Introduction
Primary sarcomas of the mediastinum have been
reported to be rare, and leiomyosarcomas account for approximately
9% of the mediastinal sarcomas (1).
A leiomyosarcoma is an aggressive malignant tumor that originates
in the mesenchymal tissue (2).
Mediastinal leiomyosarcomas mostly occur in mediastinal organs,
such as the heart, great vessels, and esophagus, usually
manifesting as posterior mediastinal tumors, and rarely as anterior
mediastinal tumors (3). Only few
cases of anterior mediastinal leiomyosarcomas have been reported to
date (3). Here we report an
extremely rare case of an anterior mediastinal leiomyosarcoma that
was considered to have originated from a bronchogenic cyst.
Case report
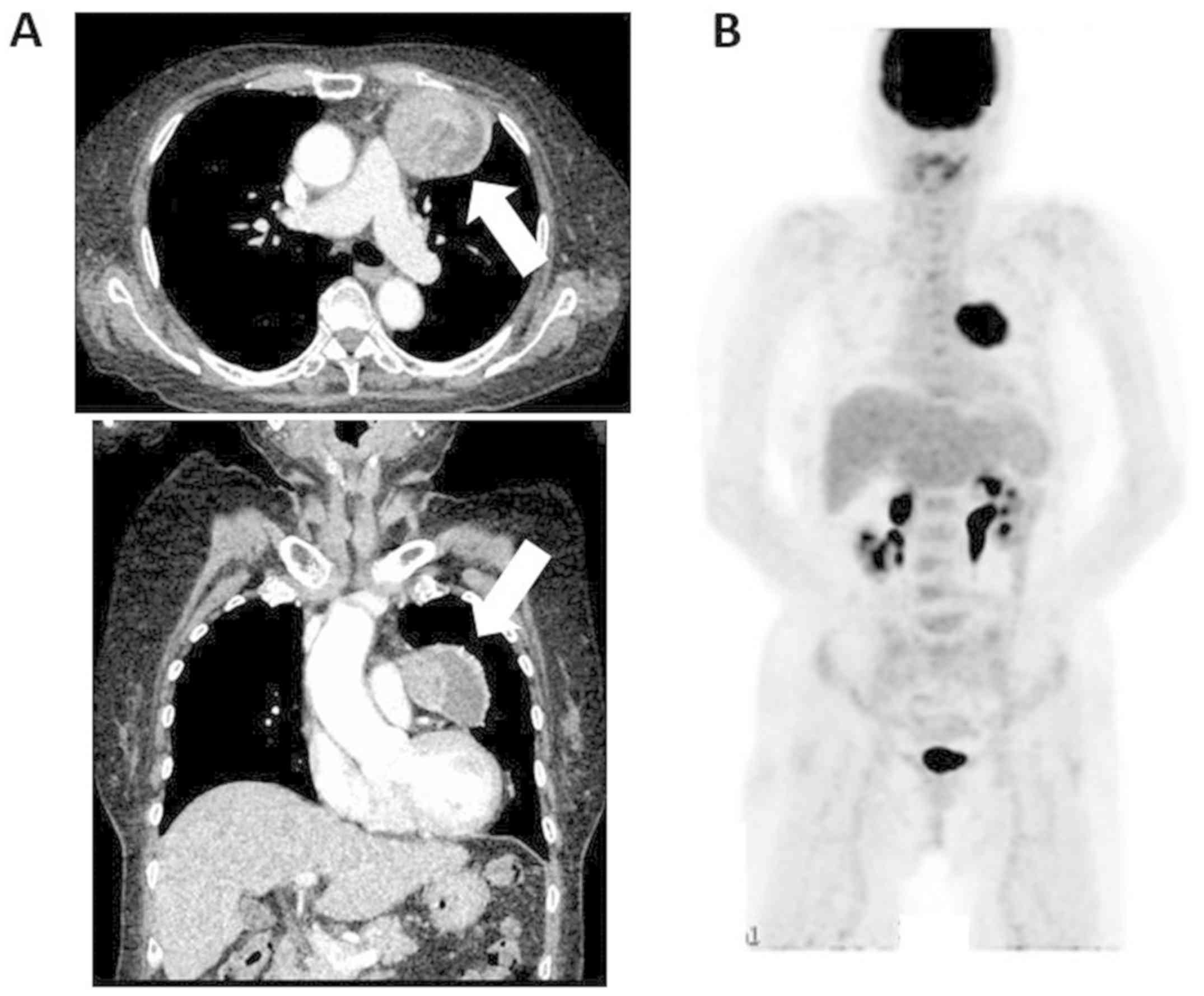
An 82-year-old woman with a medical history of
hypertension presented to us with chest pain. Her chest radiograph
revealed a giant mass in the left lung field, and chest CT scan
revealed a 70-mm mass in the anterior mediastinum (Fig. 1A). Positron emission tomography-CT
scan revealed strong fluorodeoxyglucose accumulation in the tumor
(maximum standardized uptake value, 10.9), and no other lesion was
detected (Fig. 1B). A needle biopsy
of the tumor was not performed owing to the possibility of tumor
implantation. Mediastinal tumor resection was performed via the
median sternotomy approach. The tumor adhered to the aorta,
pericardium, and left upper lung. As tumor infiltration of the left
upper lung was suspected, a part of the left upper lobe and the
thymus was resected along with the tumor. The operation time was
233 min, and bleeding was 325 ml. The postoperative course was
uneventful, and the patient was discharged 15 days postoperatively.
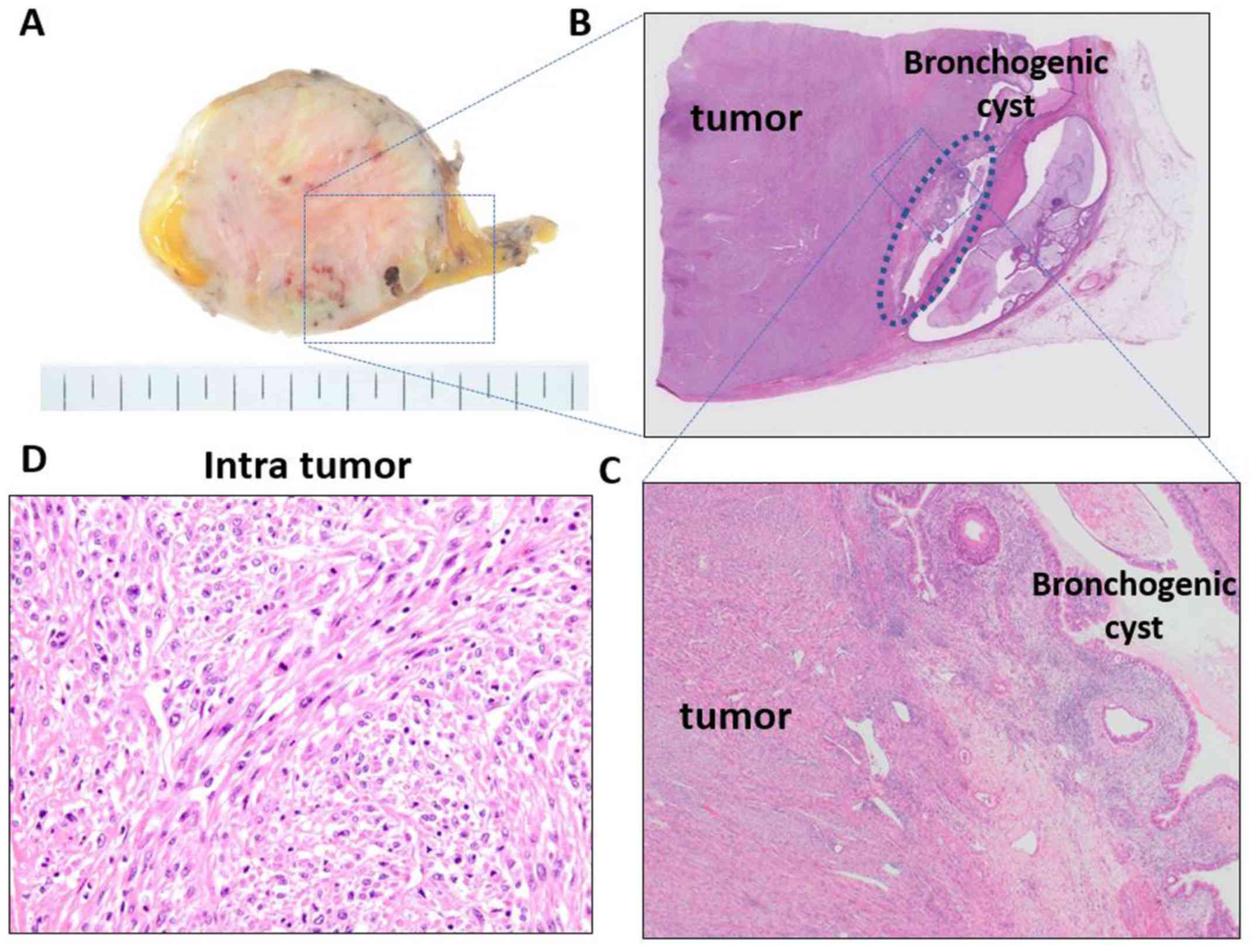
Pathological examination showed that the tumor was firm,
white-to-yellowish in color, and 65 mm in size; furthermore, it,
had a well-demarcated and fibrous capsule (Fig. 2A-C). A cystic cleft was observed in
the tumor periphery. Histologically, the tumor comprised
eosinophilic spindle cell bundles with focal necrosis and exhibited
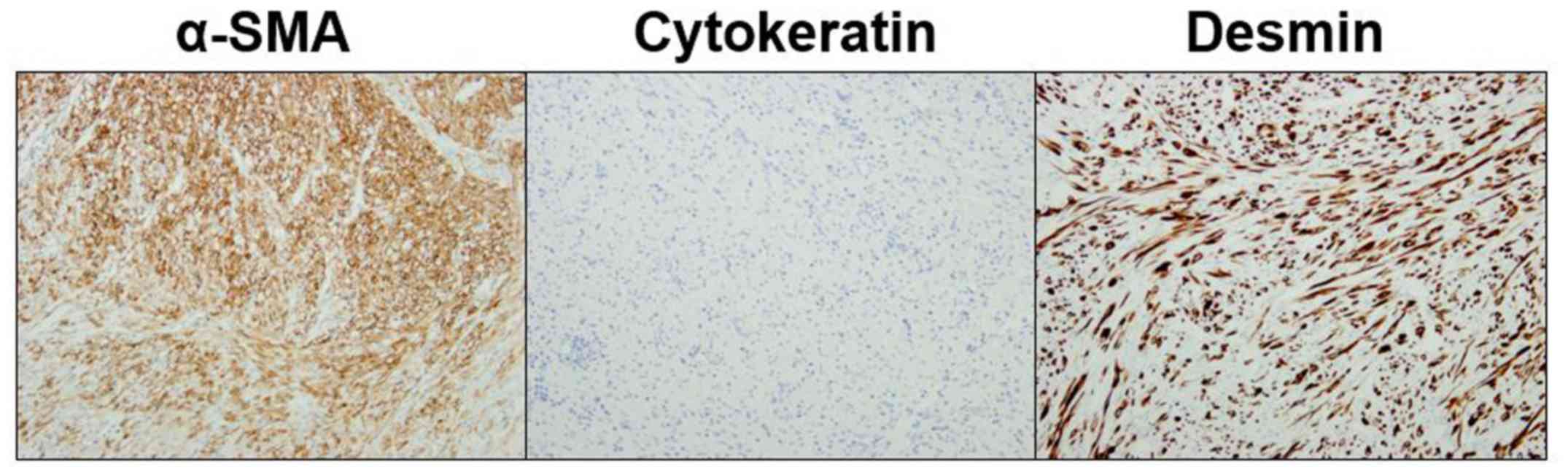
increased mitotic activity (three/high-power field) (Fig. 2D). On immunohistochemical staining,
the tumor was positive for alpha smooth muscle actin and desmin,
and negative for cytokeratin, S-100 protein, AE1/3, Cam5.2, and
CD34 (Fig. 3). Based on these
findings, the tumor was finally diagnosed as a leiomyosarcoma.
Leiomyosarcomas, which are present as anterior mediastinal tumors,
are extremely rare. The tumor was located adjacent to the cyst
wall, which was covered with ciliated columnar epithelium (Fig. 2A-C); therefore, the tumor was
suspected to have originated from the remnant tissue of the
bronchogenic cyst. The patient's chest pain disappeared after the
surgery. Recurrent lesions were noted in the right lower lobe on a
CT scan performed 24 months after the surgery. Because the
effectiveness of radiation and chemotherapy for leiomyosarcoma
remained unclear, aggressive treatments were thought to be
difficult considering her age; she now receives best supportive
care.
Discussion
We experienced a rare case of a leiomyosarcoma that
originated from the wall of a bronchogenic cyst. So far, less than
40 cases of mediastinal leiomyosarcomas have been reported, with
most of them occurred in the posterior mediastinum (2). Leiomyosarcomas presenting as anterior
mediastinal tumors are extremely rare. Mediastinal leiomyosarcomas
seem to originate from major vessels in some cases; however, the
actual site of origin is often unclear (2). In this case, there was no tissue
connection between the tumor and the wall of major vessels.
Bernheim et al (4) have
reported a case of an anterior mediastinal leiomyosarcoma that was
suspected to have originated from the wall of a bronchogenic cyst,
similar to our case. A bronchogenic cyst is a benign lesion that
often occurs in the mediastinum close to the thoracic trachea, and
it has been reported to be the origin of certain malignancies
(5). To our knowledge, this is the
second case report to show the simultaneous development of a
bronchogenic cyst and an anterior mediastinal leiomyosarcoma.
Mediastinal leiomyosarcomas are aggressive, and
local recurrence and distant metastasis have been reported to occur
in a large number of patients (2).
Patients with mediastinal leiomyosarcomas present with symptoms
(such as cough, dyspnea, chest pain, fever) because of the local
mass effect (6). The principal
treatment for a leiomyosarcoma is complete surgical resection; the
effectiveness of chemotherapy and radiotherapy remains unclear
(1). The most common site of
metastasis has been reported to be the lung, followed by the liver
and skin (7). Recurrence is more
frequent within 2-3 years of diagnosis, and the 5-year survival
rate after complete resection has been reported to be 15-20%
(8). The risk factors for poor
prognosis of leiomyosarcoma are old age and large tumor size
(7). The present patient had both
these risk factors; hence, she was considered a high-risk patient
with regard to survival.
We described the case of an elderly woman with an
anterior mediastinal leiomyosarcoma. The tumor was suspected to
originate from the remnant tissue of a bronchogenic cyst. The
findings of the present case might help in the assessment and
treatment of patients with a leiomyosarcoma in the anterior
mediastinum.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during the present
study are included in this published article.
Authors' contributions
KK and HO collaborated in the conception of the
present study. NJ prepared the pictures presented in the figures.
YM, DH, NJ and YT critically revised the manuscript and were
involved in data interpretation. All authors contributed to writing
the manuscript and approved the final version.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient prior to enrollment.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of all accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Burt M, Ihde JK, Hajdu SI, Smith JW, Bains
MS, Downey R, Martini N, Rusch VW and Ginsberg RJ: Primary sarcomas
of the mediastinum: Results of therapy. J Thorac Cardiovasc Surg.
115:671–680. 1998.PubMed/NCBI View Article : Google Scholar
|
|
2
|
den Bakker MA, Marx A, Mukai K and Ströbel
P: Mesenchymal tumours of the mediastinum-part II. Virchows Arch.
467:501–517. 2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Xue X, Liang W and Zhang W: Anterior
mediastinal leiomyosarcoma mimicking thymoma: A case report.
Medicine (Baltimore). 97(e11132)2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Bernheim J, Griffel B, Versano S and
Bruderman I: Mediastinal leiomyosarcoma in the wall of a bronchial
cyst. Arch Pathol Lab Med. 104(221)1980.PubMed/NCBI
|
|
5
|
Sullivan SM, Okada S, Kudo M and Ebihara
Y: A retroperitoneal bronchogenic cyst with malignant change.
Pathol Int. 49:338–341. 1999.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Gladish GW, Sabloff BM, Munden RF, Truong
MT, Erasmus JJ and Chasen MH: Primary thoracic sarcomas.
Radiographics. 22:621–637. 2002.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Farshid G, Pradhan M, Goldblum J and Weiss
SW: Leiomyosarcoma of somatic soft tissues: A tumor of vascular
origin with multivariate analysis of outcome in 42 cases. Am J Surg
Pathol. 26:14–24. 2002.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Moran CA, Suster S, Perino G, Kaneko M and
Koss MN: Malignant smooth muscle tumors presenting as mediastinal
soft tissue masses. A clinicopathologic study of 10 cases. Cancer.
74:2251–2260. 1994.PubMed/NCBI View Article : Google Scholar
|