez R, Plaza C, et al:
Preoperative treatment with gemcitabine plus nab-paclitaxel is a
safe and effective chemotherapy for pancreatic adenocarcinoma. Eur
J Surg Oncol. 42:1394–1400. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Conroy T, Desseifne F, Ychou M, Bouché O,
Guimbaud R, Bécouarn Y, Adenis A, Raoul JL, Gourgou-Bourgade S, de
la Fouchardière C, et al: FOLFIRINOX versus gemcitabine for
metastatic pancreatic cancer. N Engl J Med. 364:1817–1825. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Suker M, Beumer BR, Sadot E, Marhey L,
Faris JE, Mellon EA, EI-Rayes BF, Wang-Gillam A, Lacy J, Hosein PJ,
et al: FOLFIRINOX for locally advanced pancreatic caner: A
systematic review and patient-lebel meta-analysis. Lancet Oncol.
17:801–810. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Boone BA, Steve J, Zenati MS, Hogg ME,
Singhi AD, Barlett DL, Zureikat AH, Bahary N and Zeh HJ III: Serum
CA 19-9 response to neoadjuvant therapy is associated with outcome
in pancreatic adenocarcinoma. Ann Surg Oncol. 21:4351–4358. 2014.
View Article : Google Scholar : PubMed/NCBI
|