Introduction
Neurilemmoma, also referred to as Schwann cell
tumor, originates from Schwann cells in the neuroectodermal lobe.
The majority of neurilemmomas are benign tumors and malignant
transformation is rarely observed (1). By contrast, malignant peripheral nerve
sheath tumor (MPNST) is an aggressive neoplasm composed of spindled
cells that may occur sporadically, and it often associated with
radiation exposure or in the clinical context of neurofibromatosis
type 1(2). MPNST is rare and, to
the best of our knowledge, it has not been reported outside of
China. A case of intrascrotal schwannoma was first reported in
Japan in 1991 and 6 more cases were recorded in the following years
(3,4). Only one case of testicular
neurilemmoma was reported in China in 2003(5). The presence of etiological factors,
such as chronic low doses of ionizing radiation, may trigger
carcinogenesis in the testicle (6).
The aim of the present study was to discuss a case
of diagnosis and treatment of a rare case of testicular MPNST.
Case report
A 30-year-old man was admitted to the Department of
Urology of the Affiliated Hospital of Guizhou Medical University
(Guiyang, China) in August 2017 due to pain in the left testis and
groin over 1 month. The patient reported no other symptoms.
Physical examination identified a hard mass (~5.0x5.0 cm) in the
left testis. The skin temperature of the scrotum was normal and
scrotal light transmission test was negative. Urine culture and
routine blood examination revealed no significant findings.
Brightness-mode ultrasound examination revealed a mixed mass with
unclear nature, sized ~5.0x5.0 cm, in the left testis.
Subsequently, computed tomography (CT) examination revealed a left
testicular space-occupying mass and multiple enlarged
retroperitoneal and bilateral peritesticular lymph nodes. Other
laboratory tests (erythrocyte sedimentation rate and liver
function) revealed no abnormal results.
After undergoing a thorough preoperative examination
and obtaining consent from the patient and his immediate family,
the patient underwent radical resection of the left testicular
tumor (left testicular excision). After performing general
anesthesia, the skin of the left scrotum was cut and the
subcutaneous tissue and testis were gradually exposed.
Macroscopically, the tumor was sized ~5.0x5.0 cm, texture was hard
and grayish white, the fascia of testis was closely adjoined to the
skin. The left testis, epididymis and surrounding tissues were
completely removed following vascular ligation and hemostasis.
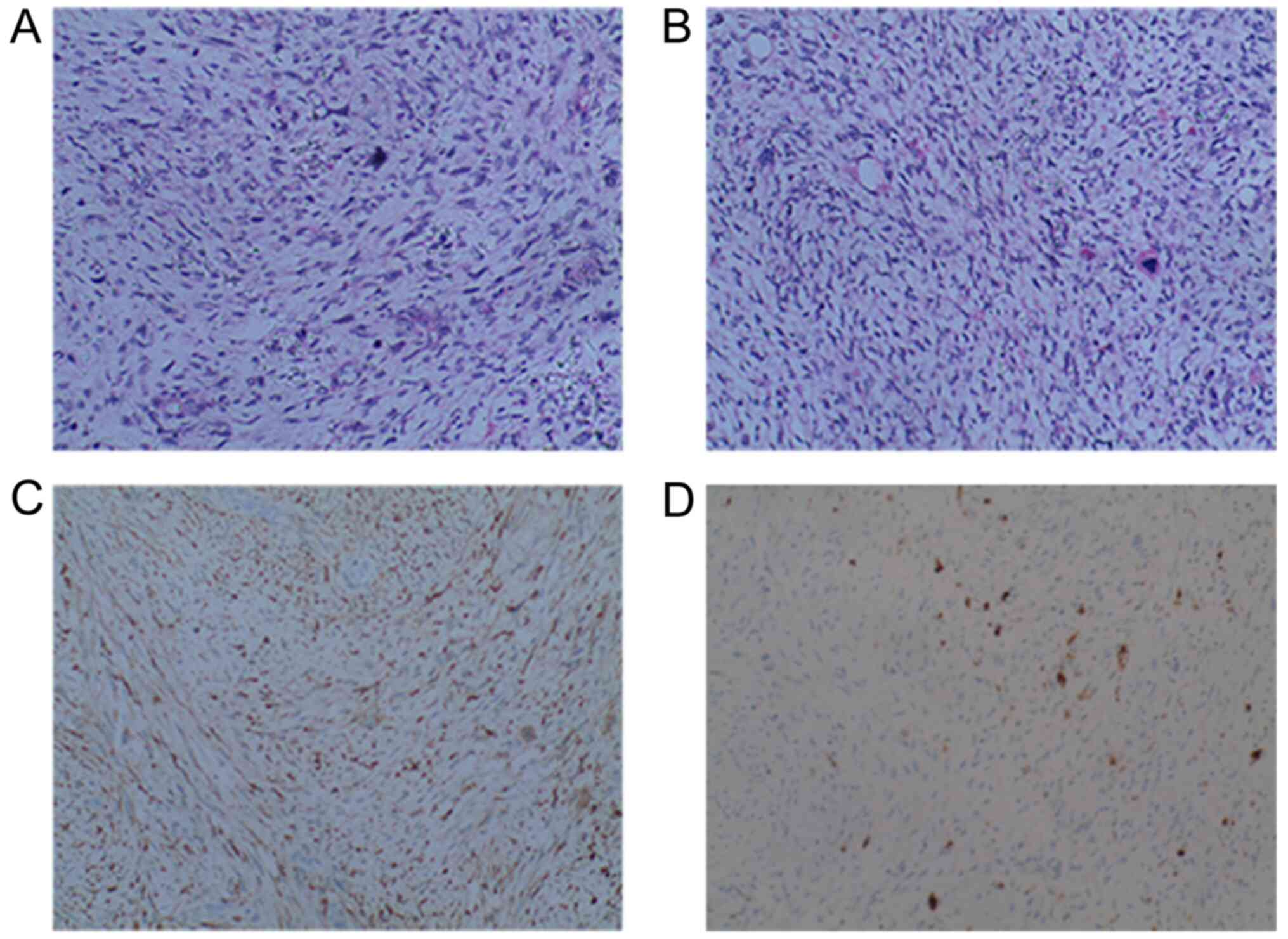
Histopathological examination of the removed tissue specimen
confirmed the diagnosis of malignant peripheral neurilemmoma
(Fig. 1). On hematoxylin and eosin
staining, the tumor was composed of spindled tumor cells, whereas
immunohistochemical examination revealed that the tumor cells were
CD57+ and S-100+, as well as identifying the
presence of giant tumor cells. The patient recovered well following
the operation and was discharged 7 days after operation. After
discharge, the patient was lost to follow-up.
Discussion
Schwannoma commonly originates from tissues with
abundant nerve supply, such as the stomach, ears and parotid glands
(7-9).
The most common age of patients with neurilemmomas is 30-50 years.
Most cases are benign, and malignant transformation is rarely
observed. The presence of additional etiological factors, such as
chronic low doses of ionizing radiation, may initiate the process
of carcinogenesis in the testicle (6). Tumor growth is slow in the early
stages. However, with increased tumor volume, compression symptoms
of adjacent organs may develop. In the urinary system, the primary
symptoms are pain and urinary tract irritation. Microscopically,
schwannoma is characterized by a constantly changing Antoni A
region (dense cellular area) and Antoni B region (hypocellular
area). In the highly differentiated Antoni A area, the nuclei may
be seen arranged in a in palisade pattern, and mitotic figures are
occasionally observed (10).
Primary MPNST is a rare and poorly understood
entity. The diagnosis of MPNST relies on clinical manifestation and
pathological results, whereas histopathological diagnosis
predominantly involves light microscopy (11). Imaging examination is helpful in
terms of localization and qualitative diagnosis of the tumor.
Brightness-mode ultrasound examination revealed a nodular
hypoechoic mass with a clear boundary. On CT scan, the tumor
density was slightly lower compared with that of muscle or
presented as mixed density. On MRI, benign schwannomas are lightly
hyperintense relative to muscle on T1-weighted images and have a
target appearance on T2-weighted images with a peripheral
hyperintense rim and central hypointensity. Intense contrast
enhancement is seen in most schwannoma cases (12). The typical target appearance may not
be present in MPNST (12). However,
the lack of MRI data may be a limitation to this study.
The primary treatment for schwannomas is surgery
(13). Particularly for MPNSTs, in
order to prevent tumor recurrence, the main tumor and its
surrounding tissue should be completely removed to the greatest
extent possible (13). The role of
chemotherapy in MPNSTs has not been clearly determined. A series of
chemotherapy drugs have been used in patients with MPNST and have
shown some effectiveness (14). It
has been reported that there is a certain association between
testicular cancer and sarcoidosis, further contributing to the
uncertainty surrounding the treatment of MPNSTs (15). With the rapid development of
biological characterization and molecular biology techniques, novel
targeted drugs and gene therapy may improve the treatment of this
disease.
At present, literature remains sparse on the
prognostic factors and ideal treatment methods to control MPNSTs.
While surgical excision with negative margins and radiation therapy
seems to be the current mainstay, the prognosis remains poor
(16). In the present case, the
tumor location was superficial, resection was complete, therefore,
the prognosis was good. However, long-term follow-up of MPNSTs is
necessary due to the possibility of recurrence.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
KT conceptualized and designed the study. DL, PC, BC
and YM performed the experiments. ZL, FS and YZ analyzed the data.
DL wrote the manuscript. YM and KT reviewed and edited the
manuscript. All authors confirm the authenticity of all the raw
data. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of the Affiliated Hospital of Guizhou Medical University
(approval no. 2013023). The patient provided written informed
consent.
Patient consent for publication
The patient agreed to the collection and publication
of the present case study.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Davis DD and Kane SM: Neurilemmoma.
StatPearls Publishing, Treasure Island, FL, 2021.
|
|
2
|
Mishra B, Madhusudhan KS, Kilambi R, Das
P, Pal S and Srivastava DN: Malignant schwannoma of the esophagus:
A rare case report. Korean J Thorac Cardiovasc Surg. 49:63–66.
2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Shimizu H, Tsuchiya A and Kusama H: A case
of intrascrotal neurilemmoma. Hinyokika Kiyo. 37:303–304.
1991.PubMed/NCBI(In Japanese).
|
|
4
|
Matsui F, Kobori Y, Takashima H, Amano T
and Takemae K: A case of intrascrotal schwannoma. Hinyokika Kiyo.
48:749–751. 2002.PubMed/NCBI(In Japanese).
|
|
5
|
Jiang R, Chen JH, Chen M and Li QM: Male
genital schwannoma, review of 5 cases. Asian J Androl. 5:251–254.
2003.PubMed/NCBI
|
|
6
|
Bazalytska SV, Persidsky Y and Romanenko
AM: Моlecular mechanisms of initiation of carcinogenesis in the
testis. Exp Oncol. 41:224–234. 2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Pu C and Zhang K: Gastric schwannoma: A
case report and literature review. J Int Med Res.
48(300060520957828)2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Kim KS, Lee H, Choi JH, Hwang JH and Lee
SY: Schwannoma of the posterior branch of the great auricular
nerve. Arch Craniofac Surg. 21:368–371. 2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Chowdhary S, Thangavel S, Ganesan S and
Alexander A: Extratemporal intraparotid facial nerve schwannoma.
BMJ Case Rep. 14(e239407)2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Donnelly MJ, al-Sader MH and Blayney AW:
Benign nasal schwannoma. J Laryngol Otol. 106:1011–1015.
1992.PubMed/NCBI View Article : Google Scholar
|
|
11
|
James AW, Shurell E, Singh A, Dry SM and
Eilber FC: Malignant peripheral nerve sheath tumor. Surg Oncol Clin
N Am. 25:789–802. 2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Anil G and Tan TY: Imaging characteristics
of schwannoma of the cervical sympathetic chain: A review of 12
cases. AJNR Am J Neuroradiol. 31:1408–1412. 2010.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Halliday J, Rutherford SA, McCabe MG and
Evans DG: An update on the diagnosis and treatment of vestibular
schwannoma. Expert Rev Neurother. 18:29–39. 2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Bradford D and Kim A: Current treatment
options for malignant peripheral nerve sheath tumors. Curr Treat
Options Oncol. 16(328)2015.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Bassoulet J, du Chatelard P, L'Her P,
Natali F, Morel C, Cosnard G, Merrer J, Guillemot MC and Timbal Y:
Cancer of the testis, sarcoidosis and neurinoma. Ann Urol (Paris).
24:219–323. 1990.PubMed/NCBI(In French).
|
|
16
|
Mullins BT and Hackman T: Malignant
peripheral nerve sheath tumors of the head and neck: A case series
and literature review. Case Rep Otolaryngol.
2014(368920)2014.PubMed/NCBI View Article : Google Scholar
|