Introduction
Radiation therapy for breast cancer has been
established as a standard treatment after breast-conserving surgery
(1). In postmastectomy radiation
therapy, the dose on the skin surface ranges from 50 to 60% of the
prescribed one, which is usually 2 Gy daily at the isocenter or the
International Commission of Radiation Units reference point
(2). Darby et al reported
that survival rates improved and relapse rates for breast cancer
decreased after radiation therapy (3). However, radiation therapy may have
adverse effects on tissues or organs of patients receiving the
same. Therefore, it is of great importance that medical staff
supports skin self-care and adequately manages the symptoms of
patients undergoing radiation therapy.
Radiodermatitis, an acute adverse effect, has been
considered as one of the most frequent symptoms. Despite the
skin-sparing benefits of contemporary techniques, most patients
experience some degree of integumentary system reaction (4,5).
Symptoms usually appear a few weeks after the onset of radiation
therapy, wherein the skin becomes red, dry, warm, and sore
(6). To take care for such patients,
medical staff needs to assess the skin condition in the irradiated
area and educate the patients regarding skin lesion care according
to the degree of skin reaction.
Generally, medical staff in Japan has used the
Common Terminology Criteria for Adverse Events (CTCAE version 4.0)
for skin evaluation (7). However,
CTCAE is limited in its capability to assess detailed changes in
skin condition because of its subjective nature. For example, under
the ‘Dermatitis radiation’ classification, CTCAE defines ‘Faint
erythema or dry desquamation’ and ‘Moderate to brisk erythema’ as
Grade 1 and Grade 2, respectively. However, nurses frequently find
it difficult to distinguish ‘Faint’ skin reactions from ‘Moderate’
one. Furthermore, the assessment of radiodermatitis using CTCAE
might vary depending on the person assessing the skin reaction.
Our previous research identified skin surface
temperature (SST) and erythema intensity (EI) as objective
assessment tools that could clarify the skin condition in detail
both during and after radiation therapy (8). However, our prior study included only a
small sample size, and the measurements of those parameters were
performed at only two points: Before and after radiation therapy.
The present study therefore investigated the changes in skin
condition among patients with breast cancer who underwent radiation
therapy using objective assessment tools in greater detail.
Patients and methods
Subjects
A total of 18 patients with breast cancer undergoing
radiation therapy after surgery were enrolled. This study was
approved by the Committee for Medical Ethics of Hirosaki University
(Hirosaki) and was conducted after obtaining written informed
consent from each patient.
Radiation therapy was performed at Hirosaki Central
Hospital using a linear accelerator (ClinaciX, Varian Medical
Systems) employing 6-MV X-rays. Tangential irradiation technique
with two non-parallel portals was used. The total target dose was
50 Gy in 25 fractions with a conventional schedule.
Measurements
The patients' skin condition was measured using a
Multi-skin instrument® consisting of
Mexameter® MX18, Corneometer® CM825, and
Skin-Thermometer® ST500 (Courage + Khazaka Corporation)
(9,10) before, during, and six months after
radiation therapy. These devices enable non-invasive measurement
through pen-type probes and can evaluate four skin parameters. The
measured parameters include SST, hydration level of the skin
surface (stratum corneum) (HL), melanin intensity (MI), and EI. The
measurement of HL was 10–20 µm of the stratum corneum to avoid the
influence of deeper skin layers (e.g., from the blood vessels).
Measurements using a 15 mm thick foil showed only 20% of the
original measurement value (9). MI
and EI were measured based on absorption/reflection of light. The
Mexameter® MX18 probe is able to emit three specific
light wavelengths (568, 660 and 870 nm), and the receiver measures
the light reflected by the skin. The highly sensitive measurement
gives broad-scale values (0–999) for melanin and erythema.
Therefore, even the smallest changes in color become traceable
(10). The quantity of light
absorbed by the skin can be calculated. The MI among healthy
Japanese women is reported to be approximately 100–200 (11,12). The
measurement procedure was performed in a medical examination room
that was maintained at a temperature of 25.4±0.6°C via an air
conditioner.
Subjective evaluation index of acute
radiodermatitis
The severity or grade of acute radiodermatitis was
clinically evaluated according to the CTCAE version 4.0, Japanese
Clinical Oncology Group version (7).
CTCAE was developed by National Cancer Institute and is widely
accepted throughout the oncology research community as the standard
grading scale for adverse events. The radiation dermatitis index of
the CTCAE consists of five scales (Table
I). In this study, one radiologist who is a specialist of
radiotherapy judged what CTCAE level of the subject's dermatitis
and one nurse confirmed that throughout the period of this
study.
 | Table I.Dermatitis radiation index of
CTCAE. |
Table I.
Dermatitis radiation index of
CTCAE.
| Index | Grade 1 | Grade 2 | Grade 3 | Grade 4 | Grade 5 |
|---|
| Dermatitis
radiation | Faint erythema or dry
desquamation | Moderate to brisk
erythema; patchy moist desquamation, mostly confined to skin folds
and creases; moderate edema | Moist desquamation in
areas other than skin folds and creases; bleeding induced by minor
trauma or abrasion | Life-threatening
consequences; skin necrosis or ulceration of full thickness dermis;
spontaneous bleeding from involved site; skin graft indicated | Death |
Statistical analysis
All data are expressed as means ± standard
deviations and were analyzed using the SPSS version 22.0 software.
Results were compared using repeated measures ANOVA followed by
Bonferroni. Comparisons between the irradiated and contralateral
side at the same time-point were performed using a two-sided paired
t-test. P<0.05 was considered to indicate a statistically
significant difference.
Results
Patient characteristics
A total of 18 patients with breast cancer who
underwent breast-conserving surgery and postmastectomy radiation
therapy were enrolled. The patient characteristics are shown in
Table II. The average age was
56.8±11.7 years, and their breast cancer stages ranged from IA
through IIIB. Moreover, the laterality of the primary lesion of six
patients was right side, while that of the other 12 patients was
left side. In the pathological classification, one patient was
adenocarcinoma, not other specified, and 11 patients were ductal
carcinoma. Women who had breast-conserving surgery for unifocal
invasive ductal adenocarcinoma (excluding invasive carcinoma of
classical lobular type) of any grade (1–3) were
recruited. Nine patients received hormone administration, four
received chemotherapy, and four received both hormone
administration and chemotherapy.
 | Table II.Subject characteristics (n=18). |
Table II.
Subject characteristics (n=18).
| Characteristics | Value |
|---|
| Age (years) | 56.8±11.7 |
| Disease stage |
|
| Stage
IA | 10 |
| Stage
IB | 5 |
| Stage
IA | 1 |
| Stage
IB | 2 |
| Laterality of primary
lesions |
|
|
Right | 7 |
| Left | 11 |
| Adenocarcinoma,
NOS |
|
| Ductal | 1 |
| Mucinous
adenocarcinoma | 1 |
| Tubular
adenocarcinoma | 1 |
| Scirrhous
adenocarcinoma | 15 |
| Combination
therapy |
|
| Hormone
therapy | 9 |
|
Chemotherapy | 4 |
| Hormone
therapy and chemotherapy | 4 |
Changes in parameters during radiation
therapy
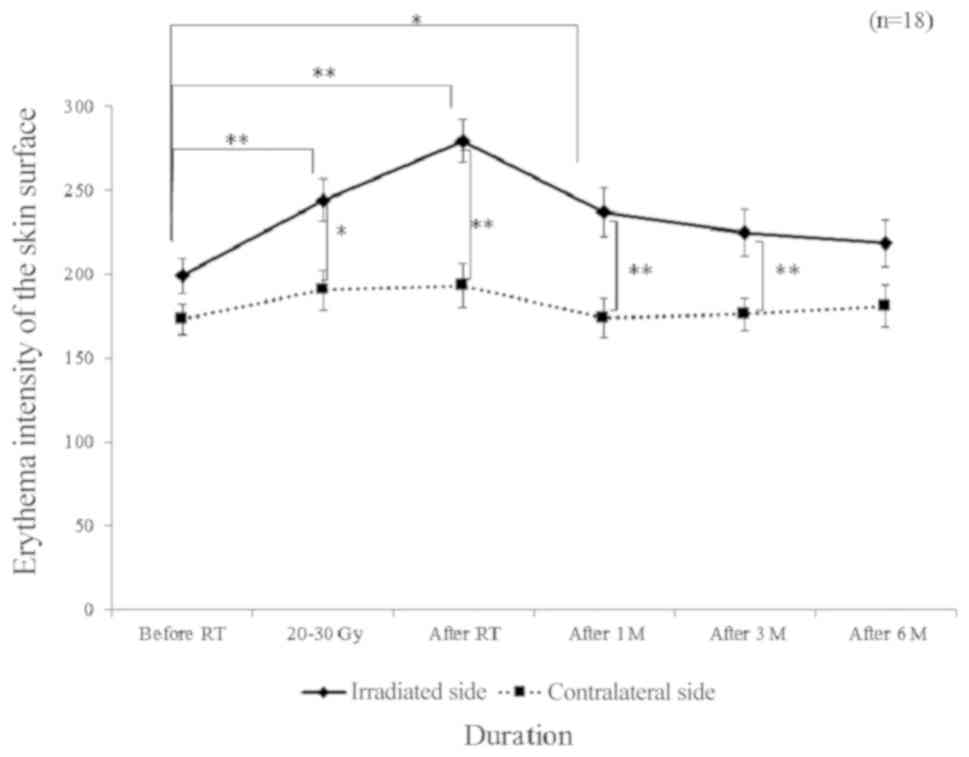
EI levels at the irradiated site gradually elevated
during radiation therapy and peaked upon completion thereof,
whereas those at the non-irradiated contralateral site remained
unchanged (Fig. 1). EI levels at the
irradiated site returned to baseline six months after cessation of
the radiation therapy and were comparable to those at the
non-irradiated site.
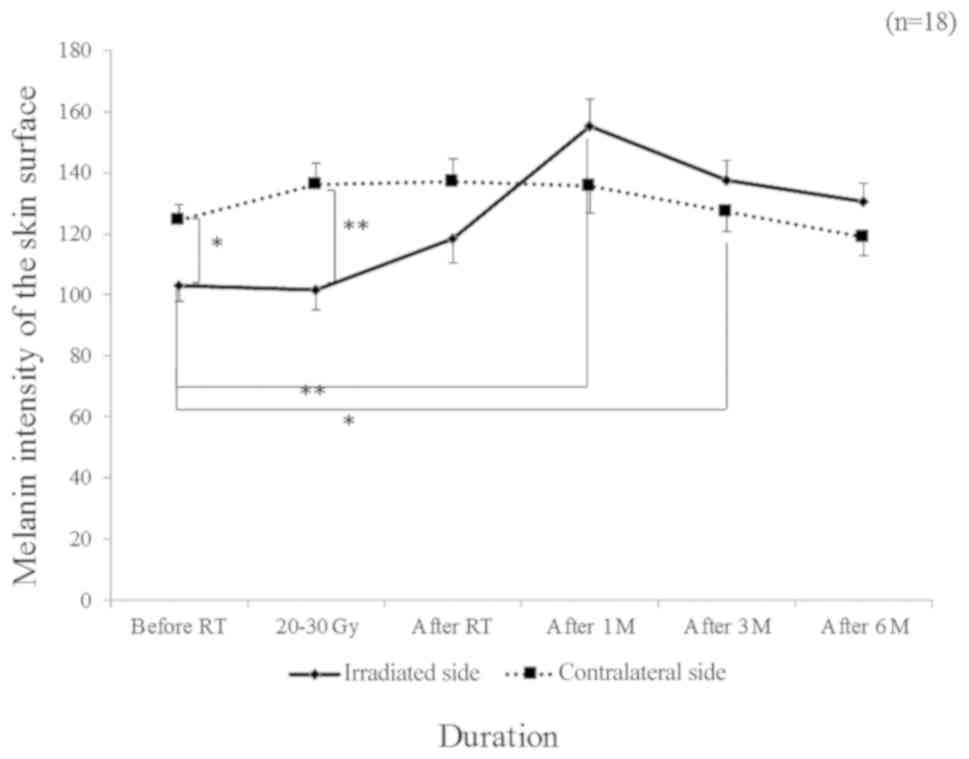
Similar to EI, MI levels at the irradiated site were
elevated during radiation therapy but those at the contralateral
non-irradiated site remained unchanged (Fig. 2). Upon completion of radiation
therapy, MI levels at the irradiated sites were higher than those
at the contralateral site (P<0.05). MI levels at the irradiated
site subsequently declined to baseline six months after radiation
therapy.
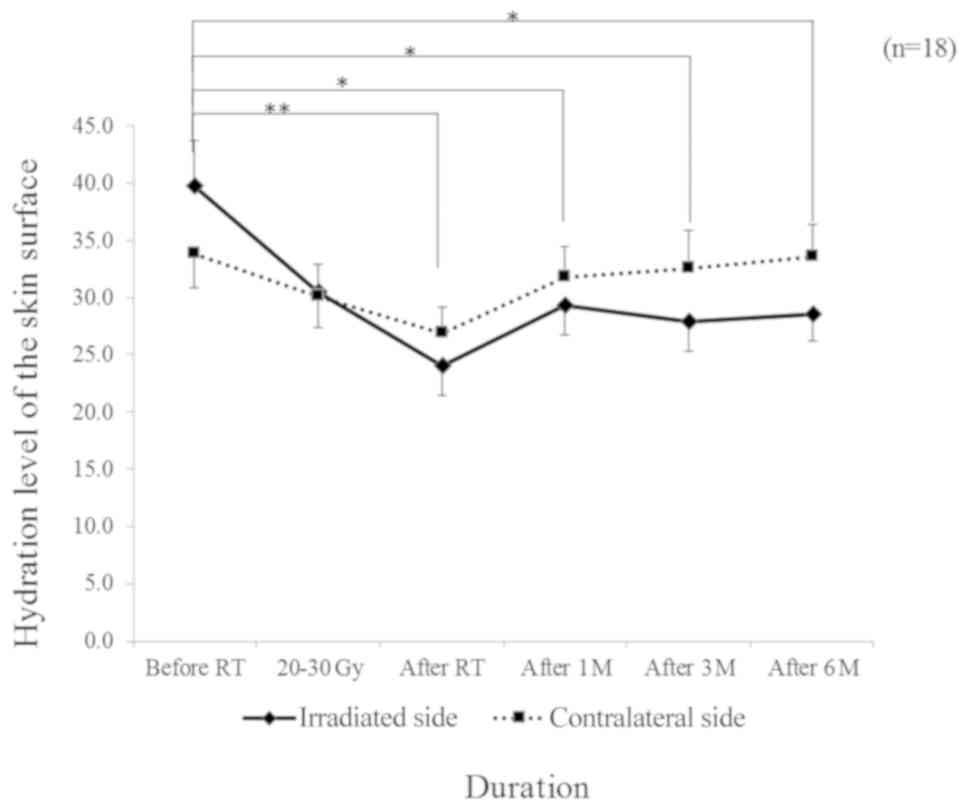
Fig. 3 shows the
changes in HL at the irradiated and nonirradiated sites during and
after radiation therapy. In contrast to EI and MI, HL at both sites
was at its lowest upon completion of radiation therapy. HL at the
non-irradiated control site recovered to baseline six months after
radiation therapy, whereas that at the irradiated site remained
lower than that at the control site.
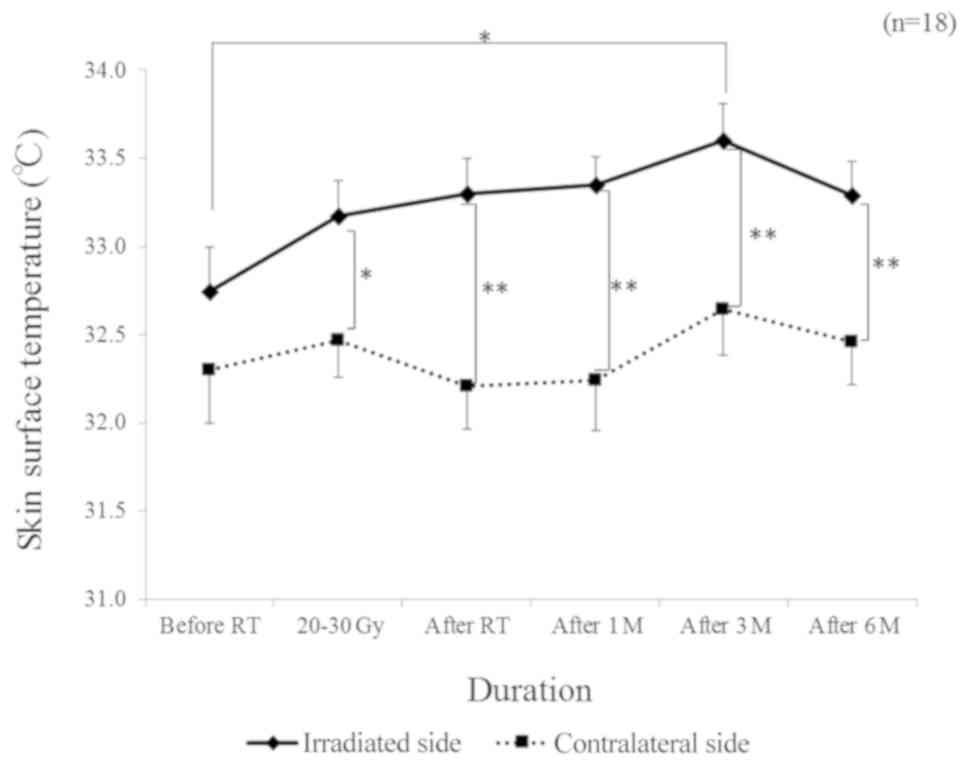
As shown in Fig. 4,
no difference in SST levels was observed between the irradiated and
nonirradiated sites before radiation therapy. However, SST levels
at the irradiated site became elevated during radiation therapy
(P<0.05) and plateaued even after its cessation, whereas that at
the non-irradiated site remained unchanged throughout the study.
Even six months after radiation therapy, the SST levels were higher
at the irradiated site than at the non-irradiated site
(P<0.05).
Comparison between the CTCAE and EI
levels
The CTCAE grades ranged from 0 to 2 in this study.
EI levels ranged from 177 to 333 and from 119 to 283 when the CTCAE
was Grade 1 and Grade 2, respectively.
Discussion
Our research revealed the degree of radiodermatitis
for breast cancer patients using novel instrument however this is a
small study. The major findings of the present study showed that EI
and MI levels at the irradiated site peaked upon completion of
radiation therapy and subsequently declined to baseline after six
months. In contrast, SST levels at the irradiated site increased
during radiation therapy and plateaued after its completion. The
same parameters at the nonirradiated control site remained
unchanged throughout the study period. Moreover, HL levels at both
the irradiated and nonirradiated sites were at their lowest upon
completion of radiation therapy. HL at the nonirradiated sites
returned to the baseline six months after radiation therapy,
whereas that at the irradiated sites remained low. No relationship
was observed between the CTCAE grade and EI level.
Duration of skin observation and
self-care
Radiodermatitis has been associated with the
integumentary system's response to planned ionizing radiation
exposure, which causes depletion of stem cells from the basal layer
of the epidermis (13). More intense
erythema and hyperpigmentation have been shown to occur after 2–3
weeks of treatment (14,15). The present study investigated changes
in skin condition before and six months after the radiation therapy
in patients with breast cancer. According to the objective
assessment tools, SST, MI, and HL remained impaired six months
after cessation of radiation therapy, although EI levels had
already recovered after radiation therapy. In addition, EI
evaluated as CTCAE-Grade 1 overlapped with that evaluated as
CTCAE-Grade 2. These findings suggest that even when skin erythema
could no longer be observed visually, observation of skin condition
should be continued for at least six months after radiation
therapy. Functional changes, such as those to the sweating ability
of the irradiated skin, might persist longer than readily visible
morphological changes.
HL at the irradiated sites was significantly lower
than that at the nonirradiated ones during and after radiation
therapy. This might be related to impaired sweating due to sweat
gland damage after irradiation. It seems reasonable to presume that
basal skin layer damage is involved in prolonged recovery. This
prolonged phenomenon strongly necessitates medical staff to provide
patient education regarding skin hydration and usage of
moisturizers. Moisturizers may facilitate skin fluid volume
recovery, which can be determined by analyzing the difference
between the presence and absence of moisturizer usage and the
frequency of application. In a study evaluating radiodermatitis
caused by accelerated partial breast irradiation (APBI) using
high-dose-rate interstitial brachytherapy, changes in moisture were
less severe and recovery was more rapid after APBI than after
external beam radiation therapy (16). Accordingly, a difference in the
appearance of dermatitis has been observed based on radiotherapy
treatment. In this study, the subjects did not use moisturizer
until after radiodermatitis occurred. Sekiguchi et al
reported that the application of a heparinoid moisturizer for 2
weeks resulted in lower skin dryness and desquamation compared to
the non-application thereof (17).
Therefore, medical staff should advice their patients regarding the
appropriate timing of moisturizer usage.
Inflammation and preventive strategy
SST levels at the irradiated sites were
significantly higher than those at the nonirradiated sites six
months after radiation therapy. Although this could have been
caused by the inflammatory response after surgery, it is difficult
to confirm the pathogenesis of the higher SST levels. We emphasize
that even when EI levels at the irradiated site had normalized,
inflammatory changes that needed self-care still persisted.
Incidence rates of dermatitis may be dependent on
various factors. For example, reports have shown that patients with
breast volume >1,600 cm3 had more acute skin lesions
(18), while incidence rates of
radiodermatitis were correlated with the planning target volume. To
anticipate the risk of adverse effects, nurses need to communicate
with radiologists and radiological technologists regarding the
treatment plan before radiation therapy. After radiation therapy
initiation, instructions regarding the appropriate underclothing
and method of skin cleaning provided by the nurses might prevent
skin problems. Given that the patients' self-care habits could
affect their skin condition, statements regarding patient self-care
should henceforth be analyzed using objective assessment tools.
Whelan et al reported that adverse effects like
radiodermatitis and breast pain induced a decline in patient
quality of life (QOL) (19). Thus,
using some objective parameters to help patients understand their
skin condition is imperative. In this study, we used noninvasive
instruments to objectively assess the patients' skin condition
objectively. Conversely, Fuzissaki et al used the Radiation
Therapy Oncology Group and the World Health Organization scale
together, whereas Partl et al employed the application of a
new image-analysis tool (20,21).
These methods can help to assess a patient's skin without
inter-observer variability. The assessment tool in this study has a
great benefit for patients to monitor their skin changes without
pain. In addition, patients who experienced stress at the beginning
of radiotherapy had the same or increased levels of stress during
and shortly after treatment (22).
The assessment of objective parameters might help patients to
maintain or improve their QOL and also provide them the opportunity
to recognize their skin condition. Significant predictors of
distress and emotional upset prior to radiation therapy included
feelings of pessimism, cancer stage, and history of mastectomy
(23). The level of distress among
patients with breast cancer did not significantly vary until six
months post-treatment, but it could span up to 12 months or more
after the initial diagnosis (24).
Therefore, we should also consider the patient's emotional state
when providing an explanation regarding their skin condition and
methods of self-care.
In conclusion, skin assessment with the instrument
used in this study is useful to assess the details of the skin and
explain patients regarding the need of good skin self-care.
Moreover, we believe that the combination of CTCAE and objective
assessment tools will enable a more accurate assessment of
radiodermatitis.
Acknowledgements
We would like to thank all of the patients and
medical staff who participated in this study. The authors would
additionally like to thank Enago (www.enago.jp)
for the English language review.
Funding
The present study was supported by JSPS KAKENHI
(grant no. 26670951).
Availability of data and materials
Datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
MK initiated the research. MK, KM, YN, CI, YF, YH,
MT, and KK collected the data from the subjects. MK, KM, YN, CI,
YF, YH, YM, MT, KK and TO analyzed the data. YM and TO drafted,
reviewed and revised the manuscript. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Committee for Medical
Ethics of Hirosaki University (Hirosaki) (approval no. 2013-65).
All patients provided informed consent prior to study participation
and for publication of any associated data.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interest.
References
|
1
|
Gordils-Perez J, Rawlins-Duell R and
Kelvin JF: Advances in radiation treatment of patients with breast
cancer. Clin J Oncol Nurs. 7:629–636. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Landberg T, Chavaudra J, Dobbs J, Gerard
PJ, Hanks G, Horiot JC, Johansson KA, Möller T, Purdy J and
Sunthara-lingam N: ICRU report62 (Supplement to ICRU report
50):International Commission on Radiation Units and Measurements.
ICRU; Bethesda, USA: 1999
|
|
3
|
Early Breast Cancer Trialists'
Collaborative Group (EBCTCG), ; Darby S, McGale P, Correa C, Taylor
C, Arriagada R, Clarke M, Cutter D, Davies C, Ewertz M, et al:
Effect of radiation therapy after breast-consercing surgery on
10-year recurrence and 15-year breast cancer death: Meta-analysis
of individual patient data for 10,801 women in 17 randomised
trials. Lancet. 378:1707–1716. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
De Conno F, Ventafridda V and Saita L:
Skin problems in advanced and terminal cancer patients. J Pain
Symptom Manage. 6:247–256. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Porock D and Kristjanson L: Skin reactions
during radiation therapy for breast cancer: The use and impact of
topical agents and dressings. Eur J Cancer Care (Engl). 8:143–153.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dodd MJ: Managing the side effects of
chemotherapy and radiation therapy2nd. UCSF Nursing Press; San
Francisco, California, USA: 2001
|
|
7
|
US Department of Health and Human
Services, . Common Terminology Criteria for Adverse Events (CTCAE).
V4.03. 2010, https://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03/CTCAE_4.03_2010-06-14_QuickReference_5×7.pdf
|
|
8
|
Fukushi Y, Kitajima M, Itaki C, Noto Y,
Mikami K, Hirota Y, Katto K and Mariya Y: Changes in skin surface
temperature and erythema intensity during and after radiation
therapy for breast cancer patients. Radiat Emerg Med. 3:47–51.
2014.
|
|
9
|
Heinrich U, Koop U, Leneveu-Duchemin MC,
Osterrieder K, Bielfeldt S, Chkarnat C, Degwert J, Häntschel D,
Jaspers S, Nissen HP, et al: Multicentre comparison of skin
hydration in terms of physical-, physiological- and
product-dependent parameters by the capacitance method (Corneometer
CM 825). Int J Cosmet Sci. 25:45–53. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Park ES, Na JI, Kim SO, Huh CH, Youn SW
and Park KC: Application of a pigment measuring
device-Mexameter-for the differential diagnosis of vitiligo and
nevus depigmentosus. Skin Res Technol. 2:298–302. 2006. View Article : Google Scholar
|
|
11
|
Tamai Y, Tsuji M, Wada K, Nakamura K,
Hayashi M, Takeda N, Yasuda K and Nagata C: Association of
cigarette smoking with skin colour in Japanese women. Tob Control.
23:253–256. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nagata C, Konish K, Tamura T, Wada K,
Hayashi M, Takeda N and Yasuda K: Skin pigmentation is inversely
associated with insulin resistance in healthy Japanese women.
Diabetes Metab. 42:368–371. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Eaton L and Tipton J: Putting evidence
into practice: Improving oncology patient outcomes1st. Oncol Nurs
Society; Pittsburgh, PA, USA: 2009
|
|
14
|
Blackmar A: Radiation-induced skin
alteration. Medsurg Nurs. 6:172–175. 1997.PubMed/NCBI
|
|
15
|
Knopf MT and Sun Y: A longitudinal study
of symptoms and self-care activities in women treated with primary
radiation therapy for breast cancer. Cancer Nurs. 28:210–218.
2005.PubMed/NCBI
|
|
16
|
Tanaka E, Yamazaki H, Yoshida K, Takenaka
T, Masuda N, Kotsuma T, Yoshioka Y and Inoue T: Objective and
longitudinal assessment of dermatitis after postoperative
accelerated partial breast irradiation using high-dose-rate
interstitial brachytherapy in patients with breast cancer treated
with breast-conserving therapy: Reduction of moisture deterioration
by APBI. Int J Radiat Oncol Biol Phys. 81:1098–1104. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sekiguchi K, Ogita M, Akahane K, Haga C,
Ito R, Arai S, Ishida Y, Tsukada Y and Kawamori J: Randomized,
prospective assessment of moisturizer efficacy for the treatment of
radiation dermatitis following radiotherapy after breast-conserving
surgery. Jpn J Clin Oncol. 45:1146–1153. 2015.PubMed/NCBI
|
|
18
|
Vicini FA, Beitsch PD, Quiet CA, Keleher
A, Garcia D, Snider HC, Gittleman MA, Zannis VJ, Kuerer H, Whitacre
EB, et al: First analysis of patient demographics, technical
reproducibility, cosmesis, and early toxicity: Results of the
American society of breast surgeouns mammosite breast brachytherapy
trial. Cancer. 104:1138–1148. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Whelan JT, Levine M, Julian J, Kirkbride P
and Skingley P: The effects of radiation therapy on quality of life
of women with breast carcinoma: Results of a randomized trial.
Ontario Clinical Oncology Group. Cancer. 88:2260–2266. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Partl R, Lehner J, Winkler P and Kapp KS:
Testing the feasibility of augmented digital skin imaging to
objectively compare the efficacy of topical treatments for
radiodermatitis. PLoS One. 14:e02180182019. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Fuzissaki MA, Paiva CE, Gozzo TO, Maia MA,
Canto PPL and Maia YCP: Is there agreement between evaluators that
used two scoring systems to measure acute radiation dermatitis?
Medicine (Baltimore). 98:e149172019. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Sehlen S, Hollenhorst H, Schymura B,
Herschbach P, Aydemir U, Firsching M and Dühmke E: Psychosocial
stress in cancer patients during and after radiotherapy.
Strahlenther Onkol. 179:175–180. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Soh SJ, Schnur JB, Sucala M, David D,
Winkel G and Montgomery GH: Distress and emotional well-being in
breast cancer patients prior to radiotherapy: An expectancy-based
model. Psychol Health. 27:347–361. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lester J, Crosthwaite K, Stout R, Jones
NR, Holloman C, Shapiro C and Andersen LB: Women with breast
cancer: Self-reported distress in early survivorship. Oncol Nurs
Forum. 42:E17–E23. 2015. View Article : Google Scholar : PubMed/NCBI
|