Introduction
Synovial sarcoma, which accounts for 5-10% of all
soft tissue sarcomas, has a high prevalence among males (1,2).
Synovial sarcoma is the most frequent soft tissue sarcoma in
children and young adults, but its peak incidence occurs in the
third decade of life (3,4). The most frequently affected sites are
the extremities. However, synovial sarcoma can develop from serosal
surfaces, such as the pleura and pericardium (4,5).
Synovial sarcoma has two pathological subtypes: Monophasic and
biphasic. Moreover, synovial sarcoma has unique genomic
characteristics, such as the translocation t(X;18)(p12.2:q11:2)
(6). The standard treatment for
localized synovial sarcoma is surgical resection with adequate
margins (7).
Several oncological reconstructions, such as
megaprostheses or biological reconstructions using irradiation,
autoclaving, pasteurization, or freezing, have been developed for
the bone defects after wide excision of malignant bone or soft
tissue sarcoma. Tsuchiya et al (8) developed a frozen autograft technique.
In the early days of the technique, the affected bone was excised
with an appropriate surgical margin. The resected bones were frozen
and consecutively reconstructed with intramedullary nails or
plates. Later, Shimozaki et al (9) modified this freezing method and
developed a pedicle freezing method. The pedicle freezing method
allows maintenance of the anatomical continuity on either the
proximal or distal side. This modified pedicle freezing method may
potentially achieve a higher bone union rate and limb function than
those achieved with the original free-freezing method.
In this case report, we discuss the excision of a
synovial sarcoma close to the elbow and the successful
reconstruction with a pedicle frozen autograft involving the elbow
joint. To our knowledge, this is the first reconstruction that used
a pedicle frozen autograft involving the joint after the wide
excision of a soft tissue tumor in the elbow.
Case report
Case history
A 35-year-old man presented to our institution with
a four-year history of a growing mass on the anterior surface of
his left elbow. Magnetic resonance imaging revealed a soft tissue
tumor in the brachialis muscle that extended into the cubital fossa
and measured 13.6x4.7x4.0 cm in size (Fig. 1A and B). We found no distant metastases on
18F-fluorodeoxyglucose positron emission tomography.
Following an open biopsy, histopathological examination allowed the
diagnosis of a monophasic fibrous synovial sarcoma. As stipulated
by our institution's standard chemotherapeutic regimen, the patient
received three courses of neoadjuvant chemotherapy with intravenous
doxorubicin and ifosfamide.
Surgical technique (therapeutic
intervention)
After neoadjuvant chemotherapy, the patient
underwent wide excision and reconstruction of his elbow joint.
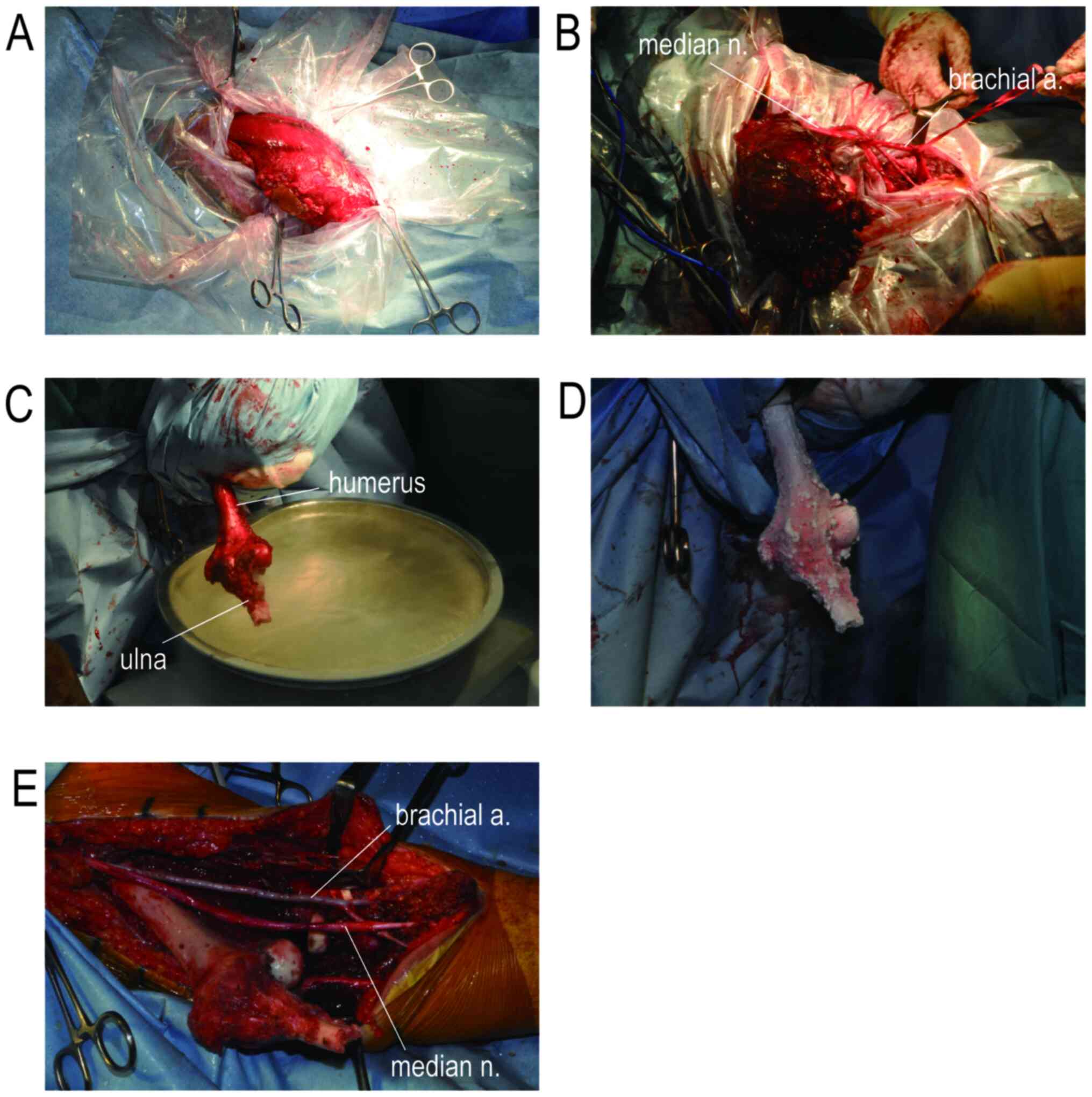
First, two longitudinal skin incisions were made on the
anteromedial and posterior aspects of the elbow. Then, we excised
the tumor together with the brachialis and biceps muscles through
the anteromedial incision (Fig.
2A). We performed careful in situ preparation (10) to preserve the musculocutaneous and
median nerves and brachial vessels close to the surgical margin. We
performed a wide excision without sacrificing these major vessels
and nerves. In the next step, we isolated the tumor, including its
soft tissue margin, using the vinyl sheet but ensuring the
continuity of the vessels and nerves (Fig. 2A). Within the vinyl sheet, we
carefully dissected the vessels and nerves from the soft tissue
before the tumor was resected (Fig.
2B). The preserved vessels and nerves were washed with 100%
ethanol and distilled water to reduce the risk of local recurrence
(10). In the next step, we
dislocated the radial head so that we could isolate the humeroulnar
joint. We performed a z-shaped osteotomy of the ulna at
approximately 8 cm from its proximal end. Finally, the humeroulnar
joint, the proximal part of the ulna, and the distal humerus were
isolated, the latter at 13 cm proximal to its distal end, in
preparation for pedicle freezing. After the tumor-bearing part of
the humerus was sufficiently isolated, the tumor and surrounding
soft tissues were removed (Fig.
2C). Pedicle freezing was performed under tourniquet control to
avoid or at least reduce tumor dissemination. The humerus,
humeroulnar joint, and proximal ulna were immersed in liquid
nitrogen and frozen for 20 min (Fig.
2C). After thawing at room temperature for 15 min (Fig. 2D and E), we washed the autograft with a solution
of distilled water and 1% iodine for 15 min to reduce the risk of
infection. The proximal ulna was fixed with a locking compression
plate, and a suture anchor was used to reattach the radial
collateral ligament.
Postoperative course (follow-up and
outcomes)
The elbow was immobilized with a splint for three
weeks. Thereafter, elbow mobilization was initiated, and two
courses of adjuvant chemotherapy with intravenous doxorubicin and
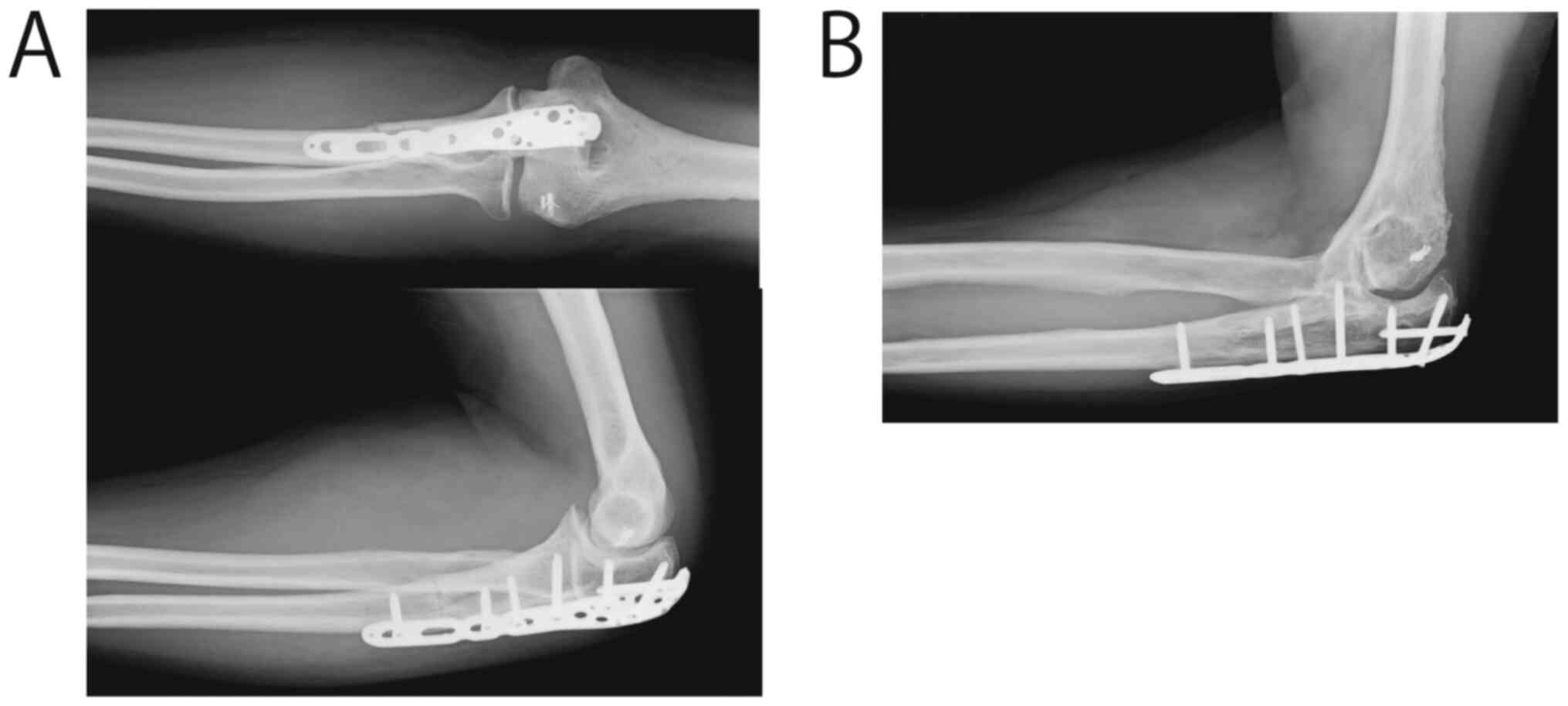
ifosfamide were administered. Seven months postoperatively,
radiography demonstrated complete bone union at the ulnar osteotomy
site (Fig. 3A). The elbow's range
of motion was normal with 0˚ of extension, 120˚ of flexion, 70˚ of
pronation, and 90˚ of supination. Three years after surgery, lung
metastases were found and resected using video-assisted thoracic
surgery. Four years after the autograft reconstruction, osteophytes
and osteosclerosis, but no signs of humeroulnar joint narrowing
were visible on radiography (Fig.
3B). The International Society of Limb Salvage (ISOLS) score
was 83% at the final follow-up four years postoperatively with
neither recurrence nor further metastases. The patient was able to
work as an electronic engineer and play bass guitar.
Discussion
The standard therapeutic approach for synovial
sarcoma is wide surgical excision combined with neoadjuvant and
adjuvant chemotherapy and/or radiotherapy (1,5,7,11).
The frozen autograft technique of Tsuchiya et al (8) uses liquid nitrogen at -196˚C as the
cryogenic agent to destroy tumor cells. Freezing at this extremely
low temperature devitalizes tumor cells by inducing ice crystal
formation and cell dehydration (12). In our case, we used the pedicle
freezing method for elbow reconstruction after wide excision of a
synovial sarcoma for the first time. Complete bone union of the
ulnar z-graft was achieved by the seventh month after surgery, and
upper extremity function was fully preserved. Although radiological
signs of osteoarthritis of the elbow joint were found at the
follow-up after four years, there was no joint space narrowing, and
the patient was not affected in his activities of daily living.
The advantages of using frozen autografts are as
follows: i) They are easy to perform; ii) They require only a short
duration of treatment; iii) They fit perfectly because the anatomy
remains unchanged; iv) There is no need for bone banking; v) They
are easy to attach to any preserved tendons and ligaments; and vi)
They achieve earlier osteogenesis do than pasteurized autografts
(13,14). Zekry et al found that the
five- and ten-year survival rates of frozen autografts were as high
as 91.2%, and that they achieved complete bony union in 97% of
patients after sarcoma or bone metastasis excision (15). Based on these findings, we chose to
perform a frozen autograft in our patient to ensure bone and joint
preservation.
Most descriptions of the use of frozen autografts
for reconstruction after wide excision of sarcomas involve the
lower extremities. There are some reports of biological
reconstruction around the elbow involving free frozen autografts
and flaps (16). Compared to a free
frozen autograft, pedicle frozen autografts have shown a shorter
bone union period and lower postoperative complication rates
(9). In our case, because the
sarcoma was adjacent to both the humerus and ulna, we immersed the
humerus and ulna with the elbow joint in liquid nitrogen during the
pedicle joint freezing to preserve the limb function. Bone union at
the osteotomy site was achieved seven months after surgery, and the
patient showed full elbow joint range of motion.
There are different methods described that preserve
elbow function. In patients with implant use for prosthetic
replacement following the resection of malignant or progressive
benign tumors around the elbow, the survival rate was 64% after
five years (17). However, the
humeral stem loosening rate was high (17). There are several bone recycling
methods, such as autoclaving, irradiation, and pasteurization.
However, these techniques may cause heat- or radiation-induced bone
weakness (18). Some studies
involving histological examinations of these autografts found that
osteogenesis occurred only slowly (13,14).
Postoperative osteoarthritis is a long-term
complication of frozen autografts. A study on frozen autografts
after resection of malignant bone tumors (mostly osteosarcomas)
with epiphyseal involvement compared 27 patients with a mean age of
31.6 years (range 12-72 years) and a mean follow-up period of 94.0
months (range 6-217 months). They found that only 1 of 23 patients
in the total epiphyseal freezing group remained osteoarticular
graft survived until the final follow-up (19). The other 22 patients had developed
osteoarthritic changes by the final follow-up (19). Meanwhile, all four of the patients
who underwent intraepiphyseal resection for partial preservation of
the healthy cartilage had excellent osteoarticular graft survival
(19). However, most of the cases
in their report involved lower extremity joints, and no elbow
joints were described. In our patient, we observed no narrowing of
the humeroulnar joint four years after the surgery. As the elbow
joint is not a weight-bearing joint, osteoarthritis may progress
more slowly than what has been observed in lower extremity
joints.
We describe the first case of wide excision and
reconstruction with pedicle freezing of the elbow joint in a
patient with a monophasic fibrous synovial sarcoma. Based on our
experience with this case, we consider this a promising method for
reconstruction after the excision of malignant bone or soft tissue
tumors around the elbow joint. More patients need to be treated and
followed up to assess the complications and long-term prognosis of
this method.
In conclusion, to the best of our knowledge, this is
the first case of a pedicle frozen autograft involving the elbow
joint following the wide excision of a soft tissue tumor. Although
the reconstruction is challenging due to the complex anatomy of the
elbow, pedicle joint freezing combined with in situ
preparation may help to preserve the limb and the function of the
elbow joint.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YH, YT, HO, YA, HM and KN wrote and edited the
manuscript. YT and HM performed the surgery and postoperative
management. YT critically revised the manuscript. YH and YT are
responsible for confirming the authenticity of the raw data. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
Ethics approval is not applicable since this case
report was considered part of routine follow-up treatment of the
patient. Written informed consent was obtained from the patient in
this case report.
Patient consent for publication
Written consent for publication was obtained from
the patient in the present case report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kottu R and Prayaga AK: Synovial sarcoma
with relevant immunocytochemistry and special emphasis on the
monophasic fibrous variant. J Cytol. 27:47–50. 2010.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Riedel RF, Jones RL, Italiano A, Bohac C,
Thompson JC, Mueller K, Khan Z, Pollack SM and van Tine BA:
Systemic anti-cancer therapy in synovial sarcoma: A systematic
review. Cancers (Basel). 10(417)2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Ferrari A, De Salvo GL, Brennan B, van
Noesel MM, De Paoli A, Casanova M, Francotte N, Kelsey A, Alaggio
R, Oberlin O, et al: Synovial sarcoma in children and adolescents:
The European pediatric soft tissue sarcoma study group prospective
trial (EpSSG NRSTS 2005). Ann Oncol. 26:567–572. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Kerouanton A, Jimenez I, Cellier C,
Laurence V, Helfre S, Pannier S, Mary P, Freneaux P and Orbach D:
Synovial sarcoma in children and adolescents. J Pediatr Hematol
Oncol. 36:257–262. 2014.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Wang S, Song R, Sun T, Hou B, Hong G,
Mallampati S, Sun H, Zhou X, Zhou C, Zhang H, et al: Survival
changes in patients with synovial sarcoma, 1983-2012. J Cancer.
8:1759–1768. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ladanyi M: Fusions of the SYT and SSX
genes in synovial sarcoma. Oncogene. 20:5755–5762. 2001.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Singer S, Baldini EH, Demetri GD, Fletcher
JA and Corson JM: Synovial sarcoma: Prognostic significance of
tumor size, margin of resection, and mitotic activity for survival.
J Clin Oncol. 14:1201–1208. 1996.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tsuchiya H, Wan SL, Sakayama K, Yamamoto
N, Nishida H and Tomita K: Reconstruction using an autograft
containing tumour treated by liquid nitrogen. J Bone Joint Surg Br.
87:218–225. 2005.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Shimozaki S, Yamamoto N, Shirai T, Nishida
H, Hayashi K, Tanzawa Y, Kimura H, Takeuchi A, Igarashi K, Inatani
H, et al: Pedicle versus free frozen autograft for reconstruction
in malignant bone and soft tissue tumors of the lower extremities.
J Orthop Sci. 19:156–163. 2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Matsumoto S, Kawaguchi N, Manabe J and
Matsushita Y: ‘In situ preparation’: New surgical procedure
indicated for soft-tissue sarcoma of a lower limb in close
proximity to major neurovascular structures. Int J Clin Oncol.
7:51–56. 2002.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Pasquali S and Gronchi A: Neoadjuvant
chemotherapy in soft tissue sarcomas: Latest evidence and clinical
implications. Ther Adv Med Oncol. 9:415–429. 2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Yamamoto N, Tsuchiya H and Tomita K:
Effects of liquid nitrogen treatment on the proliferation of
osteosarcoma and the biomechanical properties of normal bone. J
Orthop Sci. 8:374–380. 2003.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Tanzawa Y, Tsuchiya H, Shirai T, Hayashi
K, Yo Z and Tomita K: Histological examination of frozen autograft
treated by liquid nitrogen removed after implantation. J Orthop
Sci. 14:761–768. 2009.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ehara S, Nishida J, Shiraishi H and
Tanakawa Y: Pasteurized intercalary autogeneous bongraft:
Radiographic and scintigraphic features. Skeletal Radiol.
29:335–339. 2000.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Zekry KM, Yamamoto N, Hayashi K, Takeuchi
A, Higuchi T, Abe K, Taniguchi Y, Alkhooly AZ, Abd-Elfattah AS,
Fouly EH, et al: Intercalary frozen autograft for reconstruction of
malignant bone and soft tissue tumours. Int Orthop. 41:1481–1487.
2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Hirakawa A, Nagano A, Komura S, Ishimaru
D, Kawashima K and Akiyama H: Reconstruction of a malignant soft
tissue tumor around the elbow joint using a frozen autograft
treated with liquid nitrogen, in combination with a free
anterolateral thigh flap: A report of two cases. Case Reports Plast
Surg Hand Surg. 5:80–86. 2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Henrichs MP, Liem D, Gosheger G,
Streitbuerger A, Nottrott M, Andreou D and Hardes J: Megaprosthetic
replacement of the distal humerus: Still a challenge in limb
salvage. J Shoulder Elbow Surg. 28:908–914. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Singh VA, Nagalingam J, Saad M and Pailoor
J: Which is the best method of sterilization of tumour bone for
reimplantation? A biomechanical and histopathological study. Biomed
Eng Online. 9(48)2010.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Hayashi K, Yamamoto N, Takeuchi A, Miwa S,
Igarashi K, Higuchi T, Abe K, Taniguchi Y, Aiba H, Araki Y, et al:
Clinical course of grafted cartilage in osteoarticular frozen
autografts for reconstruction after resection of malignant bone and
soft-tissue tumor involving an epiphysis. J Bone Oncol.
24(100310)2020.PubMed/NCBI View Article : Google Scholar
|