Introduction
Ductal carcinoma in situ (DCIS) is a
non-invasive malignant breast disease described as a precursor
lesion to invasive breast cancer. With the progress of diagnostic
breast imaging, opportunities to diagnose DCIS are on the
increase.
If breast cancer is suspected, core-needle biopsy
(CNB) or vacuum-assisted biopsy (VAB) is performed. Those
percutaneous breast biopsies are important procedures for
decreasing the number of excisional biopsies. However, diagnosis
from such a biopsy cannot provide definitive diagnosis. For
example, a preoperative diagnosis of DCIS is sometimes upstaged to
invasive ductal carcinoma (IDC). In the literature, the
underestimation rate has been reported as 15-40% (1-4).
Upstaging to IDC is critical for both patients and
surgeons. Surgeons should consider the possibility of
underestimation, such as whether to include sentinel lymph node
biopsy (SLNB) in a subsequent definitive surgical procedure. Some
predictors of underestimation have been reported. Brennan et
al reported palpability, nuclear grade, tumor size, and other
factors (2). However, reliable
predictors have not been clearly identified.
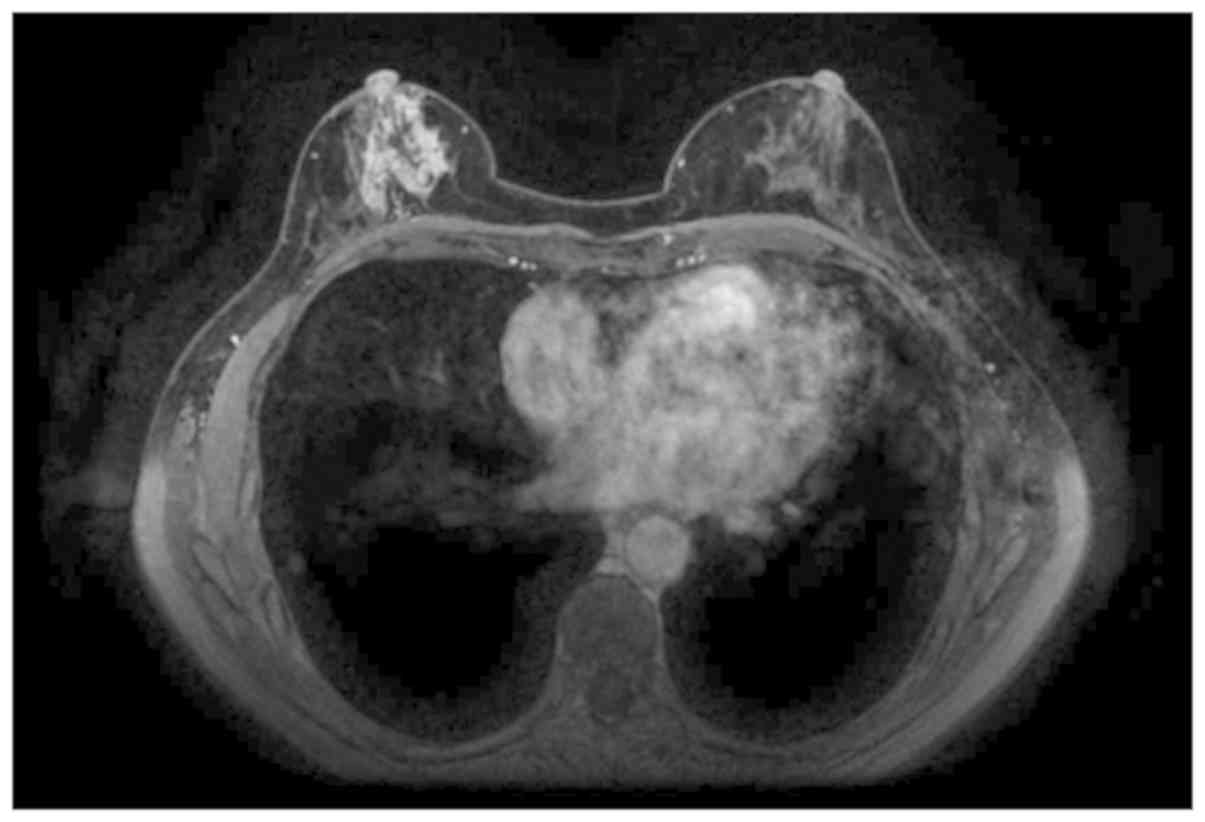
DCIS takes various forms, including solid mass
lesion, intracystic lesion, calcification alone, and distortion. An
abnormal result from palpation is sometimes a predictor of
upstaging to invasive disease (5).
However, for lesions showing an intracystic component, the
underestimation ratio may not necessarily be high even if the
results of palpation are abnormal. Investigating mass-type DCIS or
non-mass-type DCIS (Fig. 1)
separately is thus important.
This case focused on predictors for underestimation
of non-mass-type lesions. Currently, no reports from this point of
view have been published. This is thus, to the best of our
knowledge, the first report to investigate underestimation, defined
as biopsy diagnosis of DCIS with attention only on non-mass-type
lesions.
Patients and methods
Patients
The present study was conducted with approval from
the institutional review board of Tokyo Medical and Dental
University (IRB-approved number is M2000-831, 2000) and with
informed consent of the patient. Data were retrieved from our
database for 150 consecutive women with an initial CNB or VAB
diagnosis of DCIS, and who underwent surgical resection at our
institution between September, 2007 and August, 2017. Only 101
cases in which masses could not be confirmed from magnetic
resonance imaging (MRI) and ultrasound (US) were examined (Fig. 1).
Non-mass-type lesions were defined from US showing a
non-mass lesion (e.g., duct ectasia, intraductal calcification,
architectural distortion, clustered microcysts, hypoechoic area)
and MRI showing non-mass enhancement (homogeneous, heterogeneous,
clumped, or clustered ring). A lack of abnormal findings on US
and/or MRI were also considered acceptable.
Imaging evaluation
Mammography examination (craniocaudal and
mediolateral oblique views) was performed using a Lorad Selenia
mammograph (Hologic). An EUB-7500 scanner with a EUP-L54MA 9.75-MHz
linear probe (Hitachi Medical Systems) or Aplio XG scanner with a
PLT-805AT 8.0-MHz linear probe (Toshiba Medical Systems) was used
for US examinations. MRI examination was performed with a 1.5-T
system (Magnetom Vision; Siemens) and a 3.0-T system (Signa HDxt;
General Electric Medical Systems) using a breast coil in the prone
position. To evaluate the results of MRI, the early phase of a
contrast enhancement study within 1 and 2 min after intravenous
bolus injection of gadobenate dimeglumine (Gd-DTPA) (0.2 ml/kg) was
obtained. A unilateral coronal T1-weighted sequence [repetition
time (TR) = 170 msec; echo time (TE) = 4.7 msec; flip angle = 40°;
4-mm thick section, 256x256 matrix; field of view = 210 mm] using
the 1.5-T system and bilateral axial fat-suppressed T1-weighted
sequence (TR = 6.5 msec; TE = 2.4 msec; flip angle = 10°; section
thickness = 2 mm; matrix = 512x512; field of view = 360 mm) using
the 3.0-T system were employed.
Examinations were performed by one of three
radiologists with >5 years of experience in breast imaging. The
radiologists had knowledge of the clinical indications for
examination and interpreted lesions using the Breast Imaging
Reporting and Data System. For each lesion, the two most
experienced radiologists retrospectively reviewed the results
together to reach consensus.
Biopsy procedure
CNB or VAB were performed, guided by US or
mammography (MMG). If lesions were detected by US, biopsy was
performed as a US-guided procedure. If no lesion was detected by
US, stereotactic VAB (ST-VAB) was performed. CNB used a 14-G Biopsy
System (CR Bard) and VAB used needles of 10 G8- or 11-G Mammotome
(Ethicon Endo-Surgery) or 11- or 14-G Vacora (CR Bard). Our
standard protocol was to obtain 3-7 core samples per lesion in the
US-guided procedure and 5-12 core samples in ST-VAB. In specific
cases such as where the amount of tissue obtained was grossly
inadequate or targeting difficulty was experienced, the number of
samples was increased. On the other hand, when the patient proved
uncooperative or declined to continue, or when minor complications
such as pain or bleeding were encountered, fewer core samples were
obtained. Cases of excisional biopsy were excluded.
Immunohistochemical examination
All specimens were analyzed by pathologists from
Tokyo Medical and Dental university, and specimens were considered
estrogen receptor (ER)- or progesterone receptor (PgR)-positive on
immunohistochemistry (IHC) for staining rates >10%. For HER2
receptor values, IHC 3+ was defined as breast cancer with strong,
complete membrane staining observed in at least 10% of tumor cells.
For HER2 receptor overexpression of 2+, gene amplification with
fluorescence in situ hybridization was not performed in this
study.
Data analysis
After review of the postoperative pathologic
results, final diagnoses of all lesions were divided into two
groups: Pure DCIS, or invasive ductal carcinoma. Medical records
were then reviewed. Differences in proportions of categorical data
were tested using Fisher's exact probability test. Unless otherwise
indicated, significant differences among mean values of numerical
data were analyzed using the two-sample two-sided t-test.
Predictors of invasive carcinoma underestimation were determined by
uni- and multivariate logistic regression analyses. Values of
P<0.05 were regarded as statistically significant. All
statistical analyses were performed using EZR software (Saitama
Medical Center, Jichi Medical University, (http://www.jichi.ac.jp/saitama-sct/SaitamaHP.files/statmed.html),
and a graphic user interface for R (The R Foundation for
Statistical Computing). More precisely, EZR is a modified version
of R Commander designed to add statistical functions frequently
used in biostatistics (6).
Results
Clinicopathological
characteristics
The clinicopathological features of all patients are
summarized in Table I. The mean age
of all patients was 55 years (range, 33-82 years). A total of 27
patients (27%) were finally diagnosed with invasive cancer. In
breast examinations, results of palpation were normal in 81
patients (80%) and abnormal in 20 patients (20%). Mammographic
abnormality detected calcification (cal) only in 62 patients (61%),
focal asymmetric density (FAD) only in 8 patients (8%), distortion
only in 6 patients (6%), negative findings in 16 patients (16%),
and other (FAD+cal, FAD+distortion, or distortion+cal) in 9
patients (9%).
 | Table ICharacteristics at the time of biopsy
(n=101). |
Table I
Characteristics at the time of biopsy
(n=101).
| Characteristics | Patients (n=101) | Percentage of sample
(%) |
|---|
| Age (years) |
| Mean age ± SD | 56.0±11.2 | |
|
≤50 | 40 | 40 |
|
>50 | 61 | 60 |
| Postoperative
pathology |
|
DCIS | 74 | 73 |
|
IDC | 27 | 27 |
| Physical
examination |
|
Abnormal
result of palpation | 20 | 20 |
|
Normal
result of palpation | 81 | 80 |
| Mammographic
lesion |
|
Calcification | 62 | 61 |
|
FAD | 8 | 8 |
|
Distortion | 6 | 6 |
|
Others | 9 | 9 |
|
No
findings | 16 | 16 |
| Enhancement pattern
on MRI |
|
Homogenous | 1 | 1 |
|
Heterogenous | 12 | 12 |
|
Clumped | 44 | 43 |
|
Clustered
ring | 32 | 32 |
|
No
findings | 9 | 9 |
| Maximum lesion size
(mm) |
| Mean diameter ±
SD | 46 | |
| Range, 10-80 mm |
|
10-29 | 25 | 24 |
|
30-49 | 39 | 38 |
|
50-69 | 21 | 21 |
|
>70 | 4 | 4 |
|
Other | 13 | 13 |
| Biopsy method |
|
US-CNB | 28 | 28 |
|
US-VAB | 39 | 38 |
|
ST-VAB | 34 | 34 |
| ER |
|
Positive | 71 | 70 |
|
Negative | 25 | 25 |
|
Unknown | 5 | 5 |
| PgR |
|
Positive | 65 | 64 |
|
Negative | 31 | 31 |
|
Unknown | 5 | 5 |
| HER2 |
|
Positive | 20 | 20 |
|
Negative | 73 | 72 |
|
Unknown | 8 | 8 |
| Nuclear grade |
|
1,2 | 87 | 86 |
|
3 | 10 | 10 |
|
Unknown | 4 | 4 |
| Comedo necrosis |
|
Absent | 63 | 62 |
|
Present | 37 | 37 |
|
Unknown |
1 | 1 |
Enhancement patterns on MRI were categorized as
follows: Homogeneous, heterogeneous, clumped, or clustered ring
pattern. Enhancement patterns were homogeneous in 1 patient (1%),
heterogeneous in 12 patients (12%), clumped in 44 patients (43%),
and clustered ring in 32 patients (32%).
Median maximum diameter in the 90 patients with
measurable lesions on MRI was 46 mm (range, 10-80 mm). The
remaining 11 patients had negative findings for the breast or
unmeasurable findings on breast MRI. As 30 mm was the median, we
divided cases into >30 or ≤30 mm. Twenty-eight patients (28%)
underwent CNB guided by US, 39 patients (39%) underwent VAB guided
by US, and 34 patients (34%) underwent ST-VAB. All patients
underwent SLNB, revealing a positive result in only 1 patient. No
evidence of metastasis to a non-sentinel lymph node was
identified.
Immunohistochemical examination
The frequency of a HER2 score of 0-2+ was 72% and
that of 3+ was 20%. HER2 score was unknown in 8%. ER- and
PR-positive statuses were seen in 70 and 64% of our cases.
ER+/HER2- status was seen in 64%, ER+/HER2+ status
in 9%, ER-/HER2+ status in 10%, and ER-/HER2- in 5%. Among the 19
patients diagnosed with HER2-positive DCIS preoperatively, 9
patients (53%) were upstaged to IDC.
Predictors of invasive carcinoma
underestimation
Univariate analysis of predictors for the presence
of invasive components within final specimens initially diagnosed
as DCIS is summarized in Table II.
The rate of upstaging to invasive cancer in the final pathology was
significantly associated with variables such as abnormal results of
palpation on breast examination (P=0.05), comedo necrosis (P=0.05),
and HER2 status (P=0.02). Multivariate analysis of all factors
identified as significant in univariate analyses demonstrated the
presence of abnormal palpation as an independent predictor of
invasive cancer underestimation (odds ratio 4.76; confidence
interval 1.44-15.7; P=0.01) (Table
III).
 | Table IIUnivariate analysis of predictors of
invasive cancer in all 101 patients with an initial diagnosis of
non-mass DCIS. |
Table II
Univariate analysis of predictors of
invasive cancer in all 101 patients with an initial diagnosis of
non-mass DCIS.
| Final
diagnosis | |
|---|
|
Characteristics | IDC (n=27) | DCIS (n=74) | Underestimation
rate (%) |
P-valuea |
|---|
| Age |
| Mean age ± SD | 54.3±10.1 | 55.4±11.7 | | 0.64b |
| Range | 39-71 | 33-82 | | |
| Palpation |
|
Abnormal | 9 | 11 | 45 | |
|
Normal | 18 | 63 | 22 | 0.05 |
| Biopsy method |
|
ST-VAB | 8 | 26 | 23 | |
|
US-VAB | 11 | 28 | 28 | |
|
US-CNB | 8 | 20 | 28 | 0.88 |
| MMG |
|
Calcification
only or normal | 20 | 58 | 26 | |
|
FAD | 2 | 6 | 25 | |
|
Distortion | 1 | 5 | 17 | |
|
Others | 4 | 5 | 44 | 0.65 |
| Enhancement pattern
on MRI | 0 | 1 | | |
| homogenous |
|
Heterogenous | 5 | 7 | | |
|
Clumped | 10 | 34 | | |
|
Clustered
ring | 10 | 22 | | |
|
No
findings | 1 | 8 | | 0.483 |
| MRI size (mm) |
|
<30 | 12 | 38 | 24 | |
|
≥30 | 14 | 34 | 29 | |
|
Unknown | 1 | 2 | | 0.81 |
| ER |
|
Positive
(≥10%) | 19 | 58 | 25 | |
|
Negative | 8 | 14 | 36 | |
|
Unknown | 0 | 2 | | 0.48 |
| PgR |
|
Positive
(≥10%) | 18 | 52 | 26 | |
|
Negative | 9 | 20 | 31 | |
|
Unknown | 0 | 2 | | |
| HER2 |
|
Positive | 10 | 9 | 53 | |
|
Negative | 16 | 59 | 21 | |
|
Unknown | 1 | 6 | | 0.02 |
| Nuclear grade |
|
3 | 3 | 7 | 30 | |
|
1, 2 | 21 | 65 | 24 | |
|
Unknown | 3 | 2 | | 0.71 |
| Comedo
necrosis |
|
Present | 14 | 23 | 25 | |
|
Absent | 12 | 51 | 19 | |
|
Unknown | 1 | 0 | | 0.05 |
 | Table IIIMultivariate analysis for predictors
of invasive cancer in patients with non-mass-type DCIS (n=101). |
Table III
Multivariate analysis for predictors
of invasive cancer in patients with non-mass-type DCIS (n=101).
| Independent
predictors of invasive cancer | Odds ratio | 95% confidence
interval |
P-valuea |
|---|
| Abnormal
palpation | 4.76 | 1.44-15.7 | 0.01 |
| Comedo
necrosis | 2.32 | 0.76-7.14 | 0.14 |
| CNB HER2 | 2.84 | 0.85-9.46 | 0.09 |
Discussion
To the best of our knowledge, this is the first
report to assess predictive factors focusing only on non-mass-type
DCIS. Our study showed that among preoperatively diagnosed
non-mass-type DCIS, approximately 27% were underestimations. In
particular, the presence of a clinically abnormal result of
palpation appeared to increase the chance of up-staging to invasive
cancer.
Many studies have reported preoperative factors that
can predict upstaging of DCIS to invasive cancer (2,3,5,7-15).
We hypothesized that the factors listed in those reports may be
influenced by the forms of DCIS. Factors such as size and existence
of a palpable lesion depend on whether the DCIS is mass or non-mass
type. For example, among intracystic lesions, the underestimation
rate may not be high despite the large, palpable lesion. Our study
focused only on non-mass-type DCIS and evaluated preoperative
clinicopathological factors predicting underestimation.
The underestimation rate for percutaneous breast
biopsy has been reported to range between 15 and 40% (1-4).
In the present study, the underestimation rate was 27%, within the
reported range. As biopsy targeted at the component considered
invasive is difficult for non-mass-type DCIS, we thought that the
underestimation rate may be lower. However, the underestimation
rate was unchanged in the present study. The underestimation rate
may also change depending on the thickness of the needle, the
number of specimens and the number of stereotactic biopsies, thus
re-examination of an increased number of cases is necessary.
Findings of this study demonstrated that
preoperative factors predictive of the invasive component were
abnormal results of palpation, HER2-positive, and comedo necrosis
in univariate analysis. Overexpression of HER2 in invasive breast
cancer is an independent predictor of poor prognosis. The
significance of HER2 overexpression in DCIS is not well defined.
However, HER2 DCIS has recently been reported as an aggressive type
(16-18).
Monabati et al reported that HER2-positive DCIS cases were
more likely to be of high nuclear grade (18). Mustafa et al reported that
HER2-positive DCIS tended to be upstaged to invasive ductal
carcinoma (16). However, the
targets of that report were all typed as DCIS. This was the first
report to examine HER2 score for non-mass-type DCIS only. The
results showed that HER2-positive DCIS tended to be upstaged to
invasive cancer, but no significant difference was observed in
multivariate analysis. Future studies will accumulate data for
these tests from additional cases and further assessment is needed
for validation.
In our study, only an abnormal result of palpation
was a predictive factor in multivariate analysis. Other studies
have reported abnormal palpation as a predictor (1,15,18). On
the other hand, Sato et al described abnormal palpation as
irrelevant to the presence of invasion (5). However, those reports all examined
all-type DCIS, rather than restricting investigation to only
non-mass-type DCIS. No previous reports have described abnormal
palpation as a predictor in non-mass-type DCIS.
Previous findings have shown that, CNB and thinner
needles as significant predictors of underestimation compared to
VAB or thicker needles (10). In the
present study, different devices were not associated with
upstaging. Various factors may have contributed to this finding.
One was the difference in the number of cases. Another case
involved US guidance in which a lesion with suspected invasiveness
was biopsied using CNB rather than VAB. As a result, the risk of
underestimation tended to be reduced with VAB.
The present study has some limitations. First, this
study is a single-institution review and retrospective.
Nevertheless, the results of the present study may be valuable to
other institutions at the time of surgery for cases with a
preoperative diagnosis of DCIS. In particular, information
containing HER2 status is considered valuable, as our institution
routinely tests for the overexpression of HER2 in all patients with
DCIS. Second, the number of cases has been reduced by targeting
only non-mass DCIS. As a result, the essential stratification in
this study indicated the sample size of each group was reduced.
Future validation studies with a large sample set evaluating the
risk factors leading to upstaging of DCIS and potential new options
in the DCIS treatment algorithm are required.
In conclusion, preoperatively diagnosed
non-mass-type DCIS represented an underestimation in approximately
27% of cases. In particular, the presence of a clinically abnormal
result of palpation increases the chances of up-staging to invasive
cancer. In cases with an abnormal result from palpation, the
surgeon should select the operation in consideration of the
possibility of upstaging to IDC. Larger, multi-institutional
investigations are necessary to more closely examine risk factors
for upstaging of non-mass-type DCIS on breast biopsy to IDC on the
final pathology.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
GO performed surgery, wrote the manuscript, analyzed
the data and performed the statistical analysis. TN, AO, YK, TH, HS
and TI performed surgery and collected data. MM, TF and KK were
responsible for diagnostic imaging and biopsy. IO was in charge of
the pathology. HU designed the present study and wrote the
manuscript. The final version was read and adopted by all the
authors.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Tokyo Medical and Dental University Hospital (Tokyo, Japan). Signed
informed consents were obtained from the patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lee JW, Han W, Ko E, Cho J, Kim EK, Jung
SY, Cho N, Moon WK, Park IA and Noh DY: Sonographic lesion size of
ductal carcinoma in situ as a preoperative predictor for the
presence of an invasive focus. J Surg Oncol. 98:15–20.
2008.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Brennan ME, Turner RM, Ciatto S,
Marinovich ML, French JR, Macaskill P and Houssami N: Ductal
Carcinoma in situ at core-needle biopsy: Meta-analysis of
underestimation and predictors of invasive breast cancer.
Radiology. 260:119–128. 2011.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Wahedna Y, Evans AJ, Pinder SE, Ellis IO,
Blamey RW and Geraghty JG: Mammographic size of ductal carcinoma in
situ does not predict the presence of an invasive focus. Eur J
Cancer. 37:459–462. 2001.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Darling ML, Smith DN, Lester SC, Kaelin C,
Selland DL, Denison CM, DiPiro PJ, Rose DI, Rhei E and Meyer JE:
Atypical ductal hyperplasia and ductal carcinoma in situ as
revealed by large-core needle breast biopsy: Results of surgical
excision. AJR Am J Roentgenol. 175:1341–1346. 2000.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Sato Y, Kinoshita T, Suzuki J, Jimbo K,
Asaga S, Hojo T, Yoshida M and Tsuda H: Preoperatively diagnosed
ductal carcinoma in situ: Risk prediction of invasion and effects
on axillary management. Breast Cancer. 23:761–770. 2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kanda Y: Investigation of the freely
available easy-to-use software ‘EZR’ for medical statistics. Bone
Marrow Transplant. 48:452–458. 2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Jackman RJ, Burbank F, Parker SH, Evans WP
III, Lechner MC, Richardson TR, Smid AA, Borofsky HB, Lee CH,
Goldstein HM, et al: Stereotactic breast biopsy of nonpalpable
lesions: Determinants of ductal carcinoma in situ underestimation
rates. Radiology. 218:497–502. 2001.PubMed/NCBI View Article : Google Scholar
|
|
8
|
King TA, Farr GH, Cederbom GJ, Smetherman
DH, Bolton JS, Stolier AJ and Fuhrman GM: A mass on breast imaging
predicts coexisting invasive carcinoma in patients with a core
biopsy diagnosis of ductal carcinoma in situ. Am Surg. 67:907–912.
2001.PubMed/NCBI
|
|
9
|
Hoorntje LE, Schipper ME, Peeters PH,
Bellot F, Storm RK and Borel Rinkes IH: The finding of invasive
cancer after a preoperative diagnosis of ductal carcinoma-in situ:
Causes of ductal carcinoma-in situ underestimates with stereotactic
14-gauge needle biopsy. Ann Surg Oncol. 10:748–753. 2003.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Cho N, Moon WK, Cha JH, Kim SM, Kim SJ,
Lee SH, Chung HK, Cho KS, Park IA and Noh DY: Sonographically
guided core biopsy of the breast: Comparison of 14-gauge automated
gun and 11-gauge directional vacuum-assisted biopsy methods. Korean
J Radiol. 6:102–109. 2005.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Yen TW, Hunt KK, Ross MI, Mirza NQ,
Babiera GV, Meric-Bernstam F, Singletary SE, Symmans WF, Giordano
SH, Feig BW, et al: Predictors of invasive breast cancer in
patients with an initial diagnosis of ductal carcinoma in situ: A
guide to selective use of sentinel lymph node biopsy in management
of ductal carcinoma in situ. J Am Coll Surg. 200:516–526.
2005.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Cox D, Bradley S and England D: The
significance of mammotome core biopsy specimens without
radiographically identifiable microcalcification and their
influence on surgical management-a retrospective review with
histological correlation. Breast. 15:210–218. 2006.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Dillon MF, McDermott EW, Quinn CM,
O'Doherty A, O'Higgins N and Hill AD: Predictors of invasive
disease in breast cancer when core biopsy demonstrates DCIS only. J
Surg Oncol. 93:559–563. 2006.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Rutstein LA, Johnson RR, Poller WR, Dabbs
D, Groblewski J, Rakitt T, Tsung A, Kirchner T, Sumkin J, Keenan D,
et al: Predictors of residual invasive disease after core needle
biopsy diagnosis of ductal carcinoma in situ. Breast J. 13:251–257.
2007.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Trentin C, Dominelli V, Maisonneuve P,
Menna S, Bazolli B, Luini A and Cassano E: Predictors of invasive
breast cancer and lymph node involvement in ductal carcinoma in
situ initially diagnosed by vacuum-assisted breast biopsy:
Experience of 733 cases. Breast. 21:635–640. 2012.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Mustafa RE, DeStefano LM, Bahng J,
Yoon-Flannery K, Fisher CS, Zhang PJ, Tchou J, Czerniecki BJ and De
La Cruz LM: Evaluating the risk of upstaging HER2-positive DCIS to
invasive breast cancer. Ann Surg Oncol. 24:2999–3003.
2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Di Cesare P, Pavesi L, Villani L,
Battaglia A, Da Prada GA, Riccardi A and Frascaroli M: The
relationships between HER2 overexpression and DCIS characteristics.
Breast J. 23:307–314. 2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Monabati A, Sokouti AR, Noori SN, Safaei
A, Talei AR, Omidvari S and Azarpira N: Large palpable ductal
carcinoma in situ is Her-2 positive with high nuclear grade. Int J
Clin Exp Pathol. 8:3963–3970. 2015.PubMed/NCBI
|