Introduction
Primary adenocarcinoma of the rectovaginal septum
(PARS) is a rare neoplasm that arises predominantly from
endometriosis (1,2), and PARS without associated
endometriosis is even rarer. To the best of our knowledge, there
are only six previous cases of PARS without associated
endometriosis described in the literature (3–8). The
present report represents a case of laparoscopic posterior pelvic
exenteration (PPE) for PARS without associated endometriosis, which
may have arisen from metaplasia of the embryological Müllerian-duct
remnants.
Case report
A 49-year-old woman (gravida 3 and para 2) was
admitted to Hakodate Central General Hospital in August 2015 for
rectal bleeding. Her anamnesis and family history were uneventful.
Her menstrual cycle was regular with no clinical symptom of
dysmenorrhea. A colonoscopy was performed, and a tumor was found to
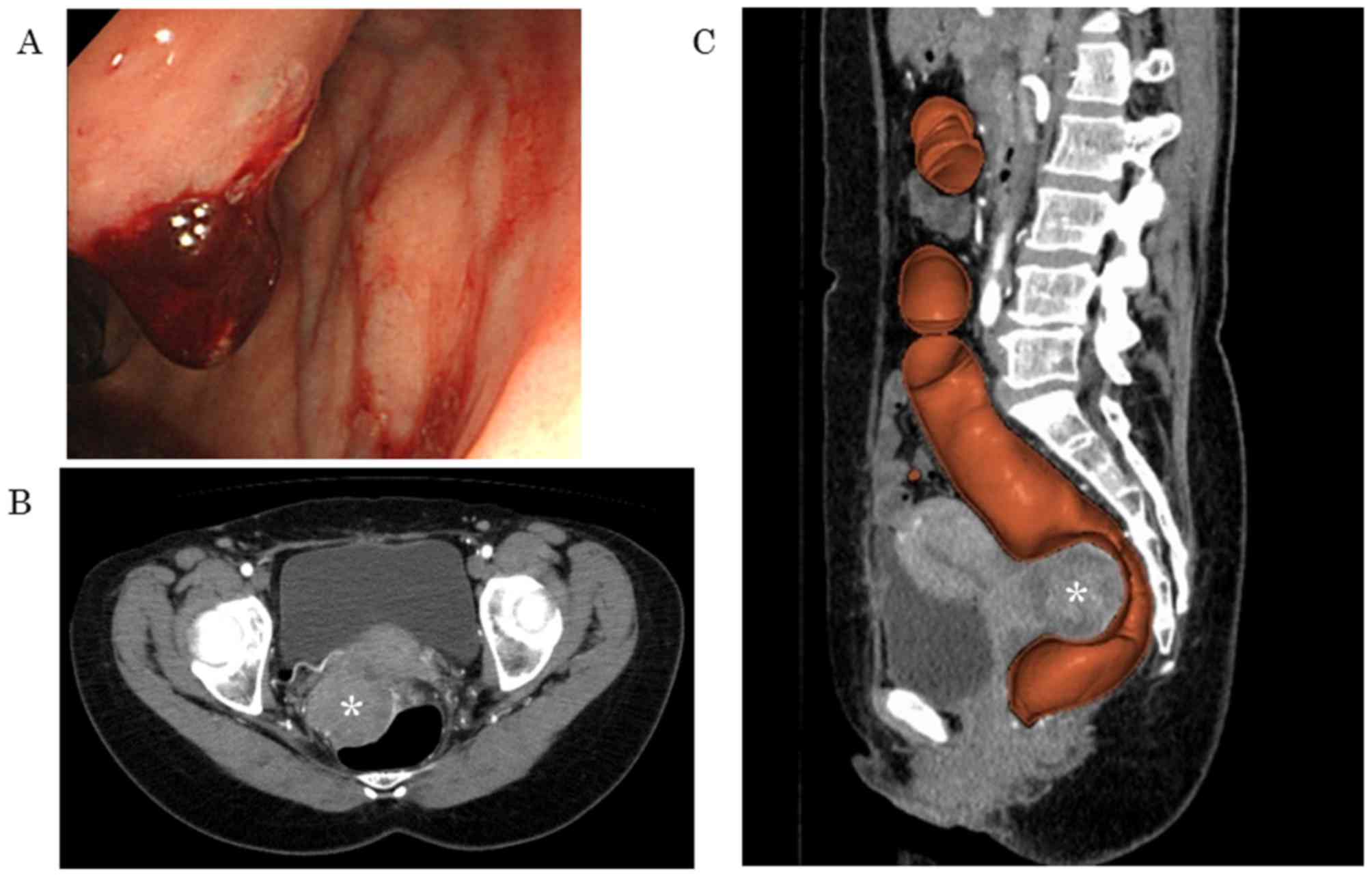
infiltrate the lower rectal mucosa compressing the rectum (Fig. 1A). Computed tomography (CT) and CT
colonoscopy revealed a solid tumor measuring 7 cm in diameter in
the rectovaginal septum, presenting with invasion to the posterior
aspect of the uterine cervix and the anterior rectal wall (Fig. 1B and C). No distant metastasis or
lymph node swelling were present. Rectal and vaginal examination
revealed a bulging tumor in the rectovaginal space. Laboratory data
revealed a high serum level of cancer antigen (CA)125 at 311.5
U/ml. No other abnormal findings were found in the full blood count
or biochemistry. Cervical and endometrial cytology were both
negative.
Laparoscopic surgery was performed. The findings of
surgery revealed peritoneal invasion of the retroperitoneal tumor
on the left side of the Douglas cavum, although no other
disseminated lesions were found. The bilateral adnexa were not
enlarged, and there were no signs of endometriosis anywhere in the
abdominal cavity. Additionally, no ascites was observed. Total
hysterectomy, bilateral salpingo-oophorectomy, rectosigmoidectomy,
peritoneal resection and pelvic lymph node biopsy were performed
laparoscopically. Subsequently, transvaginal total vaginectomy and
rectosigmoid anastomosis were performed. The rectovaginal tumor was
completely excised with the uterus, bilateral adnexa and rectum via
en bloc resection. There were no intra- or post-operative
complications, and the patient was discharged from the hospital 10
days following surgery. The histopathological diagnosis was of
poorly differentiated adenocarcinoma arising from the rectovaginal
septum of unknown origin, described further below. The patient was
treated with combined carboplatin-paclitaxel-bevacizumab (CP + Bev)
therapy for six cycles according to the treatment protocol for
ovarian cancer (9). The patient
continued to receive Bev monotherapy therapy for three cycles
following the final course of CP + Bev therapy, however, multiple
liver and lung metastases were confirmed. Although the patient had
been treated with Bev therapy, pegylated liposomal doxorubicin +
Bev (PLD + Bev) therapy was initiated according to the AURELIA
platinum-resistant recurrent ovarian cancer trial (10). However, chemotherapy did not show
therapeutic efficacy against the metastatic lesions, resulting in
further progression of multiple liver and lung metastases. The
patient had no recurrence within the pelvis, but succumbed to
mortality 14 months following initial treatment due to multiple
organ failure caused by these metastases.
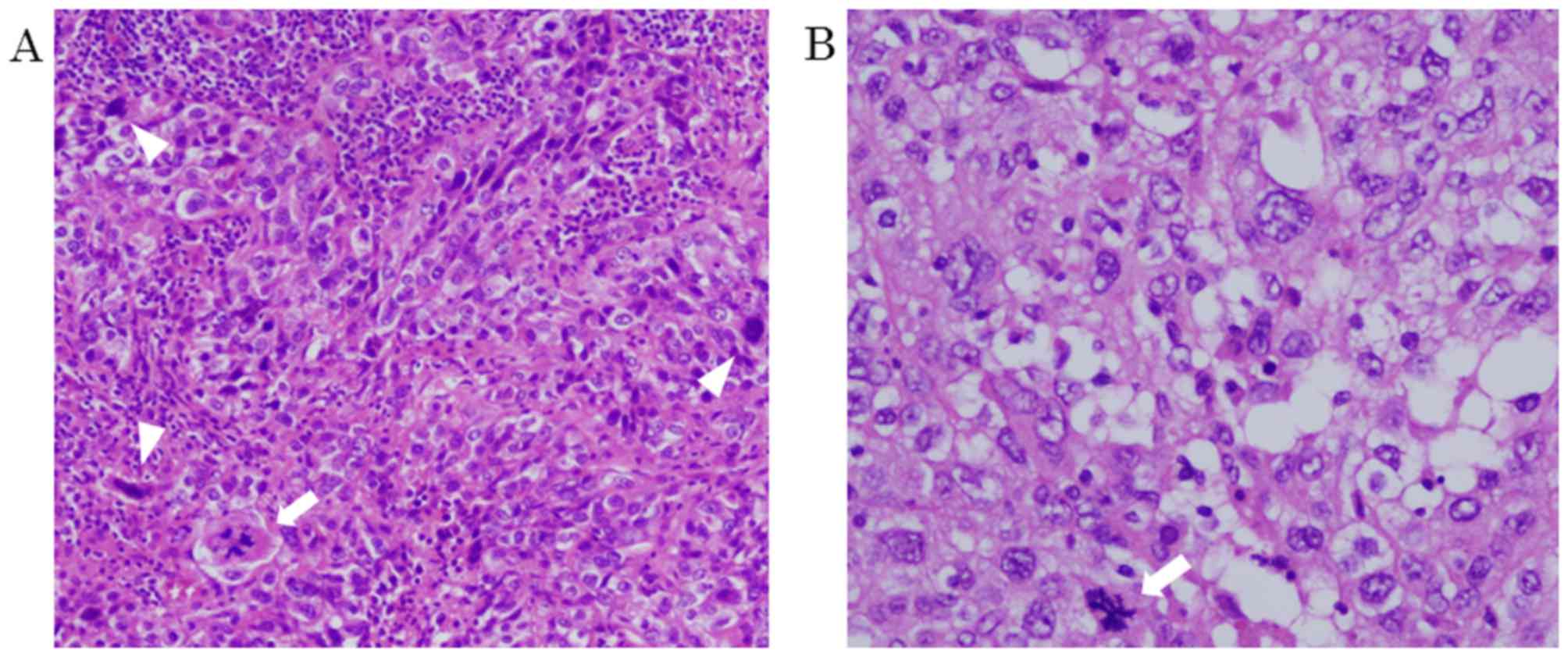
Histopathological findings. On microscopic
examination, the neoplasm was characterized by moderate to severe
cytological atypia, with bizarre multinucleated cells. Abnormal
mitoses were also observed, and the mitotic figure level was up to
14/10 HPF. The histopathological diagnosis was poorly
differentiated adenocarcinoma (Fig. 2A
and B). No endometriotic lesion was confirmed in the primary
tumor or the other removed tissues. No neoplastic lesions were
observed in the bilateral adnexa or lymph nodes. All the margins of
the resected tissues were cancer negative and, histopathologically,
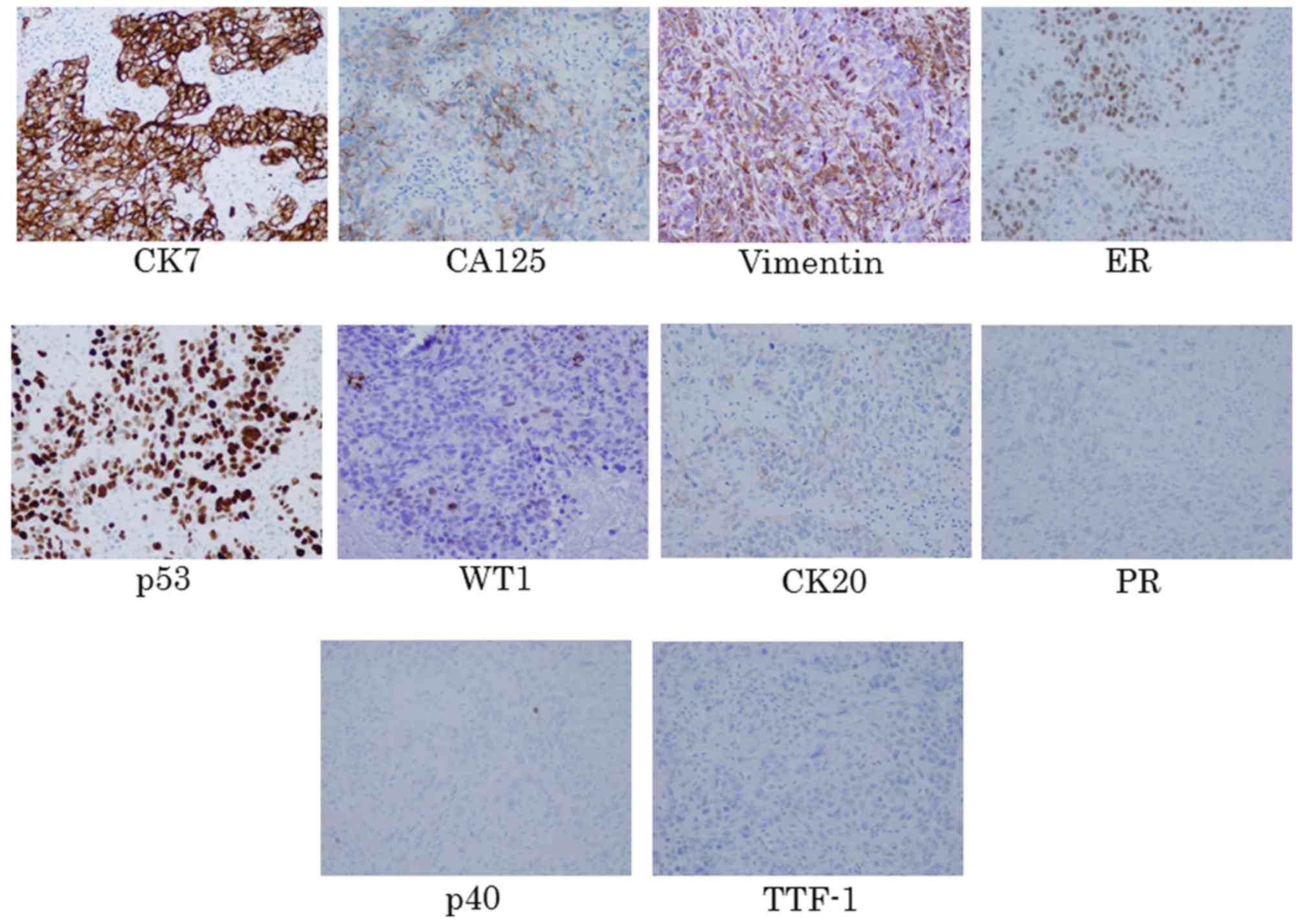
R0 resection had been achieved. The results of the
immunohistochemistry showed positive staining for cytokeratin
(CK)7, CA125, vimentin, estrogen receptor (ER) and p53; partial
positive staining for Wilm's tumor (WT)-1; and negative staining
for CK20, progesterone receptor (PR), p40, and thyroid
transcription factor (TTF)-1 (Fig.
3). From these findings and considering the location of the
tumor, the histopathological diagnosis was poorly differentiated
adenocarcinoma arising from the rectovaginal septum of unknown
origin.
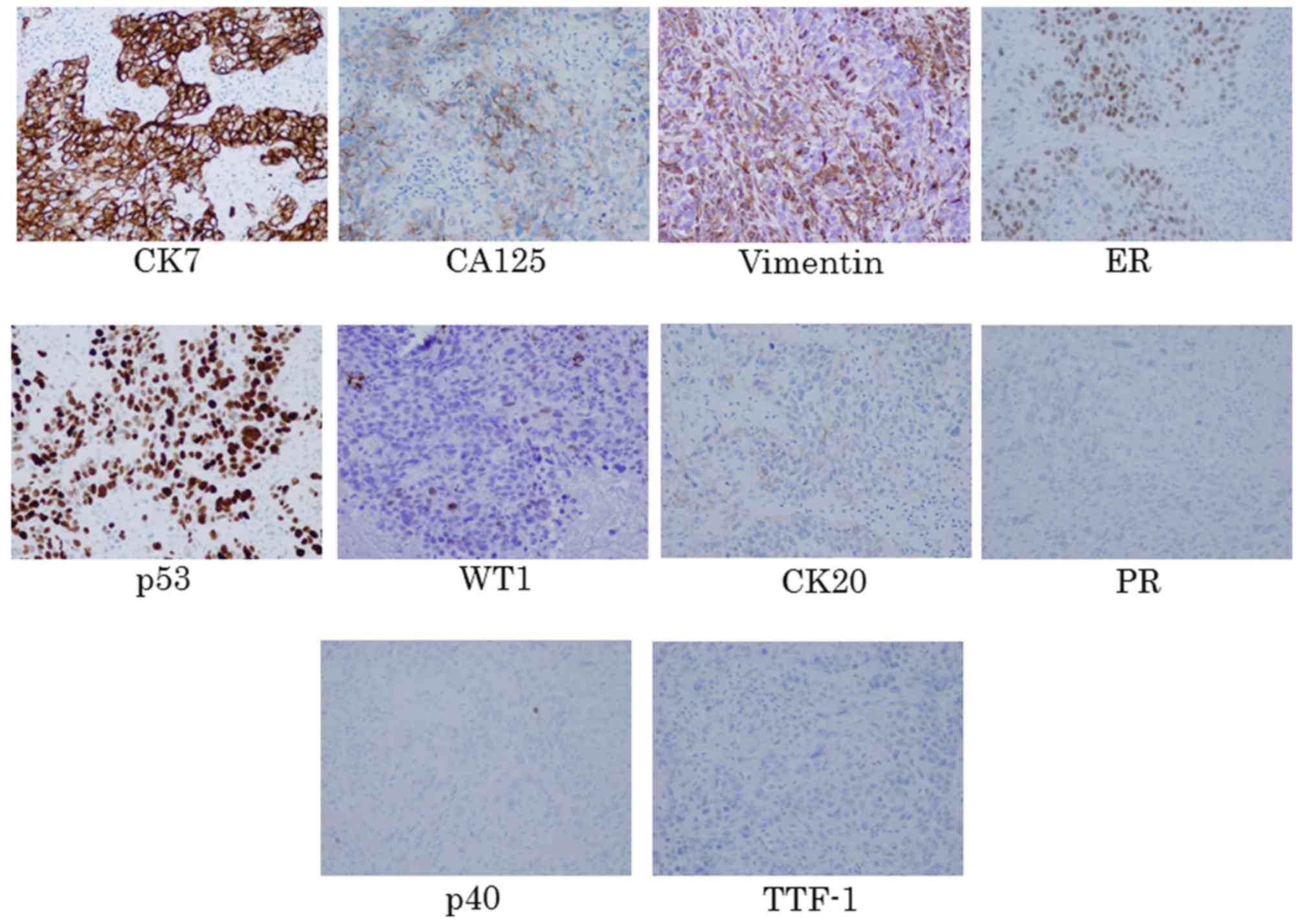 | Figure 3.Immunohistochemistry.
Immunohistochemical staining of the excised tumor revealed positive
staining for CK7, CA125, vimentin, ER and p53; partially positive
staining for WT-1; and negative staining for CK20, PR, p40, and
TTF-1 (magnification, ×40). CK, cytokeratin; CA, cancer antigen;
ER, estrogen receptor; WT, Wilm's tumor; PR, progesterone receptor;
TTF, thyroid transcription factor. |
Discussion
Tumors arising from the rectovaginal septum can be
benign or malignant lesions that have developed in the connective
tissue. For example, benign lesions include neurilemmoma (11) or endometriosis (12), whereas malignant lesions include
leiomyosarcoma (13), extra-osseous
Ewing's sarcoma (14) and
extragastrointestinal stromal tumor (15). PARS is a rare malignant tumor that
arises from the rectovaginal septum, the majority of cases of which
have been reported to occur from endometriosis (1,2). To the
best of our knowledge, only six cases of PARS without associated
endometriosis have been reported in the literature (3–8).
Therefore, the case described here is considered to be the seventh
reported case of PARS without associated endometriosis, and the
first reported case in which the tumor was completely removed by
total laparoscopic PPE.
The clinical symptoms of PARS without associated
endometriosis include lower abdominal pain, dyspareunia, vaginal
discharge, vaginal or rectal bleeding and acute urinary retention
(3–5). Due to their location, the tumors remain
latent until these clinical symptoms appear. As a result, the
diagnosis of this neoplasm tends to be delayed, and the size of the
tumor enlarges when the diagnosis has been made. This delay in
diagnosis has previously been indicated (4). According to the literature, the average
size of the reported tumor was 6.1 cm (3.7–9 cm), and the tumor
size was 7 cm in the present case.
In terms of the histopathological diagnosis of PARS
without associated endometriosis, it may be difficult to
differentiate this neoplasm from carcinomas arising from adjacent
pelvic organs and metastasis from other primary carcinomas. In this
respect, the analysis of CK7, CK20, vimentin and CA125 are pivotal
for distinguishing this neoplasm from carcinomas that develop from
adjacent organs, including rectal carcinoma, cervical carcinoma and
vaginal squamous cell carcinoma. In particular, CK7 and CK20 are
useful for differentiating between this neoplasm and primary rectal
carcinomas. As in the present case, this neoplasm frequently
exhibits positive staining for CK7 (5,7). By
contrast, the majority of cases of rectal carcinoma exhibit
negative staining for CK7 and positive staining for CK20 (16,17).
The etiology of PARS without associated
endometriosis remains to be fully elucidated. Berger et al
(4) reported four possible
hypotheses to explain the etiology of this neoplasm: i)
Endometriosis disappears after the menopause; ii) a tumor that
arose from the malignant transformation of deep endometriosis
present in the rectovaginal septum expands to destroy the adjacent
endometriotic lesion; iii) the tumor may have arisen from adjacent
organs, including rectal carcinoma, cervical and vaginal squamous
cell carcinoma; and iv) the tumor may have arisen directly from
metaplasia of embryological Müllerian-duct remnants (18). However, considering the patient's
age, regular menstrual cycle, and laparoscopic and
histopathological findings, the first three of these hypotheses are
not suitable. The fourth hypothesis is consistent with the findings
that CK7, vimentin and CA125 were positive in the present case.
From these viewpoints, the tumor may have arisen directly from the
metaplasia of embryological Müllerian-duct remnants.
The treatment and prognosis of the six cases of PARS
without associated endometriosis reported in the literature are
summarized in Table I. As this
neoplasm is rare, it is difficult to determine the recommended
treatment protocol. However, surgery appears to be one of the
curative treatments. Considering the location of the tumor, PARS
may infiltrate the rectum when the tumor becomes enlarged. In these
cases, resection of the rectum is necessary to perform complete
excision of the tumor. As laparoscopic surgery provides a detailed
view and enables meticulous dissection compared with laparotomy, it
results in minimal intraoperative blood loss and complications,
fewer postoperative complications and a shorter hospital stay.
Considering these advantages of laparoscopic surgery, laparoscopic
PPE and rectosigmoid anastomosis were performed in the case
reported here; histopathologically, R0 resection was achieved.
However, depending on cases, terminal colostomy may be necessary.
As for postoperative adjuvant therapy, there are reports that the
combination of CP therapy was effective. In addition, considering
the complications of postoperative radiation therapy, the patient
was treated with combined CP + Bev therapy according to the
treatment of ovarian cancer (9).
However, the patient showed multiple distant metastases during Bev
monotherapy. At present, there have been no results of phase three
trials evaluating the efficacy of single agent chemotherapy + Bev
in patients with platinum-resistant ovarian cancer previously
treated with Bev. Previous reports on colorectal and breast cancer
show the efficacy of standard second-line chemotherapy + Bev beyond
progressive disease (19–21). Therefore, in the present case, PLD +
Bev therapy was initiated as the second-line chemotherapy. As PARS
without endometriosis is a rare neoplasm, further investigations
are expected to determine the recommended treatment for this
neoplasm.
 | Table I.Primary carcinoma of the rectovaginal
septum without associated endometriosis reported in the
literature. |
Table I.
Primary carcinoma of the rectovaginal
septum without associated endometriosis reported in the
literature.
| Author, year | Age (years) | Tumor diameter
(cm) | Pathological
diagnosis | Treatment | Prognosis from
initial treatment | Refs. |
|---|
| Davis, 1967 | 53 | Unknown | Carcinoma of ER | TAH, ApRR | DOD 11 months
later | (3) |
| Berger et al,
2001 | 58 | 6 | Adenocarcinoma of
EMR | 1. TAH, BO, large
biopsy of tumor; | AWD 60 months
later | (4) |
|
|
|
|
| 2. ApRR, total
colpectomy; |
|
|
|
|
|
|
| 3. Radiotherapy; |
|
|
|
|
|
|
| 4. Chemotherapy |
|
|
| Giordano et
al, 2010 | 37 | 9 | Adenocarcinoma | 1.TAH, BSO, partial
colpectomy, LCR; | AWD 12 months
later | (5) |
|
|
|
|
| 2. Chemotherapy (CP,
6 cycles) |
|
|
| Papacharalabous et
al, 2004 | 57 | 7 | Adenocarcinoma | TAH, BSO, LCR | NED at 12 months | (6) |
| Guiou et al,
2008 | 52 | 5 | Adenocarcinoma
therapy (PP) | Concurrent
chemoradiation at 84 months | NED | (7) |
| Langmár et al,
2008 | 68 | 3.7 | Adenocarcinoma | 1. TAH, BSO, partial
colpectomy, LCR; | NED at 25 months | (8) |
|
|
|
|
| 2. Postoperative
chemotherapy (CP, 6 cycles) |
|
|
The number of cases of PARS without associated
endometriosis is too small to draw any definitive conclusions.
However, the prognosis of the disease may be considered poor. One
of the reasons may be the delay in diagnosis (4). Other reasons may include the malignancy
of the tumor itself, including the grade of the tumor and genetic
damage of cancer-related genes, as with other carcinomas. Poorly
differentiated adenocarcinoma is known to have higher malignant
potential compared with well-differentiated adenocarcinoma. In
addition, aberrant mitotic figures are associated with the mutation
of p53 (22), and mutation of p53 is
associated with poor prognosis in human cance (23,24). In
the present study, the histopathology of the tumor revealed poorly
differentiated adenocarcinoma with aberrant mitotic figures, and
these factors were considered to affect the poor prognosis.
In conclusion, the present report describes a case
of PARS without associated endometriosis, which may have arisen
from metaplasia of embryological Müllerian-duct remnants. Only six
previous cases of this neoplasm have been reported, and the present
case is, to the best of our knowledge, the first case to be treated
with laparoscopic PPE. As this neoplasm is rare, no standard
treatment has been established. Therefore, the accumulation of
management data on this rare neoplasm is important.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
TF, FT, and SK performed the case study, collected
the data and images of the case and produced the draft of the
manuscript. NO performed the immunohistochemical staining and the
histopathological diagnosis. All authors read and approved the
final manuscript.
Patient consent for publication
Consent to publish was obtained from the legal
relative (husband) of the patient, as she passed away prior to
manuscript planning and writing.
Ethics approval and consent to
participate
The present study was approved by the Medical Ethics
Committee of the Hakodate Central General Hospital.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ulrich U, Rhiem K, Kaminski M, Wardelmann
E, Trog D, Valter M and Richter ON: Parametrial and rectovaginal
adenocarcinoma arising from endometriosis. Int J Gynecol Cancer.
15:1206–1209. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Yazbeck C, Poncelet C, Chosidow D and
Madelenat P: Primary adenocarcinoma arising from endometriosis of
the rectovaginal septum: A case report. Int J Gynecol Cancer.
15:1203–1205. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Davis JM: Carcinoma in the rectovaginal
septum. Proc R Soc Med. 60:5021967.PubMed/NCBI
|
|
4
|
Berger A, Rouzier R, Carnot F, Braunberger
E, Cugnenc PH and Danel C: Primary adenocarcinoma of the
rectovaginal septum: A case report and literature review. Eur J
Obstet Gynecol Reprod Biol. 95:111–113. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Giordano G, Bersiga A, Marchetti G and
Melpignano M: Primary adenocarcinoma of the rectovaginal septum
arising in pregnancy in the absence of endometriosis. Eur J
Gynaecol Oncol. 31:211–213. 2010.PubMed/NCBI
|
|
6
|
Papacharalabous EN, Awad SA and Edwards
JL: A malignant tumour of the rectovaginal septum not arising from
endometriosis, presenting a diagnostic enigma. J Obstet Gynaecol.
24:599–600. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Guiou M, Hall WH, Konia T, Scudder S,
Leiserowitz G and Ryu JK: Primary clear cell adenocarcinoma of the
rectovaginal septum treated with concurrent chemoradiation therapy:
A case report. Int J Gynecol Cancer. 18:1118–1121. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Langmár Z, Harsányi L, Székely E, Járay B,
Csömör S and Kazy Z: Primary adenocarcinoma of the rectovaginal
septum without associated endometriosis. Orv Hetil. 149:2251–2253.
2008.(In Hungarian). View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Burger RA, Brady MF, Bookman MA, Fleming
GF, Monk BJ, Huang H, Mannel RS, Homesley HD, Fowler J, Greer BE,
et al; Gynecologic Oncology Group, . Incorporation of bevacizumab
in the primary treatment of ovarian cancer. N Engl J Med.
365:2473–2483. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Pujade-Lauraine E, Hilpert F, Weber B,
Reuss A, Poveda A, Kristensen G, Sorio R, Vergote I, Witteveen P,
Bamias A, et al: Bevacizumab combined with chemotherapy for
platinum-resistant recurrent ovarian cancer: The AURELIA open-label
randomized phase III trial. J Clin Oncol. 32:1302–1308. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Schut N: A neurilemmoma (schwannoma) in
the rectovaginal septum. Bull Soc R Belge Gynecol Obstet.
31:381–385. 1961.(In Dutch). PubMed/NCBI
|
|
12
|
Acién P, Núñez C, Quereda F, Velasco I,
Valiente M and Vidal V: Is a bowel resection necessary for deep
endometriosis with rectovaginal or colorectal involvement? Int J
Womens Health. 5:449–455. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Brown KL, Segal AJ and Hurd GB: Masses of
the rectovaginal septum. A proposed classification, review of the
literature and report of a case of leiomyosarcoma. Am J Surg.
99:309–315. 1960. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Petković M, Zamolo G, Muhvić D, Coklo M,
Stifter S and Antulov R: The first report of extraosseous Ewing's
sarcoma in the rectovaginal septum. Tumori. 88:345–346. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lam MM, Corless CL, Goldblum JR, Heinrich
MC, Downs-Kelly E and Rubin BP: Extragastrointestinal stromal
tumors presenting as vulvovaginal/rectovaginal septal masses: A
diagnostic pitfall. Int J Gynecol Pathol. 25:288–292. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Berezowski K, Stastny JF and Kornstein MJ:
Cytokeratins 7 and 20 and carcinoembryonic antigen in ovarian and
colonic carcinoma. Mod Pathol. 9:426–429. 1996.PubMed/NCBI
|
|
17
|
Han AC, Hovenden S, Rosenblum NG and
Salazar H: Adenocarcinoma arising in extragonadal endometriosis: An
immunohistochemical study. Cancer. 83:1163–1169. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Nisolle M and Donnez J: Peritoneal
endometriosis, ovarian endometriosis, and adenomyotic nodules of
the rectovaginal septum are three different entities. Fertil
Steri1. 68:585–596. 1997. View Article : Google Scholar
|
|
19
|
Bennouna J, Sastre J, Arnold D, Österlund
P, Greil R, Van Cutsem E, von Moos R, Viéitez JM, Bouché O, Borg C,
et al; ML18147 Study Investigators, . Continuation of bevacizumab
after first progression in metastatic colorectal cancer (ML18147):
A randomised phase 3 trial. Lancet Oncol. 14:29–37. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Grothey A, Sugrue MM, Purdie DM, Dong W,
Sargent D, Hedrick E and Kozloff M: Bevacizumab beyond first
progression is associated with prolonged overall survival in
metastatic colorectal cancer: Results from a large observational
cohort study (BRiTE). J Clin Oncol. 26:5326–5334. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
von Minckwitz G, Puglisi F, Cortes J,
Vrdoljak E, Marschner N, Zielinski C, Villanueva C, Romieu G, Lang
I, Ciruelos E, et al: Bevacizumab plus chemotherapy versus
chemotherapy alone as second-line treatment for patients with
HER2-negative locally recurrent or metastatic breast cancer after
first-line treatment with bevacizumab plus chemotherapy (TANIA): An
open-label, randomised phase 3 trial. Lancet Oncol. 15:1269–1278.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Steinbeck RG: Pathologic mitoses and
pathology of mitosis in tumorigenesis. Eur J Histochem. 45:311–318.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sadighi S, Zokaasadi M, Kasaeian A,
Maghsudi S, Jahanzad I and Kamranzadeh Fumani H: The effect of
immunohistochemically detected p53 accumulation in prognosis of
breast cancer; A retrospective survey of outcome. PLoS One.
12:e01824442017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Stelloo E, Bosse T, Nout RA, MacKay HJ,
Church DN, Nijman HW, Leary A, Edmondson RJ, Powell ME, Crosbie EJ,
et al: Refining prognosis and identifying targetable pathways for
high-risk endometrial cancer; a TransPORTEC initiative. Mod Pathol.
28:836–844. 2015. View Article : Google Scholar : PubMed/NCBI
|