Introduction
Lung cancer is the most common cause of
cancer-related mortality worldwide. It was estimated that, in 2016,
there were 158,080 deaths from lung cancer in the United States
(1). In the latest statistical
analysis, it is predicted that in 2018 the number of deaths may
reach ~154,050 and the number of new cases 234,030, and the
mortality from lung cancer is expected to be higher compared with
that from other cancers combined (2). Small-cell lung cancer (SCLC) accounts
for ~13–15% of all lung cancer cases (3) and is strongly associated with tobacco
smoking. SCLC is very chemoradiosensitive, but patients often
present with symptoms of metastatic disease at the time of SCLC
diagnosis, and the prognosis remains poor. Unfortunately, in
advanced-stage SCLC, the median survival with the currently
available standard treatments is only 9–10 months from the time of
diagnosis.
The treatment of SCLC mainly consists of
chemotherapy, with a combination of platinum and etoposide or
irinotecan. The use of prophylactic cranial irradiation (PCI) and
sequential thoracic irradiation has been reported to improve
survival in selected patients with extensive SCLC (4,5).
Unfortunately, almost all patients relapse with
chemoresistant disease (6) and there
has been almost no improvement in 1-year SCLC mortality rate over
10 years (7).
Case report
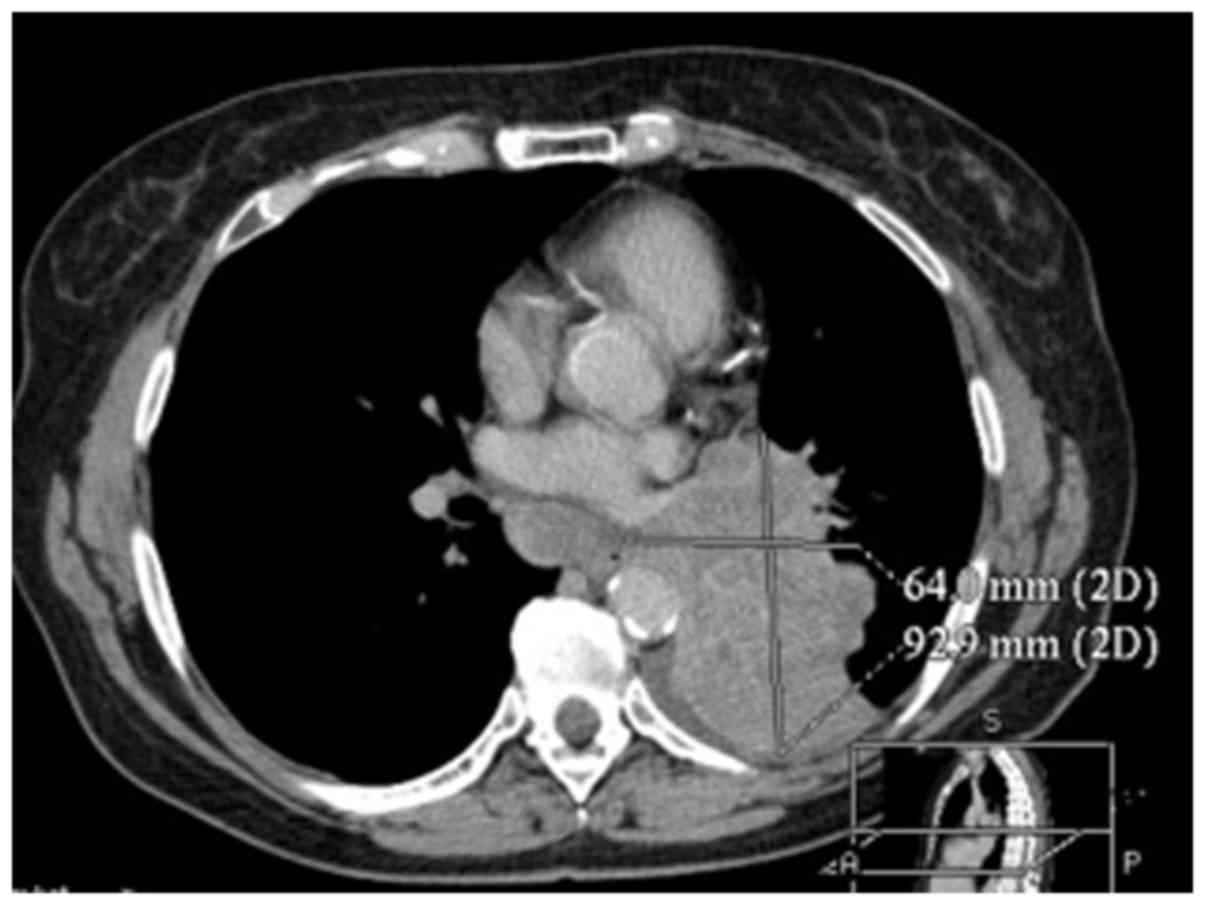
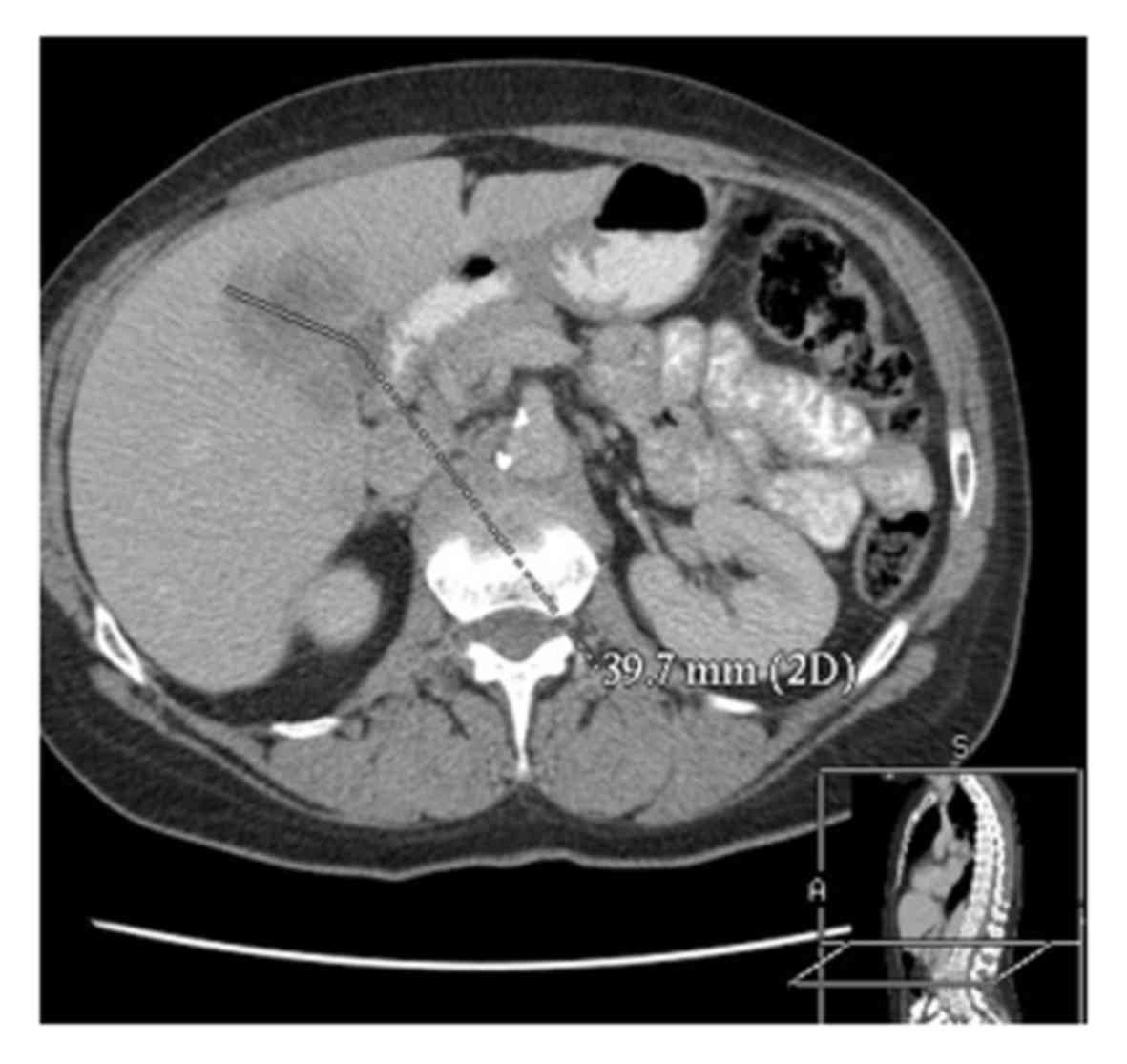
In February 2011, a 62-year-old woman was diagnosed
with SCLC (Figs. 1 and 2). The patient was a retired teacher and a
smoker (20 cigarettes/day for 45 years).A chest X-ray followed by
computed tomography were performed to explain the cause of a
persistent cough following a respiratory infection~1 month earlier.
The diagnosis of SCLC was based on microscopic examination of the
material obtained during bronchoscopy. The patient's overall health
was good, but she reported previously taking metformin due to
impaired fasting glucose and atorvastatin due to
hypercholesterolemia. At 5 weeks after the initial diagnosis,
chemotherapy with platinum (49.69 mg/day for 3 days) and etoposide
(165.62 mg/day for 3 days) was administered. The patient received 6
cycles of this treatment, but the intervals between cycles had to
be prolonged due to leukopenia (WBC <2,500/µl). Cancer remission
was achieved after 6 cycles of standard therapy. After the 4th
cycle, PCI (2.5 Gy/g; 10 cycles) was performed. In addition,
long-term enoxaparin (40 mg/day) therapy lasting 2 years was
prescribed.
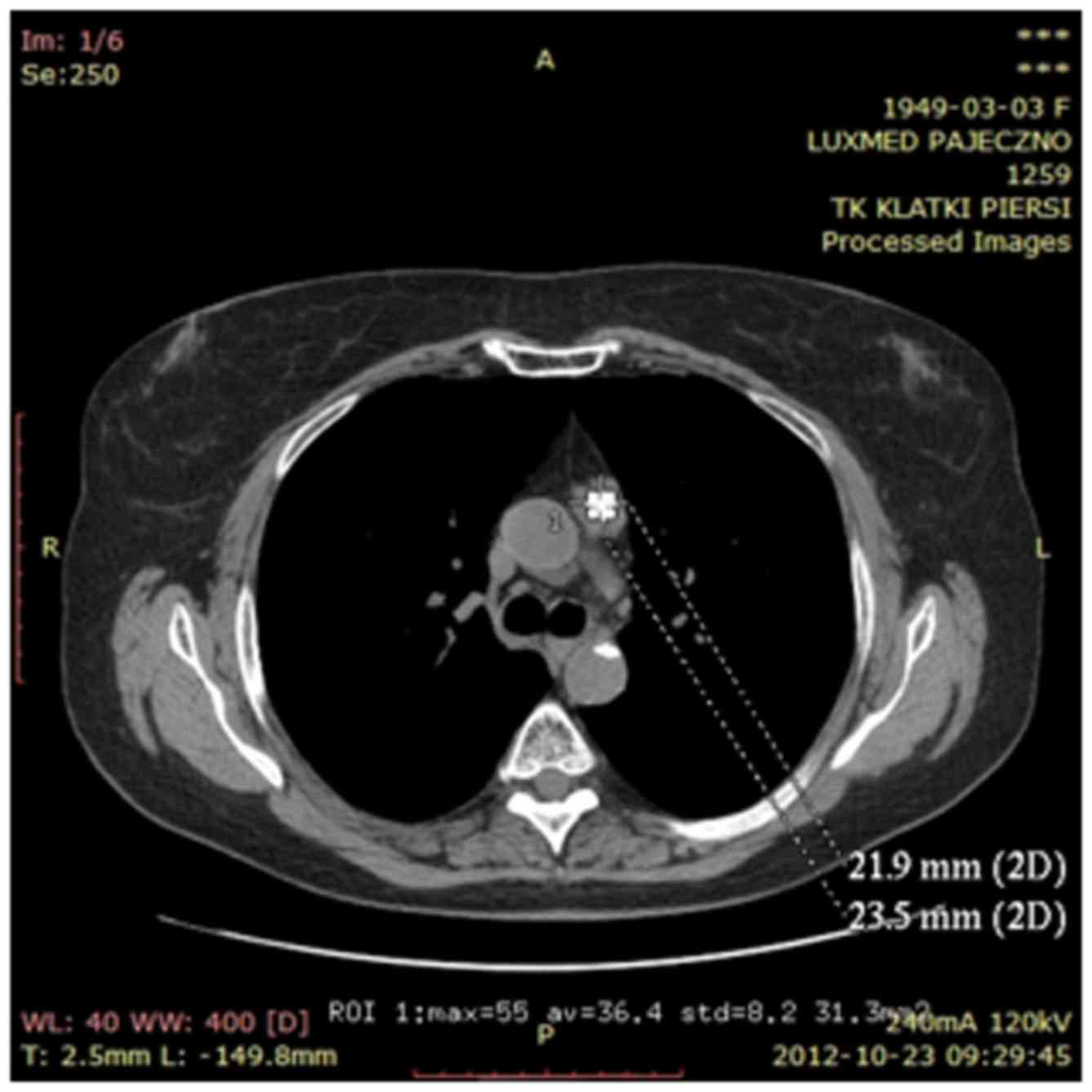
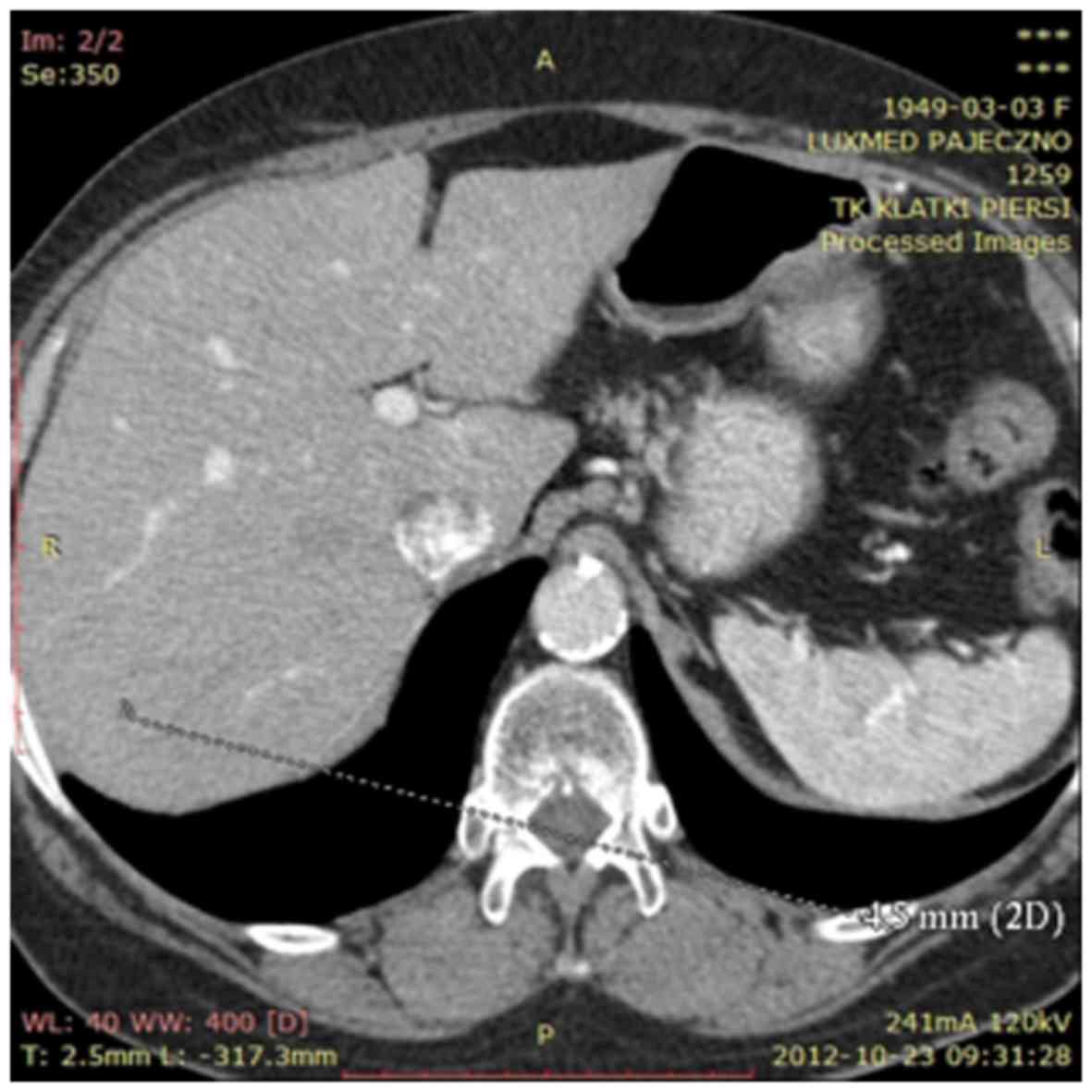
In April 2012, a computed tomography-positron
emission tomography scan was performed in order to exclude
neoplastic changes in the lymphnodes and metastatic disease. Gamma
Knife was then used to treat mediastinal lymphnodes suspected for
neoplastic infiltration. Oncological treatment was completed in May
2012 (Figs. 3 and 4). The patient was advised to visit the
oncological centre in case of tumour progression detected on annual
follow-up examinations.
Simultaneously, an off-label therapy was
administered. The individualized scheme included curcumin,
parthenolide, betuline, sulforaphane, withanolides, lactoferrin,
pomegranate fruit extract, flaxseed orally and dioscorea in
inhalational form.
The treatment strategy was based on changing the
agents every 5 days in order to avoid developing resistance to
treatment. Compounds extracted from medicinal plants usually have
low bioavailability; therefore, the pivotal role of appropriately
higher doses of certain agents should be emphasised. In the
majority of cases, double dosages were used, rather than what was
recommended by the manufacturer. However, metformin, atorvastatin
and enoxaparin were administered at doses of 850, 10 and 40 mg/day,
respectively. The patient has been continuously taking curcumin
(1,330 mg/day), betuline (10 ml 2% extract/day), withanolides
(1,100 mg/day), parthenolide (0.624 mg/day), lactoferrin (200
mg/day), sulforaphane (100 mg/day) and pomegranate fruit extract
(2,200 mg/day) to this day. Some of the active substances are
administered on a daily basis (curcumin, sulforaphane, atorvastatin
and metformin), whereas the others are changed every 5 days. All
agents mentioned above were well-tolerated. Follow-up chest X-ray
and abdominal ultrasound are performed annually and have not shown
any progression or metastasis of the lung cancer. The results of
the annual laboratory blood tests are also normal.
The patient is a member of the author's family and
remains under his medical care. She remains alive and in good
condition. The last examination took place in September 2018.
Discussion
The medications previously used by the patient due
to comorbidities (metformin and atorvastatin) were continued during
chemo- and radiotherapy. Atorvastatin may overcome the resistance
to carboplatin in patients with lung cancer and, when used together
with carboplatin, it inhibits the growth of lung cancer more
effectively compared with either of these agents used alone
(8). In addition, it has been
previously reported that patients using rosuvastatin, simvastatin,
atorvastatin and pravastatin had a significantly decreased lung
cancer risk, depending on statin doses (9). The beneficial role of metformin was
observed by Chuang et al in patients with diabetes mellitus
who had inoperable lung cancer. This patient group exhibited a
significantly longer overall survival while using metformin
(10). A number of previous studies
indicated the anticancer activity of metformin, including cell
cycle arrest, apoptosis of malignant cells and tumour growth
suppression (11). In patients
treated with cisplatin-based chemotherapy, an increased risk of
arterial and venous thromboembolic events was confirmed (12). For example, in Asian patients with
SCLC, the annual cumulative incidence of thromboembolic events is
~10% (13). Using primary
thromboprophylaxis with low-molecular-weight heparin can
significantly lower the risk of thromboembolic events in patients
treated with chemotherapy (14).
Enoxaparin may have a beneficial impact on overall survival in
patients treated for lung cancer (15); however, in patients with SCLC,
enoxaparin in supraprophylactic doses (1 mg/kg) increased the
incidence of haemorrhagic events and had no beneficial effect on
progression-free or overall survival (16).
Naturally occurring substances have known anticancer
properties. Curcumin has been reported to regulate oncogenes (p53,
egr-1, c-myc and Bcl-xL), transcription factors (NF-κB, STAT-3 and
AP-1),protein kinases (MAPK)and enzymes (cyclooxygenase and
lipoxygenase). The beneficial effects of curcumin have been
observed in terms of sensitization to chemo- and radiotherapy,
reduction of tumour invasion and metastasis (17).
Therefore, curcumin may be a potential candidate for
augmenting response to adjunctive chemotherapies in lung cancer
(17). However, due to its poor oral
bioavailability and instability, new technologies are needed to
achieve proper tissue concentration of this agent. For example, the
level of serum curcumin following oral administration may be
increased if combined with black pepper (18). Betulin [lup-20(29)-ene-3β, 28-diol]is
a naturally occurring triterpene that has anticancer properties.
Pentacyclic triterpene lupeol has also been reported to have
anti-lung cancer activity. Both have a multifactorial mechanism of
action in cancer tissues, including downregulation of isoenzyme
cyclooxygenase 2 (COX-2), inhibition of malignant cell
proliferation and inhibition of cell cycle (19,20), as
well as induction of apoptosis, which is similar to cisplatin
activity (21). Dioscorea japonica
extract has been shown to suppress the expression of COX-2 and
microsomal prostaglandin E synthase, which results in
anti-inflammatory and anticancer activity (22). Suppression of COX-2 and reduction of
prostaglandin E2 (PGE2) production are similar to the effects of
sulforaphane. Sulforaphane inhibits the synthesis of PGE2 (23) and it has been reported that hypoxia
in cancer tissues is related to increased production of PGE2, which
is associated with cancer progression. Oral talactoferrin has been
proven to be useful and was well-tolerated in patients with stage
IIIB-IV non-small-cell lung cancer (NSCLC) in whom previous
chemotherapies had failed (24).
Withaferin A is a bioactive lactone, isolated from Withania
somnifera. It has been shown that Withaferin A possesses
anti-oxidative, anti-inflammatory, anti-proliferative and
apoptosis-inducing properties (25).
The combination of paclitaxel with Withaferin A effectively treated
lung cancer in mice (26);
additionally, it was demonstrated that Withaferin A induced
inhibition of cancer growth and oxidative damage to NSCLC cells
(27,28). Pomegranate fruit extract
significantly inhibits the growth and progression of lung cancer in
mice (29) due to the induction of
apoptosis and modulation of cell signalling pathways. Moreover, the
ingredients of pomegranates exert anti-inflammatory effects and
inhibit angiogenic factors (30).
Parthenolide, which is derived from the plant feverfew, induces
apoptosis of NSCLC cells and selectively kills cancer stem cells
(31). Flaxseed possesses
antioxidant and hepatoprotective properties; in addition, in
postmenopausal women, lignans from flaxseed may act as weak
oestrogens. Its anti-inflammatory activity and influence on PGE2,
leukotriene B4, TNF-α, interleukin and cytokines was confirmed
(32). Furthermore, flaxseed may
decrease the adverse effects of radiation in cancer patients
(33).
The use of additional treatment in the form of
medicinal substances with potential antitumor properties, provided
that there are no side effects and no drug interactions, may be
helpful in the treatment of certain types of cancer. Therefore, the
long-term and alternate use of certain herbal and medicinal active
substances may reduce the risk of recurrence or progression of
certain types of cancer.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Ethics approval and consent to
participate
Not applicable.
Authors' contributions
PK prepared and approved the final manuscript.
Patient consent for publication
The patient provided written informed consent
regarding the publication of the case details and associated
images.
Competing interests
The author declares that he has no competing
interests.
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2016. CA Cancer J Clin. 66:7–30. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2018. CA Cancer J Clin. 68:7–30. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Siegel RL, Miller KD and Jemal A: Cancer
Statistics, 2017. CA Cancer J Clin. 67:7–30. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Demedts IK, Vermaelen KY and van Meerbeeck
JP: Treatment of extensive-stage small cell lung carcinoma: Current
status and future prospects. Eur Respir J. 35:202–215. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kalemkerian GP: Small Cell Lung Cancer.
Semin Respir Crit Care Med. 37:783–796. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kalemkerian GP and Schneider BJ: Advances
in small cell lung cancer. Hematol Oncol Clin North Am. 31:143–156.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dayen C, Debieuvre D, Molinier O, Raffy O,
Paganin F, Virally J, Larive S, Desurmont-Salasc B, Perrichon M,
Martin F, et al: New insights into stage and prognosis in small
cell lung cancer: An analysis of 968 cases. J Thorac Dis.
9:5101–5111. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chen J, Lan T, Hou J, Zhang J, An Y, Tie
L, Pan Y, Liu J and Li X: Atorvastatin sensitizes human non-small
cell lung carcinomas to carboplatin via suppression of AKT
activation and upregulation of TIMP-1. Int J Biochem Cell Biol.
44:759–769. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Liu JC, Yang TY, Hsu YP, Hao WR, Kao PF,
Sung LC, Chen CC and Wu SY: Statins dose-dependently exert a
chemopreventive effect against lung cancer in COPD patients: A
population-based cohort study. Oncotarget. 7:59618–59629.
2016.PubMed/NCBI
|
|
10
|
Chuang MC, Yang YH, Tsai YH, Hsieh MJ, Lin
YC, Lin CK, Chen PC and Yang TM: Survival benefit associated with
metformin use in inoperable non-small cell lung cancer patients
with diabetes: A population-based retrospective cohort study. PLoS
One. 13:e01911292018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gupta G, de Jesus Andreoli Pinto T,
Chellappan DK, Mishra A, Malipeddi H and Dua K: A clinical update
on metformin and lung cancer in diabetic patients. Panminerva Med.
60:70–75, Epub ahead of print. 2018.PubMed/NCBI
|
|
12
|
Lee YG, Lee E, Kim I, Lee KW, Kim TM, Lee
SH, Kim DW and Heo DS: Cisplatin-based chemotherapy is a strong
risk factor for thromboembolic events in small-cell lung cancer.
Cancer Res Treat. 47:670–675. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Seng S, Liu Z, Chiu SK, Proverbs-Singh T,
Sonpavde G, Choueiri TK, Tsao CK, Yu M, Hahn NM, Oh WK, et al: Risk
of venous thromboembolism in patients with cancer treated with
Cisplatin: A systematic review and meta-analysis. J Clin Oncol.
30:4416–4426. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Di Nisio M, Porreca E, Candeloro M, De
Tursi M, Russi I and Rutjes AW: Primary prophylaxis for venous
thromboembolism in ambulatory cancer patients receiving
chemotherapy. Cochrane Database Syst Rev.
12:CD0085002016.PubMed/NCBI
|
|
15
|
Liu ZL, Wang Q, Wang M, Wang B and Huang
LN: Low molecular weight heparin in treating patients with lung
cancer received chemotherapy: A meta-analysis. J Cancer Res Ther.
14:S437–S443. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ek L, Gezelius E, Bergman B, Bendahl PO,
Anderson H, Sundberg J, Wallberg M, Falkmer U, Verma S and Belting
M; Swedish Lung Cancer Study Group (SLUSG), . Randomized phase III
trial of low-molecular-weight heparin enoxaparin in addition to
standard treatment in small-cell lung cancer: The RASTEN trial. Ann
Oncol. 29:398–404. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Mehta HJ, Patel V and Sadikot RT: Curcumin
and lung cancer-a review. Target Oncol. 9:295–310. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Mahran RI, Hagras MM, Sun D and Brenner
DE: Bringing curcumin to the clinic in cancer prevention: A review
of strategies to enhance bioavailability and efficacy. AAPS J.
19:54–81. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Milhoub M, Pichette A, Sylla B, Gauthier C
and Legault J: Bidesmosidic betulin saponin bearing
L-rhamnopyranoside moieties induces apoptosis and inhibition of
lung cancer cells growth in vitro and in vivo. PLoS One. 13(3):
e01933862018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Cháirez-Ramírez MH, Moreno-Jiménez MR,
González-Laredo RF, Gallegos-Infante JA and Rocha-Guzmán NE:
Lupane-type triterpenes and their anti-cancer activities against
most common malignant tumors: A review. EXCLI J. 15:758–771.
2016.PubMed/NCBI
|
|
21
|
Pyo JS, Roh SH, Kim DK, Lee JG, Lee YY,
Hong SS, Kwon SW and Park JH: Anti-cancer effect of Betulin on a
human lung cancer cell line: A pharmacoproteomic approach using 2 D
SDS PAGE coupled with nano-HPLC tandem Mass Spectrometry. Planta
Med. 75:127–131. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Suzuki-Yamamoto T, Tanaka S, Tsukayama I,
Takafuji M, Hanada T, Arakawa T, Kawakami Y, Kimoto M and Takahashi
Y: Dioscorea japonica extract down-regulates prostaglandin E2
synthetic pathway and induces apoptosis in lung cancer cells. J
Clin Biochem Nutr. 55:162–167. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zhou J, Joplin DG, Cross JV and Templeton
DJ: Sulforaphane inhibits prostaglandin E2 synthesis by suppressing
microsomal prostaglandin E synthase 1. PLoS One. 7:e497442012.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Parikh PM, Vaid A, Advani SH, Digumarti R,
Madhavan J, Nag S, Bapna A, Sekhon JS, Patil S, Ismail PM, et al:
Randomized, double-blind, placebo-controlled phase II study of
single-agent oral talactoferrin in patients with locally advanced
or metastatic non-small-cell lung cancer that progressed after
chemotherapy. J Clin Oncol. 29:4129–4136. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lee IC and Choi BY: Withaferin-A-a natural
anticancer agent with pleitropic mechanisms of action. Int J Mol
Sci. 17:2902016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Senthilnathan P, Padmavathi R, Magesh V
and Sakthisekaran D: Chemotherapeutic efficacy of paclitaxel in
combination with Withania somnifera on benzo(a)pyrene-induced
experimental lung cancer. Cancer Sci. 97:658–664. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Choudhary MI, Hussain S, Yousuf S, Dar A,
Mudassar and Atta-ur-Rahman: Chlorinated and diepoxy withanolides
from Withania somnifera and their cytotoxic effects against human
lung cancer cell line. Phytochemistry. 71:2205–2209. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Liu X, Chen L, Liang T, Tian XD, Liu Y and
Zhang T: Withaferin A induces mitochondrial-dependent apoptosis in
non-small cell lung cancer cells via generation of reactive oxygen
species. J BUON. 22:244–250. 2017.PubMed/NCBI
|
|
29
|
Khan N, Afaq F, Kweon MH, Kim K and
Mukhtar H: Oral consumption of pomegranate fruit extract inhibits
growth and progression of primary lung tumors in mice. Cancer Res.
67:3475–3482. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Rahmani AH, Alsahli MA and Almatroodi SA:
Potential antitumor effects of pomegranates and its ingredients.
Pharmacogn Rev. 11:136–140. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Zhao X, Liu X and Su L: Parthenolide
induces apoptosis via TNFRSF10B and PMAIP1 pathways in human lung
cancer cells. J Exp Clin Cancer Res. 33:32014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kajla P, Sharma A and Sood DR: Flaxseed-a
potential functional food source. J Food Sci Technol. 52:1857–1871.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Pietrofesa R, Turowski J, Tyagi S, Dukes
F, Arguiri E, Busch TM, Gallagher-Colombo SM, Solomides CC, Cengel
KA and Christofidou-Solomidou M: Radiation mitigating properties of
the lignan component in flaxseed. BMC Cancer. 13:1792013.
View Article : Google Scholar : PubMed/NCBI
|