Introduction
Gastrointestinal stromal tumours (GISTs) comprise
0.1–3% of all gastrointestinal malignancies and represent the
majority of the gastrointestinal mesenchymal neoplasms. The major
cause of GIST is an abnormal form of tyrosine kinase protein. GISTs
may arise anywhere in the gastrointestinal tract, but are more
commonly detected in the stomach and small intestine.
Gastrointestinal bleeding and abdominal pain are the most frequent
symptoms associated with gastric GISTs. Surgical resection
currently remains the gold standard in the treatment of GISTs, and
it is indicated even when incomplete and aimed at symptom
palliation. Unresectable GISTs should be managed by molecularly
targeted intervention with imatinib mesylate (1).
Venous thromboembolism (VTE) is a common
complication in cancer patients, and three basic underlying
mechanisms have been described: Decreased blood flow, injury to the
vessel wall and disturbances in the balance between procoagulant
and anticoagulant factors (2).
However, the association and the pathophysiological mechanisms
between GISTs and VTE remain unclear. To the best of our knowledge,
there are only 4 cases in the currently available literature
highlighting the association between these rare tumours and VTE
(2–5).
We herein present a case of a gastric GIST
presenting with pulmonary embolism and discuss the mechanisms
implicated in the pathogenesis and the management of this
disease.
Case report
The patient was an 87-year-old woman with a past
history of secondary hypothyroidism five years following
thyroidectomy for non-toxic multinodular goiter, and no previous
history of VTE. The patient had no recent history of
immobilization, surgery or prolonged travel. She had no varicose
veins in the lower limbs and her body mass index was 28.2
kg/m2. The patient reported weight loss and progressive
cachexia over the last 2 months.
The patient presented in May 2017 to the Emergency
Department of University Hospital Gregorio Marañón with a sudden
onset of chest pain without dyspnea, fever or cough. On physical
examination, her blood pressure was 150/80 mmHg, with a heart rate
of 103 bpm. The remaining findings on physical examination were
unremarkable. The findings of the blood analysis were as follows:
Haemoglobin 12.5 g/dl, 215,000 platelets/mm3, creatinine
0.67 mg/dl, D-dimer 2,350 ng/ml and Nt-proBNP 378 pg/ml,
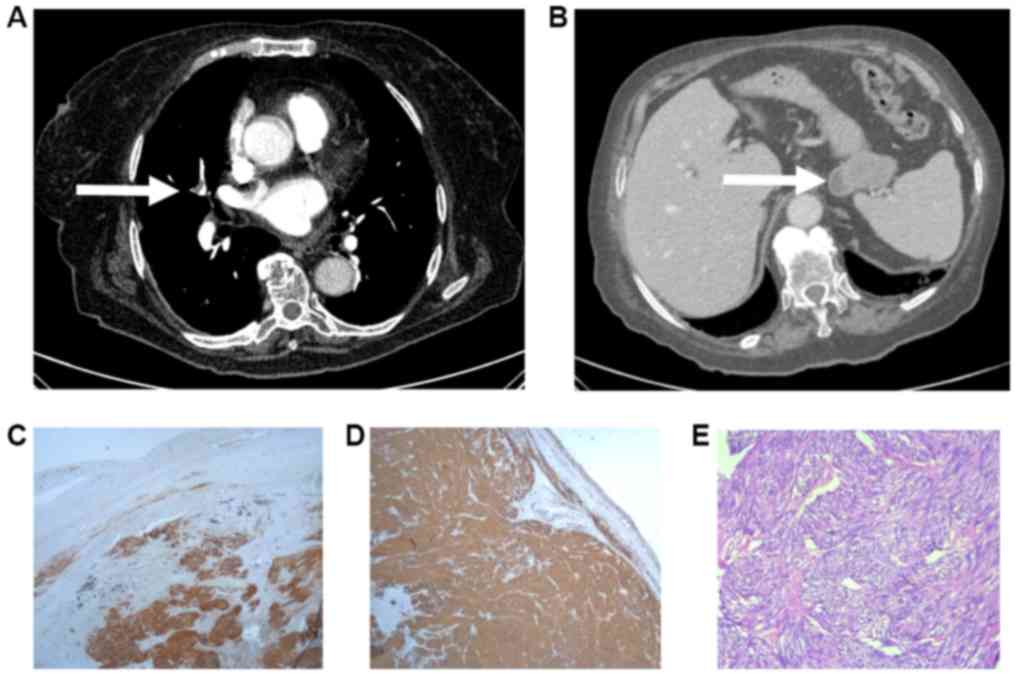
pO2 52 mm Hg and pCO2 38 mm Hg. A computed
tomography pulmonary angiography revealed multiple bilateral
filling defects in segmental and subsegmental arteries (Fig. 1A), and weight-adjusted enoxaparin was
initiated.
An abdominal computed tomography revealed a solid
heterogeneous 5.8×3.5×3.5 cm submucous mass in the gastric fundus,
suggesting the presence of a GIST (Fig.
1B). Upper endoscopy revealed a submucosal lesion in gastric
fundus. A Doppler-ultrasound of the lower extremities ruled out
deep vein thrombosis (DVT), and the findings on echocardiography
were normal. The patient was discharged with enoxaparin 100 mg/day.
Three months later, the patient underwent a gastric wedge resection
and the sample was sent for histopathological examination (Fig. 1C-E). The patient was treated with
enoxaparin 100 mg/day for 3 months. Then, enoxaparin was
discontinued one day before the surgery, and initiated again at 24
h after the surgery. A haematoma in the right flank appeared on the
second postoperative day, requiring enoxaparin withdrawal for 5
days. Anticoagulation was discontinued 3 months after surgery. Last
follow up was in December 2018 and the patient has remained
asymptomatic and has not showed evidence of recurrence of venous
thrombosis or cancer.
Discussion
VTE is a common complication in cancer patients and
three basic mechanisms have been suggested: Decreased blood flow,
injury to the vessel wall and disturbances in the balance between
procoagulant and anticoagulant factors (2). However, the association and
pathophysiological mechanisms between GISTs and VTE remain unclear.
To the best of our knowledge, there are only 4 cases in the
literature highlighting the association between these rare tumours
and VTE. Melichar et al presented the case of a patient with
peritoneal metastases of GIST involving the pelvis who was treated
with imatinib and succumbed to pulmonary embolism (PE) and DVT
caused by the compression of the common iliac vein by the tumour
(2). Kardos et al reported a
case of gastric GIST presenting as DVT and PE. In that case,
thorough evaluation did not reveal an aetiology for thrombosis
other than the GIST, suggesting that the neoplasm was the primary
cause (3). Sam et al
presented the case of a patient with small bowel GIST who was
diagnosed after jejunal intussusception and developed an episode of
DVT during hospitalization (4).
Thus, it may be hypothesized that the episode was cause by surgery
and immobilization, in addition to the presence of the tumour.
Finally, our group recently published the case of a patient with a
18×12 mm gastric GIST managed conservatively with close endoscopic
follow-up, who developed an episode of PE 6 months after the
diagnosis. In that case, the neoplasm was the only provoking factor
identified. The patient underwent tumour resection, allowing a
reduction in the duration of anticoagulant therapy (5). According to the recommendations of the
European Society of Medical Oncology-European Reference Network for
Rare Adult Solid Cancers, the standard approach to tumours >2 cm
in size is biopsy/excision, as they are associated with a higher
risk of progression if confirmed as GIST. Then, the standard
treatment for localized GISTs is complete surgical excision,
without dissection of clinically negative lymph nodes (6). The importance of the present case
report is that an associated VTE episode may worsen the prognosis
of the tumour, as VTE is a major cause of death in patients with
any type of cancer. Therefore, it is crucial to highlight the
association between VTE and this rare type of cancer, as
confirmation of such an association may prompt more aggressive
management of patients with GISTs.
The current guidelines recommend anticoagulation
with low-molecular-weight heparin as first-line treatment for the
acute phase of cancer-associated VTE. Prolonged anticoagulation
should be considered for an indefinite period of time or until
curative treatment (7). In the
present case, tumour resection enabled a reduction in the duration
of the anticoagulation, thereby reducing the risk of long-term
bleeding complications.
In summary, we herein present a case of GIST with
associated VTE. Since the association between these two entities
has not been clearly stablished, further studies evaluating the
frequency of VTE in patients with GIST are required.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
FGV, JDTC and PDR contributed to the conception and
design of the study, provided administrative support and study
materials, and recruited patients. Furthermore, they collected and
analysed data, as well as wrote the manuscript. All authors have
read and approved the final version of this manuscript for
publication.
Ethics approval and consent to
participate
The study was approved by the Research Ethics
Committee of the University Hospital Gregorio Marañón.
Patient consent for publication
The patient provided written informed consent
regarding the publication of the case details and any associated
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
El-Menyar A, Mekkodathil A and Al-Thani H:
Diagnosis and management of gastrointestinal stromal tumours: An
up-to-date literature review. J Can Res Ther. 13:889–900. 2017.
|
|
2
|
Melichar B, Laco J, Slovácek L, Grossmann
P and Vanecek T: Fatal venous thrombembolism complicating imatinib
therapy in a patient with metastatic gastrointestinal stromal
tumour. J Exp Clin Cancer Res. 25:607–610. 2006.PubMed/NCBI
|
|
3
|
Kardos M, Lundquist A, Misialek M and
Friedman LS: A rare presentation of an uncommon malignancy:
Thromboembolism in a patient with a gastrointestinal stromal
tumour. Dig Dis Sci. 56:2711–2714. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sam JJ, Mustard R, Kandel G, Gardiner G,
Ghaffar H, Kirpalani A, May G and Kim YI: Colonoscopy leads to a
diagnosis of a jejunal gastrointestinal stromal tumour (GIST).
Gastroenterology Res. 4:277–282. 2011.PubMed/NCBI
|
|
5
|
Demelo-Rodríguez P, Lavilla Olleros C,
Martín Higueras E, Peligros I and del Toro-Cervera J: Tumour del
estroma gastrointestinal como causa de trombosis asociada a cáncer.
Rev Gastroenterol Méx. 84:250–252. 2019. View Article : Google Scholar
|
|
6
|
Casali PG, Abecassis N, Aro HT, Bauer S,
Biagini R, Bielack S, Bonvalot S, Boukovinas I, Bovee JVMG,
Brodowicz T, et al: Gastrointestinal stromal tumours: ESMO-EURACAN
clinical practice guidelines for diagnosis, treatment and
follow-up. Ann Oncol. 29 (Suppl 4):iv2672018. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Konstantinides SV, Torbicki A, Agnelli G,
Danchin N, Fitzmaurice D, Galiè N, Gibbs JS, Huisman MV, Humbert M,
Kucher N, et al: Task force for the diagnosis and management of
acute pulmonary embolism of the european society of cardiology
(ESC). 2014 ESC guidelines on the diagnosis and management of acute
pulmonary embolism. Eur Heart J. 35:3033–3069. 2014. View Article : Google Scholar : PubMed/NCBI
|