Introduction
Skeletal tissues are among the most common sites of
metastases from cancers such as breast, prostate, thyroid and lung
carcinomas (1), and bone metastases
(BM) reportedly occur in 15–30% of patients with lung cancer
(2). BM strongly affect prognoses by
causing skeletal-related events (SREs), such as pathological
fracture, hypercalcaemia and spiral cord compression (3), and prevention of BM is a primary
objective of treatments for non-small cell lung cancers
(NSCLC).
Because osteoclasts induce bone resorption during
the progression of BM (4),
osteoclast inhibitors (OIs) are used as therapeutic agents, and
bisphosphonates (BPs) and denosumab are commonly used to suppress
SREs that are caused by BM. BPs are also commonly administered to
inhibit bone resorption in solid tumour patients with BM (5). Among these agents, Zoledronate (Zol)
has been shown to delay or reduce the incidence of SREs in several
solid tumours, including NSCLC (6).
Furthermore, previous studies suggest that treatments with Zol
improve overall survival (OS) and metastasis-free survival in NSCLC
patients with BM (7), presumably be
maintaining bone health. In addition, a recent study suggested that
a monoclonal antibody against receptor activator of nuclear factor
kappa-B ligand (RANKL), denosumab, is effective against NSCLC in
patients with BM (8). Moreover,
phase 3 trials of denosumab vs. Zol show significantly greater OS
after treatments with denosumab than with Zol among patients with
BM from lung cancers (9). These
studies warrant the use of OIs for the prevention of SREs.
In contrast with treatments for NSCLC patients with
BM, limited evidence is available to inform treatments for small
cell lung cancer (SCLC) patients with BM. SCLC is an aggressive
subtype of lung cancer and BM occurs in about 40% of extensive
stage (ES)-SCLC patients. Moreover, BM contributes to poor
prognoses among SCLC patients, as among NSCLC subjects, and OS of
patients with BM is demonstrably poorer than that of patients
without BM (10). However, no
published studies report the prognostic efficacy of OIs in SCLC
patient with BM.
Herein, we hypothesised that OIs prolong the
survival of ES-SCLC patients by preventing the onset of SREs and
reviewed the data from ES-SCLC patients with BM at Tokyo
Metropolitan Cancer and Infectious diseases Center Komagome
Hospital. Subsequently, we retrospectively evaluated the efficacy
of OIs in ES-SCLC patients with BM.
Materials and methods
Data acquisition
Data were retrospectively collected from records of
patients with ES-SCLC and BM who were admitted to Tokyo
Metropolitan Cancer and Infectious diseases Center Komagome
Hospital between 2008 and 2015. Among a total of 238 patients with
SCLC, 132 patients were diagnosed with ES-SCLC and 58 of these had
BM during the observation period and were enrolled in the study.
Records of sex, age, smoking history, Eastern Cooperative Oncology
Group scale performance status (ECOG PS) at the time of diagnosis
of lung cancer, serum lactate dehydrogenase (LDH), date of
treatment with OIs, date of onset of SREs, date of last follow up
and patient outcomes were reviewed, and patients were assigned to
treatment (Zol and/or denosumab, n=23) and non-treatment groups
(n=35). The decision of OIs treatment was based on physician's
choice. The patients received pre-therapy dental care to prevent
OIs related osteonecrosis of the jaw. OIs treatment was postponed
until the completion of dental surgery. SREs were used as a primary
outcome and included pathologic fracture, radiation to BM, surgery
to bone, spinal cord compression and hypercalcaemia. All study
protocols were approved by the Institutional Review Committee of
Tokyo Metropolitan Cancer and Infectious diseases Center Komagome
Hospital.
Statistical analysis
Descriptive statistics were used to summarise
baseline characteristics. OS was defined as the time from the date
of SCLC diagnosis to the date of death by any cause. Times to SREs
from BM were not determined because almost all patients in the OIs
group were treated after the onset of SREs. Categorical variables
were compared using Pearson's, chi-square or Fisher's exact tests.
Log-rank analyses were performed to compare OS using the
Kaplan-Meier method, and background intergroup differences were
minimised by calculating propensity scores based on patient
characteristics. P<0.05 was considered to indicate a
statistically significant difference. All statistical analyses were
performed using R version 3.2.2 (www.r-project.org/).
Results
Patients characteristics
Patient characteristics are summarised in Table I. The median age of patients was 70
years, and the median of Brinkman index was 1,080. SREs were
observed in 24 of 58 patients (41.4%), and 35 of 58 patients with
BM had never been treated been with OIs. The OIs group included 15
patients who were treated with ZOL and six who were treated with
denosumab. The remaining two patients were administrated Zol and
denosumab in combination. Palliative radiotherapy was the most
common (83.3%) SRE in patients with BM (Table II), and in comparisons of baseline
characteristics between groups (Table
III), SREs occurred more frequently in the control group than
in patients treated with OIs, presumably because OIs were often
administered after the incidence of SREs. In addition, recurrence
and loss to follow up rates differed between control and OIs
groups. To accommodate these differences, we performed propensity
score matching (PSM) for age, sex, serum LDH, PS (ECOG), smoking
history and recurrence, and subsequently found no significant
differences in the incidence of SREs between untreated and OIs
treated patients.
 | Table I.Baseline characteristics of small cell
lung cancer patients with bone metastases. |
Table I.
Baseline characteristics of small cell
lung cancer patients with bone metastases.
| Characteristics | No. of patients
(n) | % of total (n) |
|---|
| No. of patients | 58 |
|
| Age, years
(median) | 70 |
|
| Gender |
|
|
| Male | 47 | 81.0 |
|
Female | 11 | 18.9 |
| Smoking status |
|
|
|
Never-smoked | 1 | 1.7 |
|
Smoker | 48 | 82.8 |
| No
data | 9 |
|
| Brinkman
index (median) | 1,080 |
|
| ECOG performance
status |
|
|
| 0–1 | 29 | 50.0 |
| 2 | 9 | 15.5 |
| 3–4 | 17 | 29.3 |
| No
data | 3 |
|
| SREs |
|
|
| No | 30 | 51.7 |
| Yes | 24 | 41.4 |
| No
data | 4 |
|
| Serum LDH (U/l,
median) | 287 |
|
| Treatment of OIs |
|
|
| Never
treated | 35 | 60.3 |
| Zol | 15 | 25.9 |
|
Denosumab | 6 | 10.3 |
| Zol and
Denosumab | 2 | 3.4 |
 | Table II.Skeletal-related events in 24 of 58
extensive stage-small cell lung cancer patients with bone
metastasis |
Table II.
Skeletal-related events in 24 of 58
extensive stage-small cell lung cancer patients with bone
metastasis
| SRE | No. of patients
(n) | % of total (n) |
|---|
| Radiation to
bone | 20 | 83.3 |
| Spinal cord
compression | 4 | 16.7 |
| Pathologic
fracture | 3 | 12.5 |
| Hypercalcemia | 1 | 4.2 |
| Surgical
stabilization | 1 | 4.2 |
 | Table III.Baseline characteristics of patients
with and without osteoclast inhibitor treatments. |
Table III.
Baseline characteristics of patients
with and without osteoclast inhibitor treatments.
|
| Prior to PSM (n) | Following PSM
(n) |
|---|
|
|
|
|
|---|
| Characteristics | With OIs | Without OIs | P-value | With OIs | Without OIs | P-value |
|---|
| No. of patients | 23 | 35 |
| 19 | 19 |
|
| Age, years
(median) | 67 | 70 | 0.373 | 67 | 70 | 0.359 |
| Gender |
|
| 0.316 |
|
| 1 |
| Male | 17 | 30 |
| 15 | 15 |
|
|
Female | 6 | 5 |
| 4 | 4 |
|
| Smoking status |
|
| 0.961 |
|
| 0.364 |
|
Never-smoked | 0 | 1 |
| 0 | 1 |
|
|
Smoker | 20 | 28 |
| 19 | 18 |
|
| No
data | 3 | 6 |
| 0 | 0 |
|
|
Brinkman index (median) | 1,080 | 1,080 |
| 1,140 | 1,000 |
|
| ECOG performance
status |
|
| 0.092 |
|
| 0.145 |
|
0–1 | 14 | 15 |
| 12 | 8 |
|
| 2 | 3 | 6 |
| 2 | 3 |
|
|
3–4 | 5 | 12 |
| 5 | 8 |
|
| No
data | 1 | 2 |
| 0 | 0 |
|
| SREs |
|
| 0.027 |
|
| 0.310 |
| No | 8 | 22 |
| 8 | 10 |
|
|
Yes | 14 | 10 |
| 11 | 6 |
|
| No
data | 1 | 3 |
| 0 | 3 |
|
| Serum LDH (U/l,
median) | 297 | 271 | 0.511 | 288 | 256 | 0.839 |
Survival analysis
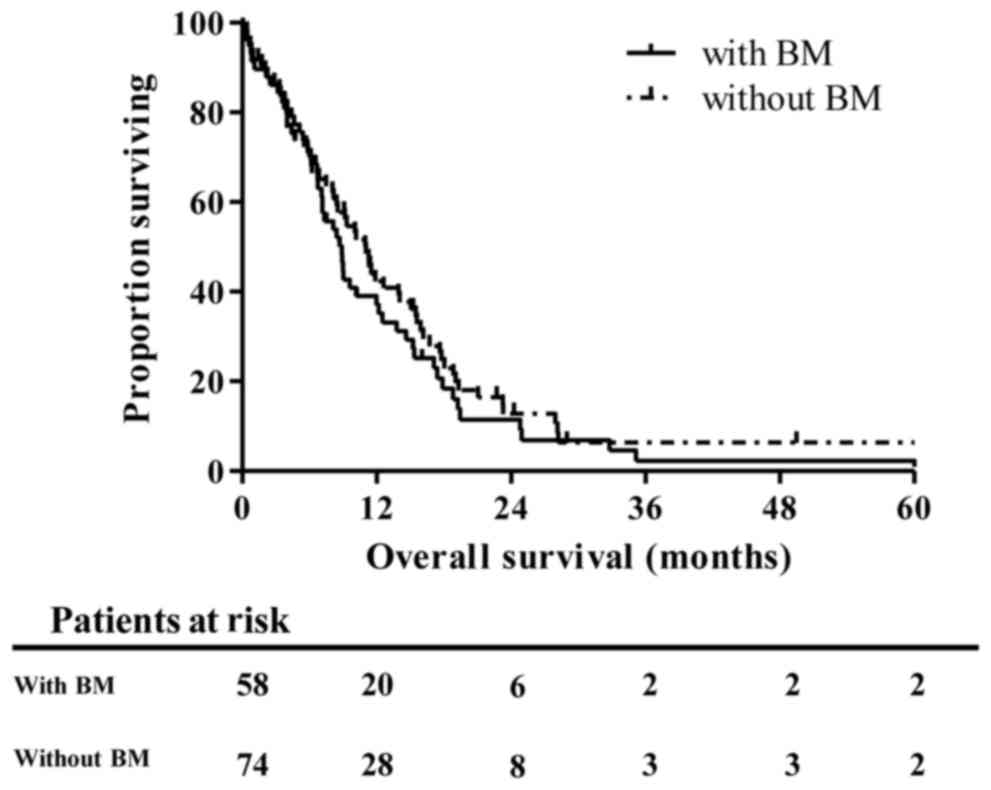
The median OS of 58 patients with BM was 8.87
months, whereas that of 74 ES-SCLC patients without BM was 11.04
months (P=0.496, Fig. 1).
Kaplan-Meir analyses showed that BM is not a significant prognostic
factor in comparison with metastases in other organs. In addition,
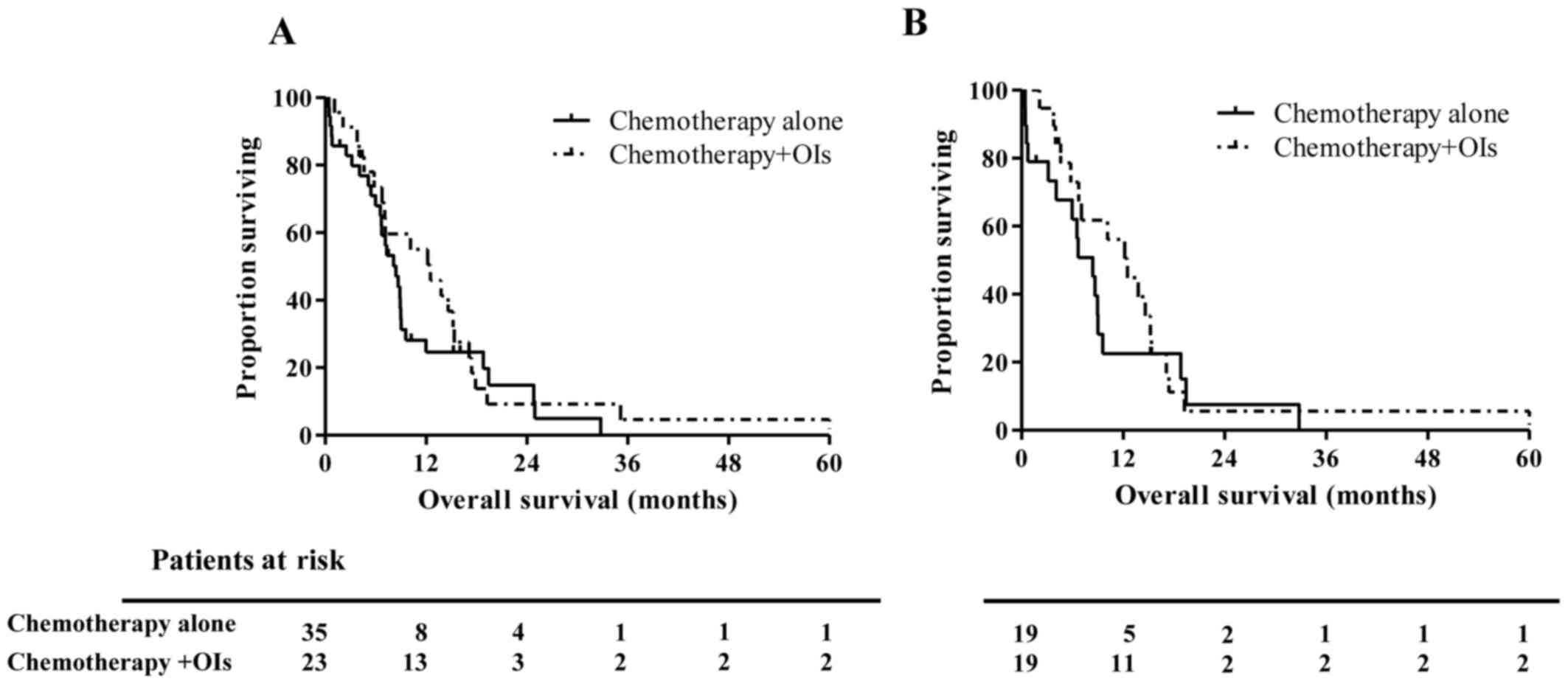
no significant survival differences were identified between
patients with (n=23) and without (n=35) OIs treatments (median OS,
8.41 vs. 12.52 months, respectively; P=0.353; Fig. 2A). However, one-year OS rate in OIs
group were much higher compared to control group (55.1 vs. 24.7%).
These data suggest a tendency for prolonged survival of ES-SCLC
patients treated with OIs, mainly in the early phase within the
observation period of one year. Finally, matched-pair analyses
using propensity scores confirmed the absence of a significant
difference between the groups of the present study (median OS, 8.41
vs. 12.52 months, P=0.409, Fig. 2B).
One-year OS rate in OIs group were also higher compared to control
group after PSM (56.1 vs. 22.6%).
Discussion
BM is a well-known negative prognostic factor in
SCLC and NSCLC patients, and a previous retrospective analysis of
SCLC patients showed significantly shorter OS of patients with BM
than among patients without BM [4.13 vs. 6.17 months, P=0.015
(11)]. In NSCLC patient cohorts,
the incidence of SREs is also a known negative prognostic factor,
with one year survival rates of 5.1 and 12.1% in a retrospective
cohort study of lung cancer patients with and without SREs,
respectively (12). However, this
study showed no significant differences in OS between ES-SCLC
patients with BM and metastasis in the brain, liver, adrenal glands
and pleural cavities. Other studies suggest that liver metastases
are the worst prognostic factor in patients with ES-SCLC (13,14), and
that BM and brain metastases are similarly negative survival
indicators. Specifically, one-year survival of SCLC patients with
liver, brain and BM was 14.5, 25.1 and 23.9%, respectively
(13), warranting consideration of
BM as an important therapeutic target in SCLC patients.
In the present study, OIs tended to prolong the
survival of SCLC patients with BM in the short term, but our data
failed to demonstrate a significant difference between the groups,
likely reflecting insufficient numbers of cases in the OIs group,
as OIs were not generally administered to SCLC patients as they
were to NSCLC patients. In a recent prospective study, BM occurred
in 39.5% of NSCLC patients who were treated with Zol, whereas only
6.7% of ES-SCLC patients developed BM in the same period (10), potentially reflecting the high
chemotherapeutic sensitivity of SCLC. In other studies, overall
response rates to combination therapy with VP-16 or etoposide and
cisplatin (EP) were 86–89% in ES-SCLC patients (15,16).
In the present study, most patients in the OIs group
were treated in response to SREs. Hence, appropriate administration
of OIs before the onset of SREs may decrease the frequency of SREs
and improve OS in SCLC patients with BM. However, future
large-scale prospective studies are required to precisely define
the benefits of OIs in SCLC patients with BM.
Although the incidence of SREs was not decreased by
OIs in the present SCLC patients with BM, likely reflecting
retrospective treatments, new incidences of SREs were observed in
10 of the 23 OIs treated patients, suggesting that OIs prolong
survival via a mechanism that is independent of the suppression of
SREs. In agreement, Zol reportedly suppressed the proliferation of
SCLC cell lines in vitro and in vivo (17,18), and
these antitumor effects of Zol were associated with inhibition of
farnesylation and geranylgeranylation of RAS related proteins, and
the induction of apoptosis (17).
Zol also showed synergistic effects with other anti-cancer agents,
such as cisplatin, etoposide and irinotecan in vitro
(19–21), and a recent preclinical study showed
that Zol promotes the maturation of γδ T cells and contributes to
antitumor immune responses (22).
Thus, Zol may improve the prognoses in SCLC patients via direct
cytotoxic mechanisms or antitumor immunity, in addition to acting
as an inhibitor of SREs.
Denosumab is also expected to have direct antitumor
effects, because Its target RANK/RANKL signalling is known to
activate NF-κB, which has been associated with carcinogenesis,
resistance to chemoradiotherapy and metastasis (8). Specifically, RANKL is expressed on
several tumour types, including lung cancers (23), and therefore, RANK/RANKL signalling
has potential as a therapeutic target. However, RANKL expression
rates have not yet been determined in SCLC, warranting further
studies of direct and indirect antitumor effects of denosumab in
this patient group.
Our analyses were limited to retrospective data from
a single institution with relatively few cases, especially in the
OIs group. In addition, we failed to distinguish between the
effects of Zol and denosumab as independent groups, again
reflecting the small number of cases treated with denosumab and
those cotreated with Zol. Finally, durations of OIs treatments
varied among the present cases, and the start times were not
determined with reference to occurrences of SREs. Hence,
prospective studies are required to confirm the relationships
between preventative effects against SREs and survival.
The present data suggest that OIs prolong the
survival period of ES-SCLC patients with BM in the short term and
warrant larger prospective studies to inform the use of OIs as
preventative treatments for SREs in ES-SCLC patients with BMs.
Acknowledgements
The authors would like to thank Dr Makoto Saito
(Division of Clinical Research Support, Tokyo Metropolitan Cancer
and the Infectious Diseases Center Komagome Hospital, Tokyo,
Japan), for his statistical expertise.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
AM and YO analyzed the data of the SCLC patients
with bone metastasis, and were major contributors in writing this
manuscript. YZ and YH analyzed and interpreted the patient data.
All authors read and approved the final manuscript.
Ethics approval and consent to
participate
All study protocols were approved by the
Institutional Review Committee of Tokyo Metropolitan Cancer and
Infectious diseases Center Komagome Hospital (Tokyo, Japan); the
requirement for written informed consent was waived due to the
retrospective nature of this study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mundy GR: Metastasis to bone: Causes,
consequences and therapeutic opportunities. Nat Rev Cancer.
2:584–593. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
2
|
Coleman RE: Clinical features of
metastatic bone disease and risk of skeletal morbidity. Clin Cancer
Res. 12:6243s–6249s. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Brodowicz T, O'Byrne K and Manegold C:
Bone matters in lung cancer. Ann Oncol. 23:2215–2222. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Roodman GD: Mechanisms of bone metastasis.
N Engl J Med. 350:1655–1664. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Serafini AN: Therapy of metastatic bone
pain. J Nucl Med. 42:895–906. 2001.PubMed/NCBI
|
|
6
|
Rosen LS, Gordon D, Tchekmedyian NS,
Yanagihara R, Hirsh V, Krzakowski M, Pawlicki M, De Souza P, Zheng
M, Urbanowitz G, et al: Long-term efficacy and safety of zoledronic
acid in the treatment of skeletal metastases in patients with
nonsmall cell lung carcinoma and other solid tumors: A randomized,
Phase III, double-blind, placebo-controlled trial. Cancer.
100:2613–2621. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zarogoulidis K, Boutsikou E, Zarogoulidis
P, Eleftheriadou E, Kontakiotis T, Lithoxopoulou H, Tzanakakis G,
Kanakis I and Karamanos NK: The impact of zoledronic acid therapy
in survival of lung cancer patients with bone metastasis. Int J
Cancer. 125:1705–1709. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
De Castro J, García R, Garrido P, Isla D,
Massuti B, Blanca B and Vázquez J: Therapeutic potential of
denosumab in patients with lung cancer: Beyond prevention of
skeletal complications. Clin Lung Cancer. 16:431–446. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Scagliotti GV, Hirsh V, Siena S, Henry DH,
Woll PJ, Manegold C, Solal-Celigny P, Rodriguez G, Krzakowski M,
Mehta ND, et al: Overall survival improvement in patients with lung
cancer and bone metastases treated with denosumab versus zoledronic
acid: Subgroup analysis from a randomized phase 3 study. J Thorac
Oncol. 7:1823–1829. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Katakami N, Kunikane H, Takeda K, Takayama
K, Sawa T, Saito H, Harada M, Yokota S, Ando K, Saito Y, et al:
Prospective study on the incidence of bone metastasis (BM) and
skeletal-related events (SREs) in patients (pts) with stage IIIB
and IV lung cancer-CSP-HOR 13. J Thorac Oncol. 9:231–238. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kang EJ, Lee SY, Kim HJ, Min KH, Hur GY,
Shim JJ, Kang KH, Oh SC, Seo JH, Lee SY and Kim JS: Prognostic
factors and skeletal-related events in patients with small cell
lung cancer with bone metastases at the time of diagnosis.
Oncology. 90:103–111. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cetin K, Christiansen CF, Jacobsen JB,
Nørgaard M and Sørensen HT: Bone metastasis, skeletal-related
events, and mortality in lung cancer patients: A Danish
population-based cohort study. Lung Cancer. 86:247–254. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ren Y, Dai C, Zheng H, Zhou F, She Y,
Jiang G, Fei K, Yang P, Xie D and Chen C: Prognostic effect of
liver metastasis in lung cancer patients with distant metastasis.
Oncotarget. 7:53245–53253. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ogino H, Hanibuchi M, Kakiuchi S, Saijo A,
Tezuka T, Toyoda Y, Tobiume M, Otsuka K, Sakaguchi S, Goto H, et
al: Analysis of the prognostic factors of extensive disease
small-cell lung cancer patients in Tokushima University Hospital. J
Med Invest. 63:286–293. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Goldhirsch A, Joss R, Cavalli F and
Brunner KW: Etoposide as single agent and in combination
chemotherapy of bronchogenic carcinoma. Cancer Treat Rev. 9:85–90.
1982. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Evans WK, Osoba D, Feld R, Shepherd FA,
Bazos MJ and DeBoer G: Etoposide (VP-16) and cisplatin: An
effective treatment for relapse in small-cell lung cancer. J Clin
Oncol. 3:65–71. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Matsumoto S, Kimura S, Segawa H, Kuroda J,
Yuasa T, Sato K, Nogawa M, Tanaka F, Maekawa T and Wada H: Efficacy
of the third-generation bisphosphonate, zoledronic acid alone and
combined with anti-cancer agents against small cell lung cancer
cell lines. Lung Cancer. 47:31–39. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kenessey I, Kói K, Horváth O, Cserepes M,
Molnár D, Izsák V, Dobos J, Hegedűs B, Tóvári J and Tímár J:
KRAS-mutation status dependent effect of zoledronic acid in human
non-small cell cancer preclinical models. Oncotarget.
7:79503–79514. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Neville-Webbe HL, Evans CA, Coleman RE and
Holen I: Mechanisms of the synergistic interaction between the
bisphosphonate zoledronic acid and the chemotherapy agent
paclitaxel in breast cancer cells in vitro. Tumour Biol. 27:92–103.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ozturk OH, Bozcuk H, Burgucu D, Ekinci D,
Ozdogan M, Akca S and Yildiz M: Cisplatin cytotoxicity is enhanced
with zoledronic acid in A549 lung cancer cell line: Preliminary
results of an in vitro study. Cell Biol Int. 31:1069–1071. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Budman DR and Calabro A: Zoledronic acid
(Zometa) enhances the cytotoxic effect of gemcitabine and
fluvastatin: In vitro isobologram studies with conventional and
nonconventional cytotoxic agents. Oncology. 70:147–153. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Fournier PG, Chirgwin JM and Guise TA: New
insights into the role of T cells in the vicious cycle of bone
metastases. Curr Opin Rheumatol. 18:396–404. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Peng X, Guo W, Ren T, Lou Z, Lu X, Zhang
S, Lu Q and Sun Y: Differential expression of the RANKL/RANK/OPG
system is associated with bone metastasis in human non-small cell
lung cancer. PLoS One. 8:e583612013. View Article : Google Scholar : PubMed/NCBI
|