Introduction
The role of cytoreductive nephrectomy (CN) in
patients with metastatic renal cell carcinoma (mRCC) was initially
defined during the era of open surgery and first-generation
immunotherapy (e.g., interleukin-2 and interferon α) (1-3).
For some patients with mRCC a survival benefit from CN was not
achieved, while there was increased morbidity as a result of
surgery; therefore, risk factors for prognosis were defined in
order to aid in surgical candidate selection (4,5). Since
then, the landscape of systemic therapy for mRCC has changed
drastically with targeted therapy, such as tyrosine kinase
inhibitors and mammalian target of rapamycin (mTOR) inhibitors, as
the mainstays of treatment (6,7) The
benefit of CN in the era of targeted therapy (TT) was subsequently
defined (8), and noted to be most
pronounced for selected patients (9-11).
In parallel with the advances in systemic therapy
for mRCC, the paradigm for CN has shifted from an open to a
laparoscopic approach (12). The
oncological safety of laparoscopic CN was established during the
first-generation immunotherapy era, and has expanded into the TT
era (13-15).
The reduced convalescence associated with laparoscopic surgery is
particularly important for patients with mRCC, as this may reduce
their time to systemic therapy initiation. However, the interplay
between laparoscopic CN and patient survival has not been studied
in the TT era.
The aim of the present study was to compare the
survival outcomes of laparoscopic CN, open CN and TT alone (for
patients who were deemed unfit for surgery) at our institution
during the TT era.
Patients and methods
Patient information
After obtaining Institutional Review Board approval,
all mRCC patients who received systemic TT between January 2007 and
December 2012 at our institution (n=132) were retrospectively
reviewed. TT patients were defined as those who received tyrosine
kinase inhibitors, mTOR inhibitors and vascular endothelial growth
factor inhibitors. We identified a total of 96 patients who
received CN prior to TT, and 36 patients who received TT alone, as
they were deemed unfit for CN. Laparoscopic CN was performed in 50%
(48/96) of the patients, with the remainder receiving open CN. The
histological subtypes for the CN patients included 71% clear cell,
17% sarcomatoid, 7% papillary type II and 5% other types. Subtype
classification for the patients receiving TT alone could not be
determined, as the patients were diagnosed clinically or on biopsy
of their metastatic site, which presented pathological
limitations.
Patient clinical variables were collected, including
age, adult comorbidity evaluation score (16) and Karnofsky performance status
score. The preoperative risk stratification variables for CN
described by Culp et al and validated by our institutional
experience were also collected (10,11).
These variables included: i) Serum albumin below laboratory normal,
ii) clinical T3 or T4 disease, iii) presence of liver metastasis,
iv) symptomatic metastasis, v) retroperitoneal lymphadenopathy and
vi) supradiaphragmatic lymphadenopathy. Survival data were gathered
using available medical records and the Social Security death
index, with final query on August 31, 2017.
Statistical analysis
Kaplan-Meier-estimated overall survival (OS) was
compared among laparoscopic CN, open CN and TT alone. The OS
end-point was reached by 100% (36/36) of patients in the TT cohort,
98% (47/48) of patients in the open CN cohort, and 96% (46/48) of
patients in the laparoscopic CN cohort. Multivariate Cox
proportional hazards analysis was also performed adjusting for age,
Karnofsky performance status score and preoperative risk
stratification variables. To calculate statistical significance,
the χ2 test was used for categorical variables and the
Student's t-test was used for continuous variables, with P<0.05
considered to indicate statistically significant differences. All
statistical analyses were completed using R software, version
3.2.2.
Results
Patient characteristics
Patient baseline clinical and tumor characteristics
are provided in Table I. The open
CN, laparoscopic CN and TT alone groups differed significantly in
the proportion of patients with Karnofsky performance status score
≤60%, mean number of preoperative risk stratification variables,
proportion of patients with serum albumin ≤3.5 g/dl, clinical stage
>T3, symptomatic metastasis and supradiaphragmatic
lymphadenopathy (P<0.01 in all cases).
 | Table IPatient baseline clinical and tumor
characteristics. |
Table I
Patient baseline clinical and tumor
characteristics.
| Variables | Open CN, n=48 | Laparoscopic CN,
n=48 | TT alone, n=36 | P-value |
|---|
| Mean age (SD),
years | 56.4 (9.2) | 58.8 (12.0) | 57.8 (10.4) | 0.54 |
| Mean ACE score
(SD) | 1.2 (0.8) | 1.0 (1.0) | 1.3 (1.0) | 0.32 |
| Karnofsky performance
status score <60, n (%) | 3/48 (6.3) | 7/48 (14.6) | 12/36(33) | <0.01 |
| Mean preoperative
risk stratification variables (SD) | 2.6 (1.1) | 2.0 (1.3) | 3.1 (1.1) | <0.01 |
| Albumin <3.5 g/dl,
n (%) | 17/48(35) | 10/48(21) | 20/36(56) | <0.01 |
| Clinical stage
>T3, n (%) | 32/48(67) | 17/48(35) | 14/36(39) | <0.01 |
| Liver metastasis, n
(%) | 10/48(21) | 9/48(19) | 11/36(31) | 0.41 |
| Symptomatic
metastasis, n (%) | 20/48(42) | 29/48(60) | 27/36(75) | <0.01 |
| Retroperitoneal LN, n
(%) | 22/48(46) | 15/48(31) | 20/36(56) | 0.08 |
| Supradiaphragmatic
LN, n (%) | 20/48(42) | 13/48(27) | 22/36(61) | <0.01 |
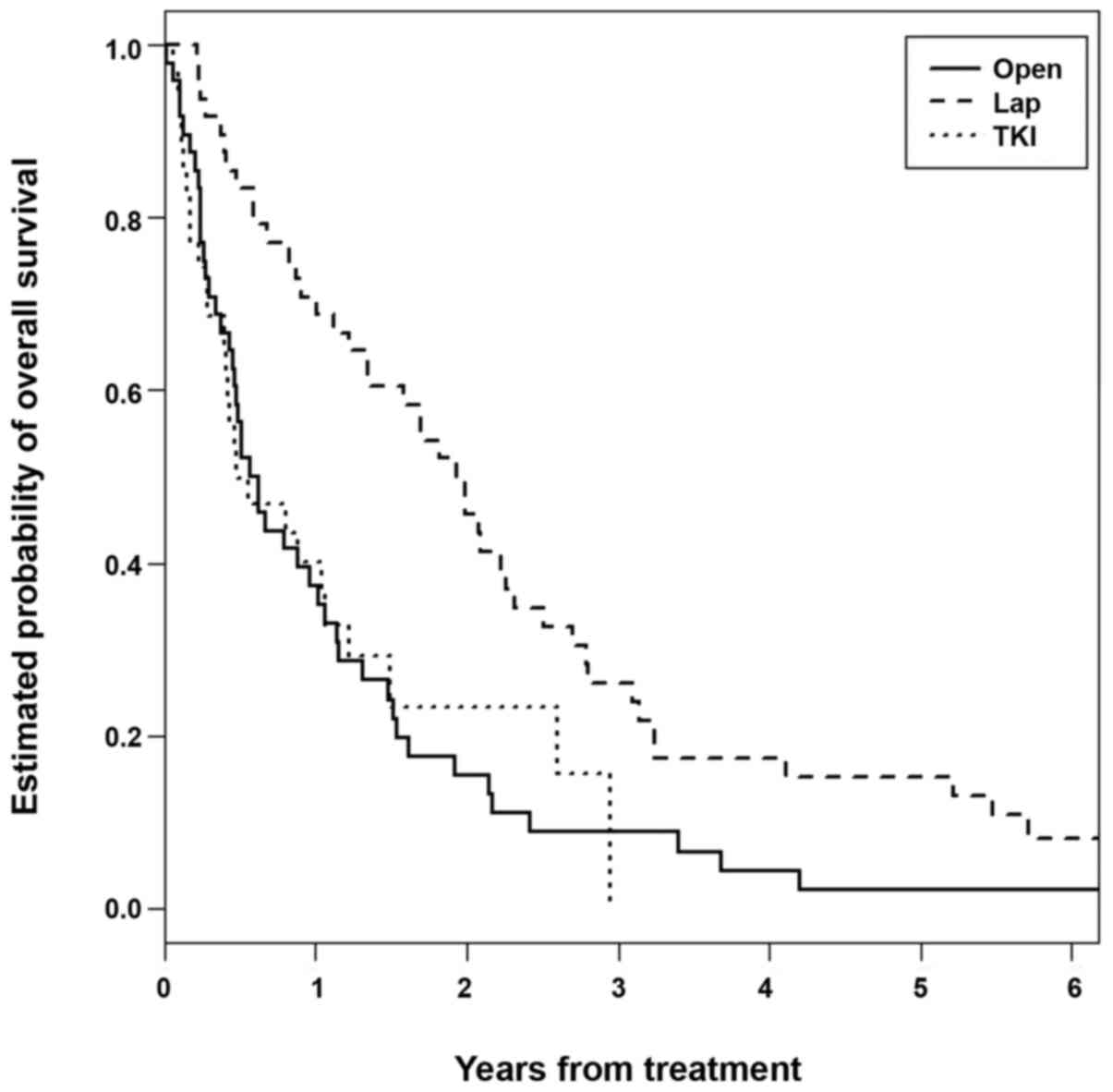
The survival of patients undergoing
laparoscopic CN is superior to that of the other two cohorts
Kaplan-Meier-estimated survival curves are provided
in Fig. 1. The median OS was 23.9
months in the laparoscopic CN group (2 patients censored), 10.8
months in the open CN group (1 patient censored), and 10.7 months
in the TT alone group (P<0.01). Multivariate Cox proportional
hazards analysis identified laparoscopic CN as an independent
predictor of survival (hazard ratio=0.48, 95% confidence interval:
0.31-0.74, P<0.01), controlling for age, Karnofsky performance
status score and the number of preoperative risk stratification
variables.
Median survival was examined with subsets of the
open CN and laparoscopic CN cohorts, which are provided in Table II. When excluding patients with
Karnofsky performance status score ≤60%, the median survival
remained significantly greater for the laparoscopic CN group (27
vs. 11 months, respectively; P<0.01). When additionally
excluding patients with ≥3 preoperative risk stratification
variables, the median survival remained significantly greater for
the laparoscopic CN group (28 vs. 11 months, respectively;
P<0.01). When additionally excluding patients with clinical
stage T3 or T4 disease, the median survival remained significantly
greater for the laparoscopic CN group (29 vs. 12 months,
respectively; P<0.01).
 | Table IIMedian survival for subsets of
patients receiving open and laparoscopic CN. |
Table II
Median survival for subsets of
patients receiving open and laparoscopic CN.
| | Median survival | |
|---|
| Patient subsets | Open CN, n
(months) | Laparoscopic CN, n
(months) | P-value |
|---|
| Entire cohort | 48 (10.8) | 48 (23.9) | <0.01 |
| Karnofsky <60%
excluded | 45 (11.1) | 41 (26.9) | <0.01 |
| >3 risk factors
excluded | 22 (11.4) | 29 (28.3) | <0.01 |
| Clinical stage >T3
excluded | 11 (12.1) | 24 (28.9) | <0.01 |
Discussion
In the present study, laparoscopic CN was found to
be associated with a significant increase in OS compared to open CN
and TT alone, independent of patient and tumor characteristics. To
the best of our knowledge, this is the first direct examination of
the CN approach and its impact on survival. It was demonstrated
that the difference in median survival between laparoscopic and
open CN was ~12 months, while open CN and TT alone exhibited
similar survival. Furthermore, this survival benefit in favor of
laparoscopic over open CN persisted in multivariate and subset
analyses.
The initial studies of laparoscopic CN focused on
its non-inferiority compared with conventional open CN, with
limited numbers of patients and limited oncological follow-up
(13-15).
The studies by Rabets et al and Eisenberg et al
included substantially fewer patients compared with the present
study (n=64, n=27 and n=132, respectively), and only included
1-year estimated survival (14,15).
Furthermore, these studies were performed in the era of
first-generation immunotherapy (e.g., interleukin-2 and interferon
α), which makes their study findings difficult to compare to those
of the present study and contemporary practice for mRCC.
Additionally, the use of laparoscopic nephrectomy and, thus,
laparoscopic CN, has markedly increased since then (12). Zlatev et al reported a
decrease in open CN from 77 to 66% between 2003 and 2015, within
the Premier Hospital Database. Associated with this increase in
utilization, they also found that laparoscopic CN significantly
reduced the rate of blood transfusion [odds ratio (OR)=0.46] and
length of hospital stay (OR=0.50) (17). Similarly, Gershman et al
found that laparoscopic CN significantly reduced the length of
hospital stay (OR=0.12) and, more importantly, significantly
reduced the time to initiation of TT (OR=5.1), when compared to
open CN in their institutional experience (n=294) (18).
Although a number of studies have focused on the
perioperative outcomes following laparoscopic CN, comparatively few
studies have been published on the OS of patients receiving
laparoscopic CN in the TT era. Nunez Bragayrac et al
reported the survival of a contemporary (2001-2013) pooled cohort
of mRCC patients (n=120) receiving laparoscopic CN at three
high-volume cancer centers. The median survival was reported as
25.7 months, with a 3-year survival rate of 35% (19). A similar survival rate was found our
laparoscopic CN cohort, with a median survival of 23.9 months and a
3-year survival rate of 26%. However, with no comparator arm, the
study by Nunez Bragayrac et al did not demonstrate the
comparative survival benefit of laparoscopic CN over open CN or TT
alone.
To the best of our knowledge, the present study is
the first to directly compare OS following laparoscopic CN, open CN
and TT alone in the TT era. Although previous studies have
demonstrated the survival benefit of CN over TT alone (8-11,20,21),
many have argued that the survival benefit is a result of surgeon
selection bias (22,23). Given the retrospective nature of
these studies (including our own), surgeon selection bias cannot be
eliminated, and likely contributes to the survival differences seen
in patients who receive CN. An example of surgeon selection bias
impacting retrospective studies of survival was published by Shuch
et al, who demonstrated that the OS in patients receiving
partial nephrectomy in the Medicare population was improved over
non-cancer controls (24).
Although some patients may not tolerate the
insufflation associated with laparoscopic surgery and some tumors
(i.e., higher clinical T stage) were not amenable to a laparoscopic
approach, we observed that laparoscopic CN was associated with
improved survival independent of these factors from a statistical
standpoint (multivariate model), as well as in a subset analysis.
However, as a retrospective study, confounding variables associated
with surgical selection bias could not be eliminated. Furthermore,
the survival benefit observed with laparoscopic CN was likely a
result of unaccounted for variables, or the value of surgeon
cognitive bias in clinical decision-making. Despite our
single-institution study being adequately powered to detect
statistically significant differences between treatment groups, and
being significantly larger than previously published studies on the
same subject, the overall size of the study (n=132) remains
limited. Of note, by including patients between 2007 and 2012,
nearly all patients in the study (129/132=98%) had reached their
survival end-points.
In conclusion, it was herein demonstrated that
laparoscopic CN was an independent and significant predictor of
survival in mRCC when compared to open CN or TT alone. In our
experience, for patients who were not candidates for laparoscopic
CN, open CN did not confer a survival benefit over TT alone.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
All authors made substantial contributions to this
article. KZ, EHK, JJH, SBB, RSF contributed to the conception and
design of the study. Data collection was performed by JMV and RV.
Data analysis was performed by KZ and EHK. The manuscript was
drafted by KZ and EHK. All authors have revised and corrected the
manuscript. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was performed with Institutional Review
Board approval.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Walther MM, Yang JC, Pass HI, Linehan WM
and Rosenberg SA: Cytoreductive surgery before high dose
interleukin-2 based therapy in patients with metastatic renal cell
carcinoma. J Urol. 158:1675–1678. 1997.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Mickisch GH, Garin A, van Poppel H, de
Prijck L and Sylvester R: European Organisation for Research and
Treatment of Cancer (EORTC) Genitourinary Group. Radical
nephrectomy plus interferon-alfa-based immunotherapy compared with
interferon alfa alone in metastatic renal-cell carcinoma: A
randomised trial. Lancet. 358:966–970. 2001.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Flanigan RC, Salmon SE, Blumenstein BA,
Bearman SI, Roy V, McGrath PC, Caton JR Jr, Munshi N and Crawford
ED: Nephrectomy followed by interferon alfa-2b compared with
interferon alfa-2b alone for metastatic renal-cell cancer. N Engl J
Med. 345:1655–1659. 2001.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Motzer RJ, Mazumdar M, Bacik J, Berg W,
Amsterdam A and Ferrara J: Survival and prognostic stratification
of 670 patients with advanced renal cell carcinoma. J Clin Oncol.
17:2530–2540. 1999.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Fallick ML, McDermott DF, LaRock D, Long
JP and Atkins MB: Nephrectomy before interleukin-2 therapy for
patients with metastatic renal cell carcinoma. J Urol.
158:1691–1695. 1997.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Hsieh JJ, Purdue MP, Signoretti S, Swanton
C, Albiges L, Schmidinger M, Heng DY, Larkin J and Ficarra V: Renal
cell carcinoma. Nat Rev Dis Primers. 3(17009)2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Choueiri TK and Motzer RJ: Systemic
therapy for metastatic renal-cell carcinoma. N Engl J Med.
376:354–366. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Choueiri TK, Xie W, Kollmannsberger C,
North S, Knox JJ, Lampard JG, McDermott DF, Rini BI and Heng DY:
The impact of cytoreductive nephrectomy on survival of patients
with metastatic renal cell carcinoma receiving vascular endothelial
growth factor targeted therapy. J Urol. 185:60–66. 2011.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Heng DY, Xie W, Regan MM, Warren MA,
Golshayan AR, Sahi C, Eigl BJ, Ruether JD, Cheng T, North S, et al:
Prognostic factors for overall survival in patients with metastatic
renal cell carcinoma treated with vascular endothelial growth
factor-targeted agents: Results from a large, multicenter study. J
Clin Oncol. 27:5794–5799. 2009.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Culp SH, Tannir NM, Abel EJ, Margulis V,
Tamboli P, Matin SF and Wood CG: Can we better select patients with
metastatic renal cell carcinoma for cytoreductive nephrectomy.
Cancer. 116:3378–3388. 2010.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Manley BJ, Kim EH, Vetter JM, Potretzke AM
and Strope SA: Validation of preoperative variables and
stratification of patients to help predict benefit of cytoreductive
nephrectomy in the targeted therapy ERA. Int Braz J Urol.
43:432–439. 2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kerbl DC, McDougall EM, Clayman RV and
Mucksavage P: A history and evolution of laparoscopic nephrectomy:
Perspectives from the past and future directions in the surgical
management of renal tumors. J Urol. 185:1150–1154. 2011.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Walther MM, Lyne JC, Libutti SK and
Linehan WM: Laparoscopic cytoreductive nephrectomy as preparation
for administration of systemic interleukin-2 in the treatment of
metastatic renal cell carcinoma: A pilot study. Urology.
53:496–501. 1999.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Rabets JC, Kaouk J, Fergany A, Finelli A,
Gill IS and Novick AC: Laparoscopic versus open cytoreductive
nephrectomy for metastatic renal cell carcinoma. Urology.
64:930–934. 2004.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Eisenberg MS, Meng MV, Master VA, Stoller
ML, Rini BI, Carroll PR and Kane CJ: Laparoscopic versus open
cytoreductive nephrectomy in advanced renal-cell carcinoma. J
Endourol. 20:504–508. 2006.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Piccirillo JF and Feinstein AR: Clinical
symptoms and comorbidity: Significance for the prognostic
classification of cancer. Cancer. 77:834–842. 1996.PubMed/NCBI
|
|
17
|
Zlatev DV, Ozambela M, Salari K, Wang Y,
Mossanen M, Pucheril D, Ingham MD, Chung BI and Chang SL: Trends
and morbidity for minimally invasive versus open cytoreductive
nephrectomy in the management of metastatic renal cell carcinoma. J
Clin Oncol. 36 (Suppl 6)(S632)2018.
|
|
18
|
Gershman B, Moreira DM, Boorjian SA, Lohse
CM, Cheville JC, Costello BA, Leibovich BC and Thompson RH:
Comprehensive characterization of the perioperative morbidity of
cytoreductive nephrectomy. Eur Urol. 69:84–91. 2016.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Nunez Bragayrac L, Hoffmeyer J, Abbotoy D,
Attwood K, Kauffman E, Spiess P, Wagner A and Schwaab T: Minimally
invasive cytoreductive nephrectomy: A multi-institutional
experience. World J Urol. 34:1651–1656. 2016.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Zini L, Capitanio U, Perrotte P, Jeldres
C, Shariat SF, Arjane P, Widmer H, Montorsi F, Patard JJ and
Karakiewicz PI: Population-based assessment of survival after
cytoreductive nephrectomy versus no surgery in patients with
metastatic renal cell carcinoma. Urology. 73:342–346.
2009.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Hanna N, Sun M, Meyer CP, Nguyen PL, Pal
SK, Chang SL, de Velasco G, Trinh QD and Choueiri TK: Survival
analyses of patients with metastatic renal cancer treated with
targeted therapy with or without cytoreductive nephrectomy: A
national cancer data base study. J Clin Oncol. 34:3267–3275.
2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Stewart GD, Aitchison M, Bex A, Larkin J,
Lawless C, Méjean A, Nathan P, Oades G, Patard JJ, Paul J, et al:
Cytoreductive nephrectomy in the tyrosine kinase inhibitor era: A
question that may never be answered. Eur Urol. 71:845–847.
2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Pindoria N, Raison N, Blecher G,
Catterwell R and Dasgupta P: Cytoreductive nephrectomy in the era
of targeted therapies: A review. BJU Int. 120:320–328.
2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Shuch B, Hanley J, Lai J, Vourganti S, Kim
SP, Setodji CM, Dick AW, Chow WH and Saigal C: Urologic Diseases in
America Project. Overall survival advantage with partial
nephrectomy: A bias of observational data? Cancer. 119:2981–2989.
2013.PubMed/NCBI View Article : Google Scholar
|