Introduction
Patients with cancer are at high risk of developing
deep vein thrombosis (DVT), which occurs mostly in the lower
extremities and rarely in the upper extremities (1). Approximately 4-10% of all cases of DVT
involve the subclavian, axillary, or brachial veins. The use of a
central venous catheter (CVC) improves the management of patients
with cancer. However, the presence of CVC increases the risk of
developing upper extremity DVT (UEDVT) and its associated
complications, such as pulmonary embolism (PE) (1). Although development of DVT after
placement of an indwelling CVC has been commonly reported (2), there are few reports of DVT occurring
after the placement of an indwelling CV port in patients with soft
tissue sarcoma (STS).
For the effective management of high-grade STS,
surgical tumor resection combined with neoadjuvant chemotherapy is
recommended and the placement of an indwelling CV port may also be
considered (3). We herein report
the clinical course of a patient with STS of the thigh who
developed UEDVT following indwelling CV port placement.
Case report
A 66-year-old man visited a local clinic in November
2012, 1 month after noticing a mass developing in his right thigh.
The patient was referred to the Department of Orthopedic Surgery at
Mie University Hospital on suspicion of STS. On physical
examination, a swelling was identified on the lateral side of the
right thigh. There was no fever, tenderness, or redness.
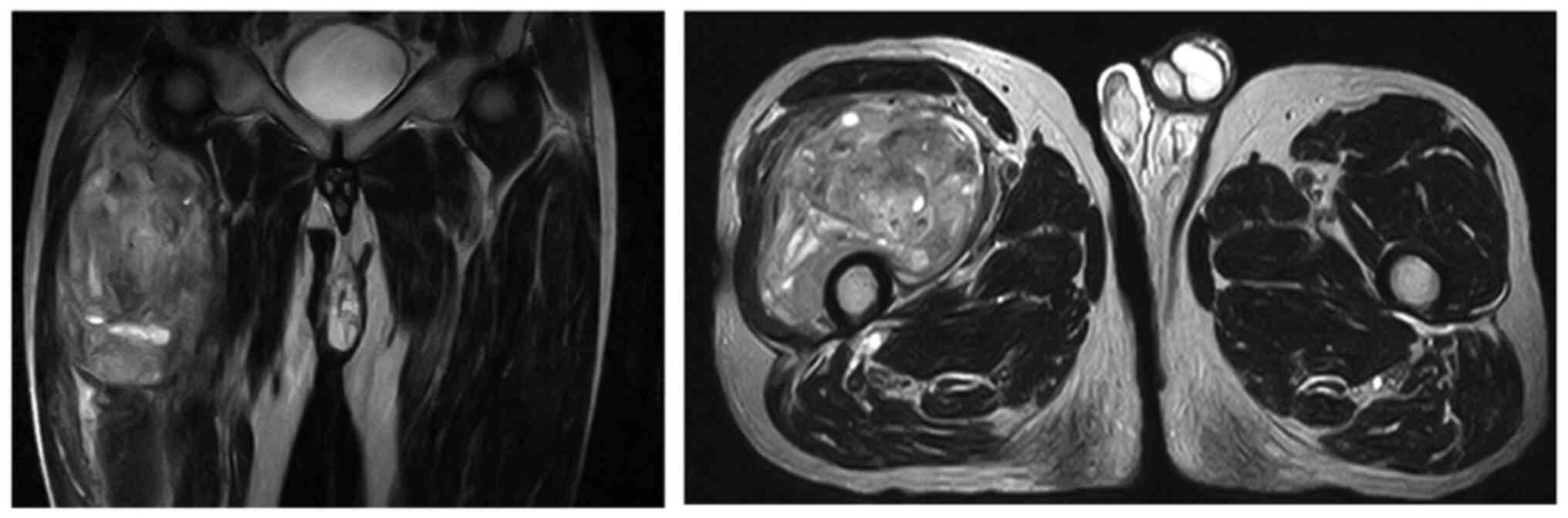
Magnetic resonance imaging examination revealed a
soft tissue mass that involved the vastus lateralis and vastus
intermedius muscles, and exhibited low signal intensity on
T1-weighted images and heterogenous signal intensity on T2-weighted
images; the administration of gadolinium enhanced the heterogeneous
signal intensity (Fig. 1).
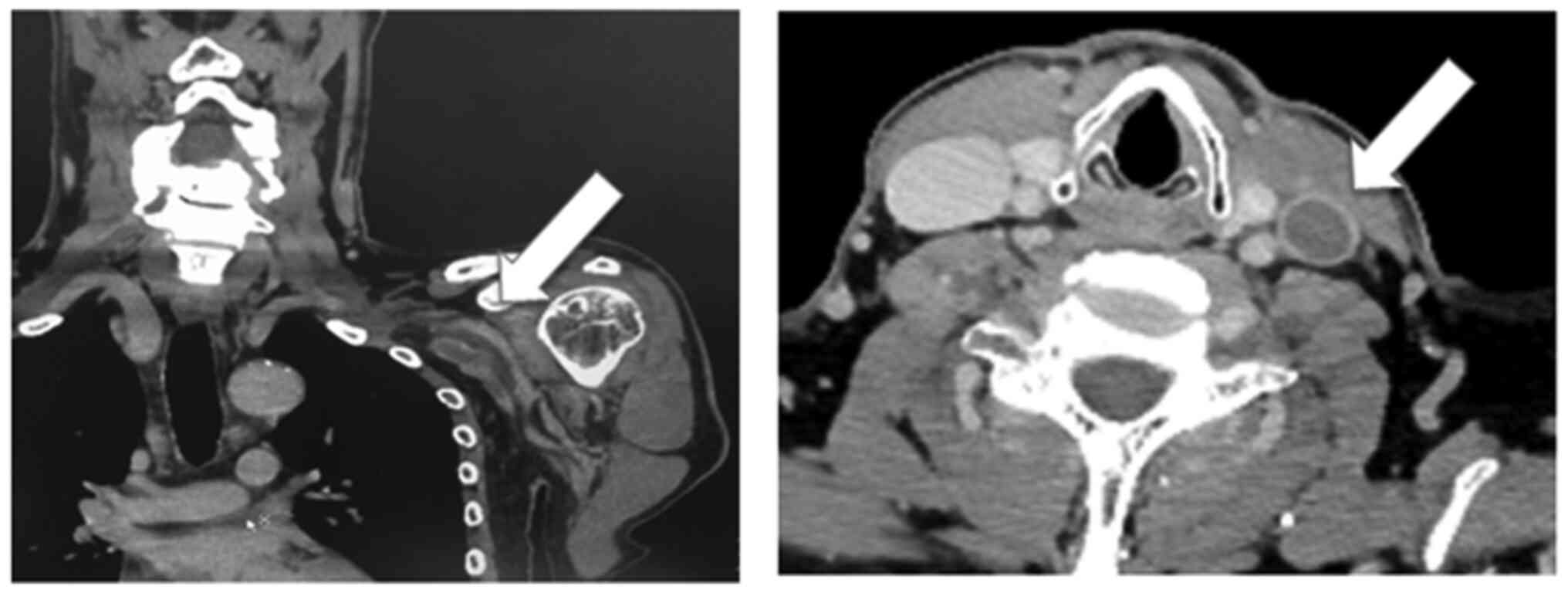
Plain and contrast-enhanced computed tomography (CT)
examination of the chest, abdomen and pelvis did not demonstrate
any distant metastasis.
Further examination of a Tru-Cut biopsy specimen
revealed undifferentiated pleomorphic sarcoma. Subsequently, an
indwelling CV port was placed through the left subclavian vein and
the patient underwent two courses of neoadjuvant chemotherapy using
doxorubicin (60 mg/m2) and ifosfamide (10
g/m2), as the tumor was high-grade, deeply situated, and
large. Two months after the indwelling port placement, a
preoperative contrast-enhanced CT scan of the chest at the
screening of post neo-adjuvant chemotherapy revealed DVT of the
left internal jugular vein. Therefore, contrast-enhanced CT of
brain, neck and upper extremity were further performed and DVT from
the left upper arm to the left internal jugular vein was observed
(Fig. 2) The D-dimer level was 8.63
µg/ml (standard, <1.0 µg/ml).
There were no associated symptoms, such as swelling
or pain, and PE was not detected on the CT images. After
administering anticoagulation therapy with heparin (10,000 U/day),
wide tumor resection and reconstruction using a prosthesis were
performed. One week after the surgery, anticoagulation therapy with
heparin was resumed; however, it was discontinued due to the
progression of anemia (hemoglobin level 6.1 g/dl; normal range,
13.5-16.8 g/dl) and a blood transfusion was performed. After 1
week, anticoagulation therapy with warfarin was resumed, as the
findings on contrast-enhanced CT revealed an increase in
thrombosis. There were no complications during the treatment.
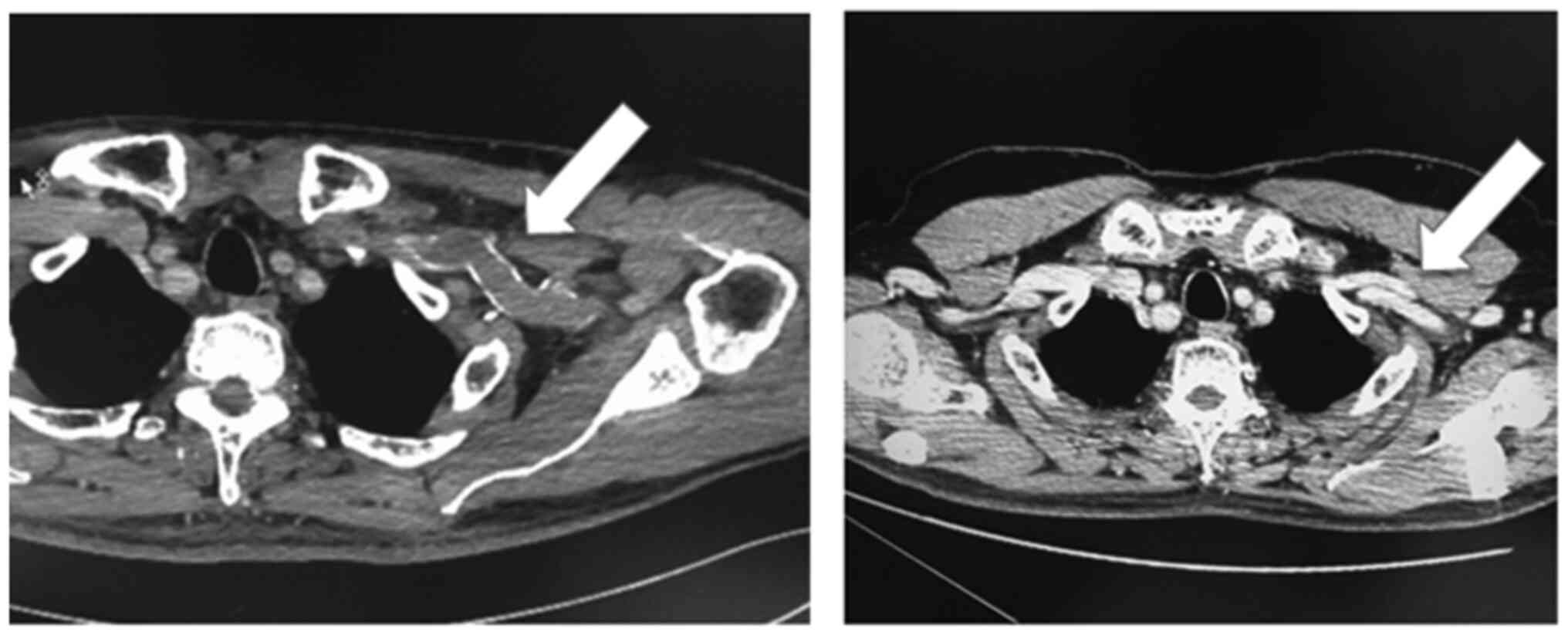
On the 5-month postoperative contrast CT scan, DVT
was not detected and the indwelling CV port was removed due to the
risk of thrombosis (Fig. 3). The
D-dimer levels had decreased to 3.28 µg/ml. Furthermore, warfarin
was discontinued 1 month after the port removal. Four months later,
the patient developed local recurrence of STS in the right thigh
that was treated with wide resection and endoprosthesis-based
reconstruction. Although adjuvant radiotherapy was performed, it
was discontinued due to the development of a postoperative
infection (pathogen: Serratia marcescens). Finally,
debridement and revision surgery were performed; however, the
patient developed multiple metastases and eventually succumbed to
the disease on May 8th, 2015.
Discussion
Patients with cancer are at a high risk of
developing DVT. Piccioli et al reported that cancer cells
can cause endothelial cell injury, thereby intensifying
hypercoagulability (4). A CVC is
commonly used in cancer patients who require chemotherapy and
intravenous administration of supportive treatment, such as
antiemetic and diuretic drugs, although its presence increases the
risk of DVT (2). However, it was
decided to proceed with the CV port placement in the present case,
as the sarcoma was large and high-grade, requiring neoadjuvant
chemotherapy and wide resection (3).
During the administration and clinical course of
chemotherapy in cancer patients with an indwelling CV port, DVT is
typically triggered when a coating of clotted blood and blood
proteins forms around the catheter (5).
Marinella et al reported that, among 90
patients who developed UEDVT, the most common underlying conditions
were the presence of CVC in 65 patients (72%), infection in 25
(28%), extrathoracic malignancy in 20 (22%), thoracic malignancy in
19 (21%), and a prior lower extremity DVT in 16 cases (18%)
(6).
The onset of UEDVT is usually characterized by arm
swelling, edema and pain, but completely asymptomatic cases are
possible, particularly in patients with long-term CVC placement
(6,7). In the present case, there were no
aforementioned symptoms, and DVT was detected incidentally on
preoperative contrast CT.
In UEDVT, early diagnosis is crucial, even for
asymptomatic cases, due to the risk of PE that may occur due to
catheter-related thrombosis. It was previously reported that PE was
implicated in ~10% of UEDVT cases (8). Recently, a lower rate (5%) of PE in
patients with isolated catheter-associated UEDVT has been
documented (9,10). Jones et al also described
that anticoagulation may not affect the rate of resolution or
decrease the progression of UEVDT, whereas it is associated with a
significant incidence of bleeding complications (9). Therefore, there is currently no
consensus on the optimal management of UEDVT.
Early detection may be difficult when there are no
symptoms, such as swelling or pain. Marinella et al noted
pain and edema in 34 and 84% of the UEDVT cases, respectively
(6). In a study by Hylton et
al, swelling was observed in 82% of the patients who developed
UEDVT after CVC insertion, but no symptoms were present in 6% of
the cases (7). DVT may be detected
by contrast CT and ultrasonography and, upon confirmation of UEDVT,
anticoagulant therapy may be administered. To the best of our
knowledge, the present report is the first to describe in detail
the clinical course of UEDVT in a sarcoma patient with an
indwelling CV port. Although sarcoma is rare and fewer patients
with sarcoma receive chemotherapy compared to those with cancer,
the possibility of UEDVT and necessity of screening sarcoma
patients with indwelling CV ports should be considered. There was a
limitation to the present case report: Ultrasound examination was
not performed, as the possibility of UEDVT was not taken into
consideration prior to its detection on CT scan. In conclusion, we
herein report the case of a patient with UEDVT who was
asymptomatic. Therefore, even in the absence of any symptoms, we
recommend that screening for DVT should be performed in patients
with indwelling CV ports.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of materials and data
Not applicable.
Authors' contributions
TN conceived the study, treated the patient,
collected the data and wrote the manuscript. KK collected, analyzed
and interpreted the clinical data. KA and TH performed the surgery,
and analyzed and interpreted the clinical data. KN collected and
analyzed the clinical data. AS analyzed and interpreted the
clinical data, and reviewed the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the case details and associated
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Gaddh M, Antun A, Yamada K, Gupta P, Tran
H, EI Rassi F, Kim HS and Khoury HJ: Venous access catheter-related
thrombosis in patients with cancer. Leuk Lymphoma. 55:501–508.
2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Yukisawa S, Fujiwara Y, Yamamoto Y, Ueno
T, Matsueda K, Kohno A and Suenaga M: Upper-extremity deep vein
thrombosis related to central venous port systems implanted in
cancer patients. Br J Radiol. 83:850–853. 2010.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Tanaka K, Kawamoto H, Saito I, Yoshimura
K, Fukuda H and Iwamoto Y: Preoperative and postoperative
chemotherapy with ifosfamide and adriamycin for adult high-grade
soft-tissue sarcomas in the extremities: Japan clinical oncology
group study JCOG0304. Jpn J Clin Oncol. 39:271–273. 2009.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ay C, Pabinger I and Cohen AT: Cancer
associated venous thromboembolism: Burden, mechanisms, and
management. Thromb Haemost. 117:219–230. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Evans NS and Ratchford EV:
Catheter-related venous thrombosis. Vasc Med. 23:411–413.
2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Marinella MA, Kathula SK and Markert RJ:
Spectrum of upper-extremity deep venous thrombosis in a community
teaching hospital. Heart Lung. 29:113–117. 2000.PubMed/NCBI
|
|
7
|
Joffe HV, Kucher N, Tapson VF and
Goldhaber SZ: Deep Vein Thrombosis (DVT) FREE Steering Committee:
Upper-extremity deep vein thrombosis: A prospective registry of 592
patients. Circulation. 110:1605–1611. 2004.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Verso M and Agnelli G: Venous
thromboembolism associated with long-term use of central venous
catheters in cancer patients. J Clin Oncol. 21:3665–3675.
2003.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Jones MA, Lee DY, Segall JA, Landry GJ,
Liem TK, Mitchell EL and Moneta GL: Characterizing resolution of
catheter-associated upper extremity deep venous thrombosis. J Vasc
Surg. 51:108–113. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Ploton G, Pistorius MA, Raimbeau A, Denis
Le Seve J, Bergère G, Ngohou C, Goueffic Y, Artifoni M, Durant C,
Gautier G, et al: A STROBE cohort study of 755 deep and superficial
upper-extremity vein thrombosis. Medicine (Baltimore).
99(e18996)2020.PubMed/NCBI View Article : Google Scholar
|