Introduction
Bladder tumors can be broadly divided into those of
epithelial or mesodermal origin. Ninety-percent of bladder tumors
arise from the epithelium of the bladder, and most cases of bladder
cancer are histologically urothelial carcinomas. Bladder cancer can
be broken down further into non-muscle invasive bladder cancer
(NMIBC) and muscle invasive bladder cancer (MIBC). Most cases of
bladder cancer (70-80%) are NMIBC and have a good prognosis; the
remaining cases are MIBC and have a poor prognosis (1). However, mesodermal tumors are
exceptionally rare and often benign. Of the mesenchymal tumors of
the bladder, leiomyomas are the most common, and their prognosis
depends on their histology (2).
The present report described a case of primary
submucosal urothelial cancer which was difficult to diagnose
preoperatively. To the best of our knowledge, there are no previous
reports of primary urothelial cancer occurring in the submucosa. In
addition to the case description, two hypotheses were advanced to
account for the oncogenesis of the present case. First, the
urothelial cancer developed within a diverticulum, then the
entrance of the diverticulum closed, sealing in the cancer. Second,
the bladder cancer stemmed from aberrant urothelium in the
submucosal tissue. If submucosal urothelial bladder carcinoma
develops within the diverticular environment, its prognosis can be
as poor as that of invasive bladder cancer due to the features of
the diverticular environment. Even in a patient with a submucosal
bladder tumor but no previous history of bladder cancer, bladder
cancer should be considered in the differential diagnosis.
Case report
An 87-year-old, male patient was referred to our
hospital for a bladder tumor which was found incidentally on
follow-up CT for hepatic cancer (Fig.
1). He had a past history of aortic valve stenosis,
hepatocellular carcinoma (HCC), and liver cirrhosis due to chronic
hepatitis C. He was a not a smoker and had no hypertension. He had
a partial hepatectomy for HCC, followed by radiofrequency ablation
and transarterial chemoembolization for a recurrence. He had no
previous history of bladder cancer. Contrast-enhanced CT revealed a
30x20 mm, homogeneously enhancing, multilobulated mass invading the
perivesical fat in the left wall but no metastasis (Fig. 1). He had no symptoms, such as gross
hematuria. Blood analysis revealed slight renal insufficiency and
anemia, but urine analysis denied microscopic hematuria and pyuria.
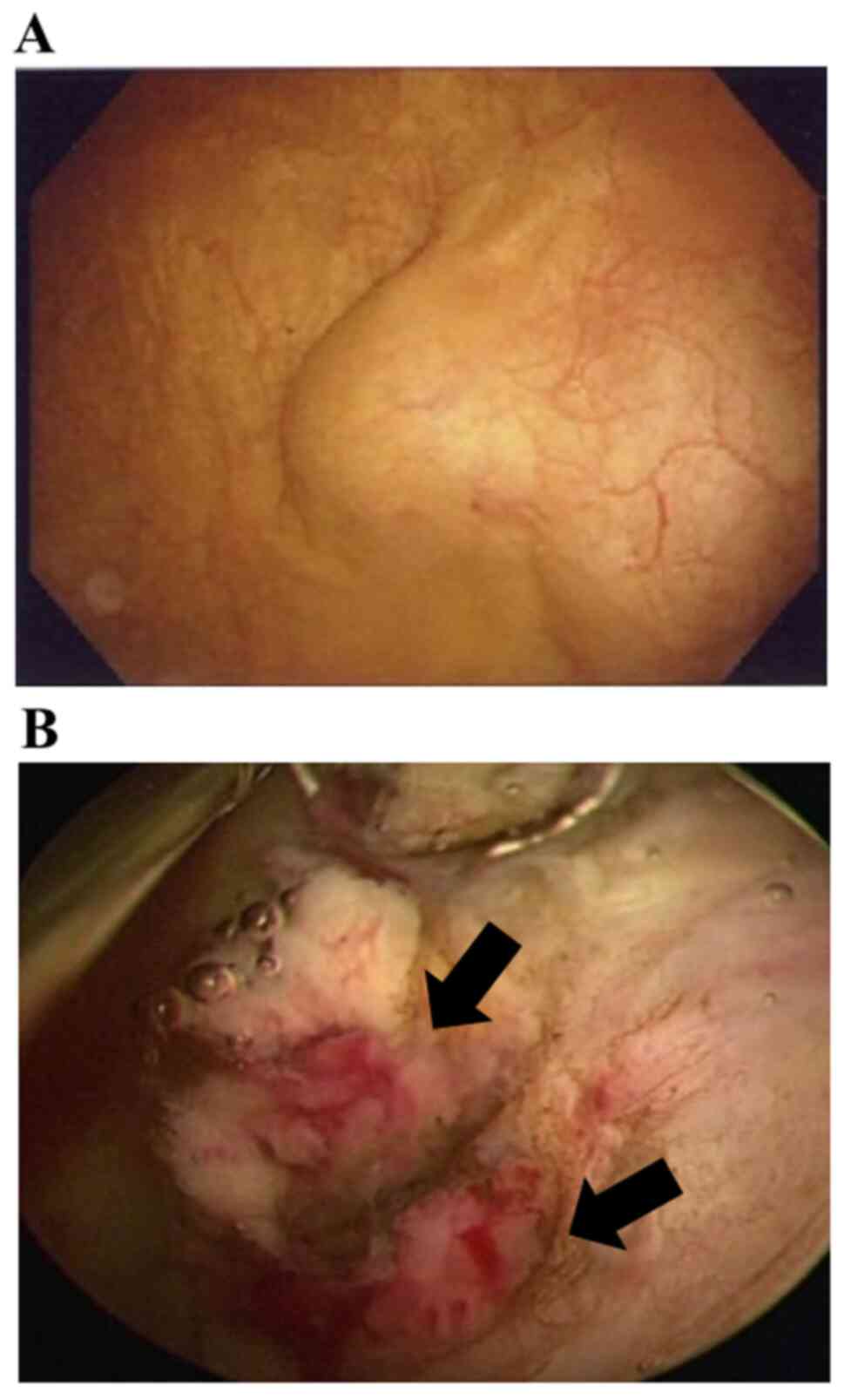
Cystoscopy revealed a sessile, non-papillary tumor covered with
normal bladder mucosa on the left bladder wall showing the typical
cystoscopic features of a submucosal bladder tumor (Fig. 2A). The preoperative diagnosis was
submucosal bladder tumor originating in the mesoderm.
Because of the patient's old age and medical
history, transurethral resection of bladder tumor (TURBT) was
performed for histological evaluation. The normal bladder mucosa
covering the tumor was resected to reveal typical urothelial
bladder cancer with a papillary morphology (Fig. 2B). The bladder tumor showed minimal
invasion of the muscle layer and was resected to the greatest
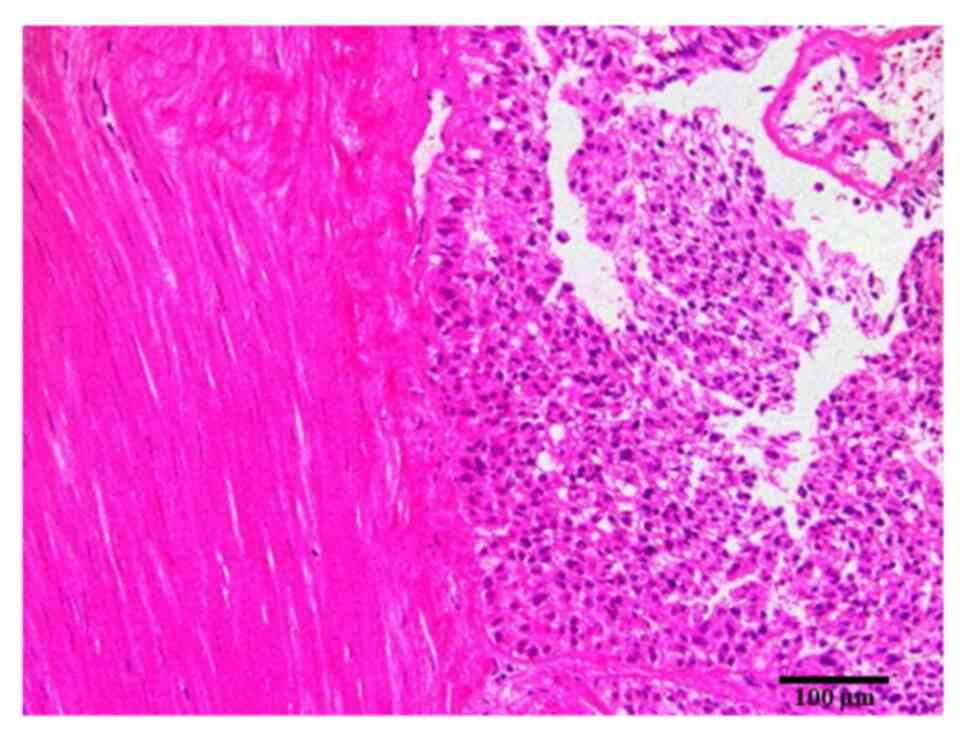
extent possible. Pathological analysis revealed that the urothelial
carcinoma, which was characterized by largely delicate and separate
papillae as well as uniformly enlarged nuclei (low grade), had
invaded the submucosa (Fig. 3). No
infiltration of the cancer cells into the muscle layer was
observed. Two months later, CT showed a local recurrence. The
patient then underwent systemic chemotherapy.
Discussion
Preoperatively identifying the histological subtype
of a submucosal bladder tumor can be difficult because this type of
tumor comprises diverse histological types, including both benign
and malignant varieties. Most cases of submucosal bladder tumor
present similar clinical symptoms, such as a pelvic mass,
hematuria, and dysuria. Imaging methods also have limitations
(3-5).
MRI is slightly better than CT and ultrasound sonography because it
has better resolution and contrast (6,7).
Cystoscopy is only useful in discriminating mesenchymal tumors from
epithelial carcinomas. The definitive diagnosis is made by
histopathological and immunohistological analysis of TURBT
specimens. In the present case, the asymptomatic tumor was
incidentally detected on CT, and cystoscopy revealed a sessile,
non-papillary tumor covered by normal urothelium. The preoperative
diagnosis was submucosal bladder tumor, but its histological
subtype was unknown. Because the patient had no previous history of
bladder cancer, urothelial bladder cancer was not considered in the
preoperative diagnosis.
To the best of our knowledge, the present study is
the first to report a case of submucosal urothelial bladder cancer.
TURBT of the normal bladder mucosa revealed a tumor with a
papillary morphology typical of urothelial bladder cancer. While it
remains unclear why the carcinoma was covered by normal
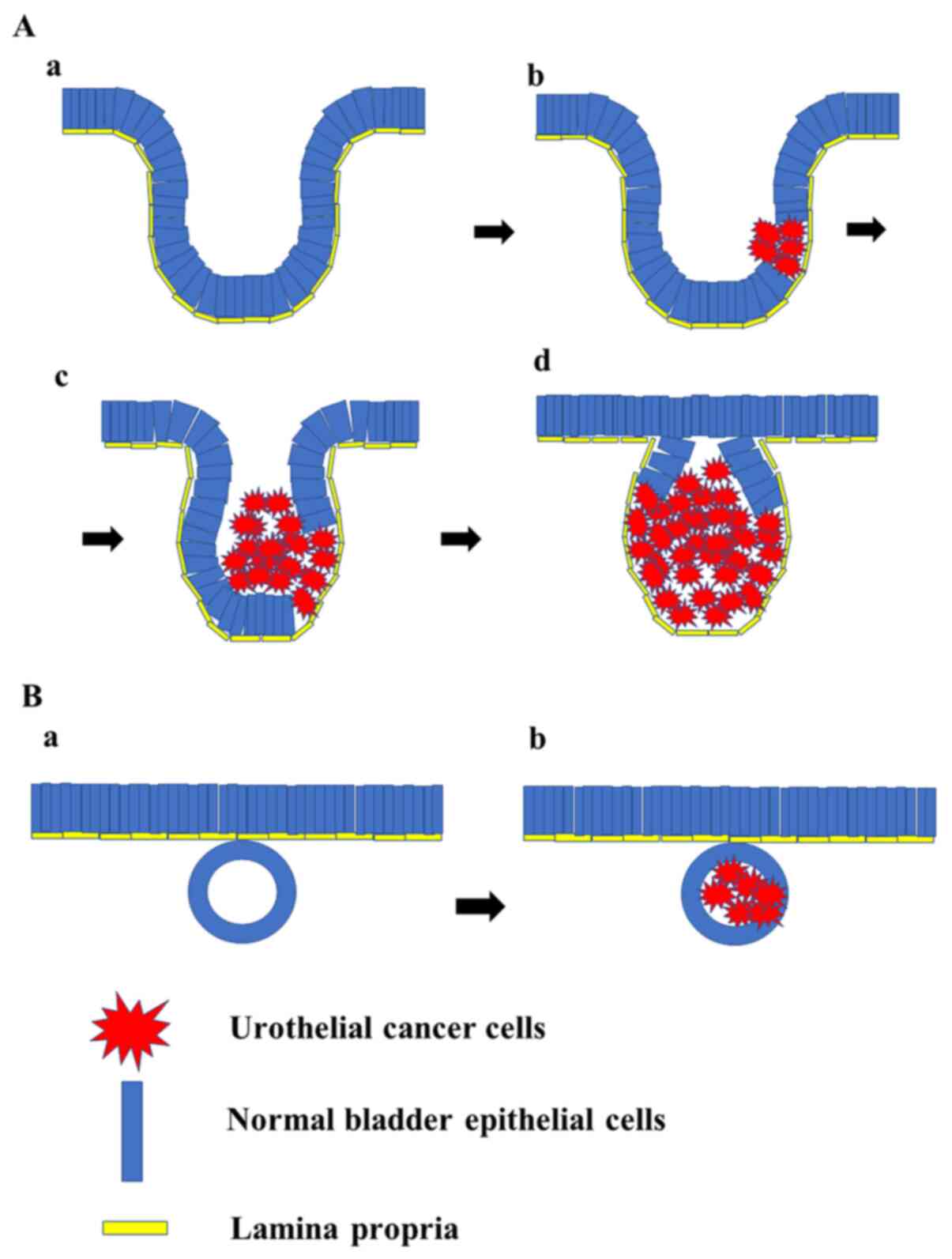
uroepithelium, two explanations are possible. First, the urothelial
cancer developed within a diverticulum, then the entrance of the
diverticulum closed, sealing in the cancer (Fig. 4A). Second, the bladder cancer
stemmed from aberrant urothelium in the submucosal tissue (Fig. 4B). However, other pathomechanisms
may also be possible. One of the limitations of this study was its
inability to clarify the pathomechanism in the present case.
The bladder diverticulum is a special environment
from which cancer can easily invade the perivesical fat surrounding
the bladder. Bladder cancer arising from a diverticulum is not
considered to be as aggressive as a common invasive cancer, which
frequently invades the normal bladder wall. However, Tamas et
al (8) reported that invasive
bladder cancer in a diverticulum can sometimes be aggressive in
terms of local recurrence or metastasis. In the present case, the
extravesical occurrence was detected on a postoperative follow-up
CT.
The present report is the first to document a case
of submucosal urothelial cancer, whose diagnosis was made possible
only by TURBT. Even in a patient with submucosal bladder tumor but
no previous history of bladder cancer, bladder cancer should be
considered in the differential diagnosis. Although the precise
pathomechanism of the present case was unclear, two hypotheses were
advanced. The prognosis of submucosal urothelial bladder carcinoma
is as poor as that of invasive bladder cancer within a diverticulum
due to the diverticular environment.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
TA, FN and SH made substantial contributions in
conception, design and interpretation of data. TA and FN wrote the
manuscript. TD, SIw, SIt and SH made substantial contributions in
interpretation and acquisition of data. SIt performed the
histological examination. TA and FN were responsible for confirming
the authenticity of all raw data. All the authors read and approved
the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient provided written informed consent for
the publication of his data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Antoni S, Ferlay J, Soerjomataram I, Znaor
A, Jemal A and Bray F: Bladder cancer incidence and mortality: A
global overview and recent trends. Eur Urol. 71:96–108. 2017.
|
|
2
|
Knoll LD, Segura JW and Scheithauer BW:
Leiomyoma of the bladder. J Urol. 136:906–908. 1986.
|
|
3
|
Park JW, Jeong BC, Seo SI, Jeon SS, Kwon
GY and Lee HM: Leiomyoma of the urinary bladder: A series of nine
cases and review of the literature. Urology. 76:1425–1429.
2010.
|
|
4
|
Mosier AD, Leitman DA, Keylock J, Nguyen D
and Grant D: Bladder schwannoma-a case presentation. J Radiol Case
Rep. 6:26–31. 2012.
|
|
5
|
Beilan JA, Lawton A, Hajdenberg J and
Rosser CJ: Pheochromocytoma of the urinary bladder: A systematic
review of the contemporary literature. BMC Urol. 13(22)2013.
|
|
6
|
Chen M, Lipson SA and Hricak H: MR imaging
evaluation of benign mesenchymal tumors of the urinary bladder. AJR
Am J Roentgenol. 168:399–403. 1997.
|
|
7
|
Roy C: Tumour pathology of the bladder:
The role of MRI. Diagn Interv Imaging. 93:297–309. 2012.
|
|
8
|
Tamas EF, Stephenson AJ, Campbell SC,
Montague DK, Trusty DC and Hansel DE: Histopathologic features and
clinical outcomes in 71 cases of bladder diverticula. Arch Pathol
Lab Med. 133:791–796. 2009.
|