Introduction
Esophageal cancer (EC) is the eighth most common
cancer worldwide, with an estimated 455,784 new cases diagnosed in
2012, and the sixth most common cause of death from cancer, with
400,169 deaths reported in 2012 (1).
Squamous cell carcinoma (SCC) is by far the most common form of EC
in Asian countries; adenocarcinomas of the lower third of the
esophagus are common in western countries but account for only 4.3%
of ECs in Japan (2). Surgery is
considered the treatment of choice for patients with locoregionally
confined EC. However, EC has a high rate of disease recurrence,
even after curative surgery (3–6).
Trimodality therapy, consisting of preoperative chemoradiation
followed by esophagectomy, was developed to improve the survival of
patients with locoregional EC, and has become the standard
treatment in the NCCN guidelines for patients with resectable
esophageal SCC (7). In Japan, the
standard treatment recommended by the Japan Clinical Oncology Group
(JCOG) 9907 Study for patients with UICC (Union for International
Cancer Control) stage II/III resectable SCC is a preoperative
chemotherapy regimen of 5-fluorouracil (5-FU) and cisplatin (CP;
the regimen: CF) followed by esophagectomy (8). In that randomized phase III trial,
patients in the neoadjuvant chemotherapy (NAC) +surgery group had a
better survival rate than patients in the postoperative adjuvant
group. However, the study was limited by its exclusion of patients
with pathological N0 disease from the adjuvant chemotherapy group
and the disparity of patients who received postoperative
chemotherapy (64.6%) and preoperative chemotherapy (97.0%).
Additionally, a subset analysis of the JCOG 9907 study showed that
NAC was not effective in patients with stage III disease or T3
tumors, thus demonstrating the need for more effective
perioperative intervention in these patients. To improve survival,
beginning in 1996, we introduced preoperative chemoradiotherapy
(CRT) for patients with resectable advanced EC. A subsequent
analysis showed increased tumor resectability, lower incidences of
both local recurrence and distant metastasis, and a more favorable
prognosis for CRT responders (9,10).
Additionally, a comparison of survival by patients with stage
II/III esophageal SCC treated with surgery alone vs. with a
protocol including neoadjuvant CRT showed that neoadjuvant CRT with
CF significantly improved disease-free survival (DFS) compared with
surgery alone (11); but these were
retrospective, observational studies that may have included some
confounding biases. Propensity score (PS) methods, including
inverse probability of treatment weighting (IPTW) and propensity
score matching (PSM) are used increasingly to reduce or minimize
confounding effects in evaluations of treatment, exposure, or
intervention based on observational or non-randomized data
(12). In our retrospective study of
patients with resectable EC, we compared those who received
neoadjuvant CRT plus surgery (trimodality therapy) with those
treated by surgery alone. After applying IPTW and PSM, we
investigated whether survival benefits were obtained for patients
in the neoadjuvant CRT plus surgery group.
Patients and methods
Patients with biopsy-proven, invasive SCC of the
esophagus that had not been previously treated were eligible for
the study. Other inclusion criteria were endoscopy and CT scan
and/or endoscopic ultrasound examination findings of resectable,
clinical stage II, III, or IV disease based on the UICC TNM
Classification of Malignant Tumors, 6th ed (13). Other eligibility criteria were as
follows: <80 years old, adequate organ function (WBC ≥3,500, Hb
≥10 g/dl, ALT/AST ≤2× upper limit of normal, platelets ≥100,000,
serum creatinine ≤1.3), and an Eastern Cooperative Oncology Group
performance status of <1 at the time of admission. The patients
who received chemotherapy, chemoradiotherapy or endocrine therapy
due to other malignancies were excluded in this study. We defined
T3.5 on CT scan as suspected T4, possibly down-staged following
neoadjuvant therapy, and included as T3. Of the 112 patients
entered into this study, 55 received preoperative CRT followed by
esophagectomy (Group A) and 57 underwent esophagectomy alone (Group
B) between August 1996 and June 2015 at the Department of Surgery,
Hyogo College of Medicine and Nara Hospital, Kindai University
School of Medicine, Japan. Most patients of Group A were treated in
Hyogo College of Medicine between 1996 to 2007, and most patients
of Group B were treated in Nara Hospital between 2002 to 2015. All
patients gave informed consent. This study was approved by the
Ethical Committees of both Nata Hospital (No. 377), Kindai
University School of Medicine (on the Kindai University web site);
and Hyogo College of Medicine (No. 2906; on their web site).
Neoadjuvant CRT followed by
esophagectomy
Preoperative radiotherapy was performed for 5 days
per week (Monday to Friday, 2 Gy/day) using a linear accelerator
(Mevatron KD2: Siemens, Germany). The radiation field encompassed
the primary tumor volume (as defined by endoscopy, esophagography,
and CT scan) with a 3-cm margin in the cephalad and caudal
directions and 4-cm horizontal margins. If lymph node metastasis
was detected by CT scan, the radiation field was extended to
include the primary tumor and metastatic lesions. Twenty fractions
of 2 Gy each were delivered for a total of 40 Gy of radiation per
patient. Concurrent chemotherapy consisted of 5-FU (500
mg/m2/day) administered for 120 h via continuous
intravenous infusion starting on Day 1 and CP (15–20 mg/day)
administered as a 2-h intravenous infusion on Days 1–5, repeated
after 3 weeks.
Response to CRT was defined according to the
criteria of RECIST guideline (version 1.1) (14). Esophagectomy was planned for 4–7
weeks after the completion of CRT. Most patients underwent
thoracotomy, laparotomy, and cervicotomy in conjunction with the
esophagectomy and two- or three-field lymphadenectomy.
Reconstruction always consisted of a gastric tube and
gastroesophageal anastomosis at the left side of the neck using a
retrosternal root. Radical resection (R0) was defined as the
removal of all macroscopic tumors with no evidence of distant
metastasis, the absence of microscopic residual tumor, free
resection margins, and lymphadenectomy extending beyond the
involved nodes. Resection was defined as non-radical when
microscopic (R1) or macroscopic (R2) residual tumor was found,
according to the TNM criteria (13).
Esophagectomy for surgery alone
Esophagectomy was performed together with a small
(~10 cm) thoracotomy via thoracoscopy-assisted esophagectomy, with
two- or three-field lymphadenectomy including the upper
mediastinum. Reconstruction was routinely performed using a
retrosternal root and a gastroesophageal anastomosis at the left
side of the neck. The degree of radical resection (R) was assessed
according to the TNM system (13).
Statistical analysis
The differences between the characteristics of
patients in Group A and Group B were analyzed using the chi-square,
Fisher's exact test and Mann-Whitney tests. Overall survival (OS)
was defined as the time from the date of initial treatment to
patient death or the date of the last available information on the
patient's vital status. DFS was defined as the period after
treatment during which time no cancer was found. With the unmatched
data, differences between the cumulative survival rates in the two
groups of patients were calculated using the log-rank test for
comparison, as well as Kaplan-Meier survival curves and unadjusted
Cox proportional hazard models. P<0.05 was considered
significant. Because therapy was not randomly assigned in this
patient population, potential confounding and selection biases were
accounted for by developing a PS, calculated using a multivariable
logistic regression model in which age, sex, cancer site
(location), primary tumor length, cTNM stage, lymph node
metastasis, and depth of tumor invasion (cT) were the independent
variables. After propensity scores were calculated, distributions
of propensity scores and it after IPTW in two evaluated groups were
analyzed by Kernel density estimation. Initially, the PSs were used
to match preoperative CRT patients to those treated by surgery
alone according to caliper matching in propensity score analysis.
Next, the PSs were used to match preoperative CRT patients to those
treated by surgery alone according to the IPTW method. IPTW was
calculated from following formula: [1/PS] in Group A and [1/(1-PS)]
in Group B. After IPTW and PSM, prognosis of patients in the two
groups were examined using univariate analyses for OS and DFS. Cox
proportional hazard models for OS were then adjusted using the IPTW
values of the two groups and subgroups. Statistical analyses were
performed using STATA version13 (Stata Corp LP, College Station,
TX, USA), R version 3.1.1 (R Project for Statistical Computing,
Vienna, Austria) and JMP version 11 (SAS Institute Inc., Tokyo,
Japan).
Results
Patients characteristics in the
unmatched analysis
Characteristics of the 112 patients included in this
study are summarized in Table I.
Group A consisted of 55 patients treated with neoadjuvant
CRT+surgery, and Group B of 57 patients who underwent surgery only.
All tumors were histologically confirmed to be esophageal SCC. The
median age in Group A was significantly younger than in Group B,
and tumor locations were generally lower in Group B than in Group
A. Group B had a higher rate of cN0 disease than Group A. Although
the tumors of group A patients were longer than those of group B
patients, the difference in the cT between the two groups was not
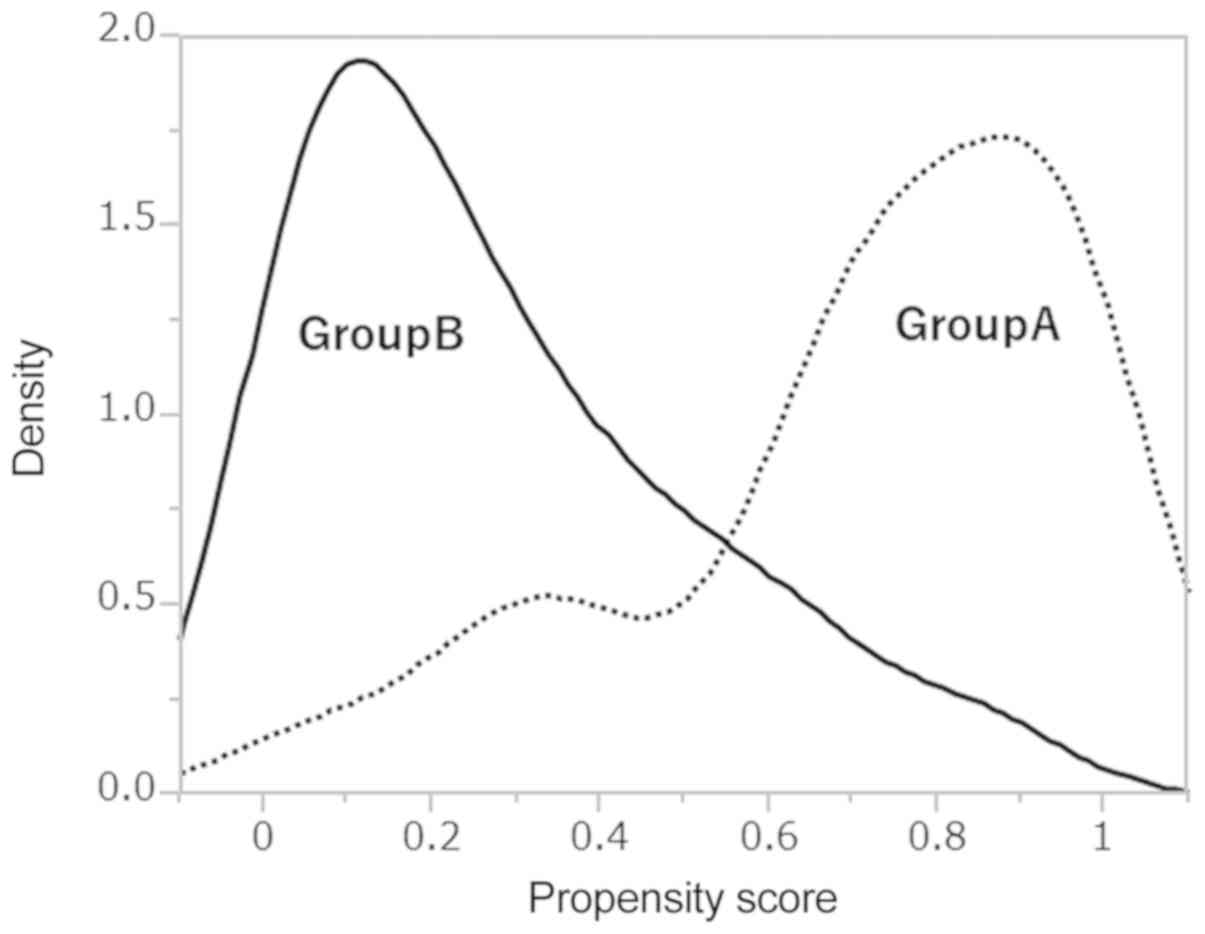
significant. PS distributions between the two treatment groups are
shown in Fig. 1, and shown in
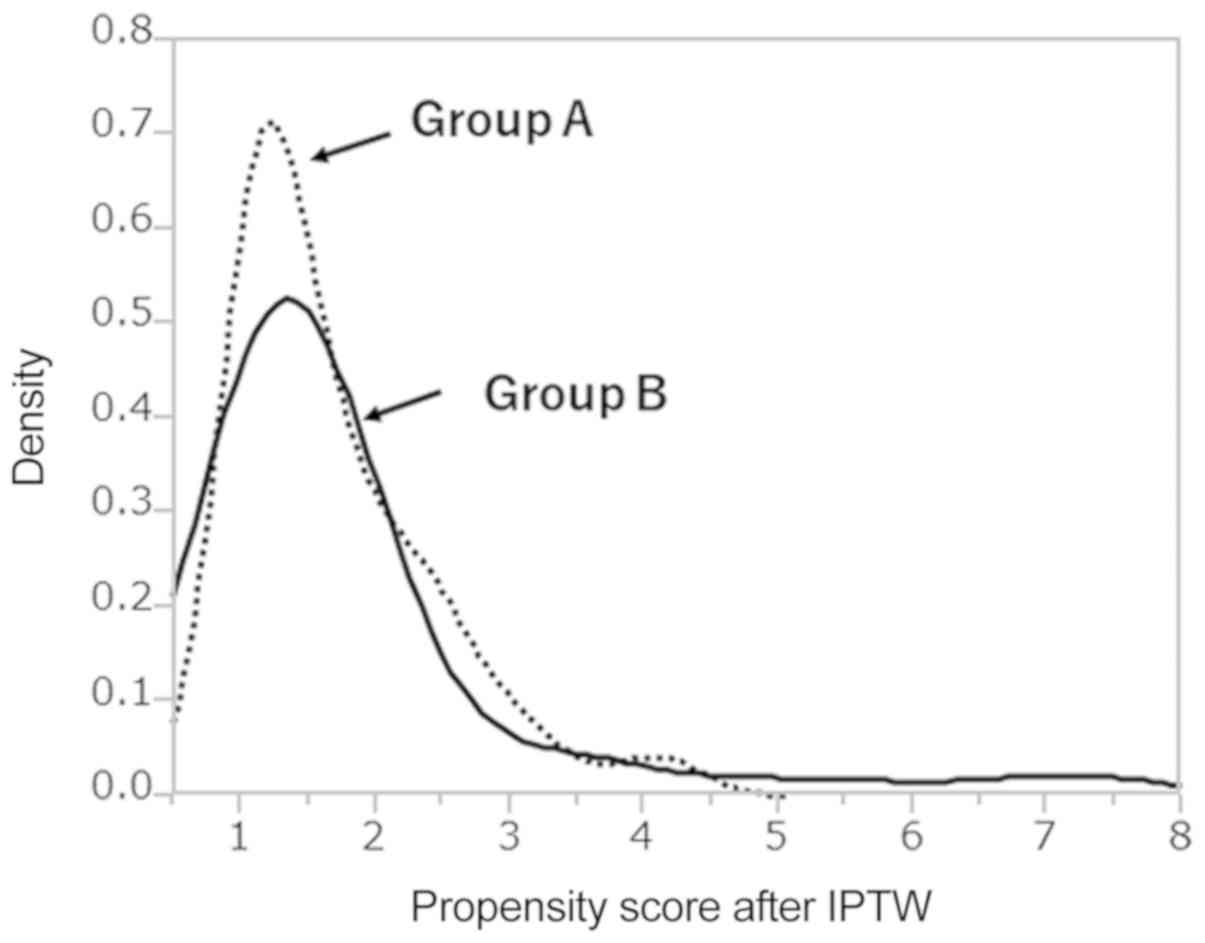
Fig. 2 after IPTW. The PS
distribution differed between the two groups. After IPTW, PSs were
similar between two groups. After PSs were calculated, 46 of 112
patients were matched by caliper-matching method (Table II). Group A and Group B did not
significantly differ in each parameter.
 | Table I.Patients characteristics in the
present study (n=112). |
Table I.
Patients characteristics in the
present study (n=112).
| Variable | Preoperative CRT
(group A) | Surgery alone
(group B) | P-value |
|---|
| No. of
patients | 55 | 57 |
|
| Age (years) | 60.49 | 65.19 | P<0.05 |
| Male/female | 44/10 | 48/9 | NS |
| Location of primary
tumor |
|
| P<0.05 |
|
Cervical | 1 | 0 |
|
| Upper
thoracic | 6 | 3 |
|
| Middle
thoracic | 32 | 23 |
|
| Lower
thoracic | 15 | 30 |
|
|
Abdominal | 1 | 1 |
|
| T-classification
(cT) |
|
| NS |
|
cT2 | 7 | 10 |
|
| cT3
(T3.5 included) | 45 | 46 |
|
|
cT4 | 3 | 1 |
|
| Tumor length | 6.76 | 5.05 | P<0.05 |
| Clinical stage (TNM
6th edition) |
|
| NS |
| II | 28 | 28 |
|
|
III | 21 | 26 |
|
| IV | 7 | 3 |
|
| N-classification
(cN) |
|
| P<0.05 |
| N0 | 36 | 18 |
|
| N1 | 19 | 39 |
|
| Resectability |
|
| NS |
| R0 | 40 | 50 |
|
| R1 | 15 | 6 |
|
| R2 | 0 | 1 |
|
 | Table II.Patients characteristics after
propensity score matching in the present study (n=46). |
Table II.
Patients characteristics after
propensity score matching in the present study (n=46).
| Variable | Preoperative CRT
(group A) | Surgery alone
(group B) |
|---|
| No. of
patients | 23 | 23 |
| Age (years) | 62.38 | 63.52 |
| Male/female | 20/3 | 19/4 |
| Location of primary
tumor |
|
|
|
Cervical | 1 | 0 |
| Upper
thoracic | 0 | 1 |
| Middle
thoracic | 12 | 11 |
| Lower
thoracic | 9 | 10 |
|
Abdominal | 1 | 1 |
| T-classification
(cT) |
|
|
|
cT2 | 1 | 2 |
| cT3
(T3.5 included) | 20 | 20 |
|
cT4 | 2 | 1 |
| Tumor length | 6.15 | 6 |
| Clinical stage |
|
|
| (TNM 6th
edition) |
| II | 9 | 12 |
|
III | 12 | 9 |
| IV | 2 | 2 |
| N-classification
(cN) |
|
|
| N0 | 8 | 10 |
| N1 | 15 | 13 |
| Resectability |
|
|
| R0 | 18 | 21 |
| R1 | 5 | 2 |
Effects of chemoradiation for Group
A
Clinical responses (complete responses +partial
responses) to neoadjuvant CRT for primary tumors and metastatic
nodes were noted in 45 of 55 patients (clinical response rate:
81.8%). All patients received R0 or R1 resections (Table I).
Survival analysis
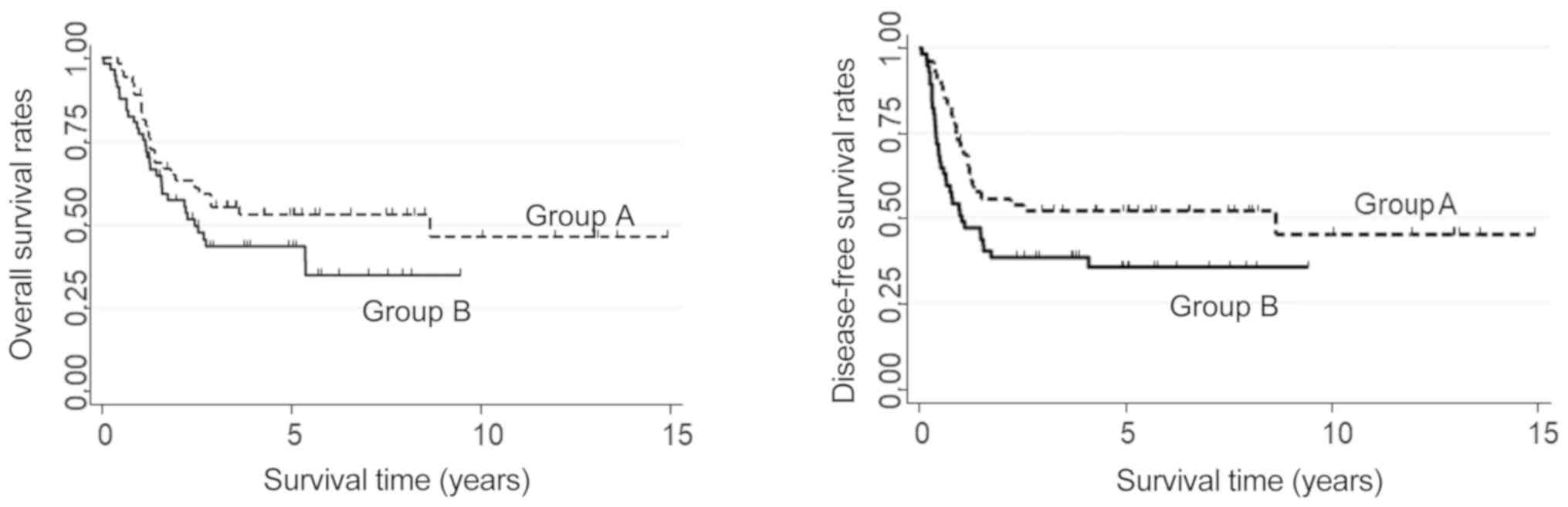
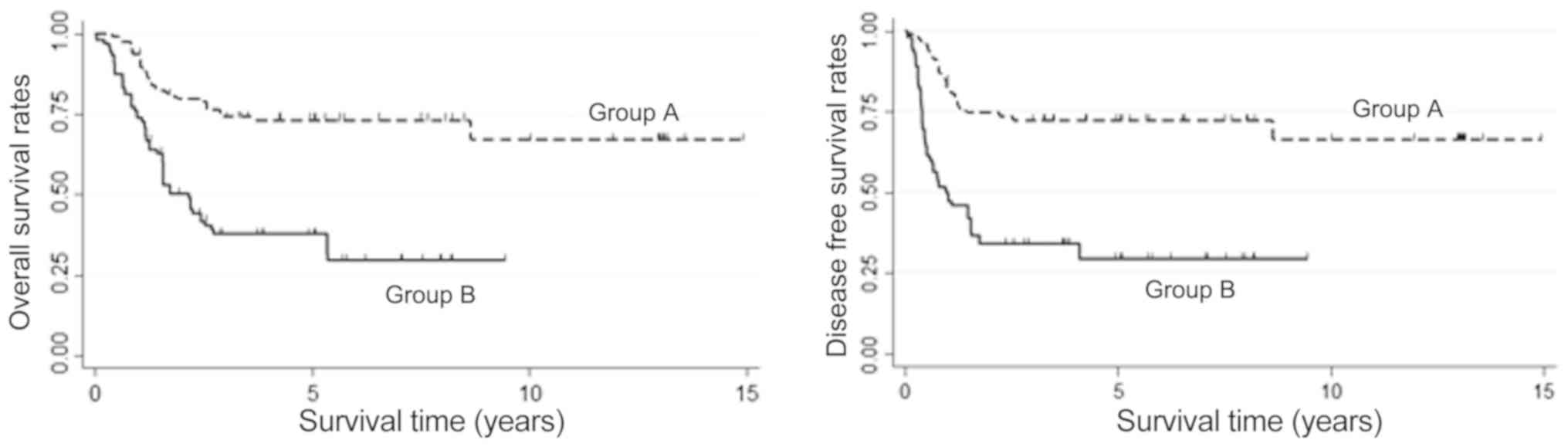
In the unadjusted data, OS was higher in Group A
than in Group B patients, but the difference was not significant.
The OS for Group A was 55.36% at 3 years and 53.06 at 5 years; in
Group B, the corresponding value at both time points was 43.44%
(P=0.138, Fig. 3). DFS was
significantly better in Group A than in Group B; in Group A, DFS at
3 and 5 years was 52.21%, whereas in Group B it was 38.7% at 3
years and 35.63% at 5 years (P<0.05, Fig. 3). In Group A, 5-year OS of patients
with R0 resections was significantly higher (72.93%) than in the R1
subgroup (6.25%, P<001). Also, 5-year OS of patients who
responded to CRT (63.01%) was better than in the non-responder
subgroup (0%; P<0.01).
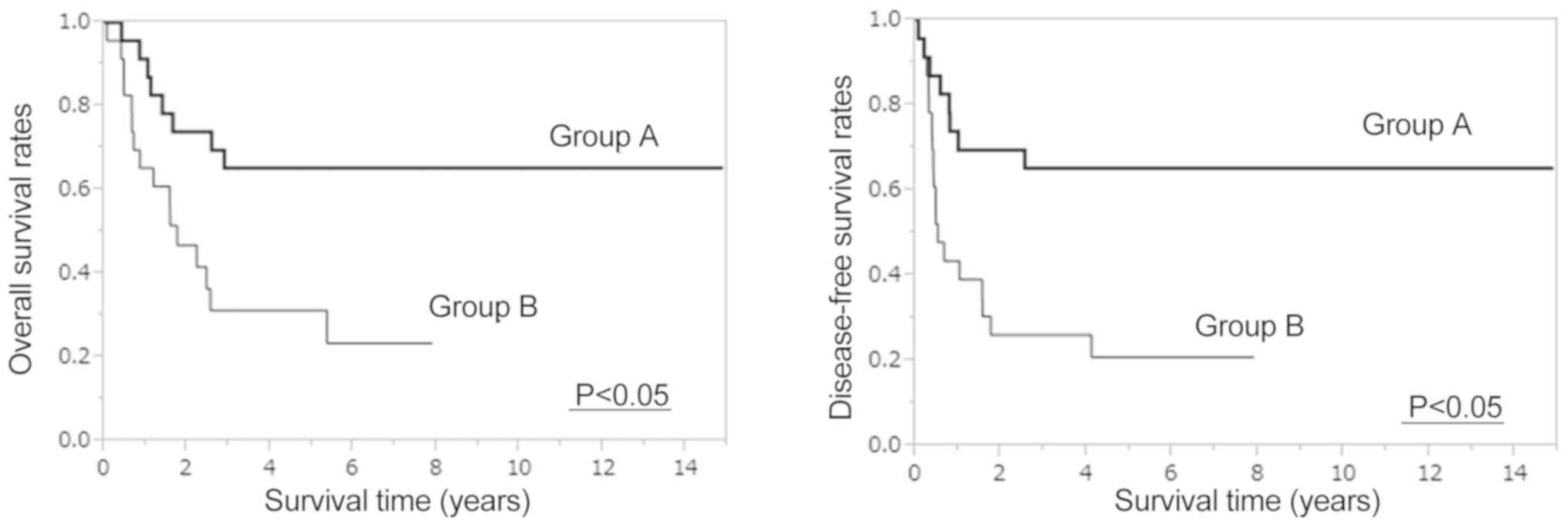
After PSM, both OS and DFS were significantly higher
in Group A than Group B (5-year OS: 65.2% vs. 31.2%, 5-year DFS:
65.2% vs. 20.9%, P<0.05, Fig. 4).
After IPTW was applied, OS was significantly higher in Group A than
in Group B, with 3- and 5-year rates of 73.77 and 73.18%,
respectively, vs. 37.69% each [hazard ratio (HR): 0.2899, 95%
confidence interval (CI): 0.1167–0.7205, P<0.05, Fig. 5]. DFS was also significantly higher
in Group A than in Group B patients, with rates at 3 and 5 years of
72.38% each vs. 34.12 and 29.37% (HR: 0.2703, 95% CI:
0.1123–0.6506, P<0.05, Fig. 5).
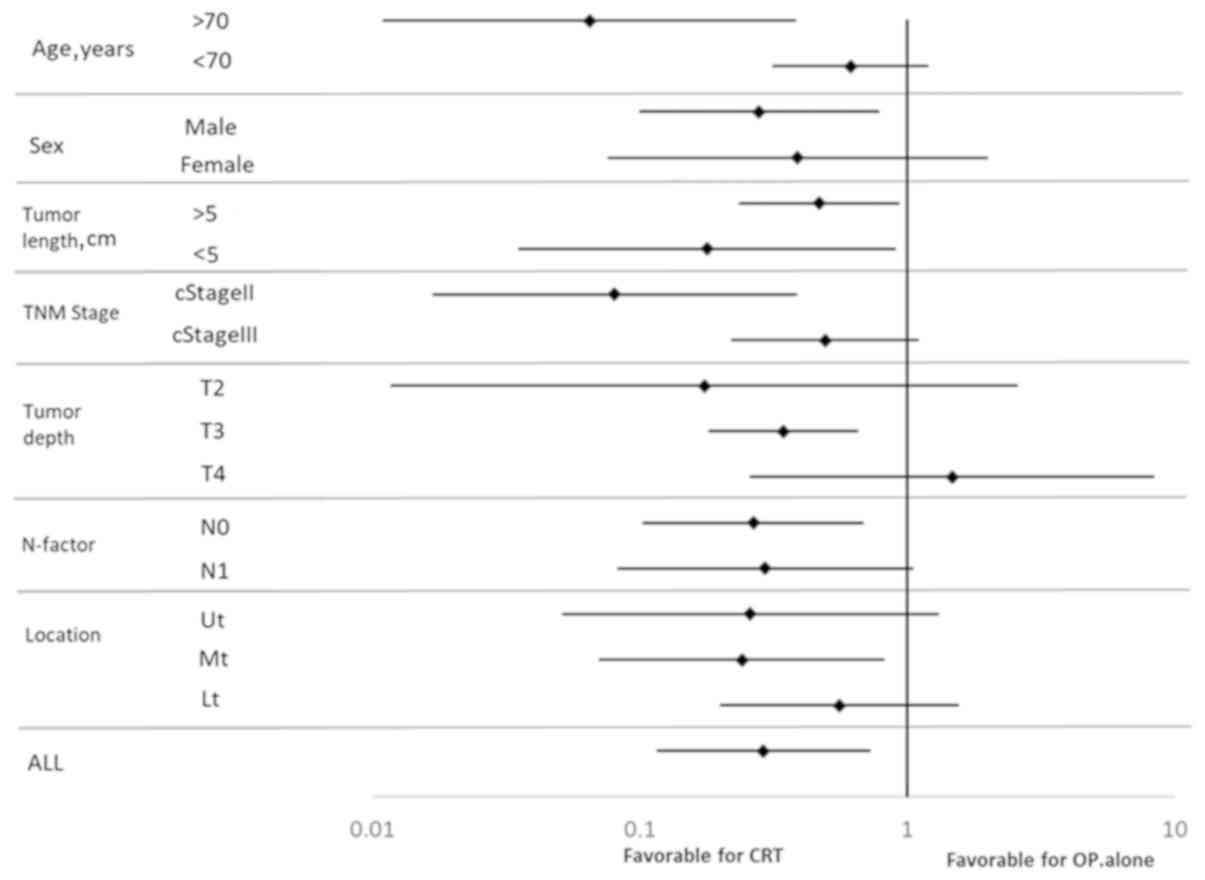
Results of subgroup analyses of OS with respect to clinical lymph
node status, cT, length, clinical stage, and location are shown in
Fig. 6. Treatment was more effective
in the preoperative CRT group with stage II disease that involved
the mid-esophagus, clinical N0, T3 status, and patients age >70
years. Preoperative CRT was significantly effective regardless of
tumor length.
Discussion
This study was carried out to evaluate the clinical
significance of preoperative CRT compared with surgery alone in
patients with resectable esophageal SCC. After applying IPTW and
PSM using PS, our results showed that preoperative CRT yielded
superior survival rates compared with surgery alone.
PS may be used four ways to reduce confounding: PS
matching, PS stratification, applying IPTW along with PS, and
covariate adjustment using PS (15,16).
Several studies have examined the performance of these different PS
methods for estimating treatment effects when the outcomes are
binary (17–20). Austin reported that PS matching and
application of the IPTW allow estimation of marginal HRs with
minimal bias. The study concluded that IPTW gave estimates with a
lower mean squared error when estimating the effect of treatment
(12). We therefore evaluated the
survival benefit of preoperative CRT vs. surgery alone after
applying both PS matching and IPTW. Four reports employed a
prognostic analysis using IPTW to analyze the data of patients with
gastric and EC (21–24). Two of those reports used PS matching
and IPTW to evaluate the effects of perioperative chemotherapy in
patients with gastroesophageal adenocarcinoma (23,24).
Fiteni et al reported better outcomes with perioperative
chemotherapy [docetaxel, cisplatin, and fluorouracil (DCF) regimen]
than with surgery alone, after applying both IPTW and PS matching
to the analysis. However, Kim et al compared standard CF
therapy with DCF therapy and obtained better outcomes from DCF,
using IPTW but not PS matching. The authors explained the different
results by the smaller sample size in the PS matched group, noting
that when the sample size is small, IPTW is more reliable than PS
matching. We used these two methods to analyze survival after
esophagectomy. Fortunately, the same results were obtained in two
analytical methods.
As shown in Fig. 1,
the density of propensity scores had different distributions in
both groups; therefore the number of matched patients had
decreased. Because only 46/112 (41.1%) of patients were matched in
the present study, statistical errors might have occurred. However,
distributions of PS after IPTW were similar in both evaluated
groups as shown in Fig. 2. The IPTW
is not a method of increasing the number of patients, but rather a
method to estimate a large amount of information from little
information without changing the number of patients. When the
number of patients is small, it might be necessary to evaluated
both PS matching and IPTW. Two other reports assessed only patients
with EC, and used only the IPTW method (21,22). In
the study of Guttmann et al, outcomes of elderly patients
with EC treated with preoperative CRT vs. surgery alone was
examined using the IPTW method, with better outcome noted in the
preoperative CRT group. Also, Yendamuri et al reported that
IPTW is preferred to matching, and other methods, in the context of
a time-to-event analysis to estimate the average treatment effect.
They evaluated the clinical characteristics of esophageal
adenosquamous cell carcinoma, and compared adenocarcinoma and SCC.
As adenosquamous cell carcinoma makes up only 1% (n=284) of 28,110
EC cases in the SEER database, therefore, it is presumed that they
preferred only IPTW metho. Based on these four papers, in our
evaluation of the two types of treatment, IPTW seemed to be the
better method of analysis rather than PSM, especially it is
considered to be excellent analysis for PS when the number of
patients is small.
In Japan the standard treatment of resectable EC is
preoperative chemotherapy using 5-FU + CP, established in the JCOG
9907 study (8). However, in the NCCN
guidelines, the standard treatment of SCC staged as T1b-T4a, N0-N+
or M0 is preoperative chemoradiation followed by esophagectomy
(7). The preferred CRT regimens are
paclitaxel/carboplatin, 5-FU/CP or 5-FU/oxaliplatin, and the
recommended irradiation dose is 41.4–50.4 Gy.
In the ESMO guideline, standard treatment of
local/locoregional (M0) SCC is neoadjuvant chemoradiation followed
by esophagectomy (25). This
guideline for EC was based on a meta-analysis and the results of
the CROSS trial (26–29), in which patients were treated with
carboplatin, paclitaxel, and 41.4 Gy of irradiation followed by
surgery. The median survival of these patients was 81.6 months in
the neoadjuvant CRT group and 21.1 months in the group treated with
surgery alone; the difference was statistically significant.
Despite the high survival rates reported with this regimen, our
patients did not receive carboplatin because it has not been tested
in a clinical trial in Japan. Clinical trials of this regimen
should be planned to verify its efficacy in Japanese patients with
EC.
Despite its long study period, the survival rates of
our present study were similar to those of the JCOG 9907 study;
therefore, we believe our present survival rates warrant
evaluation. As no randomized clinical report of preoperative CRT
vs. surgery alone in Japan is available, quasi-randomization using
propensity scores, as we have done here, are clinically useful.
Subgroup analysis after IPTW also showed that
preoperative CRT was more effective in patients with the following
characteristics: >70 years of age, male sex, clinical stage II,
T3 disease, mid-esophageal tumor, and clinical N0 disease. Notably,
preoperative CRT was more effective in treating T3 disease in the
present study cohort that in those included in the subgroup
analysis of the JCOG9907 report (8),
which further supports preoperative CRT in the treatment of
locoregional T3 disease. Although few papers report the effects of
preoperative chemotherapy or CRT by tumor locations, the CF regimen
might be especially effective for SCC of the mid esophagus
(8,30). The CROSS TRIAL results indicated that
CRT was more effective for clinical N0 disease; similar results
were obtained in this study. Additionally, preoperative CRT seemed
to be more effective for older patients in our study; however, we
cannot explain the reason for this result, as conflicting data also
exist (30).
In Japan, JCOG 1109 has been planned to verify the
effectiveness of preoperative CRT in patients with stage II/III
esophageal SCC. JCOG 1109 has three arms and is a randomized phase
III study to compare preoperative chemotherapy with CF,
preoperative CRT, and preoperative DCF chemotherapy. The results of
this study are upcoming as of this writing.
In conclusion, after applying IPTW using the PS and
PSM, we found that preoperative CRT plus esophagectomy led to
superior survival than surgery alone in patients with esophageal
SCC. Until the results of the JCOG1109 are available, our study
supports the benefit of neoadjuvant CRT for EC patients, including
those with T3 or higher disease. We also showed that IPTW using PS
is an important statistical method in studies based on
retrospective data derived from actual clinical practice.
Acknowledgements
The authors would like to thank Mrs. Kaku, medical
assistant at Kindai University Hospital, for her assistance with
data collection. The abstract was presented at American Society of
Clinical Oncology (ASCO) 2016 annual meeting, June 3–7 2016 in
Chicago and published as abstract no. e15532 in Journal of Clinical
Oncology 34 (no. 15_Suppl): 2016.
Funding
No funding was received.
Availability of data and materials
All data and materials in the present study were
anonymized. All data generated or analyzed during this study are
included in this published article.
Authors' contributions
YF, SF, MT, MY, MI and KK collaborated in the study
design, YF and SF collected and analyzed the data. YF, TU and MT
also performed data analysis. MT was a major contributor in
statistical analysis. AT, HK and MH constructed the figures. The
tables of this article were constructed by YF, MO, HK and YW. YF,
MH, HK and YW drafted the manuscript.
Ethics approval and consent to
participate
All study participants provided their informed
consent. The study design was approved by an ethics review board
(authorization no. 377, Nata Hospital, Kinki University School of
Medicine, 2906, Hyogo College of Medicine). Our study conforms to
the guidelines set forth in the Helsinki Declaration of 1975, as
revised in 2000 (5), concerning
Human and Animal Rights, and the policy concerning informed consent
was followed.
Patient consent for publication
All patients consented to publication at the time of
their surgeries.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
CF
|
fluorouracil and cisplatin regimen
|
|
CP
|
cisplatin
|
|
CRT
|
chemoradiotherapy
|
|
DCF
|
docetaxel, cisplatin, and
fluorouracil
|
|
DFS
|
disease-free survival
|
|
EC
|
esophageal cancer
|
|
IPTW
|
inverse probability of treatment
weighting
|
|
OS
|
overall survival
|
|
PS
|
propensity score
|
|
PSM
|
propensity score matching
|
|
SCC
|
squamous cell carcinoma
|
References
|
1
|
Roth JA and Putnam JB Jr: Surgery for
cancer of the esophagus. Semin Oncol. 21:453–461. 1994.PubMed/NCBI
|
|
2
|
Tachimori Y, Ozawa S, Numasaki H,
Fujishiro M, Matsubara H, Oyama T, Shinoda M, Toh Y, Udagawa H and
Uno T; Registration Committee for Esophageal Cancer of the Japan
Esophageal Society, : Comprehensive registry of esophageal cancer
in Japan, 2009. Esophagus. 13:110–137. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dresner SM and Griffin SM: Pattern of
recurrence following radical oesophagectomy with two-field
lymphadenectomy. Br J Surg. 87:1426–1433. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hulscher JB, van Sandick JW, Tijssen JG,
Obertop H and van Lanschot JJ: The recurrence pattern of esophageal
carcinoma after transhiatal resection. J Am Coll Surg. 191:143–148.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nakagawa S, Kanda T, Kosugi S, Ohashi M,
Suzuki T and Hatakeyama K: Recurrence pattern of squamous cell
carcinoma of the thoracic esophagus after extended radical
esophagectomy with three-field lymphadenectomy. J Am Coll Surg.
198:205–211. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Isono K, Sato H and Nakayama K: Results of
a nationwide study on the three-field lymph node dissection of
esophageal cancer. Oncology. 48:411–420. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ajani JA and D'Amico TA: Esophageal and
Esophagogastric Junction Cancers in NCCN Clinical Practice
Guidelines in Oncology (NCCN Guidelines version 1.2018). https://www.nccn.org/professionals/physician_gls/pdf/esophageal.pdf
|
|
8
|
Ando N, Kato H, Igaki H, Shinoda M, Ozawa
S, Shimizu H, Nakamura T, Yabusaki H, Aoyama N, Kurita A, et al: A
randomized trial comparing postoperative adjuvant chemotherapy with
cisplatin and 5-fluorouracil versus preoperative chemotherapy for
localized advanced squamous cell carcinoma of the thoracic
esophagus (JCOG9907). Ann Surg Oncol. 19:68–74. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Fujiwara Y, Kamikonya N, Inoue T, Koishi
K, Yoshikawa R, Nakao K, Yagyu R, Nishiwaki M, Fujiwara M, Kojima
S, et al: Chemoradiotherapy for T3 and T4 squamous cell carcinoma
of the esophagus using low-dose FP and radiation: A preliminary
report. Oncol Rep. 14:1177–1182. 2005.PubMed/NCBI
|
|
10
|
Fujiwara Y, Yoshikawa R, Kamikonya N,
Nakayama T, Kitani K, Tsujie M, Yukawa M, Inoue M and Yamamura T:
Trimodality therapy of esophagectomy plus neoadjuvant
chemoradiotherapy improves the survival of clinical stage II/III
esophageal squamous cell carcinoma patients. Oncol Rep. 28:446–452.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Fujiwara Y, Yoshikawa R, Kamikonya N,
Nakayama T, Kitani K, Tsujie M, Yukawa M, Hara J, Yamamura T and
Inoue M: Neoadjuvant chemoradiotherapy followed by esophagectomy
vs. surgery alone in the treatment of resectable esophageal
squamous cell carcinoma. Mol Clin Oncol. 1:773–779. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Austin PC: The performance of different
propensity score methods for estimating marginal hazard ratios.
Stat Med. 32:2837–2849. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sobin LH and Wittekind C: International
Union Against Cancer (UICC). TNM Classification of Malignant Tumors
(6th). Wiley-Liss. (New York). 2002.
|
|
14
|
Eisenhauer EA, Therasse P, Bogaerts J,
Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S,
Mooney M, et al: New response evaluation criteria in solid tumours:
Revised RECIST guideline (version 1.1). Eur J Cancer. 45:228–247.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Weitzen S, Lapane KL, Toledano AY, Hume AL
and Mor V: Principles for modeling propensity scores in medical
research: A systematic literature review. Pharmacoepidemiol Drug
Saf. 13:841–853. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
16
|
Austin PC: A critical appraisal of
propensity-score matching in the medical literature between 1996
and 2003. Stat Med. 27:2037–2049. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Austin PC, Grootendorst P, Normand SL and
Anderson GM: Conditioning on the propensity score can result in
biased estimation of common measures of treatment effect: A monte
carlo study. Stat Med. 26:754–768. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Austin PC: The performance of different
propensity-score methods for estimating relative risks. J Clin
Epidemiol. 61:537–545. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Austin PC: The performance of different
propensity-score methods for estimating differences in proportions
(risk differences or absolute risk reductions) in observational
studies. Stat Med. 29:2137–2148. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
20
|
Austin PC: The performance of different
propensity score methods for estimating marginal odds ratios. Stat
Med. 26:3078–3094. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
21
|
Guttmann DM, Mitra N, Metz JM, Plastaras
J, Feng W and Swisher-McClure S: Neoadjuvant chemoradiation is
associated with improved overall survival in older patients with
esophageal cancer. J Geriatr Oncol. 9:40–46. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yendamuri S, Malhotra U, Hennon M, Miller
A, Groman A, Halloon A and Reid ME: Clinical characteristics of
adenosquamous esophageal carcinoma. J Gastrointest Oncol. 8:89–95.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Fiteni F, Paget-Bailly S, Messager M,
N'Guyen T, Lakkis Z, Mathieu P, Lamfichekh N, Picard A, Benzidane
B, Cléau D, et al: Docetaxel, Cisplatin, and 5-Fluorouracil as
perioperative chemotherapy compared with surgery alone for
resectable gastroesophageal adenocarcinoma. Cancer Med.
5:3085–3093. 2016. View
Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kim S, Paget-Bailly S, Messager M, Nguyen
T, Mathieu P, Lamfichekh N, Fein F, Fratté S, Cléau D, Lakkis Z, et
al: Perioperative docetaxel, cisplatin, and 5-fluorouracil compared
to standard chemotherapy for resectable gastroesophageal
adenocarcinoma. Eur J Surg Oncol. 43:218–225. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lordick F, Mariette C, Haustermans K,
Obermannová R and Arnold D; ESMO guidelines committee, :
oesophageal cancer: ESMO clinical practice guidelines for
diagnosis, treatment and follow-up. Ann Oncol. 27 (Suppl
5):v50–v57. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kranzfelder M, Schuster T, Geinitz H,
Friess H and Büchler P: Meta-analysis of neoadjuvant treatment
modalities and definitive non-surgical therapy for oesophageal
squamous cell cancer. Br J Surg. 98:768–783. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Sjoquist KM, Burmeister BH, Smithers BM,
Zalcberg JR, Simes RJ, Barbour A and Gebski V; Australasian
Gastro-Intestinal Trials Group, : Survival after neoadjuvant
chemotherapy or chemoradiotherapy for resectable oesophageal
carcinoma: An updated meta-analysis. Lancet Oncol. 12:681–692.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Markar SR, Karthikesalingam A, Thrumurthy
S and Low DE: Volume-outcome relationship in surgery for esophageal
malignancy: Systematic review and meta-analysis 2000–2011. J
Gastrointestinal Surg. 16:1055–1063. 2012. View Article : Google Scholar
|
|
29
|
Shapiro J, van Lanschot JJB, Hulshof MCCM,
van Hagen P, van Berge Henegouwen MI, Wijnhoven BPL, van Laarhoven
HWM, Nieuwenhuijzen GAP, Hospers GAP, Bonenkamp JJ, et al: CROSS
study group: Neoadjuvant chemoradiotherapy plus surgery versus
surgery alone for oesophageal or junctional cancer (CROSS):
Long-term results of a randomised controlled trial. Lancet Oncol.
16:1090–1098. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Burmeister BH, Smithers BM, Gebski V,
Fitzgerald L, Simes RJ, Devitt P, Ackland S, Gotley DC, Joseph D,
Millar J, et al: Surgery alone versus chemoradiotherapy followed by
surgery for resectable cancer of the oesophagus: A randomised
controlled phase III trial. Lancet Oncol. 6:659–668. 2005.
View Article : Google Scholar : PubMed/NCBI
|