Introduction
Sarcomas are tumors originating from the connective
tissue matrix, being relatively rare but very invasive (1). Approximately 40% of the sarcomas occur
in the lower extremities, 20% in the upper extremities (1). They are very rare in adults, accounting
for approximately 1% of the cancers of this population (2) but represent 21% of malignant soft
tissue tumors in the pediatric population (3). In this population, the most common
sarcomas are rhabdomyosarcoma and synovial sarcoma (3).
Because of its heterogeneity, it is difficult to
define the diagnostic profile of this disease (4). Most sarcomas demonstrate predilection
for metastases to the lungs, liver, bones, subcutaneous tissue and
lymph nodes (5). However, high-grade
sarcomas are associated with a higher incidence of pulmonary
metastases, as well as an increased risk of local recurrence and
lower survival rates (6). The
decision to remove lung metastases through surgery should be made
based on the disease-free period after primary surgery, absence of
other metastases, number of lesions in each lung, tumor growth, and
disease evolution (7).
Advances in target therapies and studies in
molecular pathogenesis have led to an increase in the therapeutic
arsenal for the treatment of sarcomas. Immunotherapy has been shown
to be a potential therapeutic option for the management of cancer
patients. Nivolumab is a specific molecular target
immunotherapeutic that binds to programmed cell death protein 1
(PD-1), thereby preventing the PD-1 receptor on T lymphocytes from
being activated, what would cause the interruption of the immune
attack on cancer cells (8). However,
there is still insufficient information on the action of
immunotherapy on sarcomas (3). The
aim of this paper is to describe a successful treatment to synovial
sarcoma using immunotherapy with an anti PD-1 drug. We present the
case of a patient diagnosed with soft tissue sarcoma (STS) with
pulmonary metastasis treated with nivolumab 19 months ago with good
response and without considerable side effects.
Case report
A 16-year-old male patient presented to the Clinical
Oncology Service in December 2013, with a lesion in the right arm,
diagnosed by immunohistochemistry (IHC) as a grade III STS. The
patient had already undergone surgery for resection of the tumor in
October of 2013, but has presented recurrence in two months.
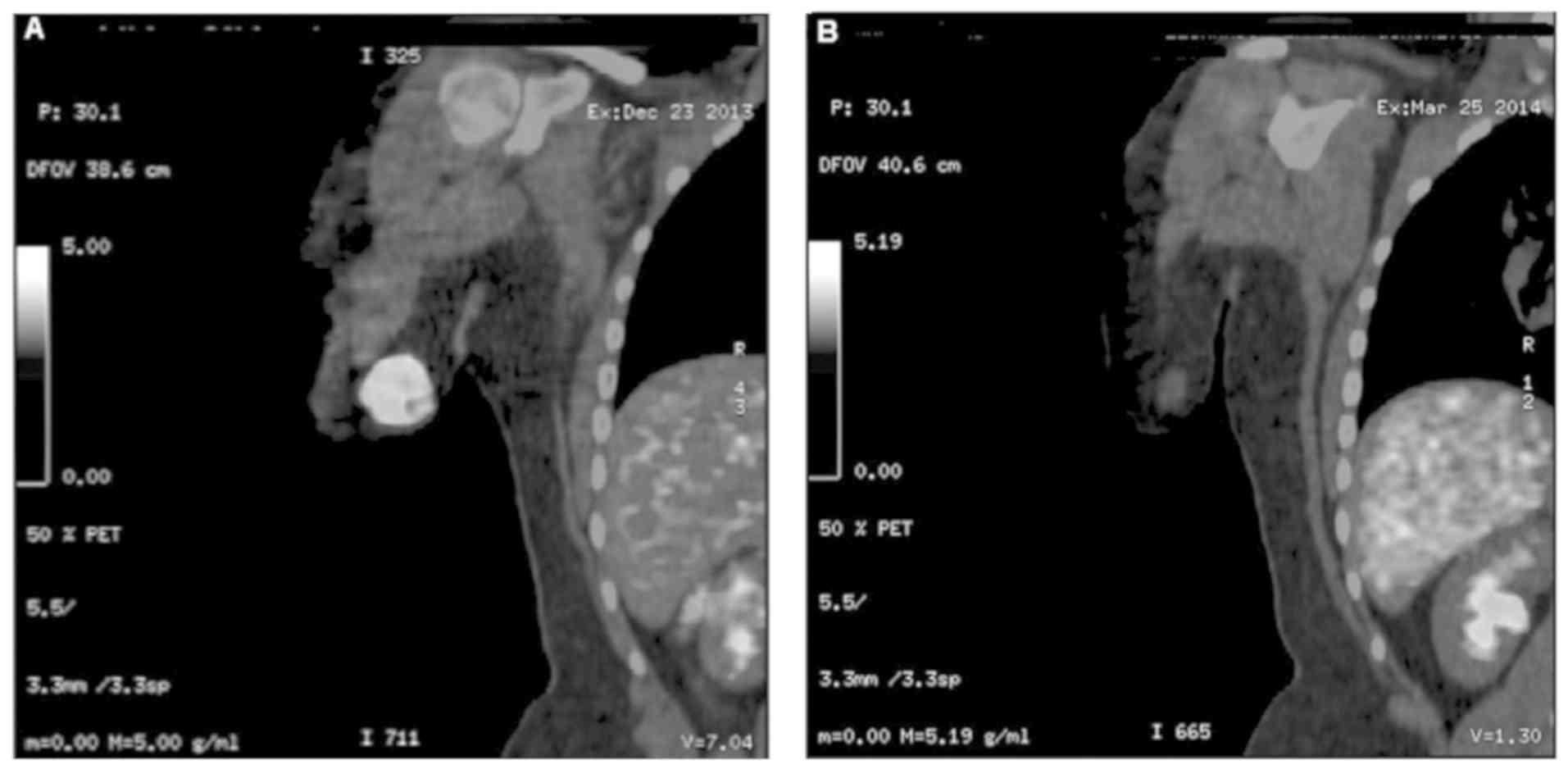
positron emission tomography-computed tomography (PET-CT) revealed
a nodule measuring 3.5 cm (SUV=8.8) in the middle third of the
right arm, characterizing recurrence of the lesion (Fig. 1A). Chemotherapy was initiated with
ifosfamide (5 mg/m2) and adriamycin (75
mg/m2) every 21 days for 4 cycles.
In April 2014, a new PET-CT showed reduction in the
volumetric dimensions of the lesion (from 3.5 to 2.0 cm) associated
to the hypercaptation degree regression (SUV=2,3), meaning residual
neoplastic activity (Fig. 1B).
Therefore, a new surgical treatment was indicated, in which all
residual lesions were removed. Subsequently, the patient was
referred to Intensity-Modulated Radiation Therapy (IMRT)
radiotherapy, with a dose of 60 Gy in a tumor bed with margin, in
30 fractions daily of 2 Gy, 5 times a week (Fig. 1A and B).
In July 2015, a computed tomography (CT) scan of the
thorax revealed peripheral pulmonary micronodules measuring 0.9 and
0.8 cm in the right lower lobe (Fig.
2A). The resection of the largest pulmonary nodule has shown
undifferentiated malignant neoplasm and the IHQ was compatible with
grade III STS.
Pharmacogenomic evaluation, sequencing a panel of
409 genes associated with cancer for the evaluation of mutations
was performed in October 2015, out of genomic DNA extracted from
the resected tumor and DNA extracted from samples of leucocytes of
the blood. Each DNA sample is amplified in 4 reactions. The
products of such are sequenced in parallel and then analyzed by
software. The test did not present mutations associated with
increased sensitivity to treatment with molecular target therapies.
However, IHQ showed a large amounts of the Immune Checkpoint PD-1
binding protein (L), which inhibit programmed cell death 1 ligand 1
(PD-L1). Elevated levels of this ligand in tumor tissues, such as
those found in our patient, indicate sensitivity of cancer cells to
Immune Checkpoints Inhibitors of PD-1 and PD-L1.
Thus, in December 2016, immunotherapy with nivolumab
(3 mg/kg in D1 and D15)-preceded by two-days administration of
Fexofenadine 120 mg (one tablet twice a day)-was initiated.
In July 2017, it was performed a new CT scan of the
torax, which showed an increase in the left axillary lymph node
(Fig. 2B), but the biopsy revealed
only reactive lymphoid hyperplasia. Currently, the patient is in
the 42nd cycle of immunotherapy with nivolumab, being asymptomatic
and leading a normal life, participating, for example, in aquatic
marathons (Fig. 2A and B). Common side effects for nivolumab
therapy, such as fatigue, musculoskeletal pain and lymphocitopenia
have not been observed throughout follow-up.
Discussion
Approximately 70% of all cases of synovial sarcomas
occur in the extremities of the body (9). STS management requires a
multidisciplinary evaluation, with surgical treatment being the
standard modality, associated to auxiliary therapies such as
radiotherapy and adjuvant chemotherapy (10). The literature recommends the
anthracycline plus ifosfamide program in three cycles, as adjuvant
therapy to surgical treatment (11),
which corroborates to the medical management adopted in our
patient. Patients with sarcomas at the extremities appear to be the
major beneficiaries of this therapy (surgery plus adjuvancy)
(10). Studies have shown efficacy
of this adjuvant chemotherapy in STS, with a reduction in the
absolute risk of death by 6% when compared to the isolated therapy
of doxorubicin plus ifosfamide (12-14).
However, many of the patients with high-grade
sarcomas still develop metastases (15), which limits the therapeutic
possibilities, with the lungs being the main sites (15). The clinical state of our patient
followed the same pattern described in the literature (16,17),
that is, recurrence of lesions and appearance of metastases,
especially in the lungs. Patients with metastatic synovial sarcomas
present survival of 7 to 37 months, depending on factors such as
lymph node involvement and localization of metastases (18). To date, our patient has been in
maintenance of the metastatic framework for 36 months, and 57
months the diagnosis of STS.
Due to the high positivity for the PD-L1 marker in
the neoplastic tissue, observed in immunohistochemical analysis,
the option for immunotherapy with nivolumab was a viable choice. A
cohort study evaluating 28 patients with metastatic sarcomas
treated with nivolumab with or without the tyrosine kinase
inhibitor (pazopanib) showed evidence of clinical benefits after
four cycles (19) of nivolumab. Two
other studies were presented at the ASCO 2016 meeting, using
pembrolizumab and nivolumab in patients with sarcomas (20,21).
However, advances using immunotherapy in sarcomas are still
limited, largely due to the heterogeneity of sarcomas (22).
Our results in this case, with the introduction of
an immune checkpoint inhibitor, suggest that more studies with
immunotherapeutics that target PD-1/PD-L1 overexpression could
offer an alternative treatment for patients with STS in order to
provide a longer survival with quality of life for these patients.
Tumor mutation burden (TMB) variation was not investigated
throughout this case, due to financial circumstances of the
patient's family. Further studies are also needed to establish
definitive therapy for STS that do not respond to chemotherapy.
Acknowledgements
Not applicable.
Funding
The present study was supported by Oncológica of
Brasil Education and Research.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
TGF and TCP reviewed the literature, collected and
interpreted the data, wrote the manuscript and conceived the study.
PBTO reviewed the literature, wrote the manuscript and conceived
the study. LEWC and NHY contributed to the conception and design of
the study, and reviewed the methodology. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Formal written consent was obtained for the present
case report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Henshaw RM (ed.): Sarcoma: A
Multidisciplinary Approach to Treatment. Springer, Cham, 2017.
|
|
2
|
Somaiah N and von Mehren M: New drugs and
combinations for the treatment of soft-tissue sarcoma: A review.
Cancer Manag Res. 4:397–411. 2012.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Uehara T, Fujiwara T, Takeda K, Kunisada
T, Ozaki T and Udono H: Immunotherapy for bone and soft tissue
sarcomas. Biomed Res Int. 2015(820813)2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Demicco EG, Maki RG, Lev DC and Lazar AJ:
New therapeutic targets in soft tissue sarcoma. Adv Anat Pathol.
19:170–180. 2012.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Amankwah EK, Conley AP and Reed DR:
Epidemiology and therapies for metastatic sarcoma. Clin Epidemiol.
5:147–162. 2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Welter S, Grabellus F, Bauer S, Schuler M,
Eberhardt W, Tötsch M and Stamatis G: Growth patterns of lung
metastases from sarcoma: Prognostic and surgical implications from
histology. Interact Cardiovasc Thorac Surg. 15:612–617.
2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
ESMO/European Sarcoma Network Working
Group. Soft tissue and visceral sarcomas: Esmo clinical practice
guidelines for diagnosis, treatment and follow-up. Ann Oncol.
25(Suppl 3):iii102–iii112. 2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Sharma P, Retz M, Siefker-Radtke A, Baron
A, Necchi A, Bedke J, Plimack ER, Vaena D, Grimm MO, Bracarda S, et
al: Nivolumab in metastatic urothelial carcinoma after platinum
therapy (CheckMate 275): A multicentre, single-arm, phase 2 trial.
Lancet Oncol. 18:312–322. 2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Nielsen TO, Poulin NM and Ladanyi M:
Synovial sarcoma: Recent discoveries as a roadmap to new avenues
for therapy. Cancer Discov. 5:124–134. 2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Brunello A, Rizzato MD, Rastrelli M, Roma
A, Maruzzo M, Basso U, Fiduccia P, Buzzaccarini MS, Scarzello G,
Rossi CR and Zagonel V: Adjuvant chemotherapy for soft tissue
sarcomas: A 10-year mono-institutional experience. J Cancer Res
Clin Oncol. 142:679–685. 2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Guest JF, Panca M, Sladkevicius E, Gough N
and Linch M: Cost effectiveness of first-line treatment with
doxorubicin/ifosfamide compared to trabectedin monotherapy in the
management of advanced soft tissue sarcoma in Italy, Spain, and
Sweden. Sarcoma. 2013(725305)2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Pervaiz N, Colterjohn N, Farrokhyar F,
Tozer R, Figueredo A and Ghert M: A systematic meta-analysis of
randomized controlled trials of adjuvant chemotherapy for localized
resectable soft-tissue sarcoma. Cancer. 113:573–581.
2008.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Casali PG: Adjuvant chemotherapy for soft
tissue sarcoma. Am Soc Clin Oncol Educ Book. e629–e633.
2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Pasquali S and Gronchi A: Neoadjuvant
chemotherapy in soft tissue sarcomas: Latest evidence and clinical
implications. Ther Adv Med Oncol. 9:415–429. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Zagars GK, Ballo MT, Pisters PW, Pollock
RE, Patel SR, Benjamin RS and Evans HL: Prognostic factors for
patients with localized soft-tissue sarcoma treated with
conservation surgery and radiation therapy An analysis of 1225
patients. Cancer. 97:2530–2543. 2003.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Vlenterie M, Litière S, Rizzo E, Marréaud
S, Judson I, Gelderblom H, Le Cesne A, Wardelmann E, Messiou C,
Gronchi A and van der Graaf WT: Outcome of chemotherapy in advanced
synovial sarcoma patients: Review of 15 clinical trials from the
European organisation for research and treatment of cancer soft
tissue and bone sarcoma group; setting a new landmark for studies
in this entity. Eur J Cancer. 58:62–72. 2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Spurrell E, Fisher C, Thomas JM and Judson
IR: Prognostic factors in advanced synovial sarcoma: An analysis of
104 patients treated at the Royal Marsden Hospital. Ann Oncol.
16:437–444. 2005.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Salah S, Yaser S, Salem A, Al Mousa A, Abu
Sheikha A and Sultan I: Factors influencing survival in metastatic
synovial sarcoma: Importance of patterns of metastases and the
first-line chemotherapy regimen. Med Oncol. 30(639)2013.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Paoluzzi L, Cacavio A, Ghesani M,
Karambelkar A, Rapkiewicz A, Weber J and Rosen G: Response to
anti-PD1 therapy with nivolumab in metastatic sarcomas. Clin
Sarcoma Res. 6(24)2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Tawbi HAH, Burgess MA, Crowley J, Van Tine
BA, Hu J, Schuetze S, D'Angelo SP, Attia S, Priebat DA, Okuno SH,
et al: Safety and efficacy of PD-1 blockade using pembrolizumab in
patients with advanced soft tissue (STS) and bone sarcomas (BS):
Results of SARC028-A multicenter phase II study. J Clin Oncol.
34(11006)2016.
|
|
21
|
George S, Barysauskas CM, Solomon S,
Tahlil K, Malley R, Hohos M, Polson K, Loucks M, Wagner AJ, Merriam
P, et al: Phase 2 study of nivolumab in metastatic leiomyosarcoma
of the uterus. J Clin Oncol. 34(11007)2016.
|
|
22
|
Bleloch JS, Ballim RD, Kimani S, Parkes J,
Panieri E, Willmer T and Prince S: Managing sarcoma: Where have we
come from and where are we going? Ther Adv Med Oncol. 9:637–659.
2017.PubMed/NCBI View Article : Google Scholar
|