Introduction
Primary idiopathic osteolysis is rare and is
classified into five types (1,2).
Gorham-Stout disease (GSD, also known as ‘massive osteolysis,’
‘vanishing bone disease,’ ‘phantom bone disease,’ ‘Gorham's
disease,’ and ‘Gorham-Stout syndrome’) is a type of idiopathic
osteolysis and is a very rare bone condition that is characterized
by spontaneous, idiopathic, and progressive proliferation of blood
or lymphatic vessels that replace the bone and marrow space with
fibrous connective tissue (3). The
precise etiology and pathophysiology of GSD remain poorly
understood. The first reported case of GSD was in 1838 by Jackson
(4). Since then, over 300 cases have
been reported in the literature worldwide (3). GSD has no predilection for a particular
sex or race, and it may occur at any age, although it is diagnosed
more often in adolescents and children. Bones are affected in a
monocentric manner, although there are reports of continuity to
adjacent bone structures (5). GSD
affects various bones (6,7). Although the most common initial symptom
is a finding of pathological fractures (8), the symptoms of GSD vary and depend on
which sites of the body are affected. Because of uncertainty about
the underlying cause, the appropriate treatment and prognosis also
remain uncertain. A medical approach (9,10),
surgery, and radiotherapy (11) are
options that have been attempted in isolated cases, with differing
degrees of success. Although GSD generally has a good prognosis,
life threatening complications may occur owing to the involvement
of the spine, viscera, or chest, resulting in chylothorax (12).
To the best of our knowledge, this is the first
reported case of GSD in the rib and thoracic spine with spinal
injury to be treated with radiotherapy, propranolol, vitamin D, and
zoledronic acid. Here, we report our experience along with a review
of existing literature.
Case report
We report about a 77-year-old man without any past
medical or family history. He visited our department of internal
medicine with complaints of constipation continuing for 10 days. A
few days later, he recognized weakness and numbness in both legs.
These lower extremity symptoms worsened and progressed to paralysis
of the 6th thoracic spinal cord within a few days. The neurological
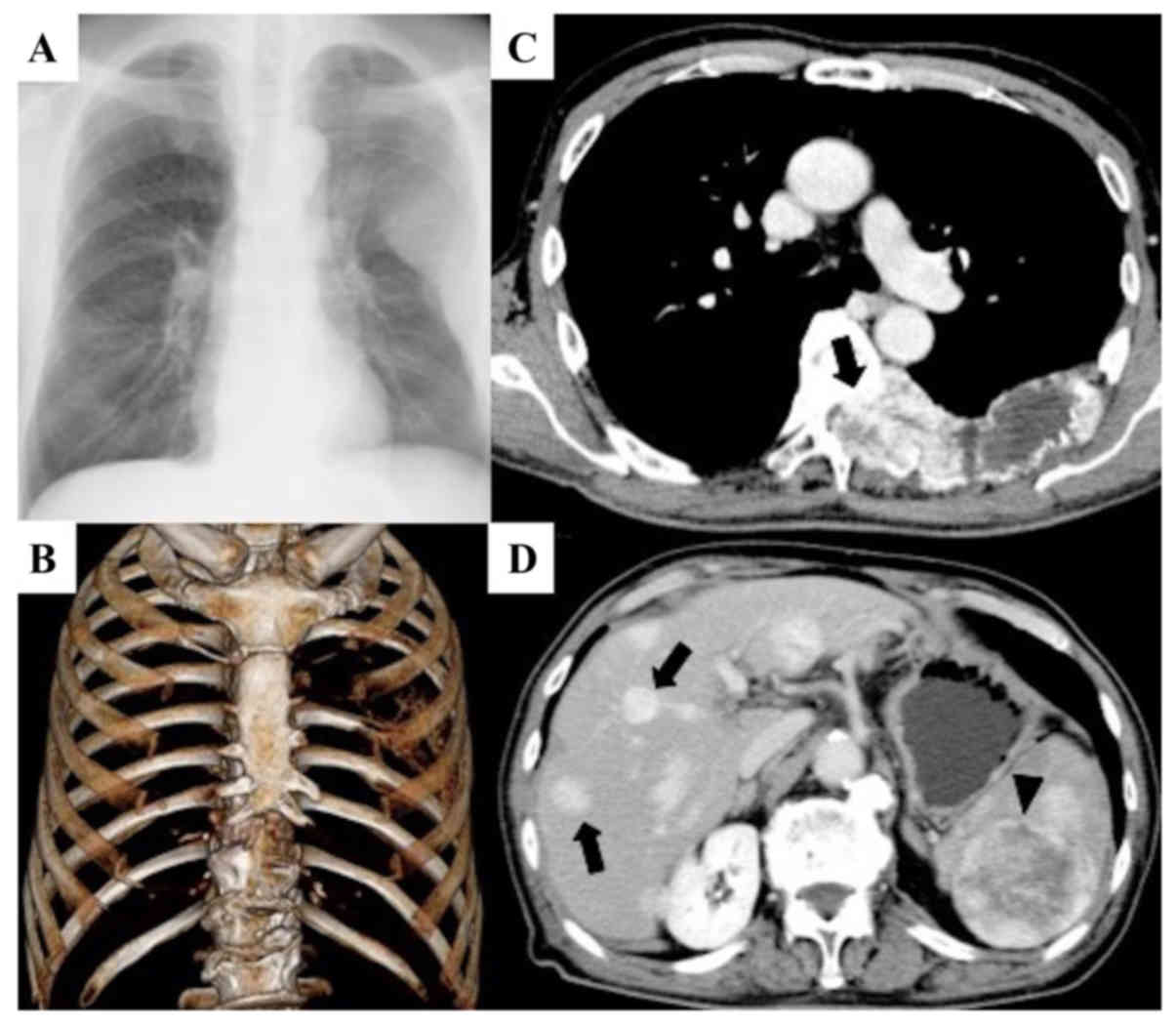
status was grade A according to the Frankel scale (13). Radiologically, massive osteolytic
lesions were confirmed in the 6, 7 and 8th right ribs and in the 6
and 7th thoracic vertebrae, and these lesions invaded into the
spinal canal. These lesions were enhanced on contrast-enhanced
computed tomography (CT). Furthermore, multiple mass lesions were
found in the liver, and a mass lesion was found in the spleen
(Fig. 1). Magnetic resonance imaging
revealed that the lesions had invaded the 6th thoracic spinal
canal, highly compressing the spinal cord. The signal intensity of
these lesions was isointense to muscle tissue on T1-weighted images
(WIs) and heterogeneously high intensity to muscle on T2WIs
(Fig. 2). Blood examination results
were mostly normal, with the exceptions of slight elevations in
carcinoembryonic antigen (5.2 ng/ml) and vascular endothelial
growth factor (VEGF) levels (Table
I).
 | Table I.Analyses upon patient admission. |
Table I.
Analyses upon patient admission.
| Parameter | Value | Reference value |
|---|
| Alkaline phosphatase
(IU/l) | 248 | (109–350) |
| Carcinoembryonic
antigen (ng/ml) | 5.2 |
(≤5.0) |
| Carbohydrate antigen
19-9 (U/ml) | 10 | (≤37) |
| Prostate specific
antigen (ng/ml) | 1.66 | (≤4.0) |
| Protein induced by
vitamin K absence or antagonist-II (mAU/ml) | 11.8 | (<40.0) |
| Vascular endothelial
growth factor (pg/ml) | 110 | (≤38.3) |
| Tartrate resistant
acid phosphatase-5b (mU/dl) | 218 | (170–590) |
| Alubumin (g/dl) | 3.3 | (3.7–5.2) |
| Total protein
(g/dl) | 6.0 | (6.5–8.3) |
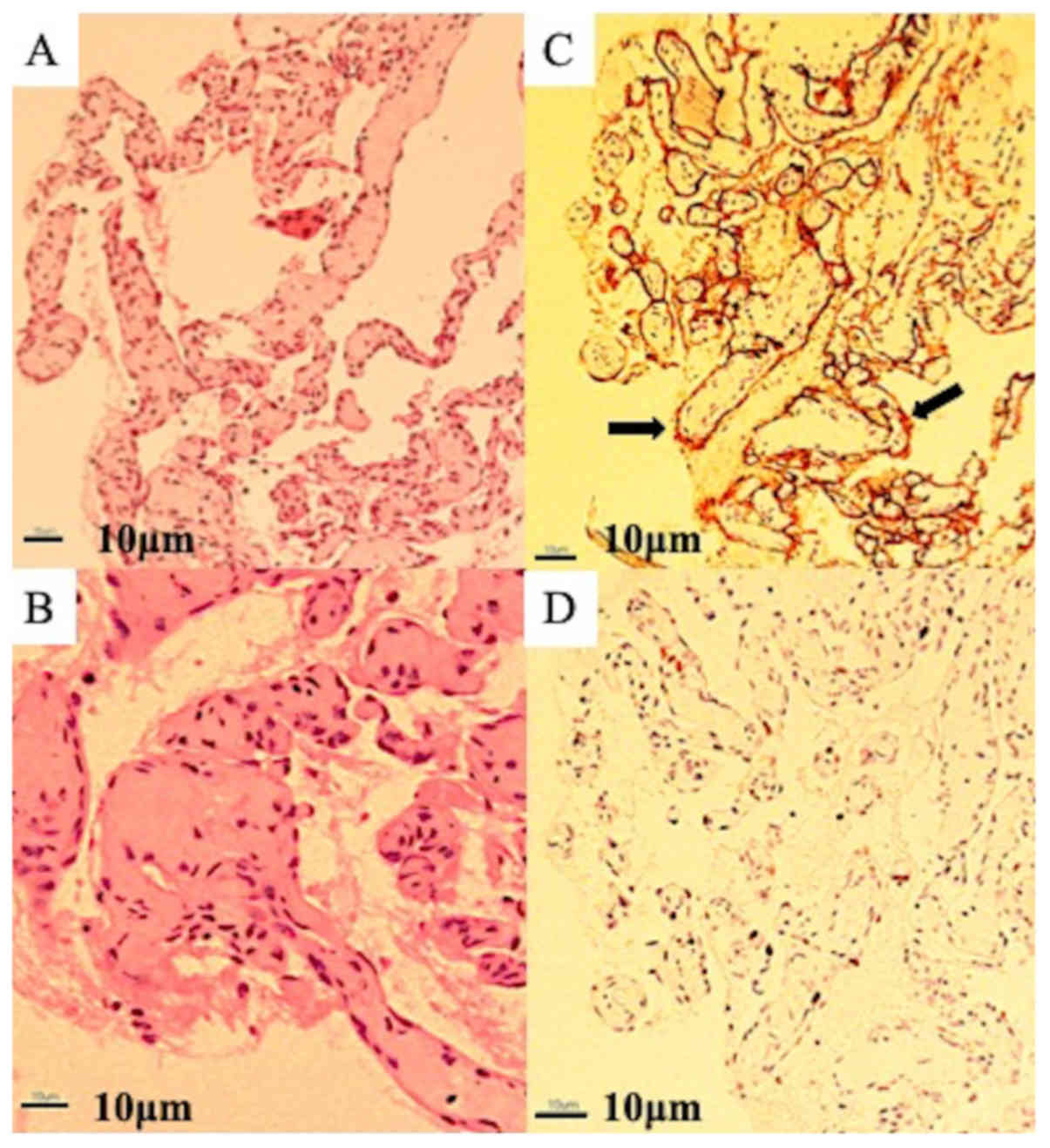
Based on clinical findings and imaging
characteristics, the lesions were diagnosed as cancer metastases. A
needle biopsy under CT guidance was performed from the left 6th
rib. Microscopic examination revealed a replacement of bone tissue
with vascular tissue, and a netlike proliferation of blood vessels
similar to capillary vessels consisting of monolayered vascular
endothelium. Hyaline fibrous interstitium was also observed. No
cellular atypia was present, and an osteoblastic response was also
absent. Immunohistochemical examination revealed an overexpression
of cluster of differentiation (CD) 34 on vascular endothelial cells
and was negative for desmin and D2-40 staining, and the MIB1
proliferation index ranged from 8 to 10% (Fig. 3). Radiologic imaging combined with
histopathology confirmed the diagnosis of GSD. At this time, the
patient was introduced to our department. Because 5 weeks had
already passed since paralysis had occurred, surgery for paralysis
was not performed. First, zoledronic acid (Zometa®, 4
mg) was intravenously administered and was continued once a month
for 5 months. Simultaneously, oral administration of activated
vitamin D was initiated. One month after the first administration
of zoledronic acid, the patient underwent transcutaneous
radiotherapy of the thoracic vertebra with a total dose of 20 Gy in
4-Gy fractions once a day for 5 days. Afterward, treatment with
propranolol was added at a dose of 0.6 mg/kg/day. Two months after
the first treatment, decubitus was noted around the sacral region,
and curettage and medical treatment for the lesion were continued.
One month later, a fever caused by pneumonia and/or decubitus was
observed, and the fever continued for approximately 2 months
despite antibiotic treatment. In addition, a chest CT scan revealed
increasing pleural effusion in the left hemithorax, and thus, a
puncture was performed. The fluid was serosanguinous, exudative,
and negative for malignancy (Table
II). At this time, a CT scan did not show clear progression of
osteolysis in the thoracic and rib lesions.
 | Table II.Biochemical and cytology analysis of
pleural fluid. |
Table II.
Biochemical and cytology analysis of
pleural fluid.
| Variable | Data |
|---|
| Appearance | Serous |
| Protein (g/dl) | 2.5 |
| LDH (U/l) | 79 |
| Glucose
(mg/dl) | 127 |
| Amilase (U/l) | 22 |
| Number of cells
(mm3) | 243 |
| Neutrophil (%) | 60 |
| Eosinophil (%) | 0 |
| Basophil (%) | 0 |
| Lymphocyte (%) | 32 |
| Methoterial cell
(%) | 5 |
| Histiocyte (%) | 3 |
| Cytology | Negative for
malignancy |
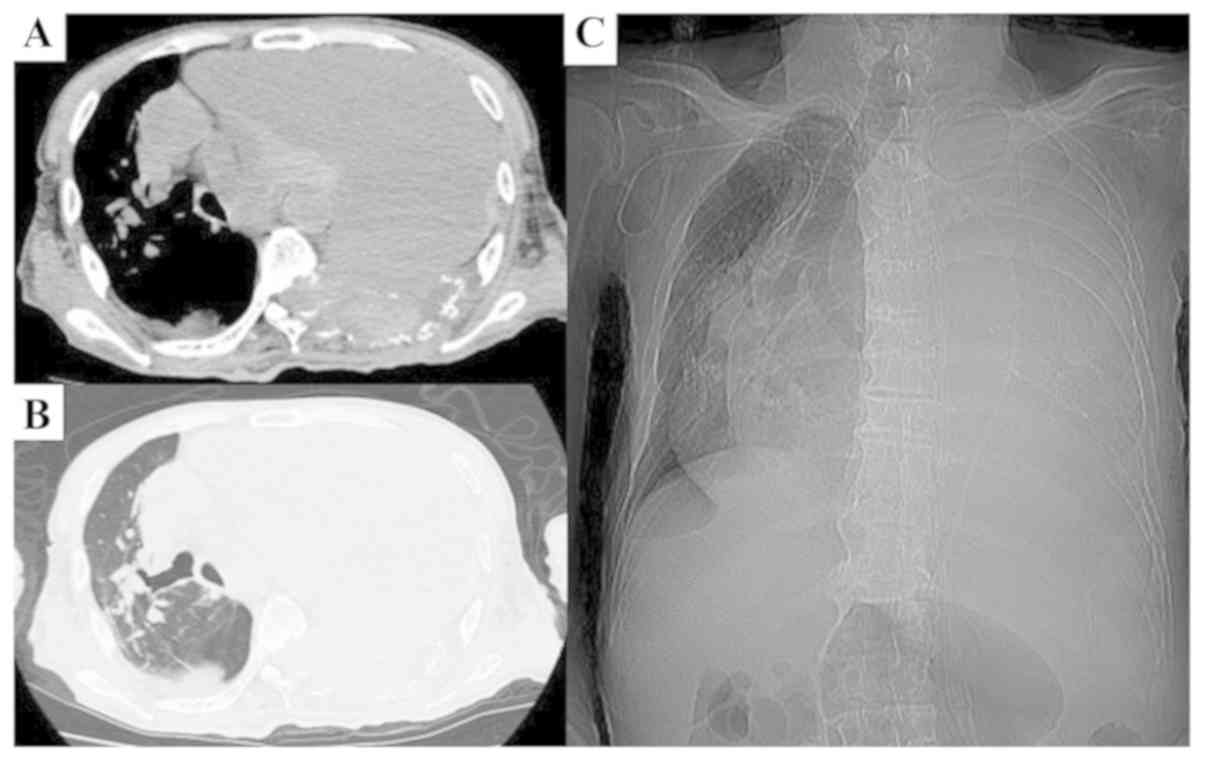
Approximately 5 months after the initial treatment,
the hemoglobin concentration suddenly dropped to 4.8 g/dl. A chest
CT scan revealed a remarkably increasing pleural effusion that
appeared to be hemorrhagic and was markedly compressing the left
lung, causing a mediastinal shift to the right thorax. The patient
received several blood transfusions and medication for anemia;
however, the condition did not improve. Furthermore, the
mediastinal shift worsened rapidly in the subsequent several days
(Fig. 4), and the patient's
breathing gradually became shallow. Unfortunately, the patient
succumbed to the disease 7 months after his initial visit.
Discussion
In GSD, massive and progressive osteolysis is caused
by the abnormal proliferation of endothelial capillaries of
vascular or lymphatic origin. The factors underlying the
pathogenesis of GSD remain unknown, although various changes in
molecular mechanisms have been reported. A high level of growth
factors, such as VEGF-A (14), basic
fibroblast growth factor (15), and
platelet-derived growth factor-BB (16), have been reported in GSD patients,
each of which may drive lymphatic endothelial cell proliferation
via the mammalian target of rapamycin pathway (15). An increased interleukin (IL)-8
concentration (17) and an
overexpression of CD105 (18) were
also reported in GSD patients. Overexpression of the growth factors
mentioned above may activate endothelial cells and induce
angiogenesis, vascular malformation, and lymphangiomatosis.
With respect to the mechanisms of osteolysis, an
increased IL-6 level in patients with GSD has been reported
(19). IL-6 stimulates osteoclasts,
leading to massive bone resorption. As such, IL-6 may play an
important role in the pathogenesis of GSD. In addition, homologous
monocytic cells producing the osteoclastogenic factors IL-1β and
transforming growth factor-β have been isolated from GSD patients
(17). Furthermore, although the
number of circulating osteoclast progenitor cells did not increase,
osteoclast precursors showed an increased sensitivity to IL-1β,
IL-6, and tumor necrosis factor-α, leading to increased
osteoclastic activity (20). Based
on these observations, the activation of both endothelial cells and
osteoclasts may be a characteristic of GSD.
The shoulder and pelvis are the commonest sites of
involvement. However, various locations, such as the humerus,
scapula, clavicle, ribs, sternum, pelvis, and femur, can be
affected by GSD (21). In spinal
GSD, 46% of cases reportedly occurred in the thoracic vertebrae
(22,23). Involvement of both the thoracic
vertebrae and ribs is extremely rare, with only three cases being
reported in the literature (23–25). One
of these reports was a 17-year-old man who had osteolysis in his
ribs and thoracic spine, with nonambulatory power in lower limbs
due to myelopathy. He received a single dose of 8 Gy and received 4
mg of zoledronic acid every month for 18 months. Thereafter,
posterior instrument fixation with anterior reconstruction was
performed. These treatments succeeded in halting the progression of
osteolysis and the patient showed complete neurological recovery
(23). Another report was for a
2-year-old girl, who had lesions in the femur in addition to the
thoracic spine and ribs. In addition, there were hemangiomas in the
liver and spleen, and hemangiomatous change on the skin surface of
the back. She was treated with IFNα and predonine for 14 months,
resulting in an improvement in the progression of osteolysis. 10
months later, there was no evidence of lesion exacerbation, and
hemangioma in the back disappeared, and the ribs which had
disappeared, reappeared (24). One
of the other reports did not describe the clinical course of the
patient, and was a report only on imaging findings (25). In current report, the patient's
paralysis was complete and the age was relatively high. These are
differences from previous reports, therefore age and degree of
paralysis might influence on the prognosis.
At present, there is no consensus on treating GSD,
and various treatment methods have been attempted, including
surgery, radiotherapy, and medications, alone or in combination.
Surgery for metastatic spinal cord compression should be performed
sooner rather than later. Furthermore, earlier surgical treatment
(within 48 h) in patients with metastatic spinal cord compression
resulted in significantly better neurological outcomes (26). In GSD, the timing of surgery is very
difficult because osteolysis continually progresses in its active
phase, even after the surgery has been performed. In the current
case, surgery was not performed because 5 weeks had already passed
since complete paralysis occurred at the time of first visit to our
department, and the lesion was considered to be in the active phase
based on the progress of paralysis. Moreover, there are no Food and
Drug Administration-approved medical therapies for treating GSD.
Several drugs have nevertheless been tried, including
bisphosphonates (10); interferon
alpha-2b (9); the anti-VEGF-A
antibody bevacizumab (27); low
molecular weight heparin, steroids, vitamin D, and calcitonin
(11,28); and sirolimus (8). Bisphosphonates are used owing to their
anti-osteoclastic properties. Furthermore, third-generation
bisphosphonates have anti-VEGF effects (29); thus, they have the potential to exert
therapeutic effects by inhibiting osteolysis and angiogenesis,
vascular malformation, and lymphangiomatosis. The use of
propranolol for GSD has been reported previously (30,31). The
mechanism of action is considered to be the downregulation of VEGF,
which leads to the inhibition of vascular proliferation. It may
also inhibit proliferation and migration of lymphatic endothelial
cells. In our case, treatment with propranolol was initiated at 0.6
mg/kg/day, with a plan to gradually increase the dose. However,
large decubitus ulcers appeared from the patient's back to his
sacrum. Thus, the propranolol dose was not increased because of the
possibility that it might adversely influence the healing of the
ulcers by inhibiting angiogenesis, which is a known property of
propranolol. In fact, serum VEGF levels were not significantly
altered before (110 pg/ml) and after (118 pg/ml) propranolol
administration. Notably, it was reported that a patient treated
with propranolol (2 mg/kg/day) responded well to this therapy, with
resolution of symptoms and reduction in VEGF-A levels after 3
months of treatment to near-control levels (32). The dose of this medication should
have been increased if the circumstances allowed it.
Radiotherapy is another treatment modality that has
been attempted for GSD. The exact mechanism of action is not known;
however, it is postulated that radiotherapy may arrest endothelial
cell proliferation and limit the progression of disease (33,34). In
a previous case report, although a total dose ranging from 36 to 45
Gy was recommended (33,34), the patient received a transcutaneous
radiotherapy dose of only 20 Gy for thoracic lesions because of
concerns around expanding the range of the spinal cord injury and
the side effects owing to high dose irradiation. As a result,
expansion of thoracic lesions was not recognized on diagnostic
imaging; however, bleeding from the lesions eventually became
uncontrolled. Based on these findings, it was necessary to
reconsider the total dose of irradiation or additional radiotherapy
for rib lesions.
In general, the clinical course of GSD varies
widely, ranging from spontaneous remission to fatal disease usually
in the context of a chylothorax (35,36). In
a literature review of 175 cases of GSD, the mean overall mortality
rate was 13.3% (37). The mortality
rate of spinal lesion was 20–53% (22,37,38), and
mortality also occurred because of complications of chylothorax.
Although chylothorax was not apparent in our case, hemothorax by
intralesional hemorrhage did occur, causing a mediastinum shift
that finally resulted in the rapid impairment of respiratory
function. So far, there have not been any reported cases of
mediastinum shift owing to intralesional hemorrhage in GSD, and
this is the first report to describe it. For future reference, it
should be noted that such processes may occur in the thoracic spine
and/or thorax owing to GSD lesions.
To the best of our knowledge, this is the first
reported case of GSD in the rib and thoracic spine with spinal
injury to be treated with radiotherapy, propranolol, vitamin D, and
zoledronic acid. Furthermore, no previous reports have described
rapid-onset mediastinum shift with respiratory impairment owing to
intralesional hemorrhage in GSD. In such rare diseases, conducting
large randomized double-blind clinical trials would be difficult;
thus, it is essential to record and share experiences obtained with
individual treatment methods. Theoretically, effective treatment by
clarifying the pathogenesis should be performed, and the results
should be shared. This case will contribute to a deeper
understanding of the very rare clinical entity of GSD.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
KK made the treatment plan, designed the study and
wrote the manuscript. KIn and MI treated the patient and have
contributed to data collection and interpretation. KIt performed
the histological examination and interpreted the results. All
authors approved the final version of this manuscript and agree to
be accountable for all aspects of the work.
Ethics approval and consent to
participate
This case report was approved by the Ethics
Committee of Meiji University of Integrative Medicine.
Patient consent for publication
Written and verbal informed consent for publication
was obtained from the patient and patient's family.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
GSD
|
Gorham-Stout disease
|
|
CT
|
computed tomography
|
|
WIs
|
weighted images
|
|
VEGF
|
vascular endothelial growth factor
|
|
CD
|
cluster of differentiation
|
|
IL
|
interleukin
|
|
CECT
|
contrast-enhanced computed
tomography.
|
References
|
1
|
Torg JS, DiGeorge AM, Kirkpatrick JA Jr
and Trujillo MM: Hereditary multicentric osteolysis with recessive
transmission: A new syndrome. J Pediatr. 75:243–252. 1969.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Macpherson RI, Walker RD and Kowall MH:
Essential osteolysis with nephropathy. J Can Assoc Radiol.
24:98–103. 1973.PubMed/NCBI
|
|
3
|
Dellinger MT, Garg N and Olsen BR:
Viewpoints on vessels and vanishing bones in Gorham-Stout disease.
Bone. 63:47–52. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jackson JSB: A singular case of absorption
of bone (a boneless arm). Boston Med Surg J. 18:368–369. 1838.
|
|
5
|
Tolis K, Triantafyllopoulos IK, Tournis S
and Papaioannou NA: Gorham-Stout disease of the pelvis: Seven years
follow up with complete radiological evaluation. J Musculoskelet
Neuronal Interact. 16:79–82. 2016.PubMed/NCBI
|
|
6
|
Vinée P, Tanyü MO, Hauenstein KH, Sigmund
G, Stöver B and Adler CP: CT and MRI of Gorham syndrome. J Comput
Assist Tomogr. 18:985–989. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Szabo C and Habre W: Gorham syndrome:
Anaesthetic management. Anaesthesia. 55:157–159. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
García V, Alonso-Claudio G,
Gómez-Hernández MT and Chamorro AJ: Sirolimus on Gorham-Stout
disease. Case report. Colomb Med (Cali). 47:213–216.
2016.PubMed/NCBI
|
|
9
|
Hagberg H, Lamberg K and Aström G:
Alpha-2b interferon and oral clodronate for Gorham's disease.
Lancet. 350:1822–1823. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Avelar RL, Martins VB, Antunes AA, de
Oliveira Neto PJ and Andrade ES: Use of zoledronic acid in the
treatment of Gorham's disease. Int J Pediatr Otorhinolaryngol.
74:319–322. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yerganyan VV, Body JJ, De Saint Aubain N
and Gebhart M: Gorham-Stout disease of the proximal fibula treated
with radiotherapy and zoledronic acid. J Bone Oncol. 4:42–46. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gorham LW and Stout AP: Massive osteolysis
(acute spontaneous absorption of bone, phantom bone, disappearing
bone); Its relation to hemangiomatosis. J Bone Joint Surg Am 37-A.
985–1004. 1955. View Article : Google Scholar
|
|
13
|
Frankel HL, Hancock DO, Hyslop G, Melzak
J, Michaelis LS, Ungar GH, Vernon JD and Walsh JJ: The value of
postural reduction in the initial management of closed injuries of
the spine with paraplegia and tetraplegia. I. Paraplegia.
7:179–192. 1969.PubMed/NCBI
|
|
14
|
Brunner U, Rückl K, Konrads C, Rudert M
and Plumhoff P: Gorham-Stout syndrome of the shoulder. SICOT J.
2:252016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hagendoorn J, Yock TI, Borel Rinkes IH,
Padera TP and Ebb DH: Novel molecular pathways in Gorham disease:
Implications for treatment. Pediatr Blood Cancer. 61:401–406. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hagendoorn J, Padera TP, Yock TI, Nielsen
GP, di Tomaso E, Duda DG, Delaney TF, Gaissert HA, Pearce J,
Rosenberg AE, et al: Platelet-derived growth factor receptor-beta
in Gorham's disease. Nat Clin Pract Oncol. 3:693–697. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Colucci S, Taraboletti G, Primo L, Viale
A, Roca C, Valdembri D, Geuna M, Pagano M, Grano M, Pogrel AM, et
al: Gorham-Stout syndrome: A monocyte-mediated cytokine propelled
disease. J Bone Miner Res. 21:207–218. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Franchi A, Bertoni F, Bacchini P,
Mourmouras V and Miracco C: CD105/endoglin expression in Gorham
disease of bone. J Clin Pathol. 62:163–167. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Devlin RD, Bone HG III and Roodman GD:
Interleukin-6: A potential mediator of the massive osteolysis in
patients with Gorham-Stout disease. J Clin Endocrinol Metab.
81:1893–1897. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Rossler J, Saueressig U, Kayser G, von
Winterfeld M and Klement GL: Personalized therapy for generalized
lymphatic anomaly/Gorham-Stout disease with a combination of
sunitinib and taxol. J Pediatr Hematol Oncol. 37:e481–e485. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Patel DV: Gorham's disease or massive
osteolysis. Clin Med Res. 3:65–74. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Tateda S, Aizawa T, Hashimoto K, Kanno H,
Ohtsu S, Itoi E and Ozawa H: Successful management of Gorham-Stout
disease in the cervical spine by combined conservative and surgical
treatments: A case report. Tohoku J Exp Med. 241:249–254. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Srivastava SK, Aggarwal RA, Nemade PS and
Bhoale SK: Vanishing bone disease of chest wall and spine with
kyphoscoliosis and neurological deficit: A case report and review
of literature. Indian J Orthop. 51:107–114. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Takahashi A, Ogawa C, Kanazawa T, Watanabe
H, Suzuki M, Suzuki N, Tsuchida Y, Morikawa A and Kuwano H:
Remission induced by interferon alfa in a patient with massive
osteolysis and extension of lymph-hemangiomatosis: A severe case of
Gorham-Stout syndrome. J Pediatr Surg. 40:E47–E50. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ceroni D, De Coulon G, Regusci M and
Kaelin A: Gorham-Stout disease of costo-vertebral localization:
Radiographic, scintigraphic, computed tomography, and magnetic
resonance imaging findings. Acta Radiol. 45:464–468. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Quraishi NA, Rajagopal TS, Manoharan SR,
Elsayed S, Edwards KL and Boszczyk BM: Effect of timing of surgery
on neurological outcome and survival in metastatic spinal cord
compression. Eur Spine J. 22:1383–1388. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ozeki M, Fukao T and Kondo N: Propranolol
for intractable diffuse lymphangiomatosis. N Engl J Med.
364:1380–1382. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Holroyd I, Dillon M and Roberts GJ:
Gorham's disease: A case (including dental presentation) of
vanishing bone disease. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod. 89:125–129. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Koto K, Horie N, Kimura S, Murata H,
Sakabe T, Matsui T, Watanabe M, Adachi S, Maekawa T, Fushiki S and
Kubo T: Clinically relevant dose of zoledronic acid inhibits
spontaneous lung metastasis in a murine osteosarcoma model. Cancer
Lett. 274:271–278. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Nir V, Guralnik L, Livnat G, Bar-Yoseph R,
Hakim F, Ilivitzki A and Bentur L: Propranolol as a treatment
option in Gorham-Stout syndrome: A case report. Pediatr Pulmonol.
49:417–419. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Morimoto N, Ogiwara H, Miyazaki O,
Kitamuara M, Nishina S, Nakazawa A, Maekawa T and Morota N:
Gorham-Stout syndrome affecting the temporal bone with
cerebrospinal fluid leakage. Int J Pediatr Otorhinolaryngol.
77:1596–1600. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Baud J, Lomri A, Graber D and Bikfalvi A:
The therapeutic response in Gorham's syndrome to the beta-blocking
agent propranolol is correlated to VEGF-A, but not to VEGF-C or
FLT1 expression. BMC Res Notes. 8:3332015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Heyd R, Micke O, Surholt C, Berger B,
Martini C, Füller J, Schimpke T and Seegenschmiedt MH; German
Cooperative Group on Radiotherapy for Benign Diseases (GCG-BD), :
Radiation therapy for Gorham-Stout syndrome: Results of a national
patterns-of-care study and literature review. Int J Radiat Oncol
Biol Phys. 81:e179–e185. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Dunbar SF, Rosenberg A, Mankin H,
Rosenthal D and Suit HD: Gorham's massive osteolysis: The role of
radiation therapy and a review of the literature. Int J Radiat
Oncol Biol Phys. 26:491–497. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Bode-Lesniewska B, von Hochstetter A,
Exner GU and Hodler J: Gorham-Stout disease of the shoulder girdle
and cervico-thoracic spine: Fatal course in a 65-year-old woman.
Skeletal Radiol. 31:724–729. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Rudert M, Gross W and Kirschner P:
Gorham-Stout massive ostelysis. A case report. Unfallchirurg.
98:102–104. 1995.(In German). PubMed/NCBI
|
|
37
|
Flörchinger A, Böttger E, Claass-Böttger
F, Georgi M and Harms J: Gorham-Stout syndrome of the spine. Case
report and review of the literature. Rofo. 168:68–76. 1998.(In
German). View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Lee S, Finn L, Sze RW, Perkins JA and Sie
KC: Gorham Stout syndrome (disappearing bone disease): Two
additional case reports and a review of the literature. Arch
Otolaryngol Head Neck Surg. 129:1340–1343. 2003. View Article : Google Scholar : PubMed/NCBI
|