Introduction
Paraganglioma, referred to as chromaffin
cell-related tumor located outside the adrenal gland (1), originates from the neuroectoderma
cells of the sympathetic nervous system (2) and may occur in retroperitoneum,
mediastinum, skull and also bladder (3). Accounting for about 10% of
extraadrenal paraganglioma and 0.06% of all bladder tumors
(1,4), bladder paragangliomas are very rare,
with only about 200 cases reported worldwide for now (5). They may occur in patients of all ages,
but typically at the age of 20-50 years, and more in female
patients than male ones (5).
Bladder paragangliomas can be occasionally found
during physical examination, presenting with no clinical symptoms,
and also may show paroxysmal hypertension, hematuria and other
clinical manifestations (6).
Because of the low incidence and usually atypical symptoms, they
are easily misdiagnosed and may further lead to trouble with
treatment. Surgical resection is the most effective way of
treatment, but the approaches of surgical resection remain
contradictory. Most urologists believe partial cystectomy is the
safer way of tumor resection, but there are also many proponents of
transurethral resection, claiming it's more minimally invasive and
also safe enough (7). Therefore, we
summarized and analyzed the 4 cases of bladder paraganglioma
surgically treated at this institution in recent years, in order to
help urologists with management of similar cases.
Patients and methods
Clinical data of all the bladder paraganglioma
patients who underwent operation in recent years in Peking
University Shenzhen Hospital were reviewed. All cases were
confirmed pathologically. We summarized the key points of clinical
diagnosis and treatments of bladder paraganglioma by analyzing
their epidemiological features, symptoms, imaging, laboratory
tests, treatments, pathology and immunohistochemistry, and also
follow-up outcomes. The informed consent was obtained from every
patient, and the study was approved by the Ethics Committees of
Peking University Shenzhen Hospital.
Results
In total, there were 4 bladder paraganglioma
patients who underwent surgical treatments from 2012-2018 at this
institution. All of them were female. Their ages ranged from 28-54
years, averagely 47.25 years old. The following are their case
reports.
Case 1
No. 1 patient was a 54 years old woman. The patient
complained of paroxysmal headache and palpitation, which often
occurred during urinating, together with cold limbs, sweating and
hypertension (220/115 mmHg), and usually disappeared spontaneously
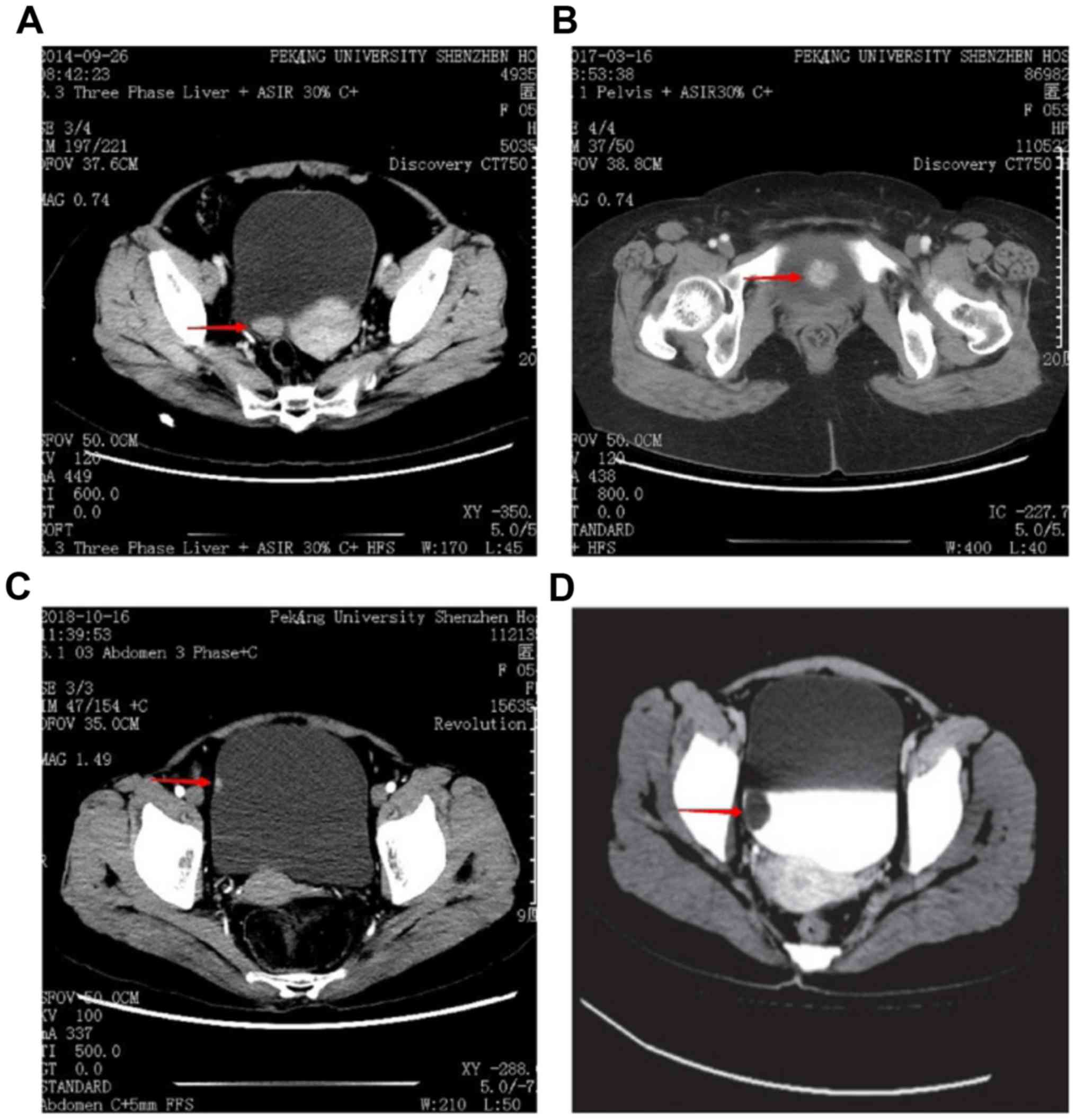
in 2-3 min. Enhanced computed tomography (CT) (Fig. 1A) before operation revealed a
solitary, round-like and intensely enhancing lesion located on the
posterior wall of bladder, with a size of 25x10 mm. The tumor
showed smooth surface in cystoscopy examination. Because of the
typical symptoms, she was suspected as paraganglioma and her blood
catecholamine level was evidently elevated when tested at headache
attacks. Diagnosed successfully before surgery, she was fully
prepared by volume hydration, phentolamine and other
anti-hypertensive medication. Then she underwent partial cystectomy
and the tumor was removed successfully and completely, with her
heart rate and blood pressure stable during the operation.
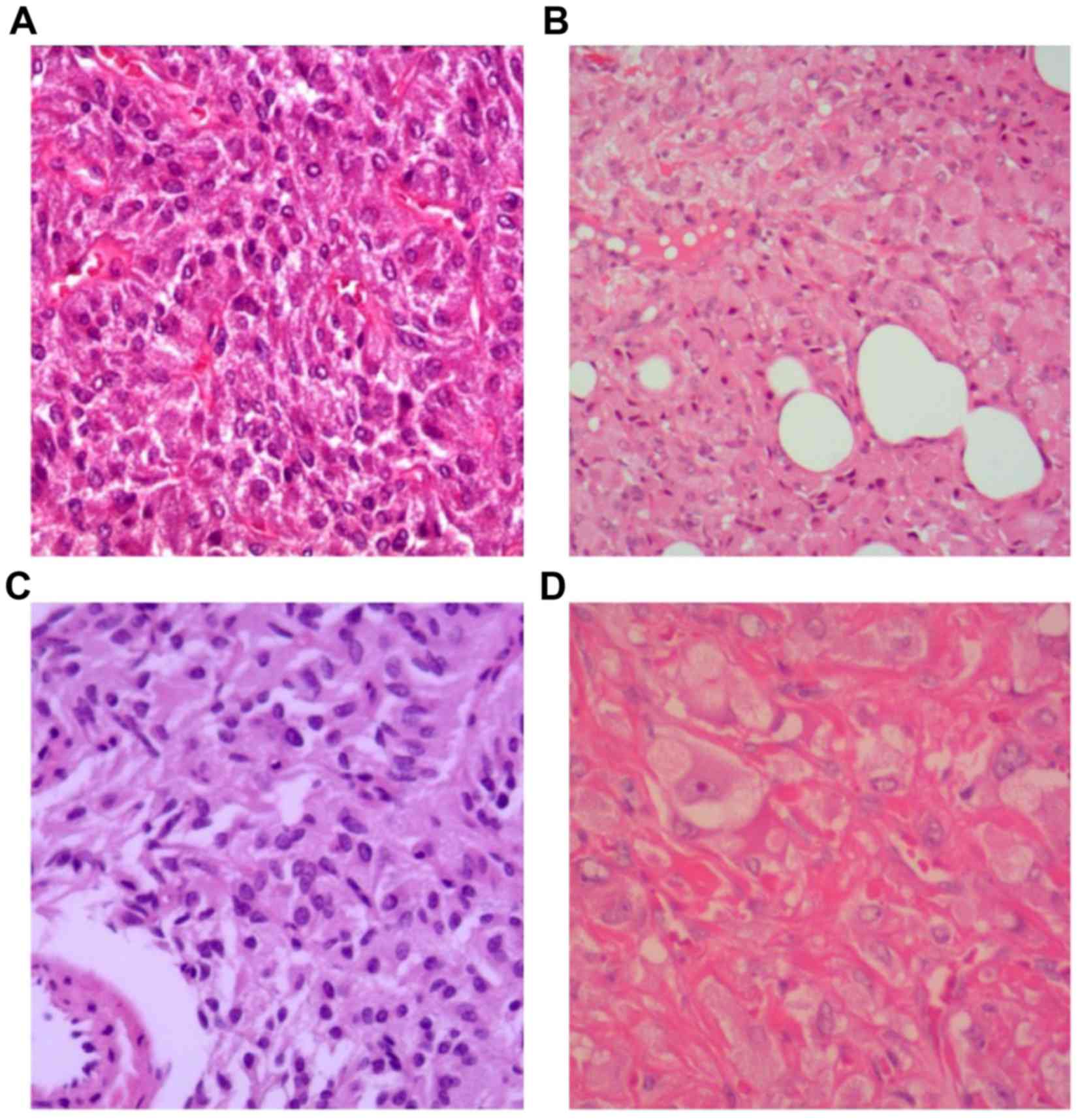
Pathological features are shown in Fig.
2A and further immunohistochemical tests revealed that the
tumor was positive for chromogranin A (CgA) and synaptophysin
(Syn), but CD56 was not did for her. The follow-up lasted for 55
months, during which she had normal blood pressure and no
recrudescence was found.
Case 2
No. 2 patient was 53 years old, female. The main
symptom was painless grass hematuria, with no urethral irritation
symptoms or hypertension. Her CT (Fig.
1B) revealed a 30x20 mm solitary lesion located on the bladder
neck. The tumor had a follicular appearance in cystoscopy. Due to
the absence of symptoms, she was not suspected as paraganglioma
before surgery. No blood catecholamine test or medical preparation
was did for her. Then she underwent transurethral resection, during
which she experienced elevated blood pressure and increased heart
rate distinctly, with complaints of palpitation and nausea.
Nevertheless, the operation was successfully finished with the help
of medical control. No complications occurred after surgery. Her
pathological features are shown in Fig.
2B and immunohistochemical tests of CgA, Syn and CD56 were
positive. She was followed up for 23 months and had no high blood
pressure or tumor recrudescence.
Case 3
No. 3 patient was 54 years old and also female. She
was identified of bladder tumor on a routine physical examination
and had no obvious symptoms or hypertension. Enhanced CT (Fig. 1C) showed a 10x6 mm solitary lesion
on the right side wall of bladder and the tumor surface looked
smooth in cystoscopy. Diagnosed as common bladder tumor before
surgery, no blood catecholamine test or medical preparation was did
for her due to the absence of symptoms. She underwent transurethral
resection had no elevated blood pressure or other problems during
the operation. After surgery, the pathological (Fig. 2C) and further immunohistochemical
reports revealed paraganglioma as CgA, Syn and CD56 were positive.
The follow-up lasted for 6 months and no hypertension or
recrudescence occurred.
Case 4
No. 4 patient was a young female aged 28. She had no
obvious symptom or hypertension and her bladder tumor was
discovered on a routine physical examination. Further examinations
including CT (Fig. 1D) and
cystoscopy demonstrated a solitary, round-like and smooth-surface
tumor on the right side wall of bladder, with a size of 20x20 mm.
She was also not suspected as paraganglioma before surgery and
blood catecholamine tests were missed. She underwent transurethral
resection as common bladder tumor, and elevated blood pressure and
increased heart rate occurred immediately, like no. 2 patient
experienced. Luckily the operation was finished with the help of
medical control with no complications. The pathological results are
shown in Fig. 2D.
Immunohistochemical tests revealed that the tumor was positive for
CgA, Syn and CD56. We followed up her for 69 months and found no
recrudescence or hypertension.
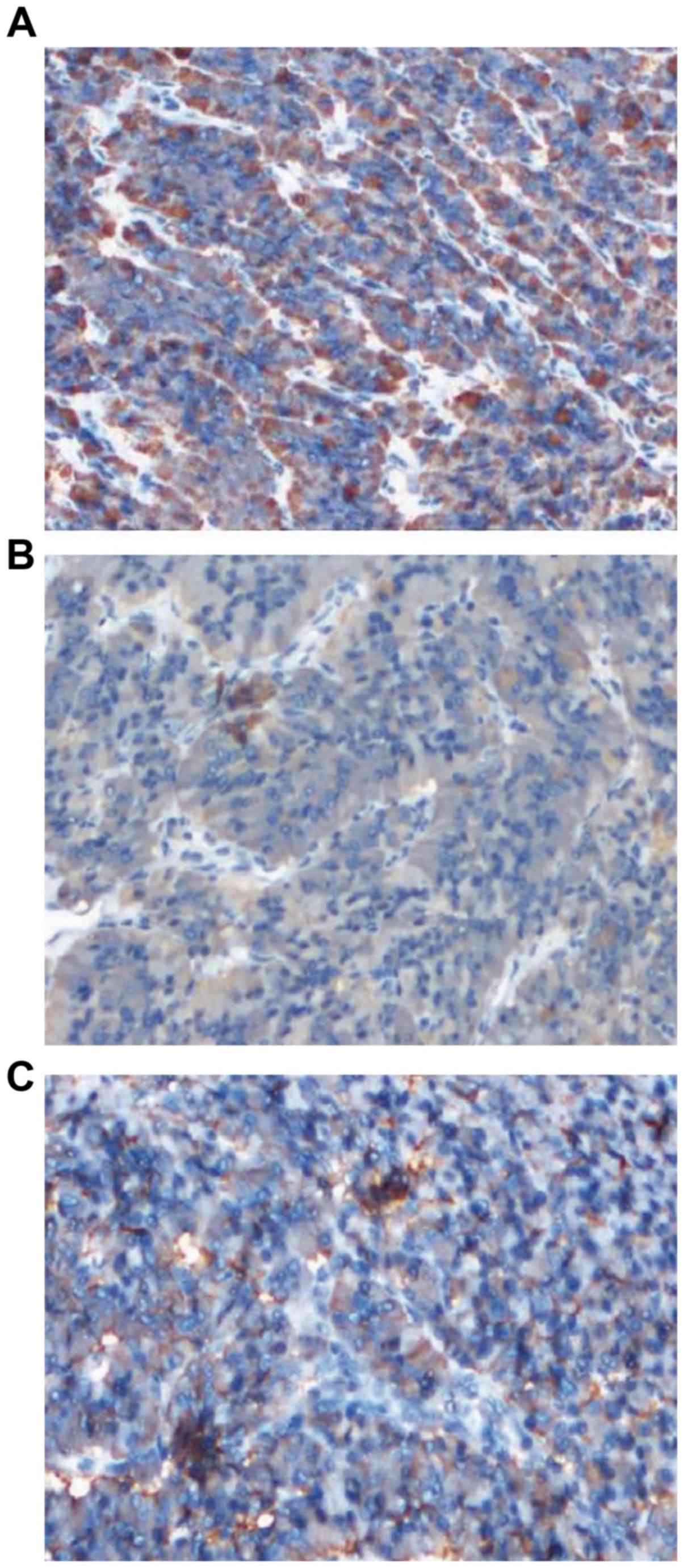
The positive immunohistochemistry for CgA, Syn and
CD56 is shown in Fig. 3, but we
lack figure evidence for urothelium cytokeratin negativity but only
reports.
To make the compares clearer, we summarized their
data in Table I.
 | Table IClinical data of patients with bladder
paraganglioma. |
Table I
Clinical data of patients with bladder
paraganglioma.
| | | | | | | |
Immunohistochemistry |
|---|
| Number | Sex | Age | First
complacation | Tumor location | Tumor size (mm) | Blood
catecholamine | CgA | Syn | CD56 |
|---|
| 1 | Female | 54 | Palpitation,
headache | Posterior wall | 25x10 | Elevated | + | + | None |
| 2 | Female | 53 | Gross hematuria | Bladder neck | 30x20 | None | + | + | + |
| 3 | Female | 54 | None | Right-side wall | 10x6 | None | + | + | + |
| 4 | Female | 28 | None | Right-side wall | 20x20 | None | + | + | + |
Discussion
Paraganglioma is a very rare kind of neoplasm,
accounting for 10% of all chromaffin tumors approximately. It is
estimated that there are only about 800 cases diagnosed in the USA
every year (8). Paraganglioma is
derived from chromaffin tissues of the autonomic nervous system and
therefore often occurs along the sympathetic chain or the organ of
Zuckerkand (3), widely distributed
in many positions like retroperitoneum, bladder, paraaorta, and
pelvic cavity (9). Paragangliomas
in urinary bladder are even rarer, accounting for 10% of all
paraganglioma and 0.06% of all bladder tumors (1,4). Since
Zimmerman described the first bladder paraganglioma in
1953(10), only 200 cases have been
spotted globally (5). Bladder
paragangliomas can be found in all ages, ranging from 11-84 years
as reported, but mostly at the age of 20-50 years (5). Females seem to have a higher incidence
than male, and the ratio is about 3:1(11). The 4 cases at this institution were
all females, aged 28-54 years. Considering the number is too few,
this situation basically correspond to the literature.
Bladder paragangliomas can be functional or
non-functional according to whether catecholamine is over-secreted.
Most of them are functional (83%) (12), with main symptoms include
persistence or paroxysmal hypertension, headache, palpitation and
sweating (13). Paroxysmal
hypertension particularly occurs during micturition, which triggers
the secretion of catecholamine due to increased bladder pressure
caused by bladder contraction, and therefore also called as
‘micturition attacks’. Other common symptoms of bladder
paragangliomas are painless gross hematuria (55-58%), lower urinary
tract irritation symptoms (about 10%) (14), and so on. Non-functional bladder
paragangliomas can be easily misdiagnosed as bladder cancer before
surgery, especially for those with gross hematuria as main
complaint. It is reported that only 28.9% of bladder paraganglioma
were successfully diagnosed before surgery, and 61.6% were
initially suspected as bladder cancer or intramucosal bladder tumor
(15). No. 1 of our patients had
typical symptoms like paroxysmal hypertension and was successfully
diagnosed and fully prepared preoperation, while the others had no
obvious symptom and were finally diagnosed by postoperative
pathology and immunohistochemistry. This reminds urology surgeons
that when finding non-epithelial bladder tumors, paraganglioma must
be taken into consideration.
Adequate medical preparation is very important
before surgery, or hypertensive crisis may happen during the
operation and the mortality risk will increase correspondingly.
Therefore, when paraganglioma is suspected, some endocrine tests
must be conducted, including methoxyadrenaline, adrenaline,
norepinephrine, dopamine and vanillylmandelic acid (VMA) of blood
and urine. However, as catecholamine is secreted intermittently,
positive rate of direct test is too low. It is reported that only
about 60% of paraganglioma cases can be found of ascended urine VMA
and blood catecholamine (15),
which makes the differential diagnosis quite difficult. To improve
the accuracy, respective blood catecholamine tests before, during
and after micturating are suggested (16).
Imaging examinations are also very important for
diagnosis. Ultrasound and CT / Magnetic Resonance Imaging (MRI) are
the basic estimated methods for the shapes, sizes and locations of
the tumors. Ultrasound usually shows clear boundary, wide base and
abundant blood supply. On CT scanning, they mostly have equal or
slightly higher density (17). The
characteristic feature of MRI is slightly higher signal on T1W1,
which is just opposite of adrenal pheochromocytoma, and marked
enhancement on enhanced scanning (18). For the diagnosis of bladder
paraganglioma, CT and MRI have a sensitivity as high as 90-100%,
but relatively lower specificity of 70-80% (19). Besides, some functional imaging
technology can also describe anatomy and function situation of the
tumors and provides even higher value when judging whether tumors
are multiple or metastatic. For example,
I131-methyliodobenzylguanidine (131I-MIBG) and positron emission
tomography (PET) have a sensitivity of 80-95% for diagnosis and
locating and are very effective for finding possible metastasis
(20). But they are used not as
extensive as CT or MRI, mainly limited by the equipments and high
costs.
Pathologically, the tumor cells usually grow in a
characteristic nested pattern, with full and sometimes granular
cytoplasm and surrounded by rich blood vessels (21). But they are still easily confused
with urothelial carcinoma because many of them also show features
like diffuse growth, necrosis and lamina propria infiltration
(22,23). Therefore, immunohistochemistry is
extremely significant for the definitive diagnosis. Neuroendocrine
markers are the most characteristic, like chromogranin A (CgA),
synaptophysin (Syn), neuron-specific enolas (NSE) and CD56(21), while urothelial markers like
cytokeratin (CK) are generally negative (24). Except No. 1 case missed the CD56
test, all our 4 cases are positive in CgA, Syn and CD56 and
negative in CK, corresponding to the literature reports.
Surgical resection is the most effective way of
treatment, including transurethral resection, partial cystectomy
and maybe total cystectomy. If the diagnose of paraganglioma is
basically certain before surgery, it is generally believed that
partial cystectomy is superior to transurethral resection (25). There are two possible reasons for
this. Firstly, transurethral resection will damage the tumor body,
which may lead to excessive release of catecholamine and increase
the risk of hypertensive crisis (26). Secondly, the tumor usually locates
in the very deep layer of bladder wall, therefore transurethral
resection may carry the problem of complete resection and increase
the potential risk of recrudescence (27). Among the 3 transurethral resection
cases at this institution, 2 patients experienced severe
hypertension during operation. Even though they were both fortunate
enough to avoid any complication with the help of active control,
the increasing of risks could not be ignored. Transurethral
resection may be suitable for those non-functional, small and
well-located ones (7).
Surgical resection generally ensures effective
treatment in long term. In a summary involving 75 successfully
followed-up cases, about 20% patients experienced disease
recurrence or metastasis at the time of last follow-up (5). None of our 4 patients were found of
recurrence or metastasis in the 5-69 months of follow-up. Patients
with metastatic tumors can hardly get cured by surgery, but they
can still benefit form surgery by distracting tumor burden and
reducing complications like hypertension. Radiotherapy and
chemotherapy are also necessary for metastatic cases and detailed
plan should be made according to the specific situation of the
patient and disease (28,29). Long-term follow-up is recommended
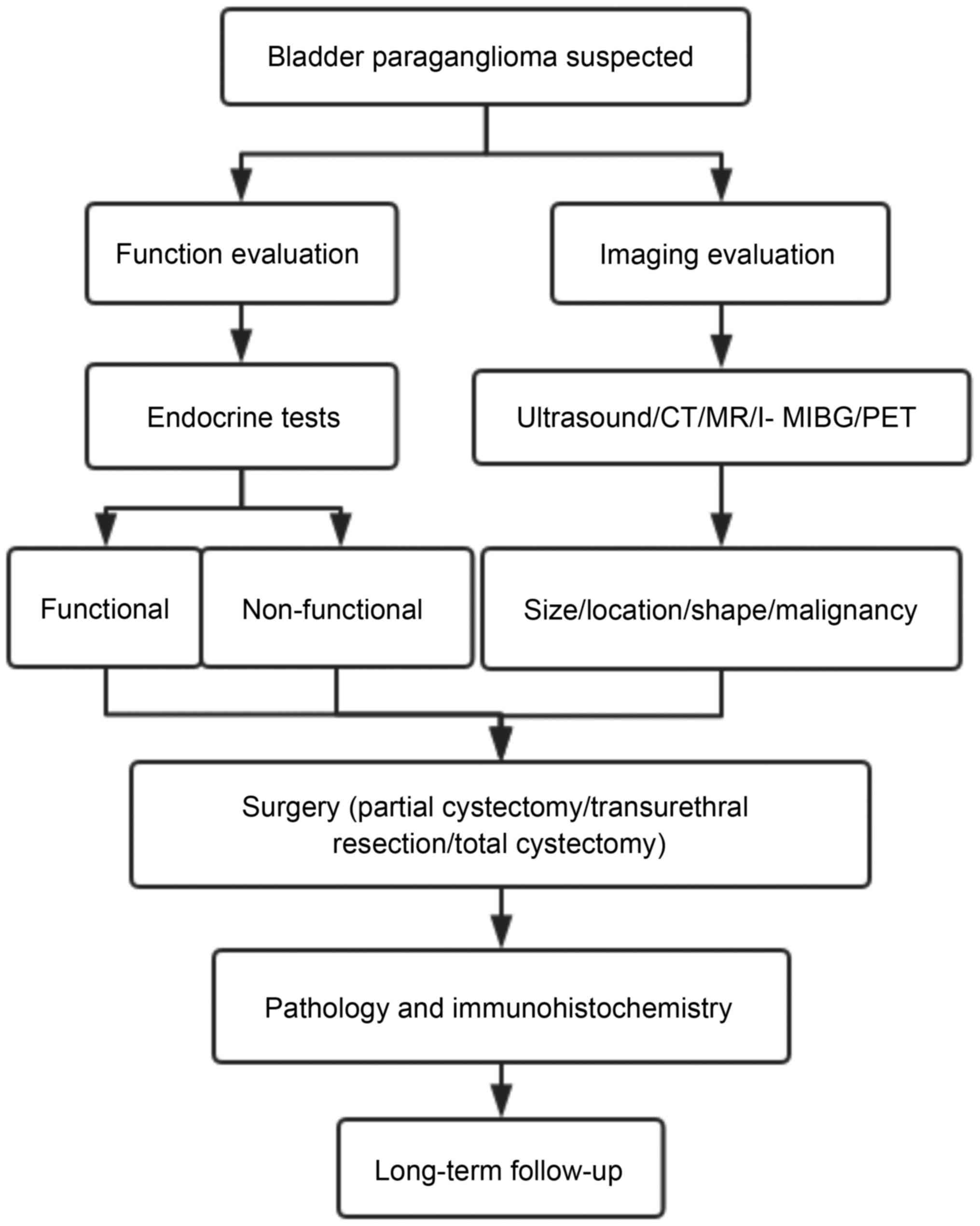
for patients with bladder paraganglioma (30). Fig.
4 is a diagram that summarize the diagnosis and treatment steps
highlighted in our discussion.
In summary, bladder paraganglioma is a very rare
disease with various complications like paroxysmal hypertension,
hematuria and some other symptoms, therefore many are easily
misdiagnosed due to lack of specificity. This disease must be taken
into consideration when non-epithelial bladder tumors are found.
Imaging examination including CT and MRI and laboratory tests like
catecholamine will help to diagnose, but a definitive diagnose
often relies on immunohistochemistry. For treatment, surgical
resection is the most effective method, mostly with satisfactory
results. Adequate reparation before surgery is the key to a steady
and successful operation. For the patients successfully diagnosed
before surgery, partial cystectomy should be given priority. Some
limitations of our study must be considered. Firstly, we lack the
figures of urothelium cytokeratin negativity as evidence. Secondly,
the number of cases is low because of the rare prevalence. A
multicenter study involving enough cases to provide more reliable
proof is needed in the future.
Acknowledgements
Not applicable.
Funding
The current study was supported by Research Fund
Project of Peking University Shenzhen Hospital (grant no.
JCYJ2017001) and Clinical Research Project of Shenzhen Health
Commission (grant no. SZFZ2018072).
Availability of data and materials
The datasets used during the present study are
available from the corresponding author on reasonable request.
Authors' contributions
YL made a substantial contribution to the conception
and design of this study and performed manuscript review. JX
acquired the clinical data and summarized the diagnosis and
treatment procedures. SY and ZC analyzed and interpreted the
patient data regarding management of bladder paraganglioma. HL
participated in the histological examination, was a major
contributor in writing the manuscript, and also analyzed and
interpreted the data of the study. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
The informed consent was obtained from every
patient, and the study was a approved by the Ethics Committees of
Peking University Shenzhen Hospital.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lloyd RV, Osamura RY, Klöppel G and Rosai
J (eds): WHO classification of tumours of endocrine organs. 4th
edition. vol 10:WHO Press. 2017.
|
|
2
|
Young WJ Jr: Paragangliomas: Clinical
overview. Ann N Y Acad Sci. 1073:21–29. 2006.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Lee KY, Oh YW, Noh HJ, Lee YJ, Yong HS,
Kang EY, Kim KA and Lee NJ: Extraadrenal paragangliomas of the
body: Imaging features. AJR Am J Roentgenol. 187:492–504.
2006.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Leestma JE and Price EB Jr: Paraganglioma
of the urinary bladder. Cancer. 28:1063–1073. 1971.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Beilan JA, Lawton A, Hajdenberg J and
Rosser CJ: Pheochromocytoma of the urinary bladder: A systematic
review of the contemporary literature. BMC Urol.
13(22)2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Eisenhofer G, Tischler AS and de Krijger
RR: Diagnostic tests and biomarkers for pheochromocytoma and
extra-adrenal paraganglioma: From routine laboratory methods to
disease stratification. Endocr Pathol. 23:4–14. 2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ahn SG, Jang H, Han DS, Lee JU and Yuk SM:
Transurethral resection of bladder tumour (TURBT) as an optional
treatment method on pheochromocytoma of the urinary bladder. Can
Urol Assoc. J 7:E130–E134. 2013.PubMed/NCBI View
Article : Google Scholar
|
|
8
|
Elder EE, Elder G and Larsson C:
Pheochromocytoma and functional paraganglioma syndrome: No longer
the 10% tumor. J Surg Oncol. 89:193–201. 2005.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Jiang LL, Wu HH, Bu N, Zhang JQ, Zhou LQ
and Guo XH: Analysis of clinical characteristics of paraganglioma
in 42 patients. Zhonghua Yi Xue Za Zhi. 98:280–283. 2018.(In
Chinese). PubMed/NCBI View Article : Google Scholar
|
|
10
|
Zimmerman IJ, Biron RE and Macmahon HE:
Pheochromocytoma of the urinary bladder. N Engl J Med. 249:25–26.
1953.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Yadav R, Das AK and Kumar R: Malignant
non-functional paraganglioma of the bladder presenting with
azotemia. Int Urol Nephrol. 39:449–451. 2007.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Al-Zahrani AA: Recurrent urinary bladder
paraganglioma. Adv Urol. 2010(912125)2010.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Chaaya G, Morales J, Castiglioni A,
Subhani N and Asmar A: Paraganglioma of the urinary bladder: A rare
cause of hypertension and urinary tract infections. Am J Med Sci.
355:191–194. 2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Beysens M, Lapauw B, Gykiere PJ, Dekeyzer
S, Lumen N and Decaestecker K: Minimally invasive approach of
bladder paraganglioma: Case report and review of literature. Austin
J Clin Case Rep. 1(1034)2014.
|
|
15
|
Iwamoto G, Kawahara T, Tanabe M, Ninomiya
S, Takamoto D, Mochizuki T, Kuroda S, Takeshima T, Izumi K, Hattori
Y, et al: Paraganglioma in the bladder: A case report. J Med Case
Rep. 11(306)2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Lecube A, Peña A, Hernández C and Simó R:
.: Bladder pheochromocytoma: A variation in the plasma
catecholamines during micturition. Med Clin (Barc). 112:477–478.
1999.(In Spanish). PubMed/NCBI
|
|
17
|
Vyas S, Kalra N, Singh SK, Agarwal MM,
Mandal AK and Khandelwal N: Pheochromocytoma of urinary bladder.
Indian J Nephrol. 21:198–200. 2011.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Wang H, Ye H, Guo A, Wei Z, Zhang X, Zhong
Y, Fan Z, Wang Y and Wang D: Bladder paraganglioma in adults: MR
appearance in four patients. Eur J Radiol. 80:e217–e220.
2011.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Zeitlin I, Dessau H, Lorberboym M and
Beigel Y: Malignant pheochromocytoma of the urinary bladder:
Challenges in diagnosis and management. Isr Med Assoc J.
13:311–313. 2011.PubMed/NCBI
|
|
20
|
Furuta N, Kiyota H, Yoshigoe F, Hasegawa N
and Ohishi Y: Diagnosis of pheochromocytoma using (123I)-compared
with (131I)-metaiodobenzylguanidine scintigraphy. Int J Urol.
6:119–124. 1999.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Chen CH, Boag AH, Beiko DT, Siemens DR,
Froese A and Isotalo PA: Composite paraganglioma-ganglioneuroma of
the urinary bladder: A rare neoplasm causing hemodynamic crisis at
tumour resection. Can Urol Assoc J. 3:E45–E48. 2009.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Zhou M, Epstein JI and Young RH:
Paraganglioma of the urinary bladder: A lesion that may be
misdiagnosed as urothelial carcinoma in transurethral resection
specimens. Am J Surg Pathol. 28:94–100. 2004.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Menon S, Goyal P, Suryawanshi P,
Tongaonkar H, Joshi A, Bakshi G and Desai S: Paraganglioma of the
urinary bladder: A clinicopathologic spectrum of a series of 14
cases emphasizing diagnostic dilemmas. Indian J Pathol Microbiol.
57:19–23. 2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Priyadarshi V and Pal DK: Paraganglioma of
urinary bladder. Urol Ann. 7:402–404. 2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Bishnoi K, Bora GS, Mavuduru RS, Devana
SK, Singh SK and Mandal AK: Bladder paraganglioma: Safe and
feasible management with robot assisted surgery. J Robot Surg.
10:275–278. 2016.PubMed/NCBI View Article : Google Scholar
|
|
26
|
El-Tholoth HS, Al RS, Alharbi F,
Alshammari W, Alzahrani T and Al Zahrani A: Paraganglioma of
urinary bladder managed by laparoscopic partial cystectomy in
conjunction with flexible cystoscopy: A case report. J Endourol
Case Rep. 4:15–17. 2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Adraktas D, Caserta M and Tchelepi H:
Paraganglioma of the urinary bladder. Ultrasound Q. 30:233–235.
2014.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Dahm P and Gschwend JE: Malignant
non-urothelial neoplasms of the urinary bladder: A review. Eur
Urol. 44:672–681. 2003.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Ibuki N, Komura K, Koyama K, Inamoto T,
Segawa N, Tanimoto K, Tuji M, Azuma H and Katsuoka Y: A
pheochromocytoma of urinary bladder treated with neoadjuvant
chemotherapy. Hinyokika Kiyo. 55:765–768. 2009.(In Japanese).
PubMed/NCBI
|
|
30
|
Zhai H, Ma X, Nie W, Li H, Peng C, Li X,
Zhang Y and Zhang X: Paraganglioma of the urinary bladder: A series
of 22 cases in a single center. Clin Genitourin Cancer.
15:e765–e771. 2017.PubMed/NCBI View Article : Google Scholar
|