Introduction
Transcatheter arterial chemoembolization (TACE) is
considered to be one of the most effective palliative measures for
patients with inoperable hepatocellular carcinoma (HCC). Recently,
TACE using the drug-eluting embolic microsphere DC Beads
(Biocompatibles, Farnham, UK) loaded with doxorubicin resulted in
better objective response rates with fewer systemic complications
compared with those in patients who underwent conventional TACE
procedures (1). Chemoembolization
with drug-eluting beads has the potential advantage of increasing
local, effective drug delivery, while reducing the systemic
bioavailability of the chemotherapeutic drug.
Rarely, extrahepatic organs may incur ischemic
damage, such as acute cholecystitis (2), necrosis of the epigastric skin
(3), interstitial pneumonitis
(4), gastrointestinal tract
ulceration (5) and acute
pancreatitis (6–9). The proposed mechanism underlying these
complications is inadvertent embolization through the collateral
vessels or regurgitation of the chemotherapeutic agent into the
arteries of other organs. However, only few reports have confirmed
the presence of embolic material in damaged organs on pathological
examination (3).
We herein present the case of a patient with HCC who
developed acute necrotizing pancreatitis as a fatal complication
following TACE with DC Beads. To the best of our knowledge, this is
the first report of an autopsy case due to acute necrotizing
pancreatitis after TACE using DC Beads.
Case report
An 85-year-old male patient with alcohol-related
cirrhosis (Child-Pugh class A) was admitted to the Kansai Medical
University Medical Center (Moriguchi, Japan) in April 2014 for
treatment of relapsed HCC. The patient had received three sessions
of TACE with lipiodol (conventional TACE) to treat HCC in segments
4 and 8, measuring ~70 mm in greatest diameter. After the last TACE
procedure 3 months earlier, contrast-enhanced computed tomography
(CT) indicated that the tumor exhibited early arterial phase
enhancement. The laboratory findings were as follows: Hemoglobin,
11.5 g/dl; white blood cell count, 3,600/µl; platelet count,
174,000/µl; albumin, 4.0 g/dl; aspartate aminotransferase (AST), 25
IU/l; alanine transaminase (ALT), 10 IU/l; alkaline phosphatase,
333 IU/l; γ-glutamyltransferase, 28 IU/l; total bilirubin, 0.6
mg/dl; prothrombin time international normalized ratio (INR), 1.08;
α-fetoprotein, 3.4 ng/ml; and protein induced by vitamin K
absence/antagonist-II, 450 AU/l. Given the diagnosis of local
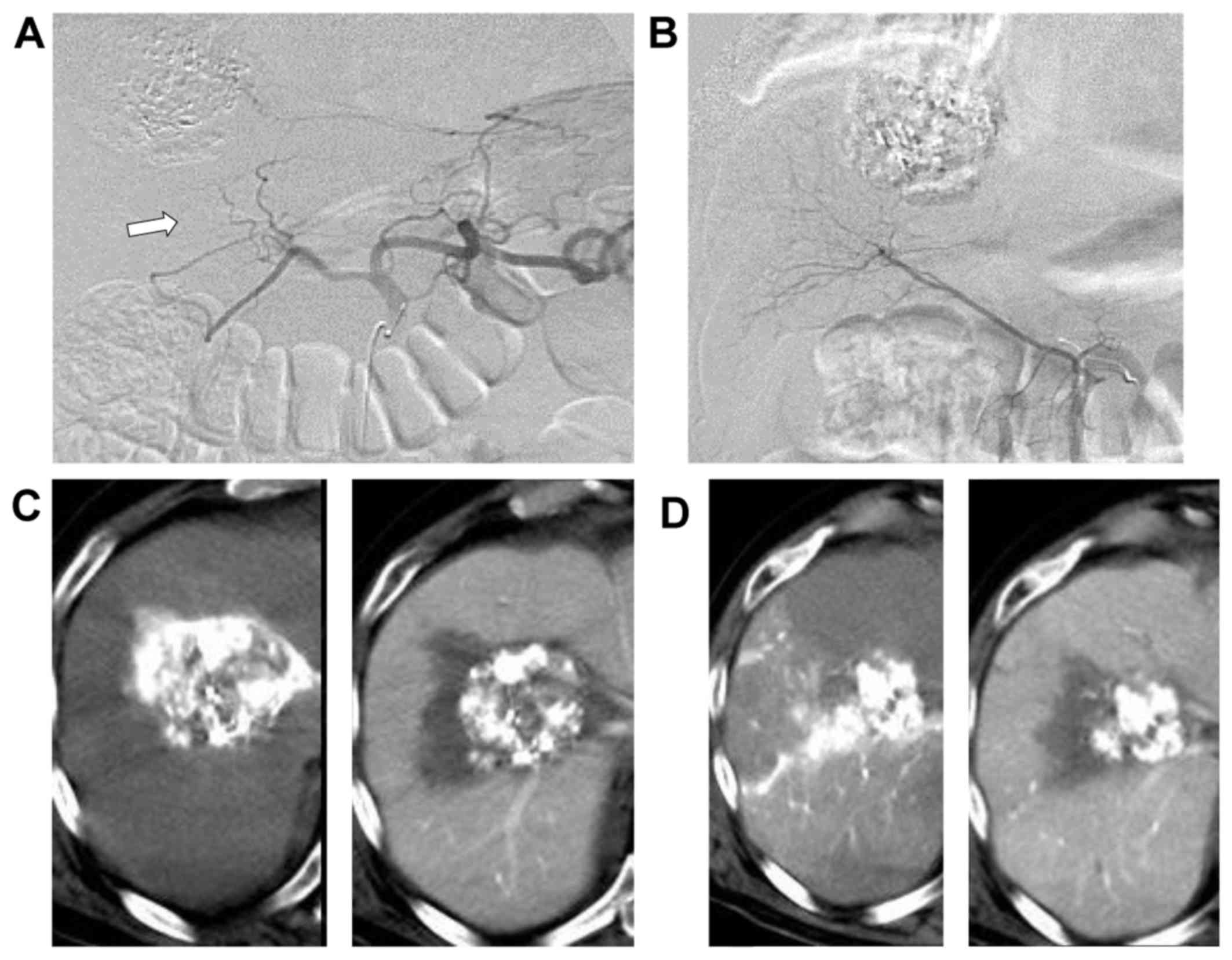
recurrence, TACE was performed. Hepatic arteriography demonstrated
replacement of the origin of the right hepatic artery to the
superior mesenteric artery, while the left hepatic artery
originated from the celiac artery (Fig.
1A and B). CT during hepatic arteriography demonstrated
hypervascular tumors in segments 4 and 8, which were fed by the
right hepatic artery and the medial segmental artery arising from
the left hepatic artery, respectively (Fig. 1C and D). After selection of the
segmental arterial branches feeding the tumors, 2 ml of
100–300-µm-sized DC Beads loaded with 150 mg epirubicin were
injected through the microcatheter, and successful embolization was
achieved with complete stasis of blood flow at the level of the
segmental arteries. Another arteriography performed after TACE
showed disappearance of blood flow within the peripheral branches
of the hepatic artery, but the flow through the gastroduodenal
artery (GDA) and its branches remained intact. A few hours after
the procedure, the patient complained of abdominal pain and vomited
a small amount of blood, and his laboratory results revealed
increased levels of AST (267 IU/l) and ALT (81 IU/l). The patient's
symptoms were treated conservatively with hydration, pain relief
and fever control, and they were consistent with post-embolization
syndrome. Three days after the procedure, the patient underwent
pan-endoscopy of the upper gastrointestinal tract and
contrast-enhanced CT. The liver enzyme levels were found to be
drastically increased, with an AST level of 2,538 IU/l and an ALT
level of 1,161 IU/l. The white blood cell count (5,100/µl)
C-reactive protein (31.7 mg/dl) and serum amylase (865 IU/l) levels
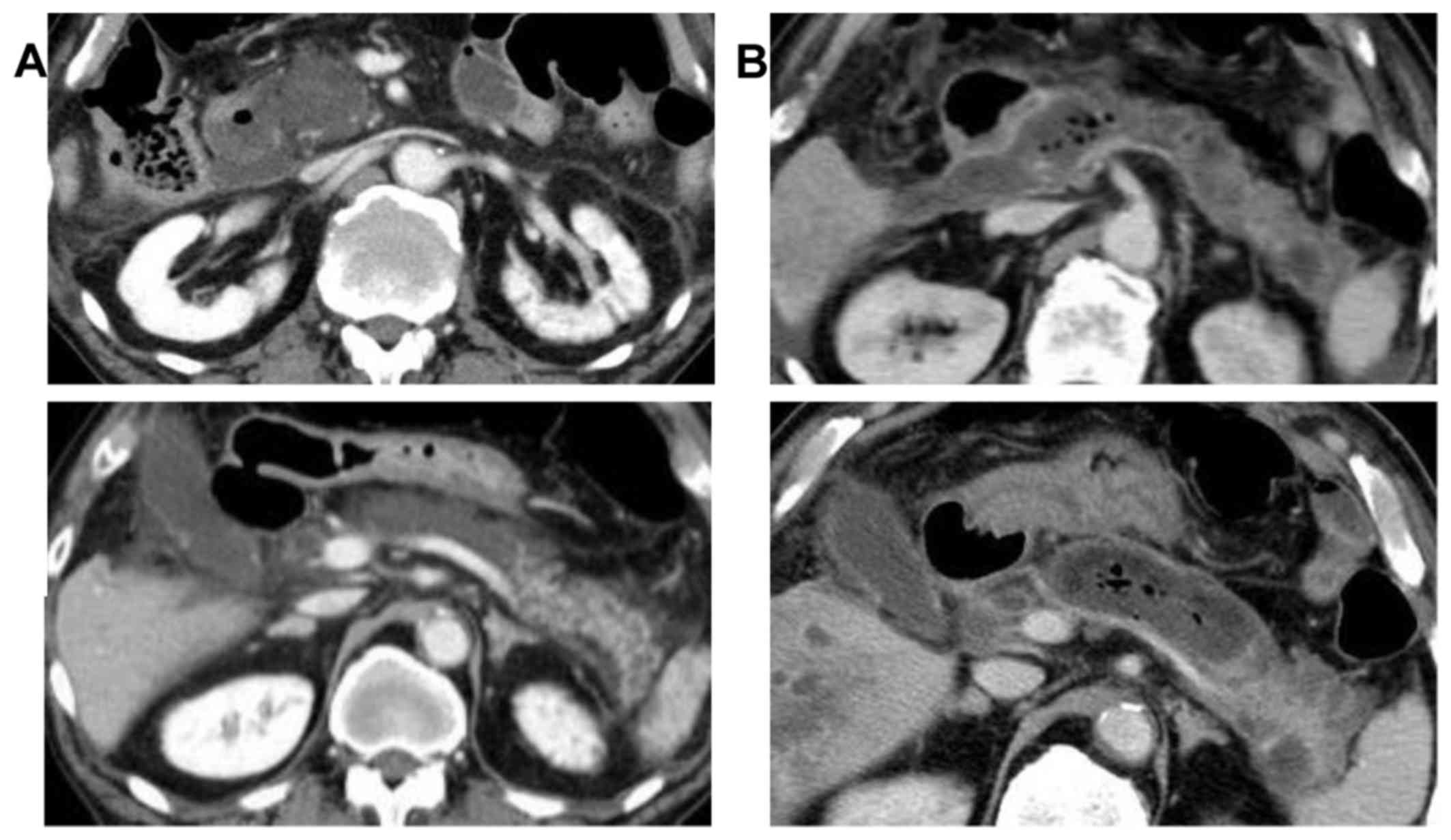
were also elevated. The contrast-enhanced CT revealed swelling of
the pancreas and focal areas of low density in the pancreatic body,
suggesting necrosis (Fig. 2A),
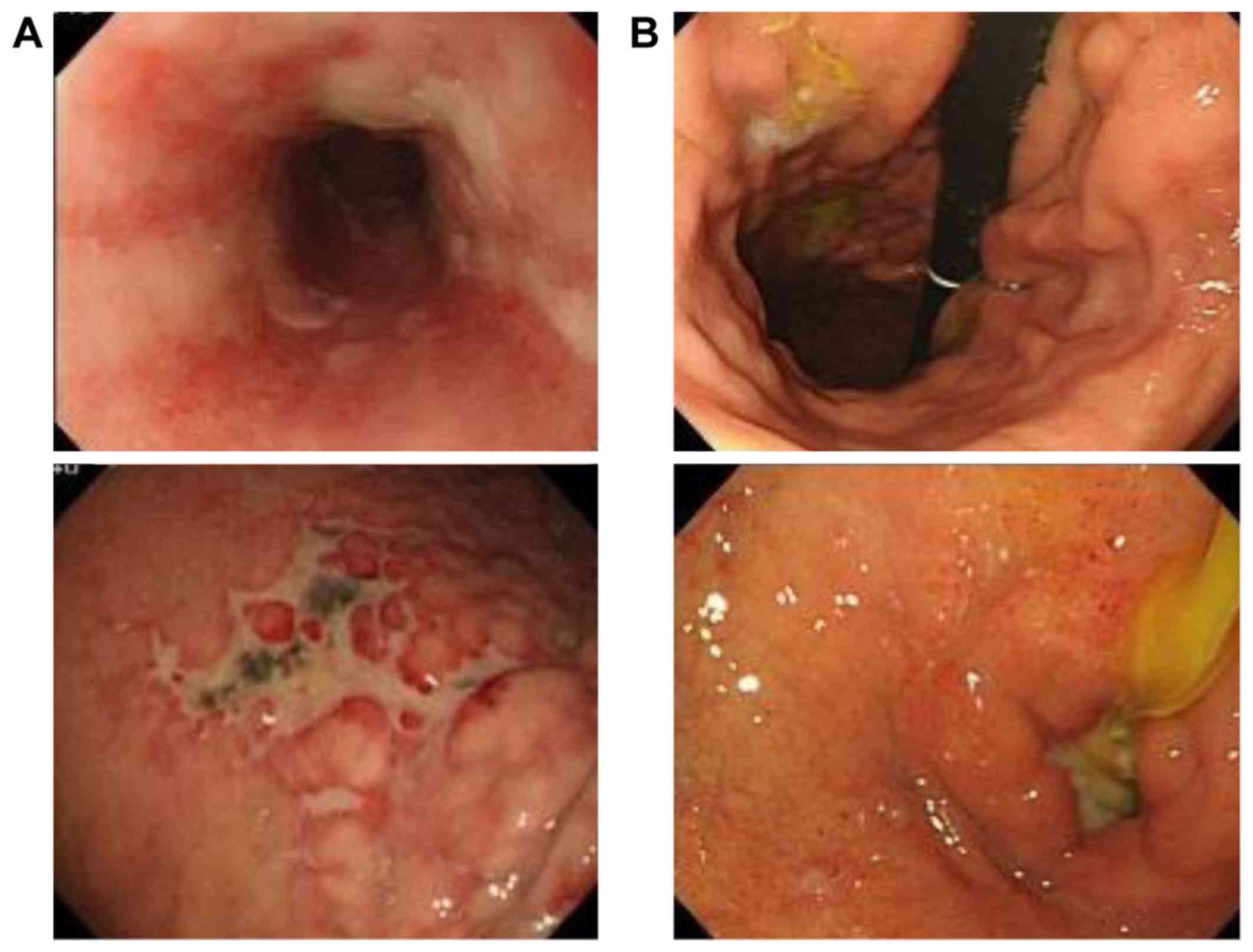
whereas upper gastrointestinal endoscopic examination revealed
longitudinal ulcers from the esophagus to the duodenum (Fig. 3A). The patient was treated for 2
weeks with general management of acute pancreatitis, including pain
control, hydration, fasting and total parenteral nutrition.
However, the follow-up abdominal CT revealed peripancreatic fluid
collection, with a thick, enhancing wall, suggesting necrotizing
pancreatitis and an infected pseudocyst (Fig. 2B); the follow-up upper
gastrointestinal endoscopy revealed purulent discharge from the
duodenum (Fig. 3B). Drainage or
surgical resection was not performed due to the poor general
condition of the patient. He developed respiratory insufficiency,
renal failure and sepsis, and eventually succumbed to the
complications 54 days after the procedure. An autopsy was conducted
with the consent of the patient's family.
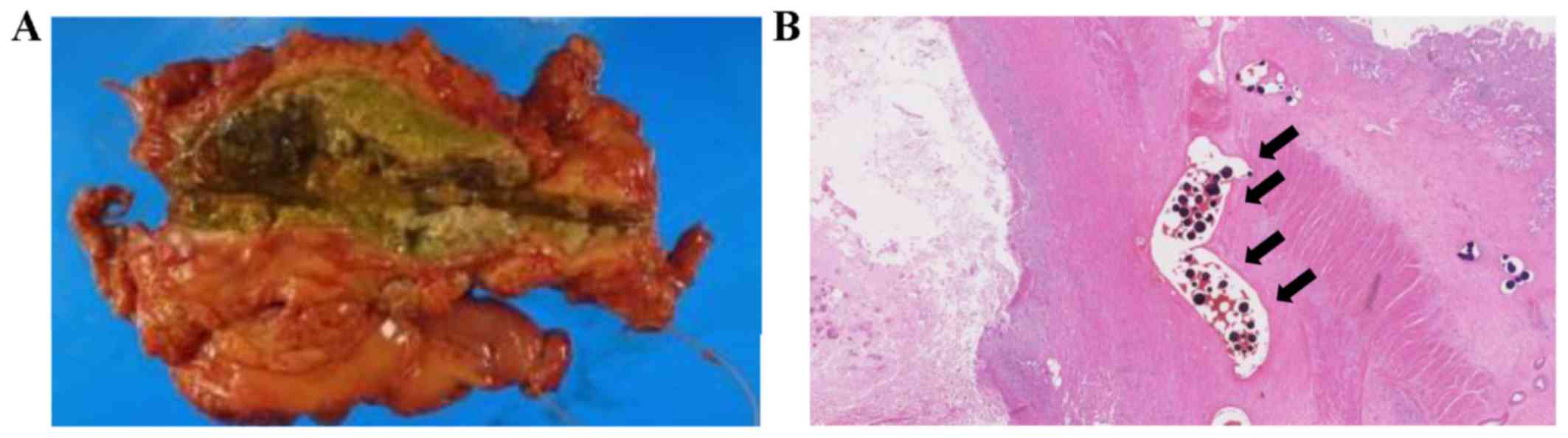
The autopsy revealed necrosis of most of the hepatic
tumor and extensive pancreatic necrosis. The peripancreatic tissue
was also extensively necrotized, and the pancreatic head displayed
hemorrhagic necrosis (Fig. 4A),
involving both acinar and ductal cells, with an adjacent intense
acute inflammatory reaction. In the hepatic arteries and the GDA,
as well as the renal arteries, there was detection of scattered DC
Beads (Fig. 4B). According to the
pathologist, the patient's cause of death was extensive pancreatic
necrosis due to GDA embolism after TACE with DC Beads.
Discussion
Acute pancreatitis is a rare yet well-known
complication after TACE. It occurs in ~1.7–2% of all patients
following selective and superselective liver tumor embolization
(6). This complication results from
a retrograde injection of the chemotherapeutic, embolizing agent
into the pancreatic arteries, giving rise to ischemic pancreatitis
(8). To prevent this complication,
it is important to reduce the backflow of embolic material by
placing the catheter tip as close to the distal branches of the
hepatic artery as possible, and embolic materials should be
injected carefully to avoid regurgitation (7). From the variant arterial anatomy
aspect, when numerous vessels arise from a common trunk with early
bifurcation, this may affect the probability of developing ischemic
injury and the severity of the injury. Our patient exhibited
replacement of the origin of the right hepatic artery to the
superior mesenteric artery. The left hepatic and left gastric
arteries originated from the common hepatic artery in a linear
manner (Fig. 1A). These anatomical
characteristics are a cause of regurgitation; however, TACE
procedures may be safely completed with selective, slow, steady
injection into the left medial hepatic artery under fluoroscopic
monitoring. It is also possible that there is an association
between the frequency of this complication and the type of
particles used for the embolization, the volume of particles
(6), or the size of the tumor
(10). In addition, the procedure
must be performed with caution, as in patients with advanced
atherosclerosis, iatrogenic dissection of the GDA during the
procedure may cause acute pancreatitis from ischemia, since
anastomosis of the superior pancreaticoduodenal artery and the
superior mesenteric artery may be ineffective. However, vascular
injury was not observed on pathological examination in the present
case. The microscopic findings of the pancreas with the presence of
foreign body material confirmed that infusion of DC Beads through
the GDA may cause pancreatitis.
Post-TACE gastric lesions are also due to the
backflow of embolic materials into the gastric artery and a
subsequent decrease in gastric mucosal blood flow, which may cause
complications such as gastric erosion or ulceration. Certain
anatomical variations, such as the right gastric artery branching
distally from the hepatic artery proper or from its branch or the
accessory left gastric artery arising from the left hepatic artery,
are most likely to be associated with a high incidence of post-TACE
gastric lesions (5).
In conclusion, we herein report the case of a
patient with HCC who developed the fatal complication of acute
necrotizing pancreatitis following TACE with DC Beads. To the best
of our knowledge, this is the first report of an autopsy case due
to acute necrotizing pancreatitis after TACE using DC Beads.
Although the advantage of TACE with DC Beads is fewer symptoms of
post-embolization syndrome compared with lipiodol, DC Beads are
hardly visible under fluoroscopic monitoring; therefore, it is
difficult to identify the regurgitation of the DC Beads during the
procedure. Awareness of the complications following TACE with DC
Beads is crucial, particularly in patients with anatomical
variations.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during the present
study are included in this published article.
Authors' contributions
TY and TS designed the study. TY wrote the initial
draft of the manuscript. AK, RT, RI, MM and MY contributed to the
analysis and interpretation of data. All authors revised the
manuscript critically for important intellectual content and
approved the final version of the manuscript.
Ethics approval and consent to
participate
The patient's family provided written informed
consent for the autopsy.
Consent for publication
The patient's family provided written informed
consent for publication of the present study.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lammer J, Malagari K, Vogl T, Pilleul F,
Denys A, Watkinson A, Pitton M, Sergent G, Pfammatter T, Terraz S,
et al: PRECISION V Investigators: Prospective randomized study of
doxorubicin-eluting-bead embolization in the treatment of
hepatocellular carcinoma: Results of the PRECISION V study.
Cardiovasc Intervent Radiol. 33:41–52. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Karaman B, Battal B, Ören NC, Üstünsöz B
and Yağci G: Acute ischemic cholecystitis after transarterial
chemoembolization with drug-eluting beads. Clin Imaging.
36:861–864. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kim HY, Bae SH, Park CH, Song MJ, Choi JY,
Yoon SK, Jung ES and Chun HJ: Supraumbilical subcutaneous fat
necrosis after transcatheter arterial chemoembolization with
drug-eluting beads: Case report and review of the literature.
Cardiovasc Intervent Radiol. 36:276–279. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Aladdin M and Ilyas M: Chemoembolization
of hepatocellular carcinoma with drug-eluting beads complicated by
interstitial pneumonitis. Semin Intervent Radiol. 28:218–221. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Leung TK, Lee CM and Chen HC: Anatomic and
technical skill factor of gastroduodenal complication in
post-transarterial embolization for hepatocellular carcinoma: A
retrospective study of 280 cases. World J Gastroenterol.
11:1554–1557. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
López-Benítez R, Radeleff BA,
Barragán-Campos HM, Noeldge G, Grenacher L, Richter GM, Sauer P,
Buchler M, Kauffmann G and Hallscheidt PJ: Acute pancreatitis after
embolization of liver tumors: Frequency and associated risk
factors. Pancreatology. 7:53–62. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bae SI, Yeon JE, Lee JM, Kim JH, Lee HJ,
Lee SJ, Suh SJ, Yoon EL, Kim HR, Byun KS, et al: A case of
necrotizing pancreatitis subsequent to transcatheter arterial
chemoembolization in a patient with hepatocellular carcinoma. Clin
Mol Hepatol. 18:321–325. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Alcívar-Vásquez JM, Ontanilla-Clavijo G,
Ferrer-Ríos MT and Pascasio-Acevedo JM: Acute necrotizing
pancreatitis after transarterial chemoembolization of
hepatocellular carcinoma: An unusual complication. Rev Esp Enferm
Dig. 106:147–149. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Krishnamurthy P, Brown M, Agrawal S and
Short RF: Acute pancreatitis as a complication of trans-arterial
chemoembolization of hepatocellular cancer-case report and review
of literature. J Gastrointest Oncol. 8:E26–E30. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Malagari K, Pomoni M, Spyridopoulos TN,
Moschouris H, Kelekis A, Dourakis S, Alexopoulou E, Koskinas J,
Angelopoulos M, Kornezos J, et al: Safety profile of sequential
transcatheter chemoembolization with DC Bead™: Results of 237
hepatocellular carcinoma (HCC) patients. Cardiovasc Intervent
Radiol. 34:774–785. 2011. View Article : Google Scholar : PubMed/NCBI
|