Introduction
The Ommaya reservoir has been a treatment option as
an alternative to lumbar puncture since the 1960s (1). Previous findings have demonstrated it
to be generally well-tolerated in both pediatric and adult settings
despite its slightly higher infection risk (2) and other reported complications
(3). Patients' comfort and other
psychological factors often play a significant role in evaluating
its use (4). Ommaya reservoir use
for chemotherapy administration has in some settings (e.g.,
leptomeningeal malignancy) shown higher overall survival compared
to intrathecal chemotherapy via lumbar puncture (5). It has been used more extensively as
image guidance techniques have advanced (6). Ommaya reservoir is indicated in
treatment plans requiring repeated access to the intrathecal space.
Applications include treating cancer pain, chronic central nervous
system (CNS) infections, leptomeningeal metastasis, and prophylaxis
of CNS involvement in acute lymphoblastic leukemia (7).
In the present study, the case of a woman with
leukemic meningitis who repeatedly developed severe headache,
nausea, emesis, and diarrhea upon administration of intrathecal
chemotherapy via an Ommaya reservoir due to catheter migration into
brain parenchyma was investigated.
Case report
The patient was a 39-year-old woman who presented
with a three-week history of headaches, dizziness, and night
sweats. After noting leukocytosis, the patient was transferred to a
tertiary center the following day and a bone marrow biopsy revealed
acute lymphoblastic leukemia (8).
Her cerebrospinal fluid (CSF) was evaluated and found to have rare
blasts. She underwent a lumbar puncture with triple intrathecal
chemotherapy (methotrexate + hydrocortisone + cytarabine). Magnetic
resonance imaging (MRI) of the brain was subsequently performed and
demonstrated mild symmetrical pachymeningeal enhancement which was
thought to reflect sequela of the prior lumbar puncture. No
abnormal parenchymal or leptomeningeal enhancement was present. The
patient developed severe orthostatic headache after the lumbar
puncture, and the decision was made to place an Ommaya reservoir
with concern that repeated lumbar punctures would increase her risk
of CSF leak with persistent headaches secondary to intracranial
hypotension.
Three days later, she began oral dasatinib and
dexamethasone therapy per treatment protocol. The following day, a
right frontal Ommaya reservoir was placed with the aid of
electromagnetic intraoperative stealth guidance (6). The intraventricular catheter was
inserted into the right frontal horn and clear CSF could be seen
coming out. The opening pressure was approximately 5-6 mmHg. The
Ommaya reservoir was then tested with a small blunt needle and was
found to be working optimally. No intraoperative complications were
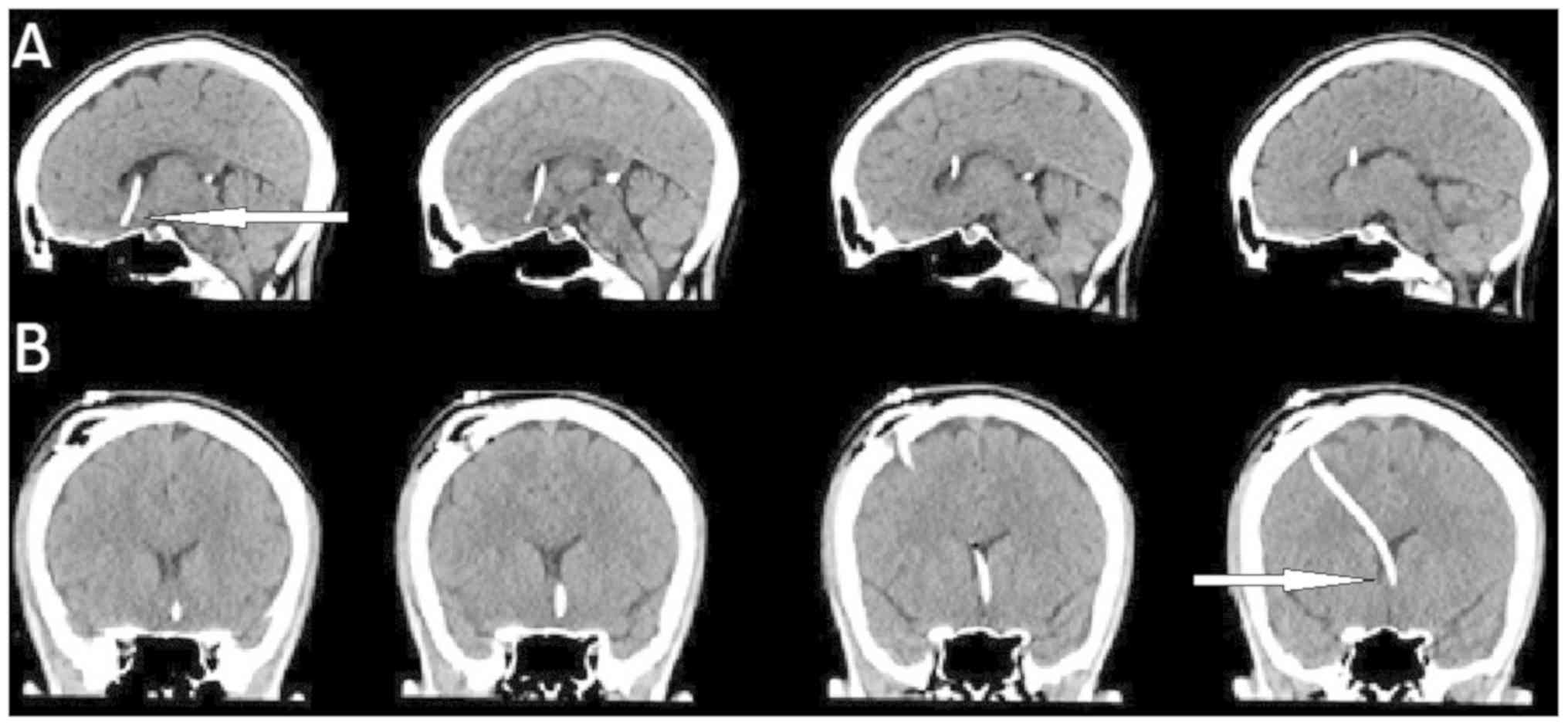
reported. Follow-up computerized tomography (CT) head showed the
new right-sided Ommaya reservoir with the tip of the catheter
projecting approximately 1.5 cm inferior to the floor of the left
frontal ventricle (Fig. 1). Despite
its deep positioning, the decision was made to use the catheter
without moving it since normal CSF flow had been observed.
One day after the Ommaya placement, the patient
underwent her second intrathecal administration of chemotherapy. A
butterfly needle was inserted in the Ommaya dome and 15 ml of
pinkish CSF was withdrawn using a 10 cc syringe. This was followed
by administration of 15 mg of methotrexate mixed in with 50 mg of
hydrocortisone. The procedure was carried out over 5 min, with the
drugs being flushed from the tubing with the patient's autologous
CSF. At the end of the infusion the patient started developing a
frontal headache, followed by nausea and an episode of emesis and
diarrhea. Vital signs were stable during that episode. The fluid's
pink color was attributed to blood products from recent surgery
still present in the CSF spaces. CSF cytology was negative for
malignancy. The post-infusion symptoms were felt to be due to a
reaction to the medication and the plan going forward was to
continue biweekly intrathecal chemotherapy treatments with
prophylactic anti-nausea and pain medication if symptoms recurred.
Five days later, the patient received her next intrathecal
chemotherapy via the Ommaya reservoir. A 25-guage butterfly needle
was inserted in the Ommaya dome and a small 5 cc syringe was used
for very gentle aspiration given a low platelet count as well as
prior complications. Clear fluid (8 ml) was withdrawn without
complications, followed by administration of 15 mg of methotrexate
and 50 mg of hydrocortisone, for a total volume of 5 ml. The drug
was pushed over 5 min. Close to the conclusion of the injections,
the patient started developing a frontal headache and before and
then at the conclusion of the injection the patient experienced
several episodes of emesis. She was then medicated with lorazepam
and ondansetron. It was unclear at the time whether the etiology of
the adverse symptoms was mechanical or chemical in nature.
Three days later, a third dose was attempted via the
Ommaya reservoir. This time, modifications were made such that the
patient was pre-medicated with lorazepam and ondansetron. A 3 cc
syringe as opposed to a 5 cc syringe was used to decrease the
pressure of injection. A 23-guage butterfly needle was inserted in
the Ommaya dome and 3 cc syringes were used to withdraw the fluid.
Then, 12 ml of fluid was gradually withdrawn, followed by a very
slow chemotherapy injection of 1 ml per 2 min. At approximately 2
ml into the injection, the patient started experiencing a frontal
headache again. Another 0.5 ml was injected and the patient started
feeling nauseous. At this point, the injection was aborted and the
needle was withdrawn after flushing the tubing with 2 ml of CSF.
The patient went on to vomit and had an episode of diarrhea.
The head CT images were reviewed, and there was
concern that the location of the catheter could be playing a role
in the patient's adverse reaction after each intrathecal injection.
It was thought that possibly changing the location of the Ommaya
catheter would improve tolerance of chemotherapy. The decision was
made to return to the operating room for a revision of the Ommaya
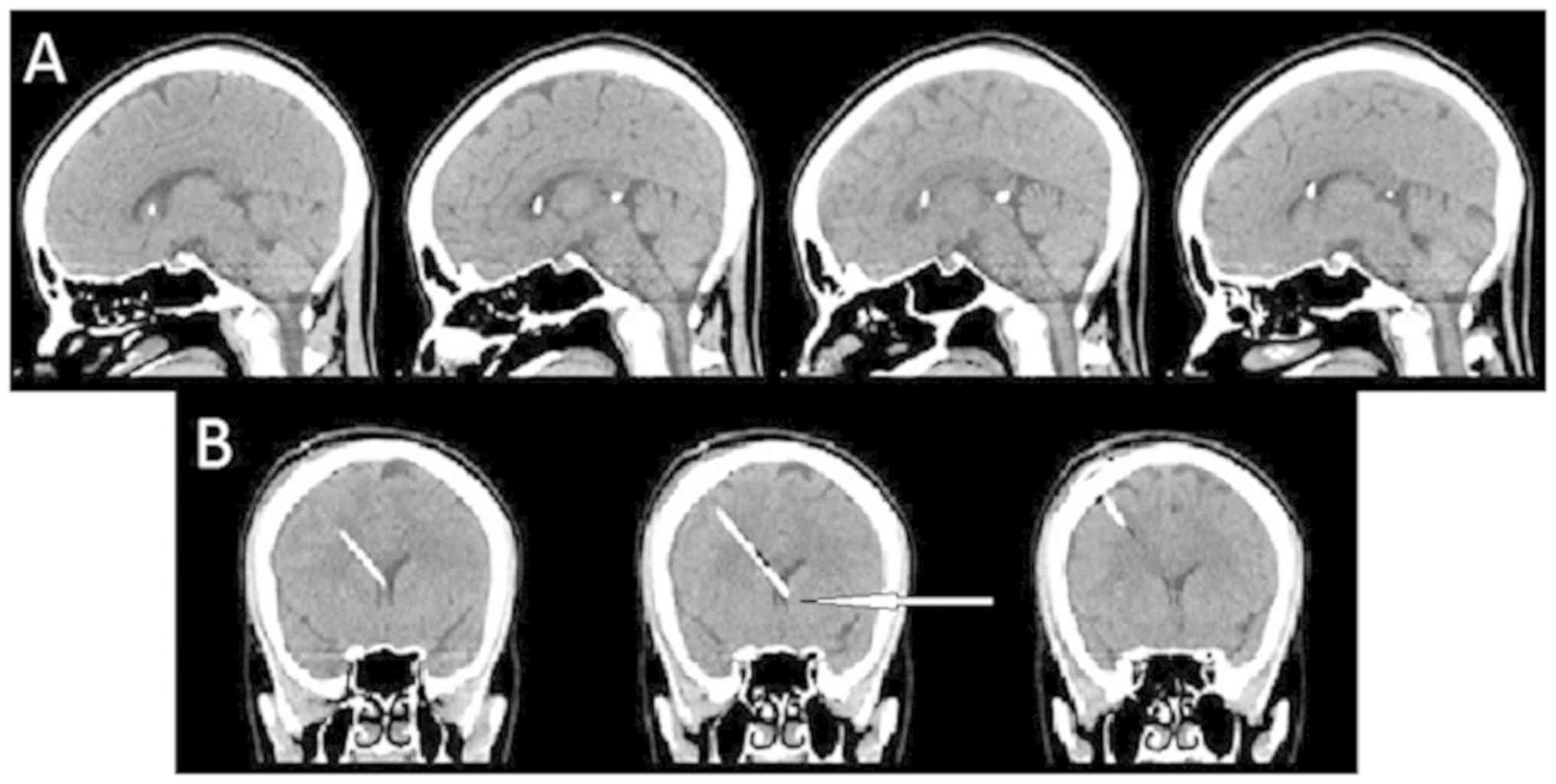
catheter. The Ommaya reservoir was felt to be intact. As optimal
placement would be approximately 2 cm shorter for the distal
catheter location, the Ommaya reservoir was gently lifted out of
the bur hole and held in place using a rubber shod-covered
hemostat. The suture around the Ommaya reservoir was cut, and then
the Ommaya reservoir itself was disconnected. The ventricular
catheter was slowly advanced out of the bur hole until 22 mm was
excised from the proximal end of the catheter. At this point, the
Ommaya reservoir was reconnected and secured. Compression of the
Ommaya reservoir did reveal excellent flow in and out of spinal
fluid. Head CT imaging the following day verified a successful
repositioning (Fig. 2).
Four weekly doses were administered following the
Ommaya revision. In each case, a 23 gauge butterfly needle was
inserted in the Ommaya dome and 15 ml of clear CSF was withdrawn.
This was followed by the administration of 15 mg of intrathecal
cytarabine in a total volume of 5 ml. The drug was pushed at a rate
of 1 ml/min. The drug was flushed from the tubing with autologous
CSF to the amount of 5 ml. Contrary to previous instances, the
patient tolerated all procedures well without complications. More
specifically, the reproducible frontal headache, nausea, emesis and
diarrhea previously seen were completely absent.
Discussion
The patient's original adverse symptoms can almost
certainly be attributed to catheter misplacement, given the fact
that the symptoms improved after repositioning the catheter.
However, we can only hypothesize what the pathophysiological
explanation may have been. Side effects of intrathecal methotrexate
toxicity are well documented in the literature, but do not match
the patient's experience. Acute neurotoxicity due to intrathecal
methotrexate overdose typically presents within 24-48 h as chemical
arachnoiditis with symptoms that include headache, nuchal rigidity,
back pain, vomiting, fever, and CSF pleocytosis (9,10). Other
documented side effects of intrathecal chemotherapy toxicity in
general include spinal cord lesions (manifesting most commonly as
tetraplegia, paraplegia, and cauda equina syndrome), seizure, and
encephalopathy (11). Furthermore,
methotrexate has a half-life in CSF on the order of hours (11). It seems unlikely that adverse
symptoms due to a toxic concentration within the parenchyma would
subside within minutes, as experienced by the patient. Rather, we
consider the proximity of the catheter tip to the hypothalamus as a
better explanation. The nucleus tractus solitarius (NTS) is central
to the vagal neurocircuits involved in nausea and vomiting, and
exchanges both inputs and outputs with the hypothalamus (12).
Irrespective of the underlying pathophysiology, the
case demonstrates the value in troubleshooting Ommaya reservoir
complications rather than prematurely abandoning its use in favor
of lumbar puncture, which is also associated with adverse
complications (i.e., post-LP headache, CSF leak, and discomfort to
the patient). It should be noted that lumbar puncture allows the
patient to avoid surgery and potential infection risk associated
with the presence of a permanent catheter. However, an Ommaya
reservoir was deemed appropriate in this case due to the patient's
severe spinal headache following her initial lumbar puncture, as
well as her requirement for repeated intrathecal chemotherapy
delivery. Using an Ommaya reservoir minimizes patient discomfort
and takes advantage of the natural flow of CSF, providing a more
direct delivery and even distribution of chemotherapy along the CNS
axis as compared to lumbar puncture (5).
The case also demonstrates the profound effects that
can be caused from a small displacement of any sort of catheter
within the brain. In other words, this case is of an Ommaya
reservoir, these complications can arise from a small misplacement
of an external ventricular device, a catheter-delivering tissue
plasminogen activator, or any other catheter placed within the
brain. Utmost care was taken to ensure precise initial placement of
the catheter, with stereotactic trajectories planned and followed
with the aid of stealth navigation registered with MRI scans taken
within 3 days of surgery. Movement of catheters post-placement is a
known complication, with up to 33% of misplaced ventricular
catheters showing movement between intraoperative image guidance
and the first post-operative scan (13).
In conclusion, both initial precision in placement
and continued monitoring of catheter location can lead to drastic
differences in patient care and outcomes. For this reason, catheter
location should be verified with repeated imaging before and
potentially between intrathecal chemotherapy infusions, especially
when there are unexpected or disproportionate negative side effects
from medications delivered through the device.
Ackowledgements
We would like to express our gratitude to the
patient for letting us present and publish her case. Publication of
this study was supported by the Comprehensive Neuro-Oncology
Program Fund at Mayo Clinic, Arizona.
Funding
Not applicable.
Availability of data and materials
Not applicable.
Authors' contributions
MMM was responsible for the article concept. CVS
acquired imaging. The draft of the manuscript was prepared by DJM.
All authors contributed to the design of the work and participated
in the critical revision of the manuscript. All authors read,
approved the final version and agreed to be accountable for all
aspects of the work.
Ethics approval and consent to
participate
IRB approval not required.
Patient consent for publication
Written consent obtained.
Competing interests
Not applicable.
References
|
1
|
Cohen-Pfeffer JL, Gururangan S, Lester T,
Lim DA, Shaywitz AJ, Westphal M and Slavc I:
Intracerebroventricular delivery as a safe, long-term route of drug
administration. Pediatr Neurol. 67:23–35. 2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Mead PA, Safdieh JE, Nizza P, Tuma S and
Sepkowitz KA: Ommaya reservoir infections: A 16-year retrospective
analysis. J infect. 68:225–230. 2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Lishner M, Perrin RG, Feld R, Messner HA,
Tuffnell PG, Elhakim T, Matlow A and Curtis JE: Complications
associated with Ommaya reservoirs in patients with cancer. The
Princess Margaret Hospital experience and a review of the
literature. Arch Intern Med. 150:173–176. 1990.PubMed/NCBI
|
|
4
|
Bin Nafisah S and Ahmad M: Ommaya
reservoir infection rate: A 6-year retrospective cohort study of
Ommaya reservoir in pediatrics. Childs Nerv Syst. 31:29–36.
2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Montes de Oca Delgado M, Cacho Diaz B,
Santos Zambrano J, Guerrero Juárez V, López Martínez MS, Castro
Martínez E, Avendaño Méndez-Padilla J, Mejía Pérez S, Reyes Moreno
I, Gutiérrez Aceves A and González Aguilar A: The comparative
treatment of intraventricular chemotherapy by ommaya reservoir vs.
Lumbar puncture in patients with leptomeningeal carcinomatosis.
Front Oncol. 8(509)2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Lau JC, Kosteniuk SE, Walker T,
Iansavichene A, Macdonald DR and Megyesi JF: Operative
complications with and without image-guidance: A systematic review
and meta-analysis of the Ommaya reservoir literature. World
Neurosurg. 122:404–414. 2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Sundaresan N and Suite ND: Optimal use of
the Ommaya reservoir in clinical oncology. Oncology (Williston
Park). 3:15–22; discussion 23. 1989.PubMed/NCBI
|
|
8
|
Papanastasiou L, Fountoulakis S, Pappa T,
Liberopoulos K, Malliopoulos D, Markou A and Piaditis G: Brain and
optic chiasmal herniation following cabergoline treatment for a
giant prolactinoma: Wait or intervene? Hormones (Athens).
13:290–295. 2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Livshits Z, Rao RB and Smith SW: An
approach to chemotherapy-associated toxicity. Emerg Med Clin North
Am. 32:167–203. 2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kerr JZ, Berg S and Blaney SM: Intrathecal
chemotherapy. Crit Rev Oncol Hematol. 37:227–236. 2001.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kwong YL, Yeung DY and Chan JC:
Intrathecal chemotherapy for hematologic malignancies: Drugs and
toxicities. Ann Hematol. 88:193–201. 2009.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Babic T and Browning KN: The role of vagal
neurocircuits in the regulation of nausea and vomiting. Eur J
Pharmacol. 722:38–47. 2014.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Whitehead WE, Riva-Cambrin J, Wellons JC
III, Kulkarni AV, Browd S, Limbrick D, Rozzelle C, Tamber MS, Simon
TD, Shannon CN, et al: Factors associated with ventricular catheter
movement and inaccurate catheter location: Post hoc analysis of the
hydrocephalus clinical research network ultrasound-guided shunt
placement study. J Neurosurg Pediatr. 14:173–178. 2014.PubMed/NCBI View Article : Google Scholar
|