Introduction
First described by Peacock in 1850, a bronchobiliary
fistula (BBF) is a rare complication after hepatectomy, which
consists of an abnormal intercommunication between the biliary
tract and bronchial tree (1). This
may occur due to an obstruction of the biliary tract, trauma or
hepatic abscess. Especially in endemic regions, hydatid or amebic
disease of the liver are common causes of BB (2,3). The
classic clinical presentation includes cough producing yellow
sputum, known as bilioptysis, which represents a pathognomonic sign
of BBF (4). Of note, BBF is
associated with high morbidity and mortality rates. The management
of this rare entity is challenging with limited current evidence to
date on how to treat this condition (5). Herein, we present a case of BBF
following a central hepatectomy and the successive steps of the
management. In addition, we sought to conduct a review the
literature to summarize all the available evidence regarding
post-hepatectomy BBFs.
Case presentation
A 64-year-old Caucasian male was diagnosed with
adenocarcinoma of the rectum in 2012 for which he underwent low
anterior resection with adjuvant chemotherapy (FOLFOX). The
histological report of the specimen revealed a moderate to poorly
differentiated adenocarcinoma of the rectum with T3c invasion of
the bowel wall and metastases to mesorectal lymph nodes (stage
IIC). The patient was referred to the oncology department for
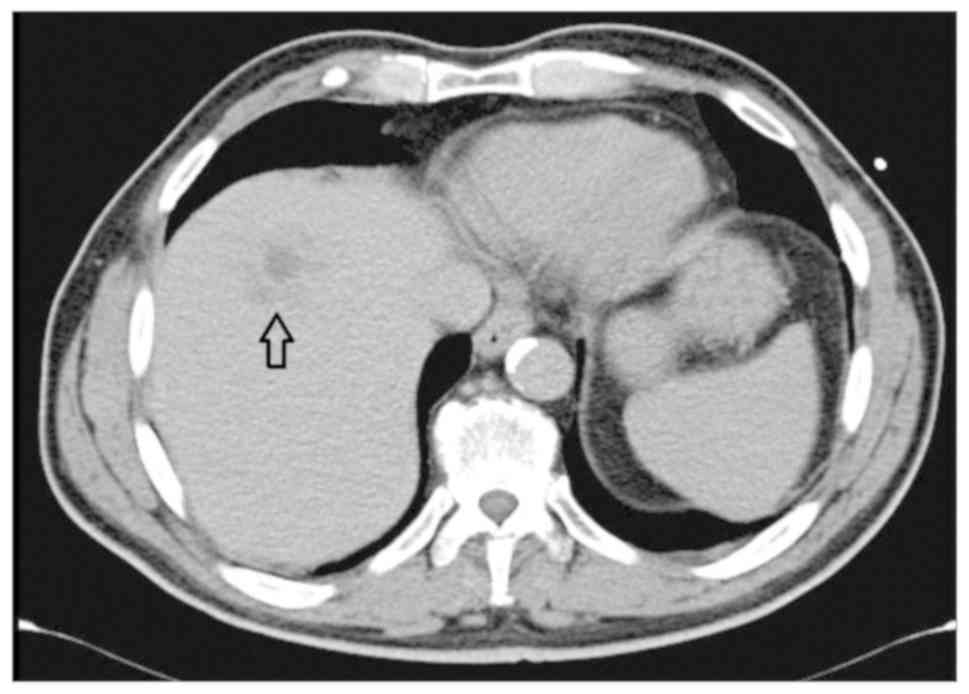
further treatment. During a routine follow-up at three years, the
computer tomography (CT) scan demonstrated an asymptomatic solitary
hypoechoic lesion in segment VIII measuring approximately 5 cm in
diameter (Fig. 1). Given the absence
of other comorbidities, the multidisciplinary team decided that
liver resection was appropriate.
During exploratory laparotomy, intraoperative
findings with hepatic U/S confirmed a solitary lesion in segment
VIII of the liver. A central hepatectomy was performed without any
intraoperative complications and the immediate postoperative
clinical course was uneventful. Histological report confirmed that
the lesion was of metastatic nature, from poorly differentiated
adenocarcinoma of colon, and the patient was referred to the
oncology department.
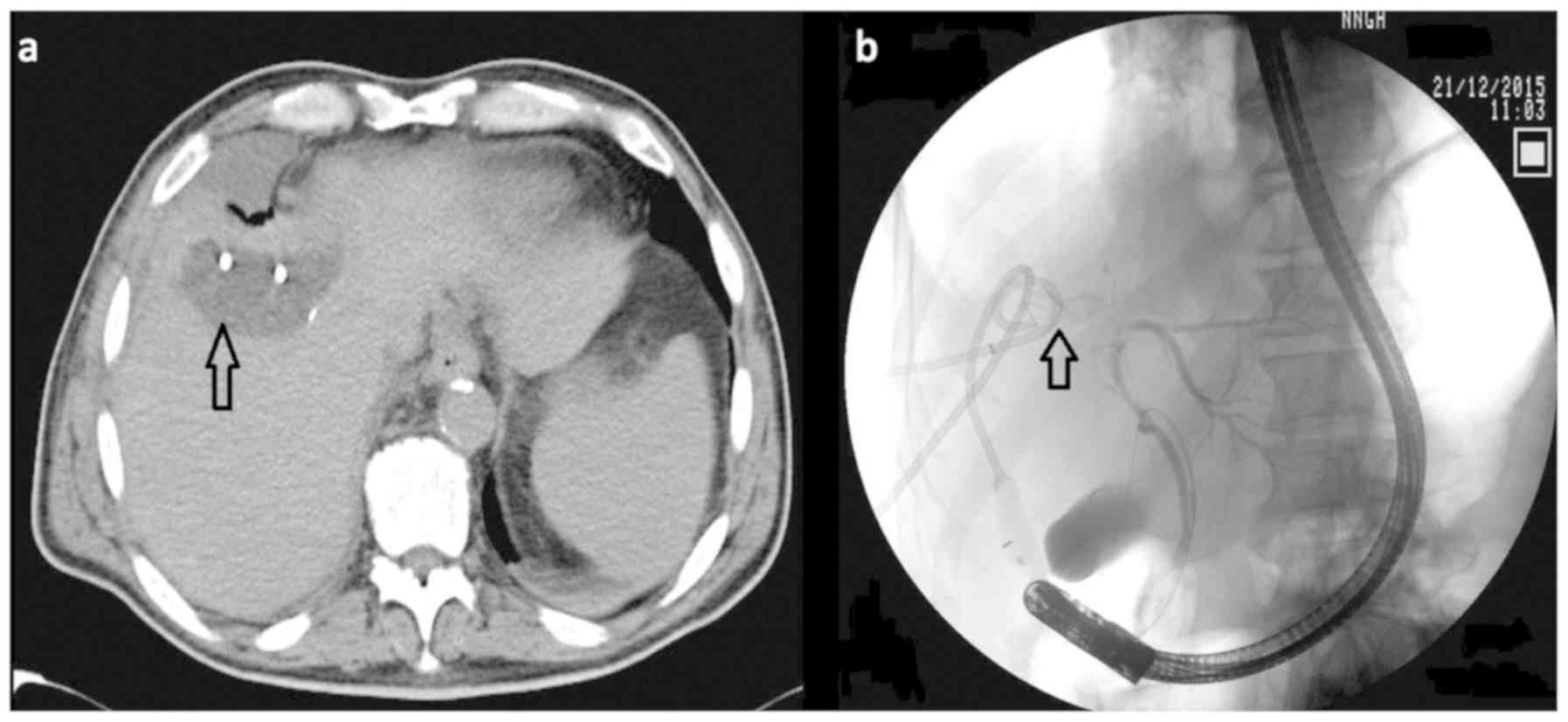
Three months later, the patient was admitted under
the care of the medical oncology team with a history of fatigue for
two days, weight loss and fever up to 39°. A CT scan demonstrated a
postoperative intrahepatic collection (Fig. 2A) and a 12F drain was inserted by a
radiologist with CT guidance. An endoscopic retrograde
cholangiopancreatography (ERCP) was performed which demonstrated a
bile leak, and a 9 cm 10 F stent was placed (Fig. 2B). The patient was discharged 20 days
later with the drain in situ and was examined regularly in our
outpatient clinic.
However, 14 months postoperatively, the patient
presented to the oncology department complaining of new onset fever
and expectoration. A chest x- ray was performed demonstrating
atelectasis of the lower right lobe and was treated as suspected
pneumonia. Given the patient previous history, an inflammatory
tumor was included in the differential diagnosis. Although
afebrile, the patient reported episodes of a productive cough with
dark-yellow sputum, raising concerns for bronchobiliary fistula.
The patient underwent a CT scan which confirmed the clinical
suspicion and he was subsequently referred to our department for
further treatment. Since the patient had a biliary stent in situ,
the surgical team decided that a further operation was required.
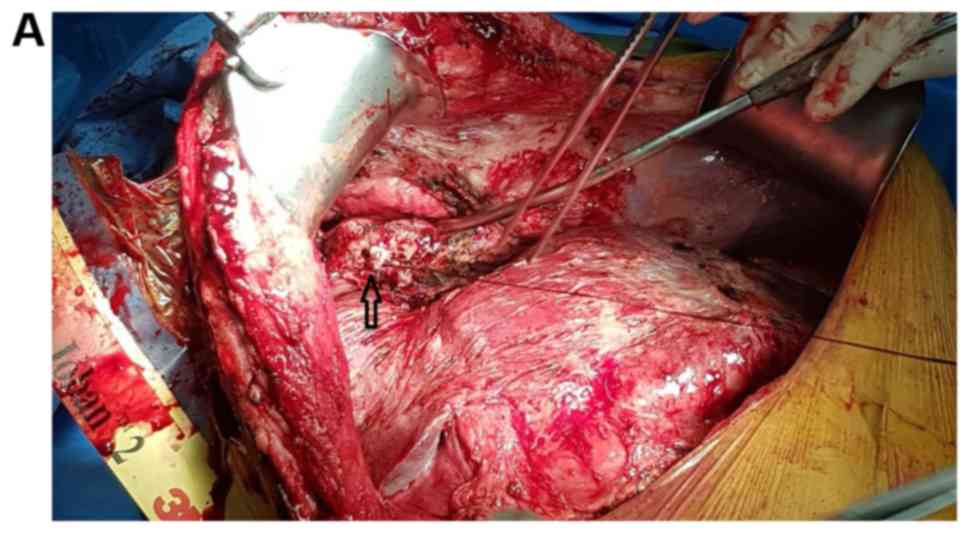
Using a transabdominal approach, a communication between the
initial intrahepatic collection and one inferior lobular bronchus
was demonstrated. Transhiatal removal of fistula was performed with
closure of the defect through the abdomen (Fig. 3). There was no bile leak through the
remaining liver parenchyma.
The postoperative course was uneventful with no
further bilioptysis or other pulmonary symptoms. At radiological
follow up one month postoperatively, a CT showed a postoperative
biloma for which the patient underwent CT guided drainage with a
12F catheter. A further ERCP revealed leakage and communication of
the bile duct with the biloma which was drained and a stent was
inserted. The patient was discharged 2 months after surgery and was
examined regularly in the outpatient clinic. He was readmitted on a
schedule to remove the plastic stent by ERCP. Currently, there are
no signs of further bile leakage, BBF or pulmonary symptoms.
Discussion
BBP is an uncommon condition whose etiology can
differ by geographical region; in developing countries echinococcal
and amebic disease are the most common causes, whereas in developed
countries trauma and biliary obstruction predominate (6). According to a recent systematic review,
tumor is the most frequent cause (32.3%) of BBF formation, followed
by bile duct obstruction (30.8%) (7). Other causes have also been identified,
such as chronic pancreatitis, trauma and congenital malformation.
The pathogenesis of fistula formation has not been completely
understood yet, although increased pressure within the biliary tree
and local inflammation appeared to be the two major factors that
contribute to the development of BBF. In our case, intrahepatic
abscess triggered the formation of adhesions between the diaphragm
and the lung and was thought to be the cause of the BBF formation
(4,8–10).
The clinical presentation is variable, and may
include fever, irritating cough, jaundice, and abdominal pain. The
pathognomonic feature is a productive cough of bile stained sputum
(7,11). Chest pain or episodes of dyspnea
occur only in a minority of patients, while nausea, vomiting,
portal hypertension and liver dysfunction are rarely found. In
terms of diagnosis, CT imaging is usually the predominant modality
or biliary scintigraphy with hepatic iminoacetic acid (HIDA) which
demonstrates initial tracer activity in the liver which migrates
into the chest cavity (12). BBF can
also be diagnosed by interventional techniques, such as ERCP,
percutaneous transhepatic cholangiography, bronchoscopy or
fistulography (4,13,14).
Currently, there are no guidelines on how to treat
this rare complication with both conservative and surgical
approaches considered acceptable to date. Some authors suggest that
BBF associated with benign causes should be treated conservatively;
endoscopic retrograded biliary drainage (ERBD), endoscopic
nasobiliary drainage (ENBD), percutaneous transhepatic
cholangiography and biliary drainage (PTCD), and abscess drainage
(15–17). Adjunct use of octreotide might have a
role in some cases due to reports of successful resolution or
reduction of symptoms with its use (18). On the other hand, surgical management
should be considered in case BBF has developed in a background of
tumor, trauma or obstruction and conservative therapy has
previously failed (7). Operative
exploration and repair of the initial injury is usually performed,
whereas resection of the involved pulmonary area and removal of the
fistula is advised in the form of thoracobiliary fistula
decortication (18).
Table I summarizes a
brief review of the literature on bronchobiliary fistulas after
liver surgery for both benign and malignant diseases (9,11,19–30).
 | Table I.Review of reported cases with
bronchobiliary fistula after hepatectomy. |
Table I.
Review of reported cases with
bronchobiliary fistula after hepatectomy.
| Author, Year | Age/sex | Type of disease | Primary disease | Treatment | Bilioptysis | Fever | Jaundice | Approach | Outcome | (Refs.) |
|---|
| Lucero et al,
2005 | 63/F | Benign | Hydatid cyst | Right
hepatectomy | Yes | N/A | N/A | Surgery | Cure | (29) |
| Memis et al,
2000 | 40/M | Benign | Hepatic Alveolar
disease | Partial
hepatectomy | Yes | N/A | Yes | Histoacryl injection
through microcatheter and ERBD | Cure | (26) |
| Senturk et al,
1998 | 26/M | Benign | Hydatid cyst | Partial right
lobectomy | Yes | Yes | Yes | ERBD | Cure | (21) |
| Schwartz et
al, 1988 | 18/M | Unknown | Unknown | Right heptectomy | Yes | N/A | N/A | PTCD and balloon
dilation cholangioplasty | Cure | (24) |
| Chua et al,
2000 | 61/M | Benign and
Malignant | Gangrenous
Cholecystitis Carcinosarcoma | Right
hepatectomy | Yes | Yes | N/A | Surgery | Cure | (9) |
| Ong et al,
2004 | 71/F | Malignant | Metastatic colon
Ca | Right
hepatectomy | Yes | Yes | No | Octreotide
injection | Cure | (30) |
| Kaido et al,
2006 | 76/M | Malignant | Hepatocellular
Ca | Right
hepatectomy | Yes | Yes | Yes | surgery | Failure | (28) |
| Jung et al,
2003 | 65/M | Malignant | Metastatic colon
Ca | Right
hepatectomy | Yes | Yes | N/A | Multiple ERBD then
surgery | Cure | (27) |
| Oettl et al,
1999 | 56/M | Malignant | Metastatic colon
Ca | Right
hepatectomy | Yes | Yes | Yes | ERBD | Cure | (19) |
| Rose et al,
1998 | 61/M | Malignant | Metastatic colon
Ca | Wedge liver resection
right lobe | Yes | N/A | Yes | ERBD | No BBF died 5
months later | (20) |
| Velchik et
al, 1991 | 38/F | Malignant | Mucinous
adenocarcinoma | Right
hepatectomy | Yes | N/A | N/A | PTCD | Cure | (23) |
| George et
al, 1988 | 58/M | Malignant | Metastatic colon
Ca | Hepatic
resection | Yes | Yes | Yes | Surgery | Failure | (22) |
| Hai et al,
2016 | 70/M | Malignant | Hepatocellular
Ca | Partial resection
segment 8 | Yes | Yes | N/A | ERBD then
surgery | Cure | (11) |
| Kuo et al,
2014 | 68/M | Malignant | Hepatocellular
Ca | Central
lobectomy | Yes | Yes | N/A | Surgery | Cure | (25) |
| Current case,
2019 | 64/M | Malignant | Metastatic colon
Ca | Central
hepatectomy | Yes | Yes | Yes | ERBD then
surgery | Cure | Present study |
Due to low incidence of BBF, there is no clear
consensus on the treatment of this uncommon complication to date.
Multidisciplinary management of such patients should be considered
taking into consideration the underlying pathology leading to this
rare complication. Conservative treatment should be considered
first, while surgical resection of the BBF remains an option when
other therapies have failed. Surgeons should have low suspicion of
diagnosing and managing this complication after biliary tract
operations.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during the present
study are included in this published article.
Authors' contributions
VL, DM and APe were involved in the study conception
and design. VL and APa contributed to the acquisition of data. VL,
DM, DIT and GSK were involved in data analysis and interpretation.
DM, DIT and GSK drafted the manuscript. APa and APe critically
revised the manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Nicosia Hospital.
Patient consent for publication
Informed consent was obtained.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Peacock TB: Case in which hydatids were
expectorated, and one of suppuration in a hydatid cyst of the liver
communicating with the lungs. Edinb Med Surg J. 74:33–46.
1850.PubMed/NCBI
|
|
2
|
Mantonakis E, Papalampros A, Moris D,
Dimitrokallis N, Sakarellos P, Griniatsos J and Felekouras E:
Radiofrequency energy in hepatic bed during partial cystectomy for
hydatid liver disease: Standing out from the usual conservative
surgical management. Gastroenterol Res Pract. 2016:10786532016.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Moris DN, Mantonakis EI, Papalampros AE,
Petrou AS and Felekouras ES: Pushing the frontiers of operative
treatment of hydatid liver disease a step forward. Surgery.
160:8182016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gugenheim J, Ciardullo M, Traynor O and
Bismuth H: Bronchobiliary fistulas in adults. Ann Surg. 207:90–94.
1988. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Janczak D, Zielińska D, Pawelczyk J,
Dorobisz T, Garcarek J, Patrzałek D and Chabowski M: Embolizations
of the hepatic tumors-two-year single center experience.
Vojnosanitetski Pregled. 2017.
|
|
6
|
Jamal Y, Tombazzi C, Waters B and Ismail
MK: Bronchobiliary fistula in a cirrhotic patient: A case report
and review of the literature. Am J Med Sci. 335:315–319. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Liao GQ, Wang H, Zhu GY, Zhu KB, Lv FX and
Tai S: Management of acquired bronchobiliary fistula: A systematic
literature review of 68 cases published in 30 years. World J
Gastroenterol. 17:3842–3849. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Akazawa S, Omagari K, Amenomori M,
Nishiyama H, Mizuta Y and Kohno S: Bronchobiliary fistula
associated with intrahepatic biloma after transcatheter arterial
chemoembolization for hepatocellular carcinoma. J Hepatol.
40:1045–1046. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chua HK, Allen MS, Deschamps C, Miller DL
and Pairolero PC: Bronchobiliary fistula: Principles of management.
Ann Thorac Surg. 70:1392–1394. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Baudet JS, Medina A, Moreno A, Navazo L,
Avilés J and Soriano A: Bronchobiliary fistula secondary to
ruptured hepatocellular carcinoma into the bile duct. J Hepatol.
41:1066–1067. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hai S, Iimuro Y, Hirano T, Suzumura K,
Yada A and Fujimoto J: Bronchobiliary fistula caused after
hepatectomy for hepatocellular carcinoma: A case report. Surg Case
Rep. 2:1472016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Andalkar L, Trow TK, Motroni B and Katz
DS: Bronchobiliary fistula as a complication of liver metastases:
Diagnosis by HIDA scan. Clin Nucl Med. 29:289–291. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hibi T, Sakamoto Y, Asamura H, Tochigi N,
Ojima H, Shimada K, Sano T and Kosuge T: Successful resection of
hepatocellular carcinoma with bronchobiliary fistula caused by
repeated transcatheter arterial embolizations: Report of a case.
Surg Today. 37:154–158. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Cropper LD Jr, Gold RE and Roberts LK:
Bronchobiliary fistula: Management with percutaneous catheter
drainage of a subphrenic abscess. J Trauma. 22:68–70. 1982.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yilmaz U, Sahin B, Hilmioglu F, Tezel A,
Boyacioglu S and Cumhur T: Endoscopic treatment of bronchobiliary
fistula: Report on 11 cases. Hepatogastroenterology. 43:293–300.
1996.PubMed/NCBI
|
|
16
|
Singh B, Moodley J, Sheik-Gafoor MH,
Dhooma N and Reddi A: Conservative management of thoracobiliary
fistula. Ann Thorac Surg. 73:1088–1091. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ertuğrul I, Köklü S, Köksal AS, Coban S,
Başar O, Ibiş M and Sahin B: Treatment of bronchobiliary fistula
due to an infected hydatid cyst by a nonsurgical approach. Dig Dis
Sci. 49:1595–1597. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Crnjac A, Pivec V and Ivanecz A:
Thoracobiliary fistulas: Literature review and a case report of
fistula closure with omentum majus. Radiol Oncol. 47:77–85. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Oettl C, Schima W, Metz-Schimmerl S,
Függer R, Mayrhofer T and Herold CJ: Bronchobiliary fistula after
hemihepatectomy: Cholangiopancreaticography, computed tomography
and magnetic resonance cholangiography findings. Eur J Radiol.
32:211–215. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Rose DM, Rose AT, Chapman WC, Wright JK,
Lopez RR and Pinson CW: Management of bronchobiliary fistula as a
late complication of hepatic resection. Am Surg. 64:873–876.
1998.PubMed/NCBI
|
|
21
|
Senturk H, Mert A, Ersavasti G, Tabak F,
Akdogan M and Ulualp K: Bronchobiliary fistula due to alveolar
hydatid disease: Report of three cases. Am J Gastroenterol.
93:2248–2253. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
George TK and Carignan JR: Bronchobiliary
fistula after hepatic resection for metastatic colon cancer. J Surg
Oncol. 25:198–200. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Velchik MG, Roth GM, Wegener W and Alavi
A: Bronchobiliary fistula detected by cholescintigraphy. J Nucl
Med. 32:136–138. 1991.PubMed/NCBI
|
|
24
|
Schwartz ML, Coyle MJ, Aldrete JS and
Keller FS: Bronchobiliary fistula: Complete percutaneous treatment
with biliary drainage and stricture dilation. Radiology.
168:751–752. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kuo YS, Lee SC, Chang H, Hsieh CB and
Huang TW: Thoracoscopic surgery for bronchobiliary fistula: A case
report. J Cardiothorac Surg. 9:1392014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Memis A, Oran I and Parildar M: Use of
histoacryl and a covered nitinol stent to treat a bronchobiliary
fistula. J Vasc Interv Radiol. 11:1337–1340. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Jung SI, Goo JM, Han JK, Jang JY, Lee KU,
Lee KH and Im JG: Recurrent bronchobiliary fistula: Unsuccessful
management with repeated insertion of metallic biliary stent. J
Vasc Interv Radiol. 14:1577–1579. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kaido T, Kano M, Suzaki S, Yanagibashi K
and Shiota M: Bronchobiliary fistula after hepatectomy for
hepatocellular carcinoma. Dig Dis Sci. 51:1117–1121. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lucero Pizones JA, Iglesias López A,
Alcázar Iribarren Marín M and Márquez Galán JL: Bronchobiliary
fistula secondary to biliary stricture after hepatectomy. Rev Esp
Enferm Dig. 97:135–136. 2005.(In English, Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Ong M, Moozar K and Cohen LB: Octreotide
in bronchobiliary fistula management. Ann Thorac Surg.
78:1512–1513. 2004. View Article : Google Scholar : PubMed/NCBI
|