Introduction
Paget's disease has been classified as mammary and
extramammary. Mammary Paget's disease is an adenocarcinoma
originating mainly in the mammary duct and characterized by
eczematous erosion. Extramammary Paget's disease is a rare
condition typically presenting as a reddish patch and/or nodule and
is commonly found in the vulvar area, followed by the perianal
area, scrotum, penis and axillae. Perianal Paget's disease, defined
as intraepithelial adenocarcinoma of the perianal skin (1,2) is a
rare condition. There are two types of perianal Paget's disease:
Primary and secondary. When an underlying adenocarcinoma is
present, perianal Paget's disease usually represents intraepidermal
extension of an invasive carcinoma from an adjacent internal organ
and generally regarded as secondary.
During the early years of this century, preoperative
chemoradiotherapy (CRT) and total mesorectal excision were reported
to remarkably reduce rates of local recurrence and this approach
facilitates tumor downstaging, increases sphincter preservation and
CRT plus total mesorectal excision has gained acceptance as the
gold standard for surgical treatment of rectal cancer. In our
department, we performed preoperative CRT in patients with advanced
carcinoma of the lower rectum. But in perianal Paget's disease the
role of preoperative CRT is presently unclear because of the rarity
of the disease.
Here, we report a case of anal canal cancer with
pagetoid spread and inguinal lymph node metastasis, which showed a
significant response to preoperative CRT and discuss on the
clinical and pathological findings.
Case report
A 58-year-old woman was admitted to University of
Tokyo Hospital (Tokyo, Japan) complaining of discomfort around her
anus. She had no history of abdominal or anal surgery, no family
history of malignancy, no change in bowel habits, and no
gastrointestinal symptoms. Laboratory data revealed elevation of
carcinoembryonic antigen (CEA) (13.2 ng/ml), and anti-P53 antibody
(105 U/ml), but not carbohydrate antigen 19-9 (CA19-9) (1 U/ml) nor
SCC (3.0 ng/ml). The patient had normal renal and liver functions
and a normal hemoglobin level.
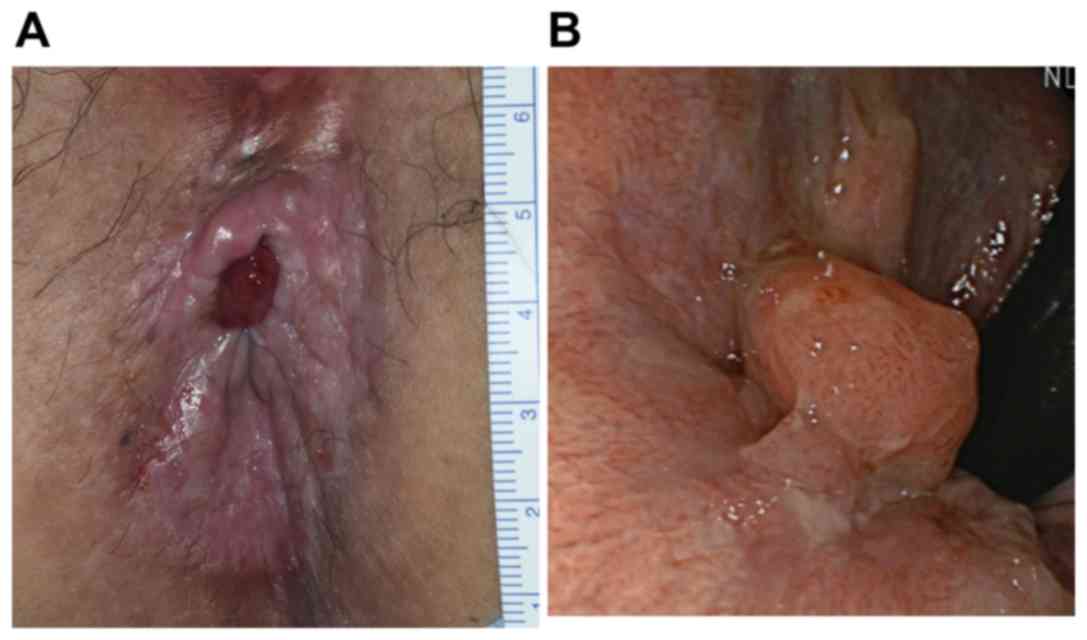
Physical examination of the patient revealed an
erythematous inflamed skin lesion in the perianal region (Fig. 1A) and a tumor of 15 mm in diameter
detected on palpation in the left inguinal region. Digital
examination and colonoscopy revealed a tumor of 15 mm in diameter
in the left posterior wall of the anal canal located just on the
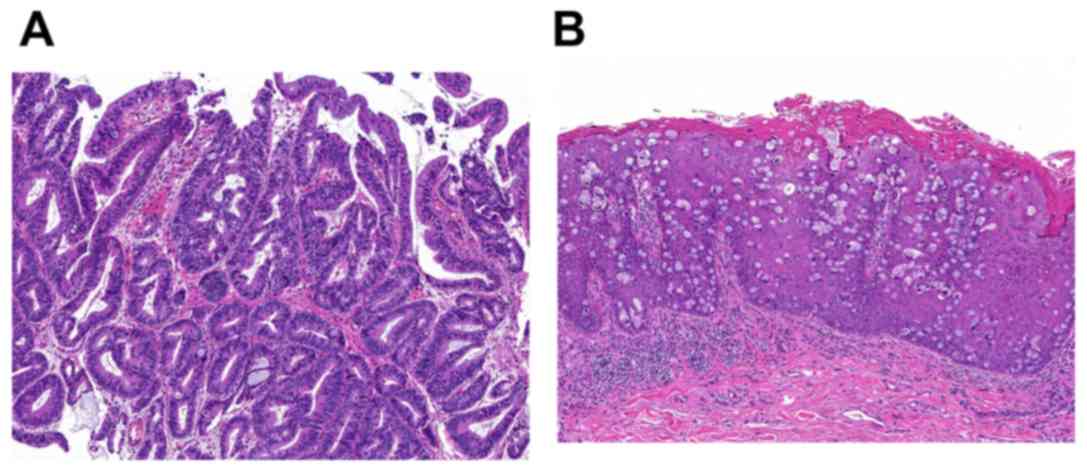
dentate line (Fig. 1B). Tumor biopsy
of anal canal revealed moderately differentiated adenocarcinoma
cells (Fig. 2A). Skin biopsy
revealed an epidermal infiltration of pagetoid cells, characterized
by abundant cytoplasmic mucin showing signet ring cell morphology
(Fig. 2B), which were positive for
cytokeratin 7 (CK7) and Caudal-type homebox transcription factor 2
(CDX2), and negative for cytokeratin 20 (CK20) and Gross cystic
disease fluid protein 15 (GCDFP15).
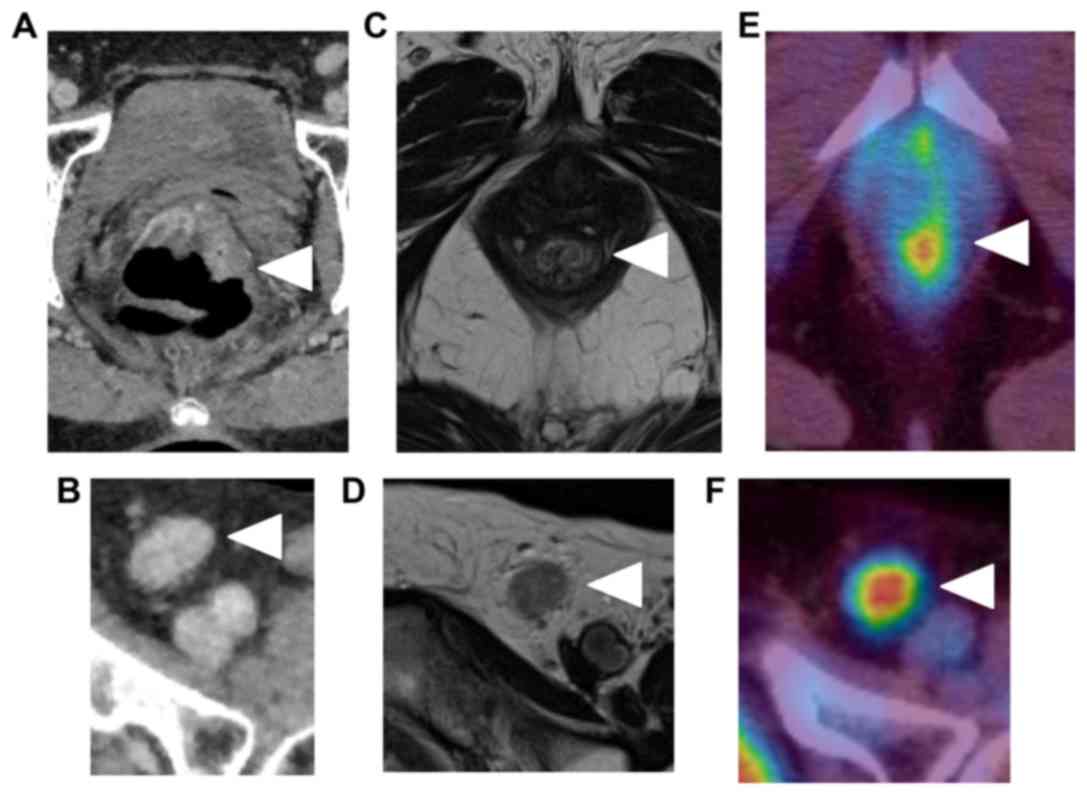
Abdominal computed tomography (CT) showed thickness
of the wall of the lower rectum (Fig.
3A) and a left inguinal lymph node of 15 mm diameter (Fig. 3B). Magnetic resonance imaging (MRI)
confirmed thickness of the lower rectum without evident invasion
into the muscular propria (depth: T1) (Fig. 3C), and a left inguinal lymph node of
15 mm diameter (Fig. 3D). Positron
emission tomography (PET) revealed lower rectum tumor (Fig. 3E) and a left inguinal lymph node
(Fig. 3F).
Excisional biopsy of the left inguinal lymph node,
performed for the staging of the tumor, revealed metastatic
involvement of the left inguinal lymph node (adenocarcinoma).
Taking the results of resection of left inguinal lymph node, the
patient was diagnosed as anal canal cancer with lymph node
metastasis. So preoperative CRT (oral tegafur-uracil 300 mg/day and
leucovorin 75 mg/day, 1.8 Gy x28 fr, a total dose of 50.4 Gy)
including bilateral inguinal region to improve local control was
indicated.
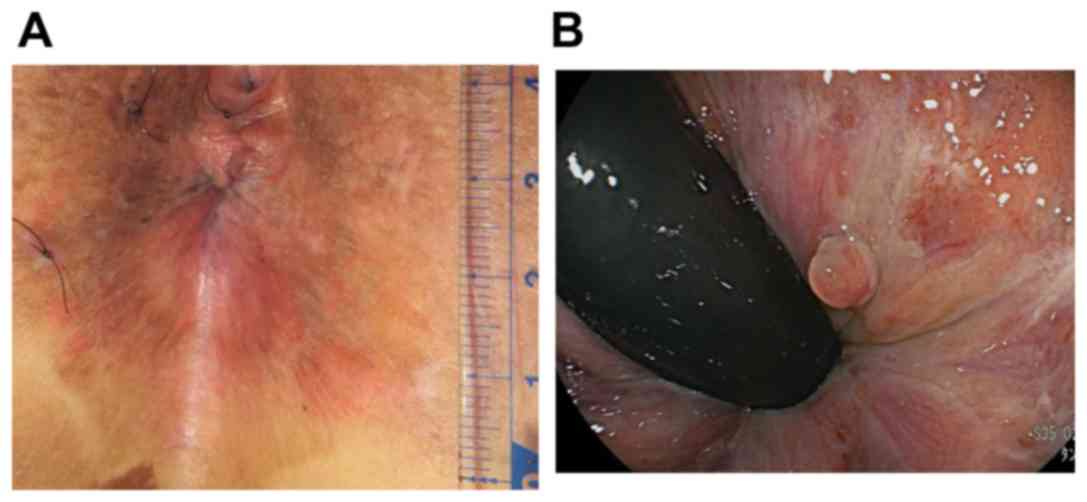
After the CRT, physical examination of the patient
revealed a reduced erythematous inflamed skin lesion in the
perianal region (Fig. 4A) and the
colonoscopy revealed regression of the tumor (Fig. 4B). It could not be detected in either
the CT or the MRI.
Robotic-assisted laparoscopic abdominoperineal
resection was performed. Antibiotics were administered for the
control of surgical site infection from post-operative day 7. No
postoperative urinary dysfunctions were observed, and the patient
was discharged on post-operative day 25. The macroscopic findings
of the surgical specimen confirmed the formation of a scar due to
the preoperative CRT (Fig. 5).
Microscopic examination of the anal tumor revealed no residual
carcinoma including the perianal pagetoid lesion nor lymph node
metastasis.
Discussion
Anal cancer accounts for 2-3% of all GI
malignancies, and among them, 95% are squamous cell carcinomas and
the remainder, primarily adenocarcinomas (3). Anal canal adenocarcinomas are rare.
According to the World Health Organization classification, anal
canal adenocarcinomas are subclassified into adenocarcinoma arising
from the anal mucosa and extramucosa, adenocarcinoma arising from
anorectal fistula or adenocarcinoma of anal glands (4). In the present case, the
subclassification of the anal tumor was adenocarcinoma of anal
gland according to the findings of colonoscopy and the tumor
biopsy.
Paget's disease was first described by Sir James
Paget in 1874(4) and it is
classified into mammary and extramammary. About one-third of
patients affected by Paget's disease have an underlying malignancy,
often represented by an anorectal carcinoma (5,6).
Extramammary Paget's disease is a rare condition typically
presenting as a reddish patch and/or nodule (7) and is commonly found in the vulvar area,
followed by the perianal area, scrotum, penis and axillae (8). Perianal Paget's disease is classified
as an extramammary Paget's disease. The true incidence of the
disease is difficult to estimate due to its rarity, but it is known
to represent <1% of all anal diseases and about 6.5% of all
cases of Paget's disease (9). There
are two types of perianal Paget's disease, the primary disease,
which consists of intra-epithelial neoplasm from an apocrine
source, and the secondary disease, which consists of a ‘pagetoid’
spread from an anorectal malignancy (9). Immunostaining for GCDFP15, CDX2, CK7,
CK20 is useful in enhancing the accuracy of diagnosis, such as the
type and the origin of Paget's disease. GCDFP15 is considered as
apocrine epithelium-specific tissue marker and is usually not
expressed in secondary perianal Paget's disease (1). The expression of CDX2 is a sensitive
and specific marker for the secondary type, arising from anorectal
or colonic adenocarcinoma, but CDX2 fails to distinguish between
the primary disease and the secondary type to urothelial or
prostatic malignancy (1). Although
most anal gland adenocarcinomas, similar to the normal anal gland,
are CK7 positive, but CK20 negative, several cases of secondary
type arising from anal gland carcinoma were reported to be positive
for both CK7 and CK20(1). In our
case, the skin biopsy revealed an infiltration of pagetoid cells,
which were positive for CK7 and CDX2, and negative for CK20 and
GCDFP15. From these findings, we diagnosed as perianal Paget's
disease secondary to the anal canal carcinoma.
There are no reports of clinically T1 anal gland
adenocarcinoma with pagetoid spread that caused inguinal lymph node
metastasis in English literature. Only one report of total pelvic
exenteration with lateral and inguinal lymph node dissection
followed by skin reconstruction in a case of T1 anal canal cancer
with pagetoid spread was found in the Japanese literature (10). It is suggestive that anal canal
adenocarcinoma with pagetoid spread may cause inguinal lymph node
metastasis in an early stage.
Lateral lymph node metastasis occurs in 15-20% of
lower rectal cancers, and treating such metastases is critical for
reducing local failure rates after surgical treatment of rectal
cancer (11). In Japan, mesorectal
excision with lateral lymph node dissection is the standard
treatment, suggestive that lateral lymph node dissection
significantly reduces local recurrence (12). However, lateral lymph node dissection
is also associated with postoperative urinary and sexual
dysfunctions, which can significantly deteriorate the patients'
quality of life. Furthermore, in Western countries, lateral lymph
node metastasis is treated with preoperative CRT (11). Previously, we demonstrated that
lateral lymph node dissection is not required in terms of
curability for patients with advanced carcinoma of the lower rectum
without apparent lateral pelvic lymph node metastasis treated with
preoperative radiotherapy (13).
Therefore, in our department, lateral lymph node dissection was
only indicated to patients with lateral lymph node metastasis and
it was avoided in those without, treated with preoperative CRT (a
total dose of 50.4 Gy in 28 fractions with concomitant
fluorouracil-based chemotherapy) (11,14-17).
Consensus has not yet been achieved concerning preoperative CRT
against anal canal cancer with pagetoid spread, but our present
report is supportive of its effectiveness for the safe resection of
this condition.
In conclusion, we experienced a rare case of early
anal canal adenocarcinoma with pagetoid spread and inguinal lymph
node metastasis, which could be effectively managed by preoperative
CRT followed by surgical resection. This case supports the
potential effectiveness of preoperative CRT for the safe resection
of pagetoid spread associated with anal canal adenocarcinoma, and
it should be carefully considered as a therapeutic modality.
Acknowledgements
Not applicable.
Funding
The present study was supported by Grants-in-Aid for
Scientific Research (grant nos. 16K07143, 16K07161, 17K10620,
17K10621C: 17K10623 and 18K07194) from the Japan Society for the
Promotion of Science, associated with cancer research. This
research was also supported by the Project for Cancer Research and
Therapeutic Evolution (grant no. 18cm0106502h0003) from the Japan
Agency for Medical Research and Development, associated with cancer
research.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
TN decided the treatment strategy and drafted the
article. TU diagnosed the anal canal adenocarcinoma with pagetoid
spread and inguinal lymph node metastasis and designed the
pathological comments and drafted the pathological pictures. SE,
KM, MK, HS, KS, YS, TT, KH, KK and HN decided the treatment
strategy of this case and revised the article critically for
important intellectual content. SI contributed to the conception of
the manuscript. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was conducted in accordance with the
Ethical guidelines of the Declaration of Helsinki and was approved
by the Ethics Committee of the University of Tokyo (approval no.
3252-9; Tokyo, Japan). The opportunity to opt out is always
available to the patients on our website.
Patient consent for publication
Written informed consent for the publication of data
and associated images was obtained from the patient.
Competing interests
The authors declares that they have no competing
interests.
References
|
1
|
Ishioka K, Koyama F, Kuge H, Inoue T,
Obara S, Nakamoto T, Sasaki Y, Nakamura Y, Takeda M, Ohbayashi C,
et al: Anal gland adenocarcinoma in situ with pagetoid spread: A
case report. Surg Case Rep. 4(63)2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Suenaga M, Oya M, Ueno M, Yamamoto J,
Yamaguchi T, Mizunuma N, Hatake K, Kato Y and Muto T: Anal canal
carcinoma with Pagetoid spread: Report of a case. Surg Today.
36:666–669. 2006.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Harris RE (ed): Epidemiology of Vaginal,
Vulvar and Anal Cancer. In: Epidemiology of chronic disease: Global
perspective. 2nd edition, Jones & Bartlett, 2019.
|
|
4
|
Bosman FT, Carneiro F, Hruban RH and
Theise ND (eds): WHO classification of tumours of the digestive
system. 4th edition. Lyon, IARC Press, 2010.
|
|
5
|
Goldman S, Ihre T, Lagerstedt U and
Svensson C: Perianal Paget's disease: Report of five cases. Int J
Colorectal Dis. 7:167–169. 1992.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kubota K, Akasu T, Nakanishi Y, Sugihara
K, Fujita S and Moriya Y: Perianal Paget's disease associated with
rectal carcinoma: A case report. Jpn J Clin Oncol. 28:347–350.
1998.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Paget J: On the disease of the mammary
gland areola preceding cancer of the mammary gland. St
Bartholomew's Hosp Rep. 10:87–89. 1874.
|
|
8
|
Lam C and Funaro D: Extramammary Paget's
disease: Summary of current knowledge. Dermatol Clin. 28:807–826.
2010.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Lopes Filho LL, Lopes IM, Lopes LR,
Enokihara MM, Michalany AO and Matsunaga N: Mammary and
extramammary Paget's disease. An Bras Dermatl. 90:225–231.
2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Dos Santos JS, Bonafé GA, Pereira JA,
Kanno DT, Martinez CAR and Ortega MM: Rare perianal extramammary
Paget disease successfully treated using topical Imiquimod therapy.
BMC Cancer. 18(921)2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ito T, Ishibashi K, Tajima Y, Hatano S,
Sobajima J, Ohsawa T, Okada N, Kumamoto K, Haga N and Ishida H: A
case of anal canal cancer with pagetoid spread and inguinal lymph
node involvement. Gan To Kagaku Ryoho. 38:2274–2276.
2011.PubMed/NCBI(In Japanese).
|
|
12
|
Ishihara S, Kawai K, Tanaka T, Hata K and
Nozawa H: Correlations between the sizes of lateral pelvic lymph
nodes and metastases in rectal cancer patients treated with
preoperative chemoradiotherapy. ANZ J Surg. 88:1306–1310.
2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Fujita S, Mizusawa J, Kanemitsu Y, Ito M,
Kinugasa Y, Komori K, Ohue M, Ota M, Akazai Y, Shiozawa M, et al:
Mesorectal excision with or without lateral lymph node dissection
for clinical stage II/III lower rectal cancer (JCOG0212): A
multicenter, randomized controlled, noninferiority trial. Ann Surg.
266:201–207. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Nagawa H, Muto T, Sunouchi K, Higuchi Y,
Tsurita G, Watanabe T and Sawada T: Randomized, controlled trial of
lateral node dissection vs. nerve-preserving resection in patients
with rectal cancer after preoperative radiotherapy. Dis Colon
Rectum. 44:1274–1280. 2001.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ishihara S, Kawai K, Tanaka T, Kiyomatsu
T, Hata K, Nozawa H, Morikawa T and Watanabe T: Oncological
outcomes of lateral pelvic lymph node metastasis in rectal cancer
treated with preoperative chemoradiotherapy. Dis Colon Rectum.
60:469–476. 2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ishihara S, Kawai K, Tanaka T, Kiyomatsu
T, Hata K, Nozawa H, Morikawa T and Watanabe T: Diagnostic value of
FDG-PET/CT for lateral pelvic lymph node metastasis in rectal
cancer treated with preoperative chemoradiotherapy. Tech
Coloproctol. 22:347–354. 2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Kawai K, Hata K, Tanaka T, Nishikawa T,
Otani K, Murono K, Sasaki K, Kaneko M, Emoto S and Nozawa H:
Learning curve of robotic rectal surgery with lateral lymph node
dissection: Cumulative sum and multiple regression analyses. J Surg
Educ. 75:1598–1605. 2018.PubMed/NCBI View Article : Google Scholar
|