Introduction
Pulmonary sclerosing hemangioma (PSH) is an uncommon
benign tumor of the lungs, first reported by Liebow and Hubbell in
1956(1). Its origin has been
suggested to be vascular, mesothelial, mesenchymal, epithelial and
neuroendocrine (1-5),
but immunohistochemical examination suggests that PSH is derived
from primitive respiratory epithelium. It primarily affects Asian
women and the female: Male ratio is 5:1 (6,7). PSH
predominantly presents as a solitary, sharply defined slow-growing
mass, although it may present as multiple lesions (8). On imaging, PSH appears as a mass with
distinct margins, and the majority of the patients are
asymptomatic. Definitive diagnosis requires resection and
postoperative histopathological examination. Due to its atypical
image presentations, PSH may be easily misdiagnosed as a malignant
tumor prior to surgery, with a misdiagnosis rate that ranges from
25 to 56% (8). We herein report a
case of PSH and perform a review of the literature to explore the
clinical management of PSH.
Case report
A 23-year-old unmarried woman was hospitalized after
a mass was incidentally found in her right lung during routine
physical examination. The patient had a history of allergic
reaction to penicillin and cephalosporin. The patient was in good
general health and had no unhealthy habits, such as drug or alcohol
abuse or smoking. The patient's personal, menstrual and family
history were unremarkable.
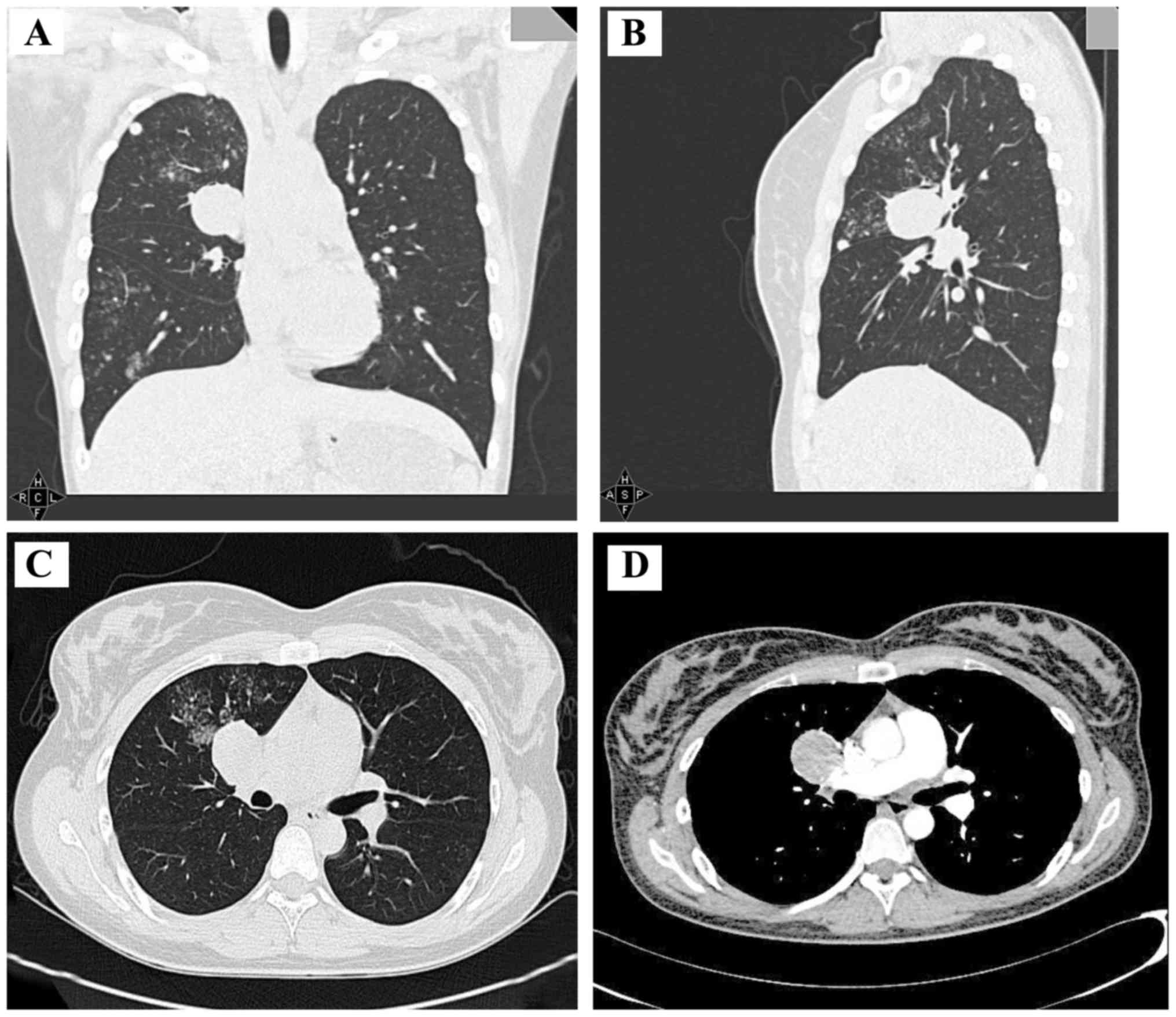
The chest computed tomography (CT) of the patient
revealed several shadows in the right lung during a physical
examination in October 2014. The patient visited Qingdao Chest
Hospital (Qingdao, China) for further evaluation and the
γ-interferon release testing was found to be positive. The patient
was diagnosed with tuberculosis and was started on antituberculosis
treatment with rifampicin, armazide, ethambutol and pyrazinamide.
The patient started to experience intermittent fevers over the next
2 months of antituberculosis treatment, with the highest
temperature reaching 39˚C, usually improving at night and relieved
by ibuprofen. Interestingly, the patient had no history of cough,
expectoration, dyspnea, chest pain, palpitations or weight loss.
The patient underwent regular chest CT re-examinations during the
antituberculosis treatment, which revealed no changes in the
lesions. The patient accepted CT examination again in March 2015
and no obvious changes were evident in the images of the right
lung. Percutaneous lung biopsy was performed, and histopathological
examination revealed inflammatory and hyperplastic changes. Most
importantly, the antituberculosis treatment was continued based on
the results of postoperative pathology.
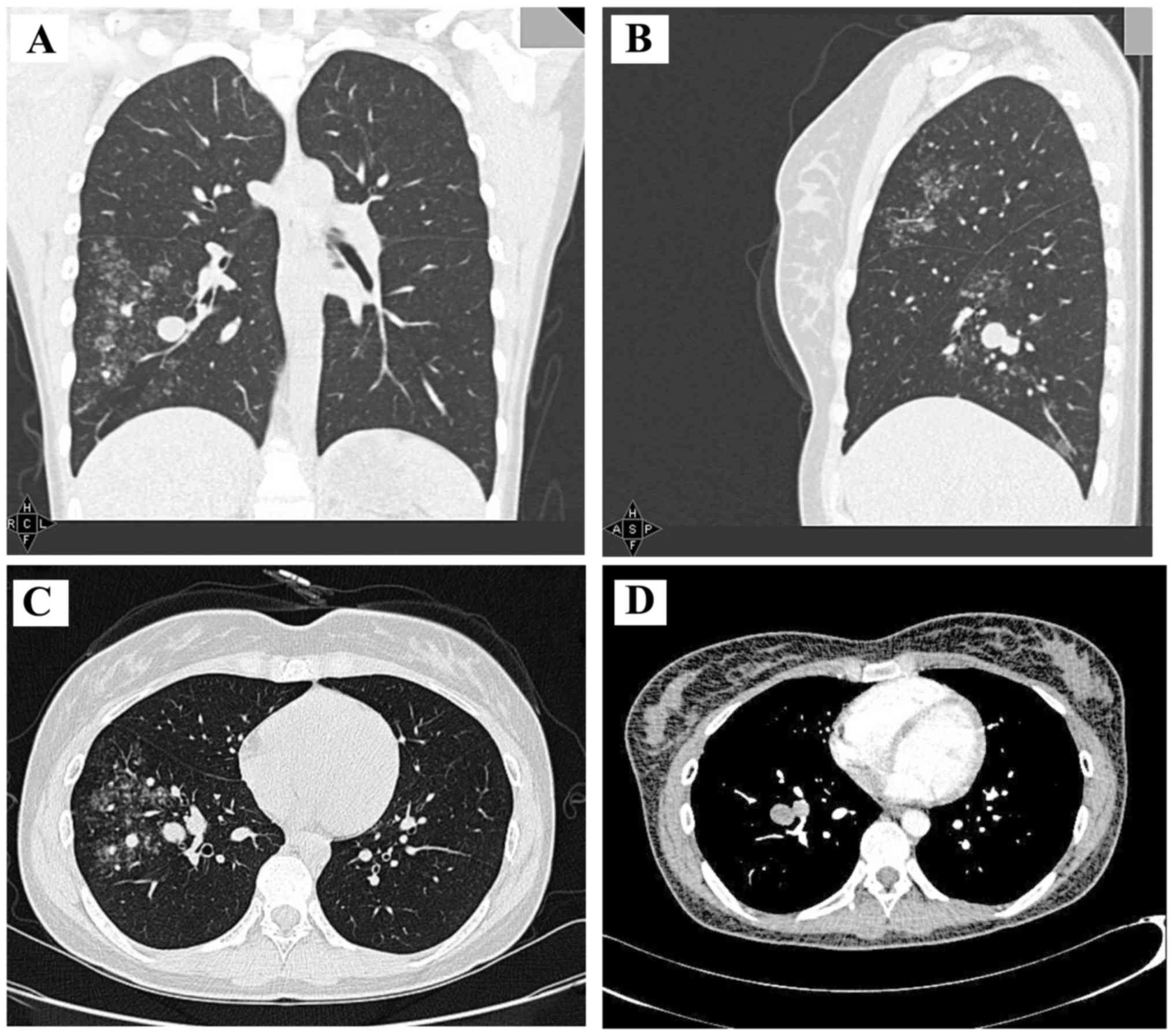
The patient first visited Chengdu Military General
Hospital (Chengdu, China) at the end of September 2015, and a CT
scan revealed a circular mass of soft tissue density in the right
upper pulmonary hilum. In addition, the right lung exhibited
scattered dot films and small nodules, consistent with the imaging
findings of pulmonary tuberculosis. Admission was recommended for
further evaluation, but the patient declined due to work
responsibilities. Antituberculosis treatment was continued on an
outpatient basis and further chest CT scans were performed in June
2016, April 2017 and August 2017. The CT scan performed in August
2017 revealed an increased number of dot films and small nodules in
the right lung, with the additional appearance of flakes of blurry
shadows (Figs. 1 and 2). The patient was then admitted to the
hospital and further examinations were undertaken.
The physical examination of the patient was normal.
The findings on routine blood and urine tests and bronchoscopy were
normal, apart from the results of the γ-interferon release testing.
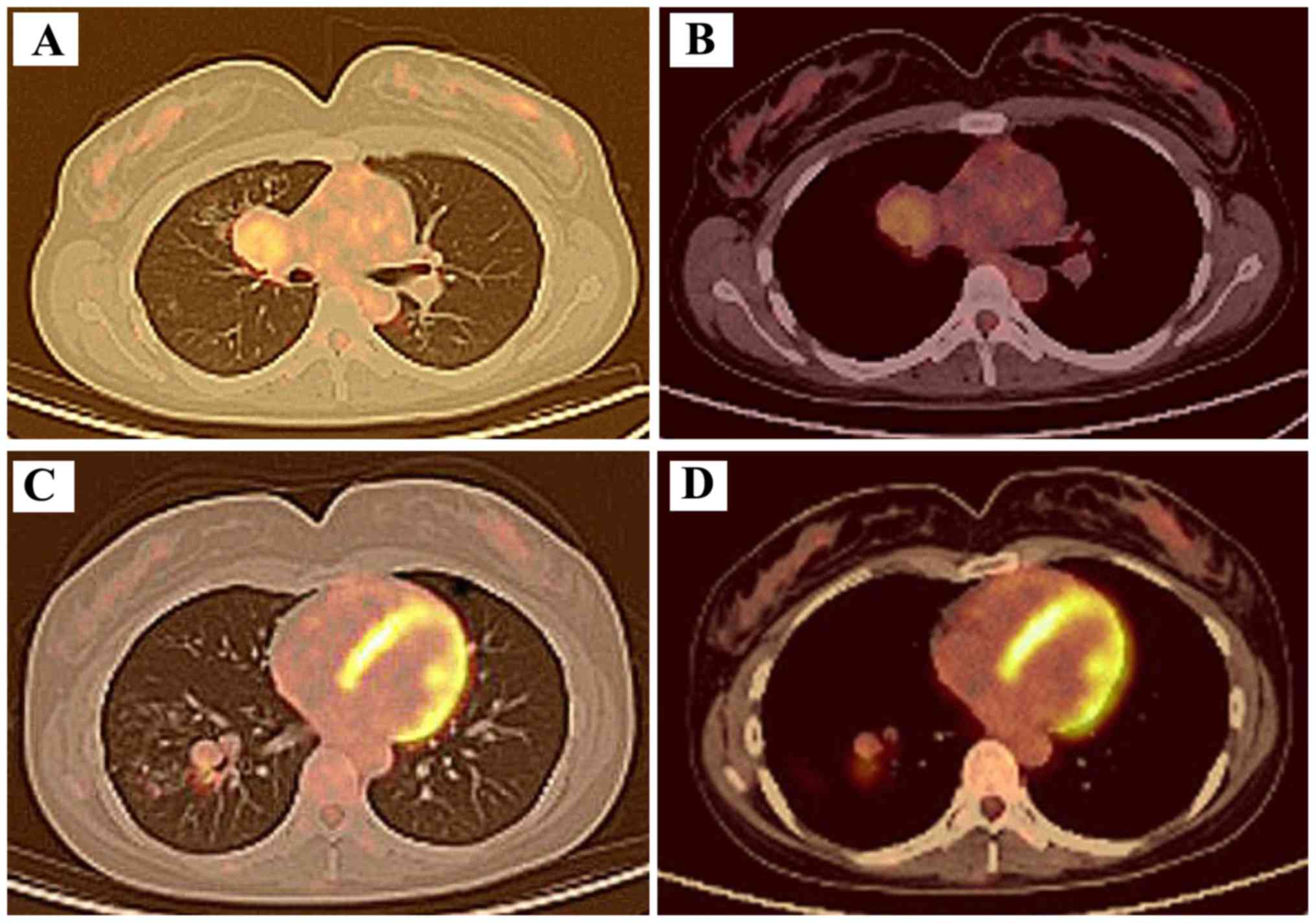
In order to reach a definitive diagnosis, positron emission
tomography (PET)-CT was performed (Fig.
3), revealing the presence of multiple nodules of varying sizes
and densities. Furthermore, increased fluorodeoxyglucose uptake was
observed in some of the nodules with calcification. As tuberculosis
recurrence was first suspected, the patient underwent thoracoscopic
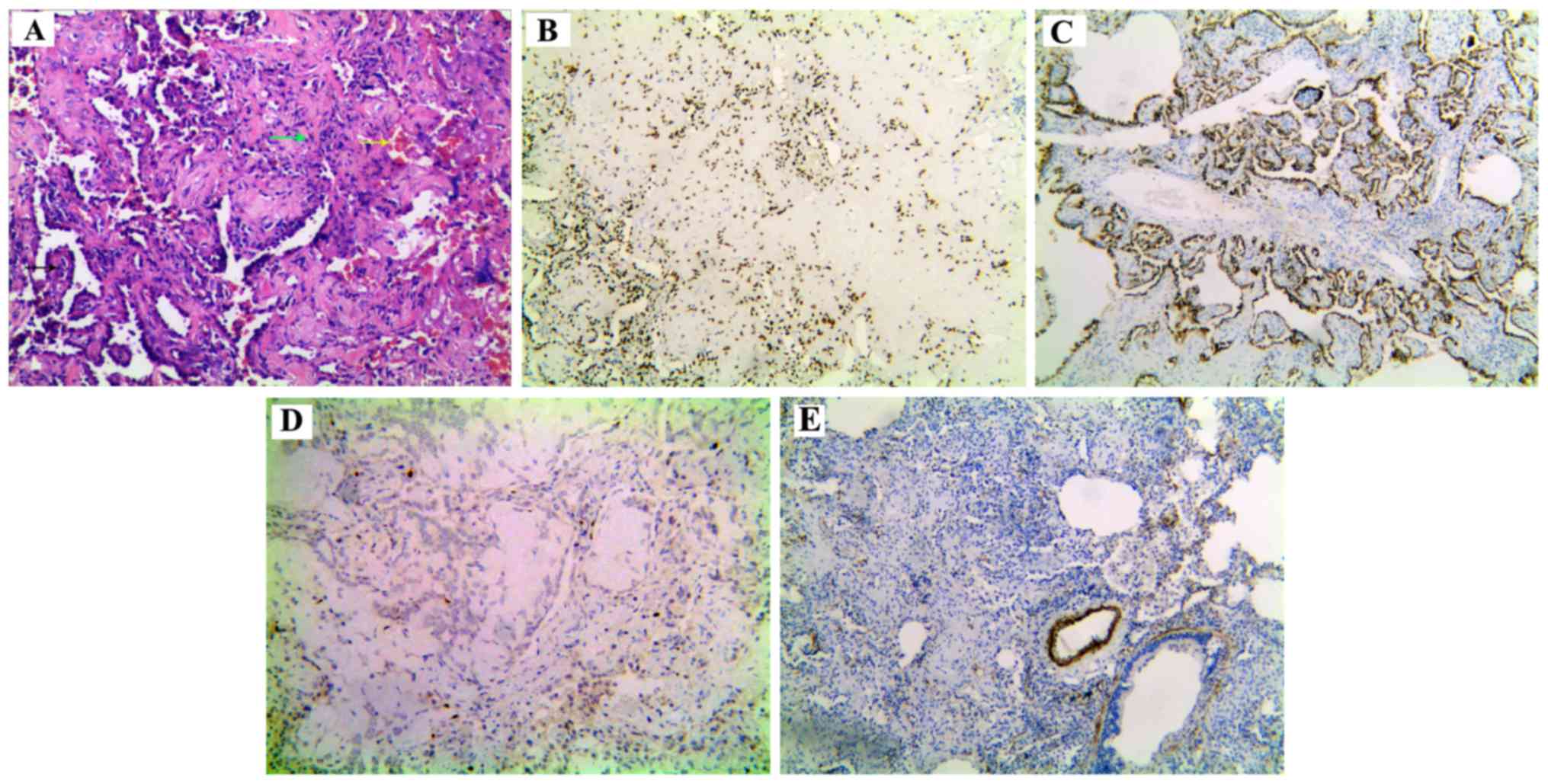
surgery with right lung nodulectomy. Based on the postoperative
pathological examination of the nodules, the lesions were diagnosed
as multiple PSH, and four different histological patterns were
identified: Papillary, solid, sclerotic and hemorrhagic (Fig. 4A). Immunohistochemical evaluation of
the lesions revealed positive staining for thyroid transcription
factor (TTF)1 (Fig. 4B) and
cytokeratin (CK) 8/18 (Fig. 4C), but
negative staining for smooth muscle actin (Fig. 4E). The Ki-67 labeling index was 1%.
(Fig. 4D).
All examinations and medical procedures were
approved by the patient and her family.
Discussion
PSH is a benign tumor of the lungs with variable
histological characteristics. PSH was originally considered to be
of vascular origin due to the obvious characteristics of
hemangioma. After the first description in 1956 by Liebow and
Hubbel (1), several theories
regarding its origin were introduced, including vascular (1), mesothelial (2), mesenchymal (3), epithelial (4) and neuroendocrine (5). Currently, the results of the
immunohistochemical examination suggest that PSH is derived from
primitive respiratory epithelium. PSH has been reported to be more
prevalent in East Asian rather than in Western countries, and
typically affects middle-aged adults and exhibits a female
predominance, with women comprising ~80% of PSH patients (6,7). In the
majority of the cases (~95%), PSH presents as a solitary
slow-growing mass located in the peripheral lung parenchyma, except
for 4% of the cases that present as multiple lesions (8). The tumor size may vary from 0.3 to 8 cm
in greatest diameter, but the majority measure <3 cm. PSH is
almost always benign, with only 4% of PSHs invading the visceral
pleura and only 1% growing into the mediastinum or the bronchial
cavity. The right lung, particularly the lower lobe, has been
reported to be most commonly affected by PSH. The findings on CT
scans include a mass with distinct margins and increased density on
contrast-enhanced CT. The majority (80%) of PSHs are asymptomatic
or present with cough, hemoptysis and, occasionally, chest
pain.
Histologically, PSH includes two essential types of
tumor cells: Round stromal cells and surface cuboidal cells. Round
stromal cells with absent or rare clear nucleoli are small and
well-circumscribed. However, the surface cuboidal cells lining
papillary structures exhibit characteristics of bronchiolar
epithelium and type II pneumocytes. These cells may display
different degrees of nuclear heterogeneity. Therefore, they may be
arranged into four different histological patterns: Papillary,
solid, sclerotic and hemorrhagic. In the present case, although the
immunohistochemical examination revealed that the two cell types
were positive for TTF-1 and epithelial membrane antigen, the
expression of pancytokeratin A and various CKs were different in
the two cell types, as pancytokeratin A and CK staining was only
observed in the surface cells of the mass. Molecular studies
confirmed that both cell types were clonal in nature, demonstrating
that PSH is a true neoplasm.
The origin and progression of PSH remain
controversial. The current consensus is that primary papillary
alveolar epithelial cells proliferate and cover the fibrous tissue
of the alveolar wall. At this stage, the epithelial cells may be
atypical, but not malignant. Subsequently, sclerosis of
interstitial alveolar cells is aggravated, leading to implantation
of capillaries. As a consequence, hemorrhage occurs in the residual
alveolar cavity, causing a hemosiderin reaction or accumulation of
vacuolar macrophages and alveolar destruction.
Our patient had no obvious causes or positive
symptoms in the early stages of the disease. Several shadows were
located in the right pulmonary hilum, and the right lower lung was
surrounded by inflammatory exudations that were consistent with the
critical changes of pulmonary tuberculosis. Antituberculosis
therapy was recommended by the first attending physician, as well
as by other consultants thereafter, based on the consideration that
China is a region of high incidence of tuberculosis. The patient
was positive for whole-blood γ-interferon release assay. After
ruling out malignant tumors, common bacteria in the region, and
infection by atypical pathogens, tuberculosis remained the most
likely diagnosis. The patient also developed high fevers in the
afternoon, which was consistent with the typical symptoms of
tuberculosis. More importantly, the high fever disappeared after
antituberculosis treatment, suggesting treatment efficacy. However,
the pulmonary lesions increased after 6 months of treatment and the
biopsy results indicated inflammatory changes in the lungs.
Antituberculosis therapy was continued, as the patient reported no
feeling of discomfort and the duration of antituberculosis therapy
was deemed insufficient. Unfortunately, the CT scan performed in
August 2017 revealed that the pulmonary lesions had increased after
the patient completed a 1-year course of antituberculosis
treatment. In addition, the PET-CT results indicated recrudescence
of tuberculosis. The clinical manifestations of the patient were
carefully analyzed and it was concluded that the diagnosis of
tuberculosis could not fully explain the patient's condition and
all the imaging findings. Thoracoscopic surgery and right lung
nodulectomy were performed in order to pathologically diagnose the
patient. Surgical excision is considered the best choice for single
PSH, while long-term follow-up is required to determine the
prognosis of multiple PSHs.
In conclusion, we herein present a rare case of PSH
with symptoms of discontinuous fever and multiple pulmonary nodules
that was misdiagnosed as tuberculosis in its initial stages.
Following adequate antituberculosis therapy, the lesions progressed
but the patient remained asymptomatic. Although bronchoscopy and
lung biopsy through percutaneous paracentesis were performed, there
were no positive results. Finally, thoracoscopy and
immunohistochemical examination were used to reach a definitive
diagnosis. In the literature, surgical resection is the preferred
treatment for solitary PSH; however, for multiple PSHs, continuous
follow-up and observation are crucial, as there is yet no effective
treatment. Although rare, PSH should be considered when the
suspected diagnosis contradicts the symptoms and results of
auxiliary examinations. Therefore, physicians must remain highly
vigilant in such cases to reach an accurate diagnosis and deliver
effective treatment.
Acknowledgements
The authors would like to thank colleagues from the
Imaging, Pathology, Laboratory and Thoracic Surgery Departments of
General Hospital of Western Theater Command for help in diagnosing
the patient.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
HL was the patient's doctor. LM analyzed the data
and wrote the article together with HL and TZ. YC was pathologist
and confirmed the pathological diagnosis. DP, ZL and XD helped
during the treatment and collected data. ZX and ZC directed the
treatment of the patient, collection of data and writing of the
article.
Ethics approval and consent to
participate
All examinations and medical procedures were
approved by the patient and her family.
Patient consent for publication
The patient agreed for the case study to be
published.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Liebow AA and Hubbell DS: Sclerosing
hemangioma (histiocytoma, xanthoma) of the lung. Cancer. 9:53–75.
1956.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ng WL and Ma L: Is sclerosing hemangioma
of lung an alveolar mixed tumour? Pathology. 15:205–211.
1983.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Huszar M, Suster S, Herczeg E and Geiger
B: Sclerosing hemangioma of the lung. Immunohistochemical
demonstration of mesenchymal origin using antibodies to
tissue-specific intermediate filaments. Cancer. 58:2422–2427.
1986.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Satoh Y, Tsuchiya E, Weng SY, Kitagawa T,
Matsubara T, Nakagawa K, Kinoshita I and Sugano H: Pulmonary
sclerosing hemangioma of the lung. A type II pneumocytoma by
immunohistochemical and immunoelectron microscopic studies. Cancer.
64:1310–1317. 1989.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Xu HM, Li WH, Hou N, Zhang SG, Li HF, Wang
SQ, Yu ZY, Li ZJ, Zeng MY and Zhu GM: Neuroendocrine
differentiation in 32 cases of so-called sclerosing hemangioma of
the lung: Identified by immunohistochemical and ultrastructural
study. Am J Surg Pathol. 21:1013–1022. 1997.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Katzenstein AL, Weise DL, Fulling K and
Battifora H: So-called sclerosing hemangioma of the lung. Evidence
for mesothelial origin. Am J Surg Pathol. 7:3–14. 1983.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Devouassoux-Shisheboran M, Hayashi T,
Linnoila RI, Koss MN and Travis WD: A clinicopathologic study of
100 cases of pulmonary sclerosing hemangioma with
immunohistochemical studies: TTF-1 is expressed in both round and
surface cells, suggesting an origin from primitive respiratory
epithelium. Am J Surg Pathol. 24:906–916. 2000.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Lee ST, Lee YC, Hsu CY and Lin CC:
Bilateral multiple sclerosing hemangiomas of the lung. Chest.
101:572–573. 1992.PubMed/NCBI View Article : Google Scholar
|