Introduction
Armand Trousseau first reported Trousseau's
syndrome, which is characterized as a cerebral embolism due to
hypercoagulability resulting from malignant tumors, in 1865
(1). Trousseau's syndrome is now
defined as an unexpected cancer-related thrombotic event, such as a
cerebral infarction or deep vein thrombosis/pulmonary embolism
(2). Trousseau's syndrome is
recognized to be a fatal condition with a poor prognosis (3).
Cancer patients have an increased risk of arterial
thromboembolism even before cancer diagnosis, and its risk is
greater in more advanced stages of cancer (4,5). Among
patients with various cancer types, patients with lung cancer had
the greatest excess risk of arterial thromboembolism, with a 3
month cumulative incidence of 6.5% since diagnosis (compared with
1.2% in control patients) (4). The
precise mechanism underlying Trousseau's syndrome is not yet known.
However, the clear correlation between cancer stage and arterial
thromboembolism risk suggests a biological gradient between cancer
activity and arterial thromboembolism risk (4). Circulating micro-particles, secretion
of pro-coagulant factors, and alterations in platelet activity and
endothelial function are potential relevant factors of Trousseau's
syndrome (2,4).
There have been several reports on lung
adenocarcinoma accompanied with Trousseau's syndrome (6–9). Here,
we present a rare case of pulmonary pleomorphic carcinoma
accompanied with Trousseau's syndrome that manifested as
thromboembolic brain infarction at the time of postoperative cancer
recurrence.
Case report
A 74 year-old asymptomatic man was referred to our
department for the evaluation of a radiographically identified
solitary pulmonary mass. He was a current heavy smoker (38
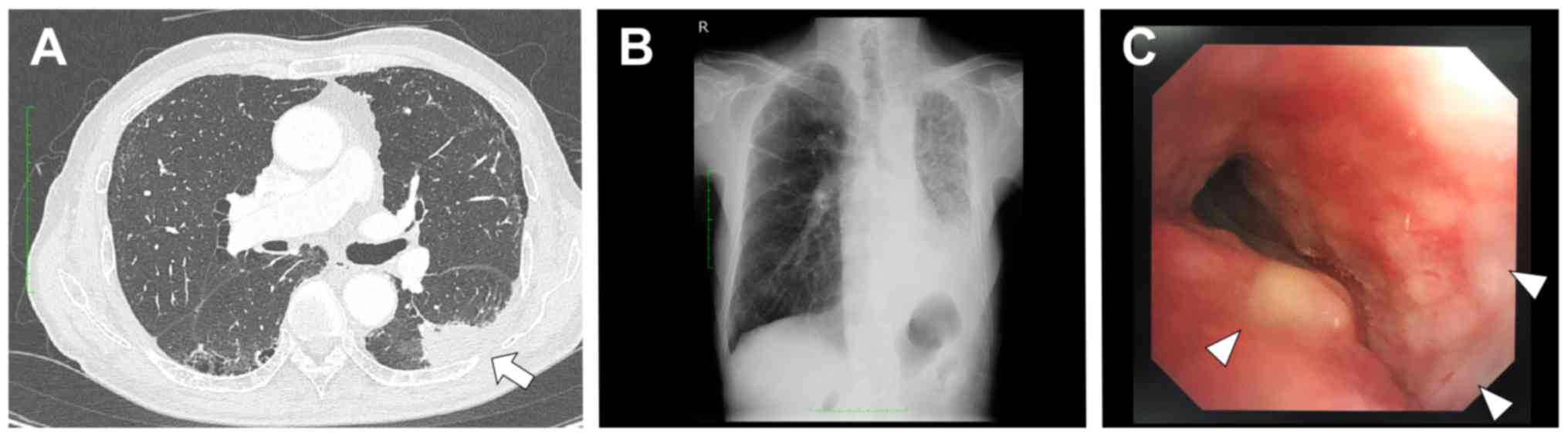
pack-years). Chest computed tomography (CT) revealed a
well-circumscribed peripheral mass (diameter: 38 mm) in the lower
lobe of the left lung (Fig. 1A). A
honeycomb finding was also detected in the dorsal portion of the
bilateral lung, indicating the presence of interstitial pneumonia.
A fluorine-18-fluorodeoxyglucose (FDG) positron-emission tomography
CT scan showed a strong accumulation of FDG (maximal level of
standardized uptake value: 24.7) in the mass. Serum
carcinoembryonic antigen (CEA) and D-dimer levels were 16.0 ng/ml
and 0.6 µg/ml, respectively. Although transbronchial biopsy failed
to yield a pathological diagnosis, the mass was suspected to be
malignant; therefore, a left lower lobectomy with systemic
mediastinal lymph node dissection was performed under
video-assisted thoracoscopic surgery.
Lung specimens were fixed in 10% buffered formalin
overnight at room temperature and embedded in paraffin. The
paraffin-embedded specimens were sliced 4 µm thick and stained with
hematoxylin and eosin, Periodic acid Schiff (PAS), and PAS with
diastase. Immunohistochemistry was performed using an
autoimmunostainer according to manufacturer instructions (Ventana
XT System Benchmark; Ventana Medical System, Inc.). The microscopic
analyses were performed by a Nikon Eclipse Ci microscope and DS-Fi2
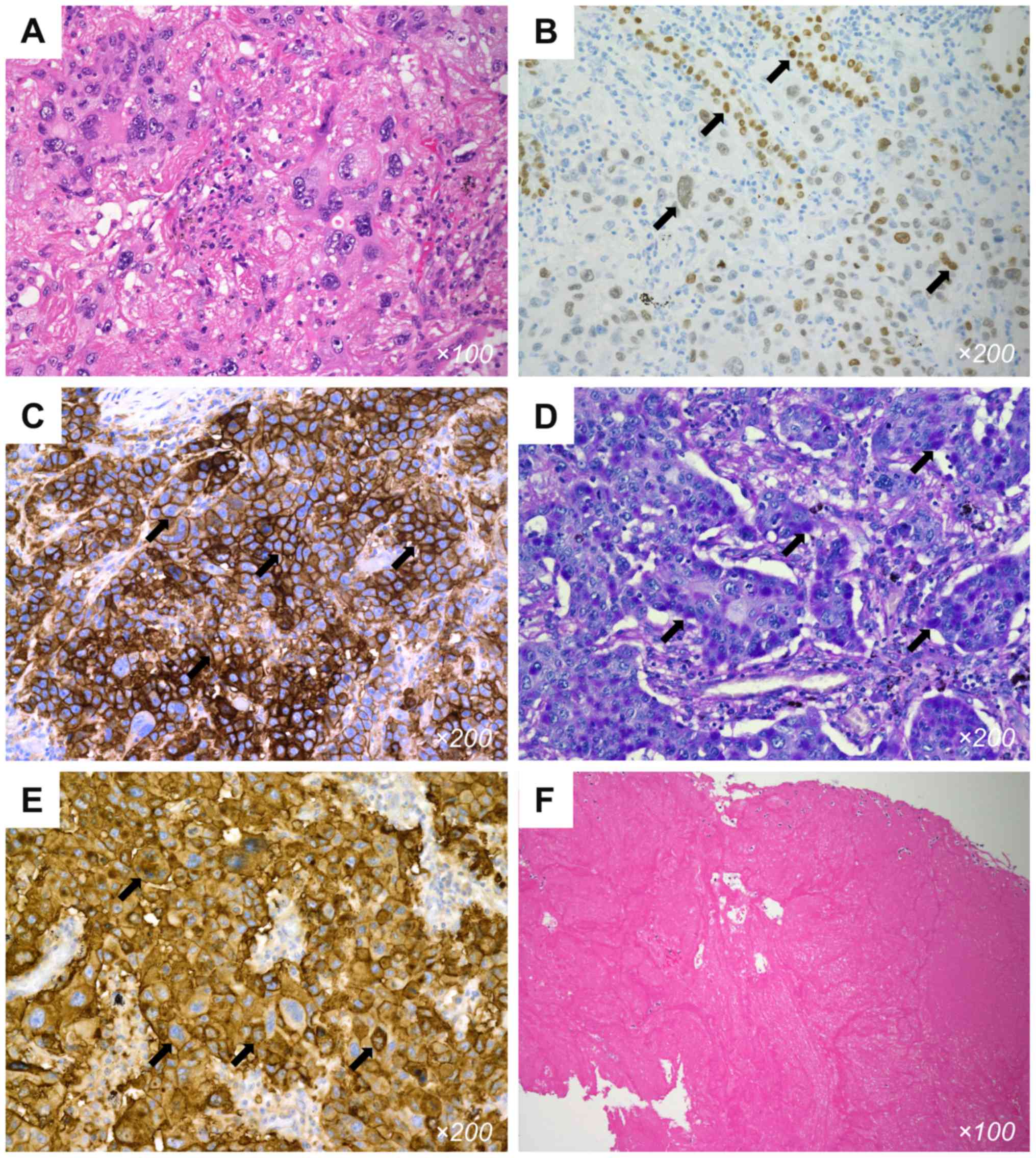
camera (Nikon Instruments). Pathological examination revealed
pleomorphic carcinoma, measuring 3.5 cm at its greatest diameter,
with visceral pleural and significant lymphatic invasion. Separate
tumor nodules were present in the same lobe. The bronchial stump
was tumor positive. The tumor extensively involved mediastinal
lymph nodes and was graded as pT3N2M0, pStage IIIB. The tumor
mainly comprised giant cells with high-grade pleomorphism and
abnormal mitosis (approximately 60% of the tumor) (Fig. 2A), admixed with a solid
adenocarcinoma component and papillary growth pattern at the
periphery, which was positive for thyroid transcription factor-1
(clone 8G7G3/1, 1:200; DakoCytomation) (Fig. 2B). High expression of programmed
death ligand-1 was confirmed in the tumor cells (clone 22C3
PharmDx, 1:100, tumor proportion score of 95%; Agilent) (Fig. 2C). Meanwhile, the tumor was negative
for epidermal growth factor receptor (EGFR) mutations and
anaplastic lymphoma kinase (ALK) protein expression. The
adenocarcinoma component was positive for periodic acid-Schiff
(PAS) stain and resistant to diastase, suggesting mucin production
(Fig. 2D). Moreover, most of the
tumor cells were strongly positive for tissue factor (clone TF
(H-9), 1:100; Santa Cruz Biotechnology, Inc.) (Fig. 2E).
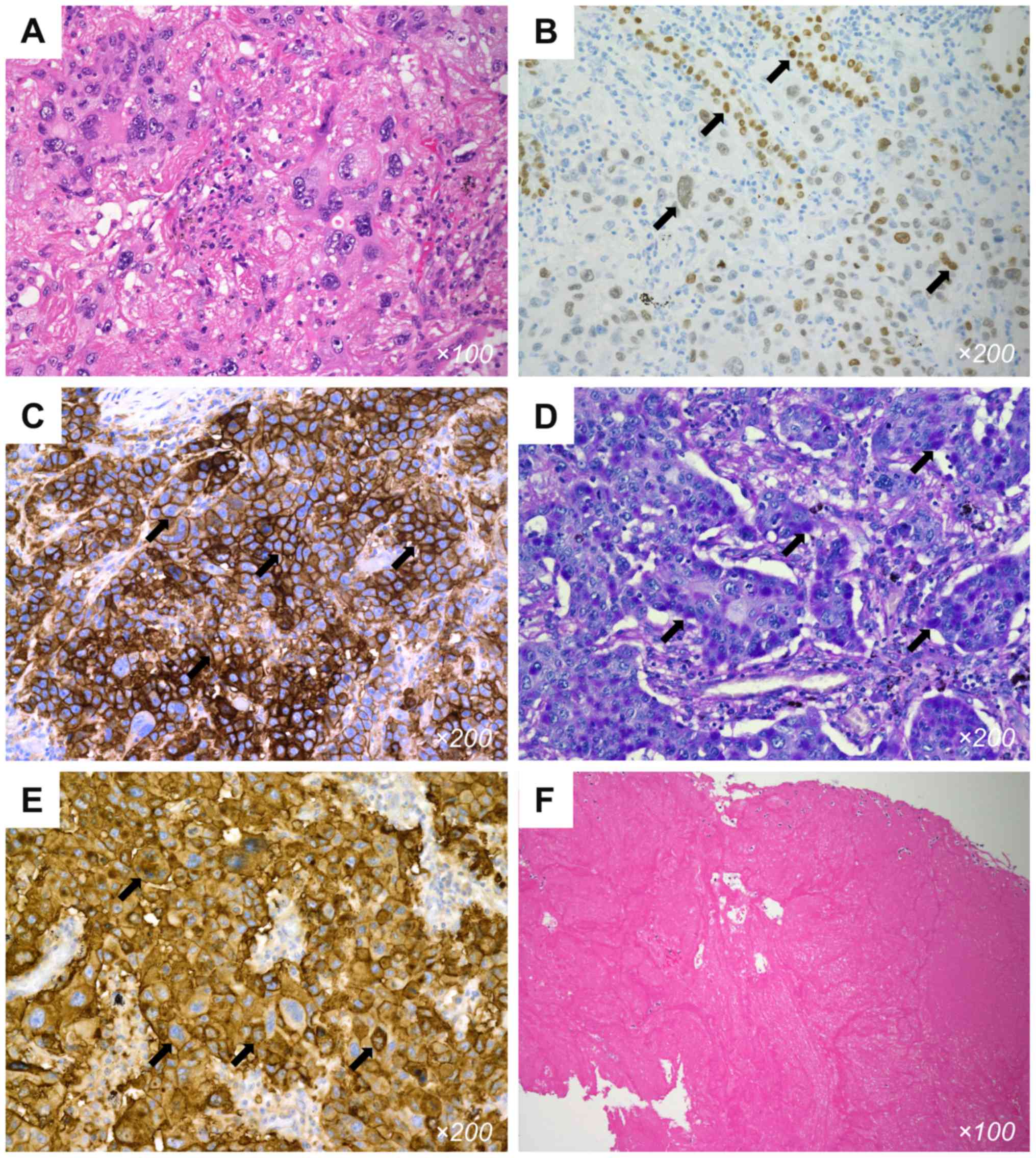 | Figure 2.Histological examination of a tumor
specimen. (A) Most of the tumor contained giant cells with atypia
as pulmonary pleomorphic carcinoma (H&E; magnification, ×100).
(B) Several tumor cell nests immunohistochemically positive for
TTF-1 were identified (arrows), suggesting adenocarcinoma (TTF-1;
magnification, ×200). (C) Immunohistochemical staining revealed
PD-L1 expression on 95% of the tumor cells (arrows; PD-L1, clone
22C3; magnification, ×200). (D) The tumor consisted, in part, of
solid adenocarcinoma harboring PAS-positive intracytoplasmic mucin
(arrows; PAS; magnification, ×200). (E) Tumor cells were strongly
positive for tissue factor [arrows; tissue factor, clone TF (H-9);
magnification, ×200]. (F) Retrieved thrombi from an occluded
intracerebral vessel was composed of fibrin (H&E;
magnification, ×100). H&E, hematoxylin and eosin; PAS, periodic
acid-Schiff stain; PD-L1, programmed death ligand-1; TTF-1, thyroid
transcription factor-1. |
Three months postoperatively, diffuse infiltration
rapidly appeared in plain chest radiographs of the left lung
(Fig. 1B), which was identified as
lymphangitic carcinomatosis rather than an acute exacerbation of
interstitial pneumonia, via bronchoscopy (Fig. 1C). Five days after examination and
prior to treatment for cancer recurrence, the patient suddenly
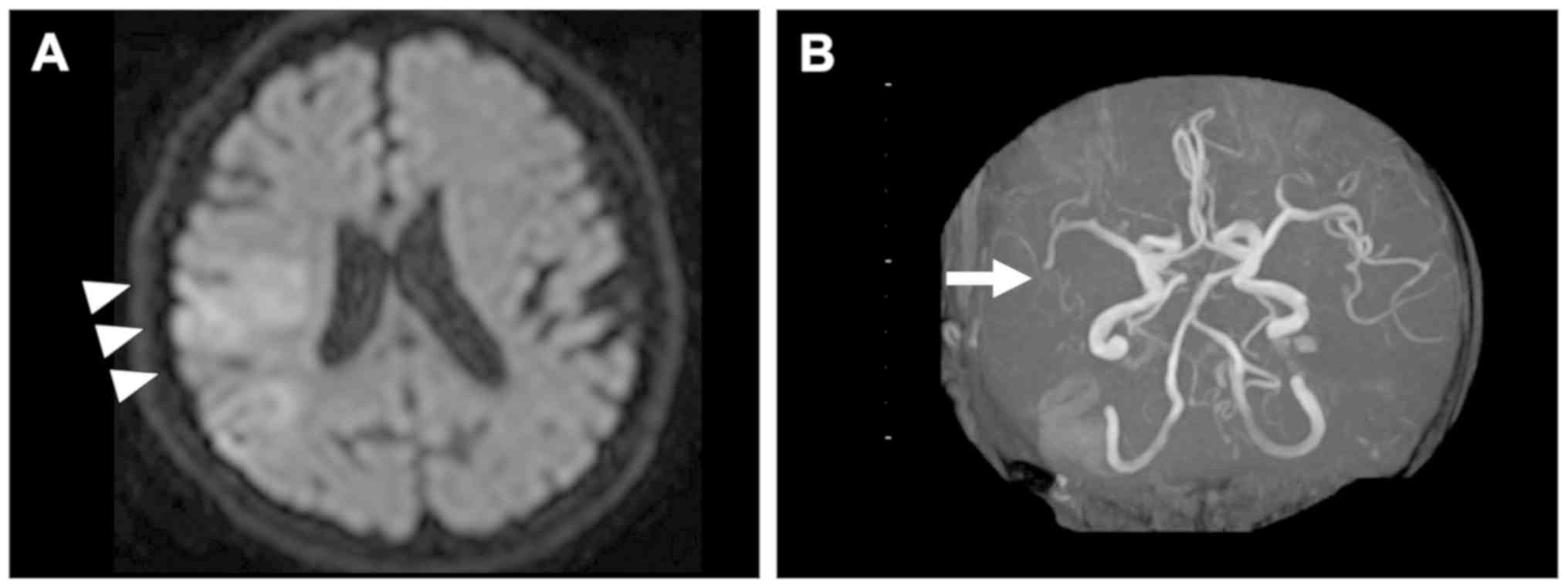
presented with dysarthria and left hemiplegia. Magnetic resonance
imaging revealed acute ischemic stroke in the right hemisphere
accompanied with subacute small infarcts in the left hemisphere and
bilateral cerebellum (Fig. 3A).
Magnetic resonance angiography revealed a right middle cerebral
artery M2 segment occlusion (Fig.
3B). An echography and a chest CT showed no evidence of
atherosclerotic thrombus or cardiac thrombus in the left atrium or
in the stump of the resected pulmonary vein. Plasma D-dimer and
fibrin/fibrinogen degradation product (FDP) levels were elevated at
17.6 µg/ml (normal <1.0) and 91.1 µg/ml (normal <5.0), as
were the CEA and carbohydrate antigen 125 (CA125) levels [73.4
ng/ml (normal <5.0) and 331 U/ml (normal <35)], respectively.
Although fibrinogen level was slightly decreased to 113 mg/dl, the
platelet count, prothrombin time international normalized ratio
(PT-INR), APTT, and, antithrombin level were within normal limits
(14.7×104/µl, 1.06, 27.6 sec, and 85%, respectively),
indicating that disseminated intravascular coagulation was not
overt (10). He underwent mechanical
thrombectomy with a stent retriever, and partial recanalization was
achieved. However, intracerebral hemorrhage was observed after
endovascular treatment. The pathology of the retrieved thrombus
showed that almost all parts consisted of fibrin without red blood
cells (Fig. 2F). These findings and
pathological findings of the primary lung cancer suggested
Trousseau's syndrome as the etiology of the cerebral infarction.
Five days following the onset of cerebral infarction, our patient
died of an intracerebral hemorrhage.
Discussion
Cancer-related arterial thromboembolism is often
accompanied with lung, pancreatic, gastric, and colon cancer
(4). The histology of most reported
cases of lung cancer with Trousseau's syndrome involves
adenocarcinoma (6–9). To our knowledge, this is the first
reported case of Trousseau's syndrome due to pulmonary pleomorphic
carcinoma.
Potential causes of brain infarction that occur
following lung cancer surgery include atherosclerotic thrombus,
cardiogenic thrombus, thrombus from the stump of the resected
pulmonary vein, tumor embolization, and Trousseau's syndrome
(2,11–13). In
this case, elevated D-dimer levels and extensive production of
tissue factor in the tumor cells indicated a hypercoagulable state
at the time of lung cancer recurrence. Moreover, elevated CA125
levels, the presence of mucin-producing adenocarcinoma as a
component of the pleomorphic carcinoma, and fibrin thrombus
indicated the possibility of a cancer-related thrombus as an
etiology of the brain infarction (6,14,15).
These findings suggested that Trousseau's syndrome in relation to
recurrent pulmonary pleomorphic carcinoma was the most probable
etiology.
Pulmonary pleomorphic carcinoma is a rare malignant
lung tumor and exhibits poor prognosis. Pulmonary pleomorphic
carcinoma is defined as a poorly differentiated non-small cell
carcinoma (NSCC), namely, a squamous cell carcinoma,
adenocarcinoma, or undifferentiated NSCC that contains at least 10%
spindle and/or giant cells, or a carcinoma consisting only of
spindle and giant cells (16). In
our case, the pleomorphic carcinoma included mucin-producing solid
adenocarcinoma that was revealed through PAS reaction, although
hematoxylin and eosin staining failed to confirm this.
Cancer-producing mucins are large, heavily
glycosylated molecules that can act as ligands for selectins,
particularly L-selectin of leukocytes and P-selectin of endothelium
and/or platelets, causing platelet aggregation without the help of
thrombin (17). Mucins are
considered to be a coagulation trigger, resulting in the induction
of disseminated thrombosis (6). In
this case, the elevated CA125 level, a potential biomarker for a
mucin-producing tumor (18), was
consistent with the presence of mucin in the tumor.
Tissue factor is a primary cellular initiator of
fluid-phase blood coagulation that changes factor VII (FVII) to its
activated form (FVIIa) and initiates the extrinsic coagulation
pathway (2). Tumor cells of various
malignancies sometimes produce tissue factor and may play an
important role in the development of a thromboembolism in cancer
patients (7,19). Sato et al (7), reported that Trousseau's syndrome
associated with tissue factor was produced by pulmonary
adenocarcinoma. Sawada et al (19), reported that high tissue factor
expression of tumor cells had close associations with advanced
stage tumors and tumor recurrence, and approximately one-third of
metastatic lung cancers had a strong tissue factor expression. Our
recurrent case had aggressive features and expressed tissue factor
extensively, which was consistent with the findings of a previous
report. An increase in tissue factor production might partially
explain the higher incidence of Trousseau's syndrome in patients
with advanced stage malignancies.
Prognosis of cancer patients with stroke is poor
(median survival 4.5 months), and 25% of them die within 30 days
after the diagnosis of stroke (3).
However, recently, a combination therapy comprising
anti-coagulation treatment and chemotherapy or molecular targeted
treatment has succeeded in inhibiting repeated thrombosis and
controlling the tumor (8,9). Pulmonary pleomorphic carcinoma often
relates with high PD-L1 expression (20), and anti-PD-1/PD-L1 antibody treatment
may be a promising treatment option (21). Early and accurate clarification of
the etiology of a brain infarction may improve outcomes, especially
for cases involving Trousseau's syndrome. Therefore, we recommend
clinicians should not exclude the possibility of Trousseau's
syndrome, even in diagnosed cases of pulmonary pleomorphic
carcinoma.
In conclusion, we report the first case of
Trousseau's syndrome accompanied with pulmonary pleomorphic
carcinoma showing aggressive features and a hypercoagulable state
at the time of recurrence. The mucin-producing component or tissue
factor present in the tumor may be associated with a
hypercoagulable state leading to cancer-related thrombosis.
Monitoring of D-dimer and CA125 levels during postoperative
follow-up after lung cancer surgery, especially in cases of
aggressive recurrence patterns, could help early detection and
treatment of a life-threatening cancer-related thrombosis.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analysed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
SO and MI conceived and designed the study. SO, JF,
NI and TN collected the clinical data during the case study. AMH
performed the pathological analyses. SO, JF and AMH wrote the
manuscript. SO, AMH, JF, NI, TN, HT, MS, JS and MI interpreted the
data and revised the clinical content. All authors read and
approved the final manuscript of the manuscript, and agreed to be
accountable for all aspects of this work.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient's kin for the publication of this data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Trousseau A: Plegmasia alba dolensLectures
on clinical medicine, delivered at the Hotel-Dieu, Paris. 5. The
New Sydenham Society; London: pp. 281–332. 1865
|
|
2
|
Varki A: Trousseau's syndrome: Multiple
definitions and multiple mechanisms. Blood. 110:1723–1729. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cestari DM, Weine DM, Panageas KS, Segal
AZ and DeAngelis LM: Stroke in patients with cancer: Incidence and
etiology. Neurology. 62:2025–2030. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Navi BB, Reiner AS, Kamel H, Iadecola C,
Okin PM, Elkind MSV, Panageas KS and DeAngelis LM: Risk of arterial
thromboembolism in patients with cancer. J Am Coll Cardiol.
70:926–938. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Navi BB, Reiner AS, Kamel H, Iadecola C,
Okin PM, Tagawa ST, Panageas KS and DeAngelis LM: Arterial
thromboembolic events preceding the diagnosis of cancer in older
persons. Blood. 133:781–789. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tachihara M, Nikaido T, Wang X, Sato Y,
Ishii T, Saito K, Sekine S, Tanino Y, Ishida T and Munakata M: Four
cases of trousseau's syndrome associated with lung adenocarcinoma.
Intern Med. 51:1099–1102. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sato T, Tsujino I, Ikeda D, Ieko M and
Nishimura M: Trousseau's syndrome associated with tissue factor
produced by pulmonary adenocarcinoma. Thorax. 61:1009–1010. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Masubuchi H, Maeno T, Uchida M, Kono S,
Suzuki M, Takemura M, Yamaguchi A, Yamaguchi K, Kanbe M and
Kitahara S: A case of trousseau syndrome caused by pulmonary
adenocarcinoma that was controlled for one year and 10 months with
thrombosis treatment using an EGFR tyrosine kinase inhibitor and
chemotherapy. Respir Med Case Rep. 15:101–105. 2015.PubMed/NCBI
|
|
9
|
Nonagase Y, Takeda M, Tanaka K, Hayashi H,
Iwasa T and Nakagawa K: Treatment of EGFR mutation-positive
non-small cell lung cancer complicated by Trousseau syndrome with
gefitinib followed by osimertinib: A case report. Oncotarget.
9:29532–29535. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Asakura H, Takahashi H, Uchiyama T, Eguchi
Y, Okamoto K, Kawasugi K, Madoiwa S and Wada H: Proposal for new
diagnostic criteria for DIC from the Japanese society on thrombosis
and hemostasis. Thromb J. 14:422016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhang YY, Cordato D, Shen Q, Sheng AZ,
Hung WT and Chan DK: Risk factor, pattern, etiology and outcome in
ischemic stroke patients with cancer: A nested case-control study.
Cerebrovasc Dis. 23:181–187. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hattori A, Takamochi K, Kitamura Y,
Matsunaga T and Suzuki K, Oh S and Suzuki K: Risk factor analysis
of cerebral infarction and clinicopathological characteristics of
left upper pulmonary vein stump thrombus after lobectomy. Gen
Thorac Cardiovasc Surg. 67:247–253. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cho Y, Hida Y, Kaga K, Kato H, Iizuka M
and Kondo S: Brain metastases secondary to tumor emboli from
primary lung cancer during lobectomy. Ann Thorac Surg. 86:312–313.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Matsumoto N, Fukuda H, Handa A, Kawasaki
T, Kurosaki Y, Chin M and Yamagata S: Histological examination of
trousseau syndrome-related thrombus retrieved through acute
endovascular thrombectomy: Report of 2 Cases. J Stroke Cerebrovasc
Dis. 25:e227–e230. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ishikawa M, Nakayama K, Ishibashi T, Sato
E, Nakamura K, Katagiri H and Kyo S: Case series of cerebral
infarction with trousseau's syndrome associated with malignant
gynecological tumors. Mol Clin Oncol. 5:138–142. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Travis WD, Brambilla E, Nicholson AG,
Yatabe Y, Austin JHM, Beasley MB, Chirieac LR, Dacic S, Duhig E,
Flieder DB, et al: The 2015 world health organization
classification of lung tumors: Impact of genetic, clinical and
radiologic advances since the 2004 classification. J Thorac Oncol.
10:1243–1260. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wahrenbrock M, Borsig L, Le D, Varki N and
Varki A: Selectin-mucin interactions as a probable molecular
explanation for the association of trousseau syndrome with mucinous
adenocarcinomas. J Clin Invest. 112:853–862. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Jovin TG, Boosupalli V, Zivkovic SA,
Wechsler LR and Gebel JM: High titers of CA-125 may be associated
with recurrent ischemic strokes in patients with cancer. Neurology.
64:1944–1945. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sawada M, Miyake S, Ohdama S, Matsubara O,
Masuda S, Yakumaru K and Yoshizawa Y: Expression of tissue factor
in non-small-cell lung cancers and its relationship to metastasis.
Br J Cancer. 79:472–477. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kim S, Kim MY, Koh J, Go H, Lee DS, Jeon
YK and Chung DH: Programmed death-1 ligand 1 and 2 are highly
expressed in pleomorphic carcinomas of the lung: Comparison of
sarcomatous and carcinomatous areas. Eur J Cancer. 51:2698–2707.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ikematsu Y, Yoneshima Y, Ijichi K, Tanaka
K, Harada T, Oda Y, Nakanishi Y and Okamoto I: Marked response to
pembrolizumab in a patient with pulmonary pleomorphic carcinoma
highly positive for PD-L1. Lung Cancer. 112:230–231. 2017.
View Article : Google Scholar : PubMed/NCBI
|