Introduction
Lung cancer has the highest morbidity and mortality
in China (1); 80-85% of patients
with lung cancer had non-small cell lung cancer (NSCLC), and the
majority were advanced at the time of initial diagnosis.
Tumor-associated anemia is one of the common concomitant diseases
of malignant tumors (2).
Tumor-associated anemia production can be caused by a variety of
factors, including tumor factors or tumor treatment factors.
Tumor-associated anemia is common in patients with lung cancer and
is often dramatically increased due to cancer therapy, especially
platinum chemotherapy (3-7).
Tumor-associated anemia can cause a variety of clinical symptoms,
seriously reduces the quality of life of patients, affects the
patient's tolerance to treatment, and reduces tumor tissue
sensitivity to treatment (8).
The relationship between tumor-associated anemia and
lung cancer prognosis has been the focus of clinicians. A recent
meta-analysis of 23 studies that included 10,612 patients showed
that preoperative anemia was a prognostic factor of lung cancer
(9), as compared with LC patients
without anemia, those with pre-operative anemia were at a 1.6-fold
greater risk of death (summarized HR=1.58; 95% CI, 1.44-1.75).
Zhang YH (10) reported that
patients with normal pre-treatment hemoglobin (NPHb) levels had a
greater chance of surviving for longer period, than did patients
with low pre-treatment hemoglobin (LPHb) levels (HR=2.05; 95% CI,
1.63-2.57; P<0.001); Mandrekar et al (11) reported that patients with low Hgb
levels had significantly worse TTP and OS. Wan et al
(12) report that compared to
patients with a low Hb change (|ΔHb|≤2.6), those having a
|ΔHb|>2.6 exhibited a significantly shorter survival [hazard
ratio=1.40, 95% confidence interval 1.31-1.50, P=4.5x10(-22), Plog
rank=1.6x10(-39)]. Aoe et al reported that anemia is a
prognostic factor of patients with lung cancer at first hospital
visit (13), survival was
significantly shorter in 298 patients with anemia (median survival
time (MST): 7.5 months) compared with 313 patients without anemia
(MST: 11.8 months, P<0.0001). The majority of studies have shown
that anemia is a prognostic factor of lung cancer, but controversy
still exists; several studies have shown that anemia is not
associated with the prognosis of lung cancer (14,15).
In previous studies on the prognoses of anemia and lung cancer,
anemia diagnostic criteria, and detection methods, the results may
be biased due to the inconsistency of anemia research subjects.
Therefore, in our single-center study, the baseline anemia of 4,874
patients with stage IV non-small cell lung cancer was used as the
research object to minimize the interference of related
factors.
This study retrospectively analyzed the incidence
and grade of baseline anemia in 4,874 patients with stage IV
non-small cell lung cancer in China. The relationship between
baseline anemia and clinicopathological characteristics and their
effects on prognosis were analyzed to further guide the treatment
of lung cancer.
Materials and methods
Clinical data
Our study retrospectively analyzed anemia-related
data in patients with stage IV NSCLC. A total of 4,874 patients who
were admitted to the Zhejiang Cancer Hospital between January 2013
and June 2019 were eligible for the study. The inclusion criteria
were as follows: i) Pathologically proven stage IV NSCLC tumor; ii)
age >18 years old; and iii) have complete clinical data and
follow-up information. The exclusion criteria were as follows: i)
With hematological basic diseases; and ii) with chronic
nephropathy. The follow-up period lasted until October 2019.
Clinical staging was based on the 8th edition of Classification of
TNM Lung Cancer (16). Subsequent
treatments received by the patient includeradiotherapy,
chemotherapy, targeted therapy and immunotherapy, some patients
receive only one type of treatment, and some patients receive two
or more therapies, combination therapy means that the patient
receives two or more treatments. Targeted therapy is defined as
targeted drugs corresponding to driver genes of lung cancer.
Immunotherapy includes PD1/PD-L1 drug. The study was approved by
the institutional review board of Zhejiang Cancer Hospital.
Grading of anemia
According to the anemia grading criteria established
by National Cancer Institution (17), anemia is defined as having
hemoglobin (Hb) levels of <120.0 g/l for males and <110.0 g/l
for females. Anemia is further categorized into five grades based
on the Hb level, as follows: Grade 0, normal Hb level; grade 1
(mild anemia), 100 g/l, normal level; grade 2 (moderate anemia),
80-100 g/l; grade 3 (severe anemia), 65-80 g/l; and grade 4
(life-threatening anemia), <65 g/l. Baseline anemia is defined
as having hemoglobin levels of <120.0 g/l for males and
<110.0 g/l for females at first visit to the hospital,and all
patients did not receive radiotherapy, chemotherapy, targeted
therapy or immunotherapy treatment.
Statistical treatment
The Statistical Package for the Social Sciences
(SPSS) version 19.0 (IBM Corp) was used to perform the statistical
analysis. Quantitative variables were presented as means ± standard
deviation (mean ± SD). The mean values from multiple comparisons
were compared by using ANOVA followed by Bonferroni-Forsythe. The
data was analyzed using χ2. Survival analysis was
conducted using the Kaplan-Meier method, and comparison was
performed via log-rank test. Multivariate analysis was conducted
using Cox proportional hazard regression model. P<0.05 was
considered to indicate a statistically significant difference.
Results
Patient characteristics
A total of 4,874 eligible patients with stage IV
NSCLC were included. Patients' sex, age, smoking history, tumor
type, bone metastases, comorbidity, and treatment are summarized in
Table I.
 | Table IDemographic characteristics of the
study population (n=4,874). |
Table I
Demographic characteristics of the
study population (n=4,874).
| Characteristic | N (%) |
|---|
| Sex | |
|
Male | 2,822 (57.90) |
|
Female | 2,052 (42.10) |
| Age (years) | |
|
>60 | 2656 (54.49) |
|
≤60 | 2218 (45.51) |
| Smoking history | |
|
Yes | 1,981 (40.64) |
|
No | 2,893 (59.36) |
| Tumor type | |
|
Adenocarcinoma | 3,872 (79.44) |
|
Squamous
cell carcinoma | 455 (9.34) |
|
Others
NSCLC | 547 (11.22) |
| Bone metastasis | |
|
Yes | 2,254 (46.25) |
|
No | 2,620 (53.75) |
| Comorbidity | |
|
Yes | 2,489 (51.07) |
|
No | 2,385 (48.93) |
| Radiotherapy | |
|
Yes | 1,627 (33.38) |
|
No | 3,247 (66.62) |
| Chemotherapy | |
|
Yes | 3,426 (70.29) |
|
No | 1,448 (29.71) |
| Targeted therapy | |
|
Yes | 2,830 (58.06) |
|
No | 2,044 (41.94) |
| Immunotherapy | |
|
Yes | 204 (4.19) |
|
No | 4,670 (95.81) |
| Combine therapy | |
|
Yes | 3,093 (63.46) |
|
No | 1,781 (36.54) |
Prevalence of anemia
For the 4,874 patients who had record of Hb level,
the prevalence of baseline anemia was 32.09%, with a mean Hb level
of 123.32±20.31 g/l, of which 19.08% had mild anemia, 10.79% had
moderate anemia, 1.91% had severe anemia, and 0.31% had
life-threatening anemia (Table
II).
 | Table IIFrequency of first admission baseline
cancer-related anemia in the current study. |
Table II
Frequency of first admission baseline
cancer-related anemia in the current study.
| Grade | Hb (mean ± SD,
g/l)a | Number | Percentage |
|---|
| 0 | 134.02±13.19 | 3,310 | - |
| 1 | 109.20±5.72 | 930 | 19.08 |
| 2 | 91.48±5.61 | 526 | 10.79 |
| 3 | 74.03±3.97 | 93 | 1.91 |
| 4 | 59.40±3.94 | 15 | 0.31 |
| Total | 123.32±20.31 | 4,874 | 32.09 |
Relationship between baseline anemia
and clinical characteristics
Less female patients had baseline anemia than male
patients (36.85 vs. 25.56%, P<0.001). Compared with younger
patients, patients who are >60 years old had higher baseline
anemia (34.41 vs. 29.31%, P<0.001). The prevalence of baseline
anemia was highest in patients with squamous cell carcinoma
(49.67%), followed by patients with other NSCLC types (36.93%).
Adenocarcinoma had the lowest prevalence of baseline anemia
(29.34%), P<0.001. Patients with smoking history had higher
baseline anemia than nonsmokers (38.97 vs. 27.38%, P<0.001).
Patients without bone metastases had less baseline anemia than
those with bone metastases (34.38 vs. 30.11%, P=0.002). Prevalence
of baseline anemia was slightly lower in patients with comorbidity
than those without comorbidity (32.06 vs. 32.12%). However, the
difference was not statistically significant (P=0.966) (Table III).
 | Table IIIRelationship between baseline anemia
and clinicopathological features in current study. |
Table III
Relationship between baseline anemia
and clinicopathological features in current study.
| Clinical
features | Anemia-free group
(n=3,310) | Anemia group
(n=1,564) | χ2 | P-value |
|---|
| Sex | | | 69.829 | <0.001 |
|
Male | 1782 | 1040 | | |
|
Female | 1528 | 524 | | |
| Age (years) | | | 14.466 | <0.001 |
|
>60 | 1742 | 914 | | |
|
≤60 | 1568 | 650 | | |
| Smoking
history | | | 72.528 | <0.001 |
|
Yes | 1209 | 772 | | |
|
No | 2101 | 792 | | |
| Pathological
type | | | 83.857 | <0.001 |
|
Adenocarcinoma | 2736 | 1136 | | |
|
Squamous
cell carcinoma | 229 | 226 | | |
|
Others | 345 | 202 | | |
| Bone
metastasis | | | 10.132 | 0.002 |
|
Yes | 1479 | 775 | | |
|
No | 1831 | 789 | | |
| Comorbidity | | | 0.002 | 0.966 |
|
Yes | 1691 | 798 | | |
|
No | 1619 | 766 | | |
Univariate analysis of clinical
features and prognosis
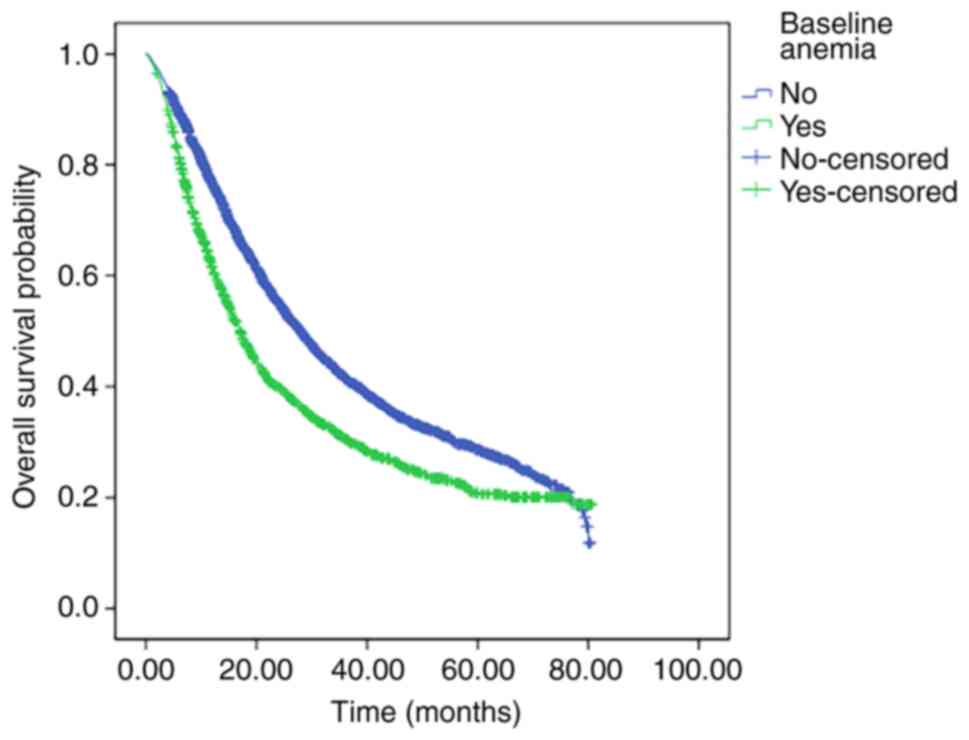
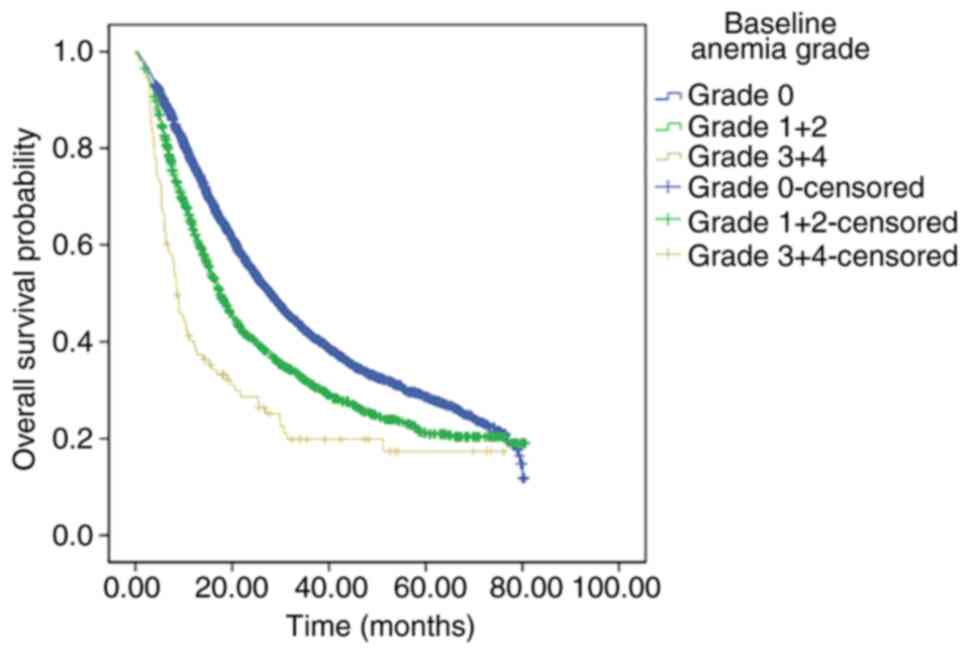
Univariate analysis shows the significant
association of OS with sex, age, pathological type, bone
metastasis, smoking history, chemotherapy, targeted therapy,
immunotherapy, baseline anemia, and anemia grade. However, OS was
not significantly associated with comorbidity and radiotherapy
(Table IV). Patients without
baseline anemia had longer OS than those with anemia (median OS:
28.0 vs. 17.4 months, P<0.001; Fig.
1). With rising grade of baseline anemia, OS became shorter.
Patients with anemia grade 0 had the longest OS (median OS: 28.0
months), followed by patients with anemia grades 1 and 2 (median
OS: 17.5 months). Patients with anemia grades 3 and 4 had the
shortest OS (median OS: 8.6 months), P<0.001 (Fig. 2).
 | Table IVUnivariate analysis of clinical
features and prognosis in current study. |
Table IV
Univariate analysis of clinical
features and prognosis in current study.
| Clinical
features | OS (months) | 95% CI | χ2 | P-value |
|---|
| Sex | | | 74.224 | <0.001 |
|
Male | 19.800 | 18.574-21.026 | | |
|
Female | 30.800 | 28.523-33.077 | | |
| Age (years) | | | 52.673 | <0.001 |
|
>60 | 20.400 | 19.198-21.602 | | |
|
≤60 | 29.400 | 27.344-31.456 | | |
| Smoking
history | | | 90.913 | <0.001 |
|
Yes | 18.300 | 17.087-19.513 | | |
|
No | 29.200 | 27.296-31.104 | | |
| Pathological
type | | | 88.626 | <0.001 |
|
Adenocarcinoma | 26.900 | 25.575-28.225 | | |
|
Squamous
cell carcinoma | 15.300 | 13.554-17.046 | | |
|
Others | 13.800 | 11.950-15.650 | | |
| Bone
metastasis | | | 32.394 | <0.001 |
|
Yes | 21.100 | 19.693-22.507 | | |
|
No | 27.100 | 25.323-28.877 | | |
| Comorbidity | | | 0.729 | 0.393 |
|
Yes | 22.800 | 21.067-24.533 | | |
|
No | 25.100 | 23.499-26.701 | | |
| Radiotherapy | | | 2.030 | 0.154 |
|
Yes | 25.200 | 23.030-27.370 | | |
|
No | 23.400 | 21.917-24.883 | | |
| Chemotherapy | | | 8.371 | 0.004 |
|
Yes | 23.100 | 21.758-24.442 | | |
|
No | 26.400 | 23.422-29.378 | | |
| Targeted
therapy | | | 182.633 | <0.001 |
|
Yes | 30.500 | 28.796-32.204 | | |
|
No | 15.700 | 14.629-16.771 | | |
| Immunotherapy | | | 6.174 | 0.013 |
|
Yes | 29.400 | 26.369-32.431 | | |
|
No | 23.800 | 22.599-25.001 | | |
| Anemia | | | 84.801 | <0.001 |
|
No
(n=3,382) | 28.000 | 26.480-29.520 | | |
|
Yes
(n=1,596) | 17.400 | 15.887-18.313 | | |
| Grade of
anemia | | | 105.379 | <0.001 |
|
0
(n=3,382) | 28.000 | 26.480-29.520 | | |
|
1+2
(n=1,146) | 17.500 | 16.190-18.810 | | |
|
3+4
(n=110) | 8.600 | 6.857-10.343 | | |
Multivariate analysis of clinical
features and prognosis
Univariateanalysis of statistically significant
sections, such as sex, age, pathological type, bone metastasis,
smoking history, chemotherapy, targeted therapy, immunotherapy,
baseline anemia, and anemia grade, were included in the COX
multivariate regression model. Multivariate analysis showed that
age, pathological type, bone metastasis, smoking history, targeted
therapy, immunotherapy, baseline anemia, and anemia grade were
independent prognostic factors of OS in patients with stage IV
NSCLC (Table V).
 | Table VMultivariate analysis of clinical
features and prognosis in current study. |
Table V
Multivariate analysis of clinical
features and prognosis in current study.
| Clinical
features | B | SE | Wald | HR | 95% CI | P-value |
|---|
| Sex | -0.068 | 0.053 | 1.655 | 0.934 | 0.842-1.036 | 0.198 |
| Age | 0.183 | 0.039 | 22.420 | 1.201 | 1.113-1.296 | <0.001 |
| Pathological
type | 0.151 | 0.028 | 28.567 | 1.163 | 1.100-1.229 | <0.001 |
| Bone
metastasis | -0.261 | 0.038 | 47.710 | 0.770 | 0.715-0.829 | <0.001 |
| Smoking
history | -0.160 | 0.052 | 9.481 | 0.852 | 0.7700-0.944 | 0.002 |
| Targeted
therapy | 0.415 | 0.040 | 108.417 | 1.514 | 1.401-1.637 | <0.001 |
| Chemotherapy | -0.008 | 0.046 | 0.029 | 0.992 | 0.907-1.085 | 0.865 |
| Immunotherapy | 0.406 | 0.111 | 13.281 | 1.501 | 1.206-1.867 | <0.001 |
| Baseline
anemia | -0.280 | 0.130 | 4.638 | 0.756 | 0.586-0.975 | 0.031 |
| Grade of
anemia | 0.489 | 0.115 | 18.213 | 1.630 | 1.303-2.041 | <0.001 |
Discussion
Our study included 4,874 patients with stage IV
NSCLC. This was the largest sample size of a research on anemia in
NSCLC in China. The prevalence of baseline anemia was 32.09% with a
mean Hb level of 123.32±20.31 g/l, of which 19.08% had mild anemia,
10.79% had moderate anemia, 1.91% had severe anemia, and 0.31% had
life-threatening anemia. Most patients with baseline anemia showed
mild to moderate anemia. The incidence of baseline anemia was
slightly lower than that reported in other countries based on
European populations (3) but
slightly higher than that reported for American populations
(6). ECAS is a prospective,
observational, and epidemiological survey of the anemia in the
European region. At ECAS enrollment, 37.6% of lung cancer patients
had Hb levels of <12.0 g/dl (3).
In a retrospective, observational study on anemia in patients
undergoing chemotherapy for solid tumors in the United States,
7,001 patients with NSCLC were enrolled. At baseline, 16.1% of the
patients were anemic with Hb levels of <11.0 g/dl, and 33.6% had
Hb levels of <12 g/dl; the mean (SD) Hb at baseline was 12.7
(1.8) g/dl (6). The difference in
results may be related to the different definitions of anemia.
Therefore, a standardized and uniform anemia definition may lead to
standardized diagnosis and treatment.
Aoe et al reported that in 611 cases of lung
cancer in Japan, a significant correlation was found between anemia
and age and Eastern Cooperative Oncology Group (ECOG) scores;
however, anemia was not correlated with sex, histological type,
clinical stage, or serum lactate dehydrogenase (13). The results of our study showed that
female patients with baseline anemia were fewer than male patients
with baseline anemia (36.85 vs. 25.56%, P<0.001). Compared with
younger patients, patients who are >60 years old had higher
prevalence of baseline anemia (34.41 vs. 29.31%, P<0.001). The
prevalence of baseline anemia was highest in patients with squamous
cell carcinoma (49.67%), followed by patients with other NSCLC
types (36.93%). Patients with adenocarcinoma had the lowest
prevalence of baseline anemia (29.34%), P<0.001. Our study shows
that the proportion of non-smokers is relatively high compared with
other study (18), which may be
related to the population of the study. A data from the Asian
population published by Zhang shows that the proportion of
non-smokers is 42.8% (10), the
proportion of non-smoking patients in our study is similar to
Zhang's study. In addition, the proportion of female patients in
our study is relatively high, while the proportion of female
patients who smoke in China is very low; the proportion of patients
receiving Epidermal growth factor receptor (EGFR)-tyrosine kinase
inhibitor (TKI) targeted therapy in our study is higher, and the
dominant population of EGFR-TKI targeted therapy is non-smokers.
Patients with smoking history had higher baseline anemia than
nonsmokers (38.97 vs. 27.38%, P<0.001). The results were
consistent with those obtained in a retrospective study involving
416 NSCLC cases reported by Zhang et al in Henan, China
(10). The study further confirmed
the basic characteristics of anemia in Chinese lung cancer
patients. The results of our study showed that patients without
bone metastases had less baseline anemia than those with bone
metastases (34.38 vs. 30.11%, P=0.002), considering that bone
marrow invasion in patients with bone metastasis leads to a
decrease in hematopoietic function.
According to previous studies on anemia and lung
cancer prognosis, radiotherapy and chemotherapy are the main
methods used to treat lung cancer (10,12,13,18,19).
In the past decade, targeted therapy and immunotherapy have changed
the treatment mode of advanced lung cancer. In our study, the
proportions of patients undergoing chemotherapy, targeted therapy,
radiotherapy and immunotherapy were 70.29, 58.06, 33.38 and 4.19%,
respectively. The proportion of patients undergoing targeted
therapy was higher, and immunotherapy was included in the study;
our research reflects the current treatment model for advanced lung
cancer (20).
A meta analysis of 23 studies including 10,612
patients showed that preoperative anemia was a prognostic factor of
lung cancer (9); patients with
preoperative anemia had reduced OS after lung surgery. For patients
with advanced lung cancer, the opportunity for surgery is lost; so,
the result helps guide patients who will undergo surgery for
treatment. Other studies also showed that anemia is associated with
the prognosis of lung cancer, but the sample sizes are relatively
small or they included multiple cancers (10-13).
The evidence from studies investigating the relationship between
anemia and the progression of NSCLC remains controversial, as
several studies have shown that anemia is not associated with the
prognosis of lung cancer (14,15).
Our study is a single-center study with a large sample size that
was performed in the real world in China. We analyzed the
relationship between baseline anemia and prognosis in 4,874
patients with IV non-small cell lung cancer. Univariate analysis
results showed that patients without baseline anemia had longer OS
than those with anemia (median OS: 28.0 vs. 17.4 months,
P<0.001). Further multivariate analysis revealed that baseline
anemia was an independent prognostic factor in patients with stage
IV NSCLC. Our conclusion is consistent with the relevant research
results (9-13).
The reason for the shortened survival of patients due to
tumor-associated anemia is the decreased sensitivity to treatment
and tolerance to treatment. According to the anemia grade, we
divided the patients into three groups, namely, anemia grades 0,
1-2, and 3-4. With rising anemia grade, the OS became shorter. The
patients with anemia grade 0 had the longest OS (median OS: 28.0
months), followed by patients with anemia grades 1 and 2 (median
OS: 17.5 months). The patients with anemia grades 3 and 4 had the
shortest OS (median OS: 8.6 months), P<0.001. Multivariate
analysis showed that baseline anemia grade was also a prognostic
factor of stage IV NSCLC patients. Results further confirmed the
importance of baseline anemia for NSCLC, which requires attention
and timely treatment (21).
Treatment of tumor-associated anemia include the correction of
nutritional deficiencies, use of intravenous (IV) iron,
erythropoietic stimulating agents (ESAs), and blood transfusions
(2), the use of ESAs is still
controversial due to its security issues. The results of a phase
III clinical study on ESAs treatment showed that Darbepoetinalfa
dosed to a 12.0-g/dl Hb ceiling was noninferior to placebo for OS
and PFS and significantly reduced odds of transfusion or Hb≤8.0
g/dl in anemic patients with NSCLC receiving myelosuppressive
chemotherapy (21). The early
treatment of anemia is very important. Whether management of anemia
can improve the survival of patients, it may be an aim of future
studies.
Our study had some limitations. The major limitation
is its retrospective nature. Moreover, the study is a single-center
study. However, as the largest sample size research on anemia in
NSCLC, our results are meaningful and can serve as a guide for the
treatment of NSCLC patients with anemia in China. In the future,
multi-center prospective studies are needed.
The study showed that the prevalence of baseline
anemia was highest in patients with stage IV NSCLC who are men,
>60 years old, with smoking history, with squamous cell
carcinoma, and with bone metastases. Baseline anemia and anemia
grading were independent prognostic factors in patients with stage
IV NSCLC.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
JZ designed the study. CC and ZS conceived of the
study. CC and WW acquired the data. CC and ZS performed data
analysis/interpretation. CC performed statistical analysis. CC
prepared the manuscript. JZ revised the manuscript. The
authenticity of all the raw data is confirmed by CC and JZ. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The current study was approved by the institutional
review board of Zhejiang Cancer Hospital.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Chen W, Sun K, Zheng R, Zeng H, Zhang S,
Xia C, Yang Z, Li H, Zou X and He J: Cancer incidence and mortality
in China, 2014. Chin J Cancer Res. 30:1–12. 2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Gilreath JA, Stenehjem DD and Rodgers GM:
Diagnosis and treatment of cancer-related anemia. Am J Hematol.
89:203–212. 2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Ludwig H, Van Belle S, Barrett-Lee P,
Birgegård G, Bokemeyer C, Gascón P, Kosmidis P, Krzakowski M,
Nortier J, Olmi P, et al: The European Cancer Anaemia Survey
(ECAS): A large, multinational, prospective survey defining the
prevalence, incidence, and treatment of anaemia in cancer patients.
Eur J Cancer. 40:2293–2306. 2004.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Crawford J, Kosmidis PA, Hirsch FR and
Langer CJ: Targeting anemia in patients with lung cancer. J Thorac
Oncol. 1:716–725. 2006.PubMed/NCBI
|
|
5
|
Gascón P, Almenárez J, Artal Á, Camps C,
Fírvida JL, Garrido P, González Larriba JL and Montalar J:
Management of lung cancer-associated anaemia: The spanish lung
cancer anaemia survey (SLCAS). Clin Transl Oncol. 13:328–334.
2011.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Wu Y, Aravind S, Ranganathan G, Martin A
and Nalysnyk L: Anemia and thrombocytopenia in patients undergoing
chemotherapy for solid tumors: A descriptive study of a large
outpatient oncology practice database, 2000-2007. Clin Ther.
31:2416–2432. 2009.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Muñoz-Langa J, De Castro J, Gascó P,
Sanchez A, Esteban E, Gasent JM, Barneto I, Montalar J, Artal A and
Vidal S: Chemotherapy-associated anemia in patients with lung
cancer: An epidemiological, retrospective and multicenter study.
Future Oncol. 11:1665–1674. 2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Cella D, Kallich J, McDermott A and Xu X:
The longitudinal relationship of hemoglobin, fatigue and quality of
life in anemic cancer patients: Results from five randomized
clinical trials. Ann Oncol. 15:979–986. 2004.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Liu Y, Bai YP, Zhou ZF, Jiang CR, Xu Z and
Fan XX: Preoperative anemia as a prognostic factor in patients with
lung cancer: A systematic review and meta-analysis of
epidemiological studies. J Cancer. 10:2047–2056. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Zhang YH, Lu Y, Lu H, Zhang MW, Zhou YM,
Li XL, Lv P and Zhao XY: Pre-treatment hemoglobin levels are an
independent prognostic factor in patients with non-small cell lung
cancer. Mol Clin Oncol. 9:44–49. 2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Mandrekar SJ, Schild SE, Hillman SL, Allen
KL, Marks RS, Mailliard JA, Krook JE, Maksymiuk AW, Chansky K,
Kelly K, et al: A prognostic model for advanced stage nonsmall cell
lung cancer. Pooled analysis of North Central Cancer Treatment
Group trials. Cancer. 107:781–792. 2006.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Wan S, Lai Y, Myers RE, Li B, Palazzo JP,
Burkart AL, Chen G, Xing J and Yang H: Post-diagnosis hemoglobin
change associates with overall survival of multiple
malignancies-results from a 14-year hospital-based cohort of lung,
breast, colorectal, and liver cancers. BMC Cancer.
13(340)2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Aoe K, Hiraki A, Maeda T, Katayama H,
Fujiwara K, Tabata M, Kiura K, Ueoka H and Tanimoto M: Serum
hemoglobin level determined at the first presentation is a poor
prognostic indicator in patients with lung cancer. Intern Med.
44:800–804. 2005.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Gauthier I, Ding K, Winton T, Shepherd FA,
Livingston R, Johnson DH, Rigas JR, Whitehead M, Graham B and
Seymour L: Impact of hemoglobin levels on outcomes of adjuvant
chemotherapy in resected non-small cell lung cancer: The JBR.10
trial experience. Lung Cancer. 55:357–363. 2007.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Trufelli DC, Moraes TV, Lima AA and Giglio
AD: Epidemiological profile and prognostic factors in patients with
lung cancer. Rev Assoc Med Bras (1992). 62:428–433. 2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kay FU, Kandathil A, Batra K, Saboo SS,
Abbara S and Rajiah P: Revisions to the Tumor, Node, Metastasis
staging of lung cancer (8th edition): Rationale, radiologic
findings and clinical implications. World J Radiol. 9:269–279.
2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Experts Committee on Cancer-Related Anemia
and Chinese Society of Clinical Oncology (CSCO). Clinical practice
guidelines on cancer-related anemia (2012-2013 Edition). Chin Clin
Oncol. 1(18)2012.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Pathak RS, Pantarotto JR, Cook G, Holmes
O, Cross P and MacRae RM: Anemia is a poor prognostic factor for
stage I non-small cell lung cancer (NSCLC) patients treated with
Stereotactic Body Radiation Therapy (SBRT). Clin Transl Radiat
Oncol. 16:28–33. 2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Topkan E, Selek U, Ozdemir Y, Yildirim BA,
Guler OC, Mertsoylu H and Hahn SM: Chemoradiotherapy-induced
hemoglobin nadir values and survival in patients with stage III
non-small cell lung cancer. Lung Cancer. 121:30–36. 2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Passiglia F, Pilotto S, Facchinetti F,
Bertolaccini L, Del Re M, Ferrara R, Franchina T, Malapelle U,
Menis J, Passaro A, et al: Treatment of advanced non-small-cell
lung cancer: The 2019 AIOM (Italian Association of Medical
Oncology) clinical practice guidelines. Crit Rev Oncol Hematol.
146(102858)2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Gascón P, Nagarkar R, Šmakal M, Syrigos
KN, Barrios CH, Sánchez JC, Zhang L, Henry DH, Gordon D, Hirsh V,
et al: A randomized, double-blind, placebo-controlled, phase ΙΙΙ
noninferiority study of the long-term safety and efficacy of
darbepoetinalfa for chemotherapy-induced anemia in patients with
advanced NSCLC. J Thorac Oncol. 15:190–202. 2020.PubMed/NCBI View Article : Google Scholar
|